 .
.
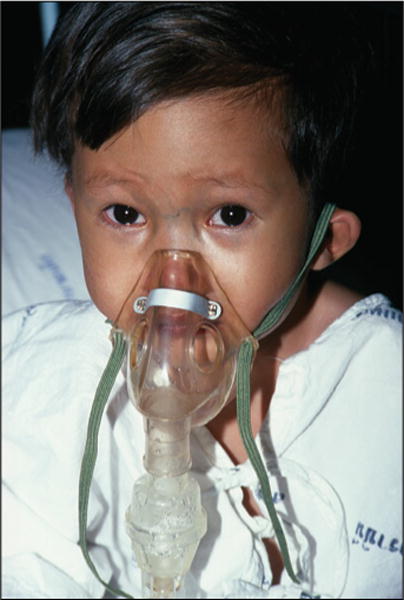
Andy Crump, TDR, WHO/Science Photo Library.
Pausing to reflect on World Pneumonia Day, we celebrate numerous achievements in the fight against pneumonia in children. Most notably, annual pneumonia deaths among children younger than 5 years old have declined from 1.7 million deaths in 2000, to 0.9 million deaths in 2015.1 Vaccine and antibiotic use have spurred this mortality reduction but maximum benefits will only be achieved when these interventions are implemented with high coverage and quality across diverse cultures and health systems. Much work remains. As we transition into the era of Sustainable Development, new interventions need to be identified that will work synergistically with established approaches to further reduce mortality, and even accelerate the pace of that decline.
The logical question is what other interventions will reach across increasingly complex settings to achieve a degree of success comparable with our current vaccine and antibiotic portfolio. No single solution will suffice. Vaccine development will continue to be central, especially new pneumococcal and respiratory syncytial virus vaccines. Beyond vaccine development, progress will rely upon a combination of locally adapted interventions optimised to address the aetiological contribution of pathogens causing pneumonia deaths, while also reducing the prevalence and improving the management of mortality risk factors such as hypoxaemia, malnutrition, anaemia, prematurity, HIV infection and exposure, and environmental factors (hygiene, water, and air pollution). Data systems and decision support tools, pulse oximetry implementation, and severity of illness scores offer insight into how mortality reduction might next unfold.
WHO Integrated Management of Childhood Illness (IMCI) guidelines recommend pneumonia management that optimises diagnostic sensitivity to ensure possible bacterial pneumonia cases do not go untreated. Yet guideline implementation remains suboptimal across the highest burden countries in Africa and Asia, largely beset by weak, understaffed health systems unable to provide adequate supervision. These systems fail to sufficiently empower health-care providers to identify and treat children with high-risk comorbidities. Continued investment to strengthen effective district and community level training and supervision will remain the essential first step, but innovative development of locally relevant data systems and decision support tools could be key adjuncts. Systems that facilitate real-time data access could enable remote, efficient, responsive, and cost-effective supervision, as has been illustrated by HIV/tuberculosis programmes in several developing countries.2 Automated decision support tools might also improve patient-centered, guideline-compliant decision-making (including comorbidity identification and management) to achieve improved health outcomes.3 Research in locally applicable data system and decision support tools should be a priority.
In the 2014 WHO IMCI update, pulse oximetry was added as an assessment step for frontline facility-based health workers, along with a recommendation to refer children with cough or difficult breathing and hypoxaemia less than 90%.4 Insights are needed into where and how oximetry best fits into the IMCI care pathways and whether it will be affordable and sustainable. Is oximetry best employed as a triage tool for all children or reserved for only those with cough or difficulty breathing? At which system levels can oximetry be cost-effectively implemented? Although promising, whether frontline health facilities or community health workers will have major impact using oximetry in all settings is unknown. Given that a health system’s capacity and hypoxaemia prevalence can vary between, and within, countries, the answer will probably be found locally.5 For example, a rural Malawian study6 of outpatient oximetry found that hypoxemia was not only commonly present in pneumonia cases, but also that oximetry improved the identification and referral of hypoxaemic children. This study also identified a concerning high proportion of cases (>60%) who were referral eligible by hypoxaemia alone, but missed by 2014 IMCI clinical referral criteria. Another forthcoming study from Malawi reports the association of an oxygen saturation 90–92%, moderate hypoxaemia, with higher pneumonia mortality risk, raising the question that a threshold of less than 90% might not be the most appropriate for initiation of oxygen or hospital referral everywhere. Additional studies from other countries examining these areas will be informative.
