Abstract
Neurostimulation is rapidly emerging as an important treatment modality for psychiatric disorders. One of the fastest-growing and least regulated approaches to noninvasive therapeutic stimulation involves the application of weak electrical currents. Widespread enthusiasm for low-intensity transcranial electrical current stimulation (tCS) is reflected by the recent surge in direct-to-consumer device marketing, do-it-yourself enthusiasm, and an escalating number of clinical trials. In the wake of this rapid growth, clinicians may lack sufficient information about tCS to inform their clinical practices. Interpretation of tCS clinical trial data is aided by familiarity with basic neurophysiological principles, potential mechanisms of action of tCS, and the complicated regulatory history governing tCS devices. A growing literature includes randomized controlled trials of tCS for major depression, schizophrenia, cognitive disorders and substance use disorders. The relative ease of use and abundant access to tCS may represent a broad-reaching and important advance for future mental health care. Evidence supports application of one type of tCS, transcranial direct current stimulation (tDCS), for major depression. However, tDCS devices do not have regulatory approval for treating medical disorders, evidence is largely inconclusive for other therapeutic areas, and their use is associated with some physical and psychiatric risks. One unexpected finding to arise from this review is that the use of cranial electrotherapy stimulation (CES) devices – the only category of tCS devices cleared for use in psychiatric disorders - is supported by low quality evidence.
INTRODUCTION
Neurostimulation can be defined as any intervention intended to alter nervous system function using energy fields such as electricity, magnetism, or both. While historical literature describes neurostimulation to treat physical maladies for over a thousand years (1), its use for psychiatric disorders became popular in the past century. Since the 1930s (2), electroconvulsive therapy (ECT) has been recognized as an effective treatment for severe depression, catatonia, and other mental health disorders. In addition to ECT, clinicians are expected to understand newer forms of neurostimulation such as vagus nerve stimulation (VNS), repetitive transcranial magnetic stimulation (rTMS), and deep brain stimulation (DBS) (3).
For a number of reasons, therapeutic neurostimulation has seen a recent surge of interest. First, neurostimulation targets electrical activity in brain networks, acting through different mechanisms than pharmacotherapy, thus offering the hope of treatment success where medications have failed. Identifying and targeting specific brain regions or circuits to reduce psychiatric symptoms may offer a level of focality beyond that offered by ECT or pharmacotherapy. Second, we are surrounded by technology that interfaces with the human body, such as “smartphones,” watches with sensors, and “apps” that monitor an individual’s physical activity. As society accepts these devices, increased use of medical technology that interacts with the central nervous system may naturally follow. Third, since neurostimulation is associated with different side effects than medications, it may be perceived as having superior tolerability for use alone or in combination with pharmacotherapy (4) or psychotherapy (5). Finally, a growing body of evidence suggests neurostimulation might modify a broad spectrum of brain functions, giving rise to speculation about its potential to improve cognition or nonspecific symptoms in healthy individuals, thereby suggesting that similar gains might be achieved in psychiatrically ill patients.
In this article, we provide an overview of the devices and modalities that use low-energy electrical current for brain stimulation, described as transcranial current stimulation (tCS). Emerging technology has fueled rapid expansion of these devices in the last few years, without commensurate growth in accessible, clinician-directed information. To address this knowledge gap, here we provide a comprehensive review of the engineering and neurophysiology underlying tCS, relevant data from clinical trials, and potential safety considerations.
SECTION 1: ELECTRICAL ENGINEERING AND NEUROPHYSIOLOGY
Based on the principle that application of an electric current to the skin generates an electric field, tCS devices differ from one another based on the waveform of the electric current used. Perhaps the best-known type of tCS is transcranial direct current stimulation (tDCS), which delivers a constant, or “direct” waveform. Another type of tCS, called cranial electrical stimulation (CES), uses proprietary waveforms that may fluctuate over time. Other tCS approaches include use of sine waves (i.e., transcranial alternating current stimulation, tACS) or broadband noise (i.e., transcranial random current stimulation, tRNS). Regardless of the waveform, the electrical resistance of the pathway through the patient’s tissues determines how much voltage the device applies to achieve the level of current selected by the user.
Stimulation devices deliver a predefined amount of electric current (I; measured in mA). According to Ohm’s law (V=IR), the amount of voltage (V) that is required to produce a specific current (I) depends on the resistance (R) between the two connectors on the device. Since the wires and electrodes have very