Practical pneumonia severity of illness scores—which use age, hypoxaemia, and comorbidities like malnutrition as cornerstones, but adapted to local disease epidemiology and health system capacity—are gaining traction as objective tools to prioritise children with an increased mortality risk for earlier referral, closer home follow-up, or advanced treatments that require greater resources, such as bubble continuous positive airway pressure (bCPAP).7–10 bCPAP reduced child pneumonia mortality versus low-flow oxygen, in a randomised trial in a Bangladesh tertiary intensive care unit;11 a randomised trial at a lower-level district hospital in Malawi is ongoing. Work to externally validate and locally adapt the South African Respiratory Index of Severity Score is also forthcoming from the Pneumonia Etiology Research for Child Health Study and from Malawi.7 Prospective implementation research evaluating the clinical impact of such scores, perhaps imbedded within decision support tools, is needed.12
Any advances in pneumonia prevention, triage, or treatment should be accompanied by improvements in care access; this is particularly critical to address for children unable to reach care in a timely manner, who present later with greater disease severity and preventable mortality. If more children are not accessed, then mortality reduction will inevitably plateau. Improving demand for care through community sensitisation to pneumonia prevention and symptom recognition should also accelerate so that no one is left behind in our collective movement to prevent child pneumonia deaths.
Acknowledgments
LLH, AHB, and KLO’B report grants from GSK and Pfizer, outside of the submitted work.
Footnotes
EDM, CK, ASG, and TC declare no conflicts of interest.
References
- 1.Liu L, Oza S, Hogan D, et al. Global, regional and national causes of child mortality in 2000–2015—implications for the Sustainable Development Goals. Lancet. doi: 10.1016/S0140-6736(16)31593-8. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Devi BR, Syed-Abdul S, Kumar A, et al. mHealth: An updated systematic review with a focus on HIV/AIDS and tuberculosis long term management using mobile phones. Comput Methods Programs Biomed. 2015;122:257–65. doi: 10.1016/j.cmpb.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Ginsburg AS, Delarosa J, Brunette W, et al. mPneumonia: development of an innovative mhealth application for diagnosing and treating childhood pneumonia and other childhood illnesses in low-resource settings. PloS One. 2015;10:e0139625. doi: 10.1371/journal.pone.0139625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Integrated Management of Childhood Illness: Chart Booklet. Geneva: WHO; 2014. [Google Scholar]
- 5.Subhi R, Adamson M, Campbell H, Weber M, Smith K, Duke T. The prevalence of hypoxaemia among ill children in developing countries: a systematic review. Lancet Infect Dis. 2009;9:219–27. doi: 10.1016/S1473-3099(09)70071-4. [DOI] [PubMed] [Google Scholar]
- 6.McCollum ED, King C, Deula R, et al. Pulse oximetry for children with pneumonia treated as outpatients in rural Malawi. Bull World Health Organ. 2016 doi: 10.2471/BLT.16.173401. published online Oct 11, 2016. http://www.who.int/bulletin/online_first/BLT.16.173401.pdf?ua=1. [DOI] [PMC free article] [PubMed]
- 7.Reed C, Madhi SA, Klugman KP, et al. Development of the Respiratory Index of Severity in Children (RISC) score among young children with respiratory infections in South Africa. PLoS ONE. 2012;7:e27793. doi: 10.1371/journal.pone.0027793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olson D, Davis N, Milazi R, et al. Development of a severity of illness scoring system (inpatient triage, assessment and treatment) for resource-constrained hospitals in developing countries. Trop Med Int Health. 2013;18:871–78. doi: 10.1111/tmi.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu LY, Ruthazer R, Wilson I, et al. Brief hospitalization and pulse oximetry for predicting amoxicillin treatment failure in children with severe pneumonia. Pediatrics. 2006;118:e1822–30. doi: 10.1542/peds.2005-2673. [DOI] [PubMed] [Google Scholar]
- 10.King C, McCollum ED, Mankhambo L, et al. Can we predict oral antibiotic treatment failure in children with fast-breathing pneumonia managed at the community level? A prospective cohort study in Malawi PLoS One. 2015;10:e0136839. doi: 10.1371/journal.pone.0136839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chisti MJ, Salam MA, Smith JH, et al. Bubble continuous positive airway pressure for children with severe pneumonia and hypoxaemia in Bangladesh: an open, randomised controlled trial. Lancet. 2015;386:1057–65. doi: 10.1016/S0140-6736(15)60249-5. [DOI] [PubMed] [Google Scholar]
- 12.McCollum ED, King C, Hollowell R, et al. Predictors of treatment failure for non-severe childhood pneumonia in developing countries—systematic literature review and expert survey—the first step towards a community focused mHealth risk-assessment tool? BMC Pediatrics. 2015;15:74. doi: 10.1186/s12887-015-0392-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


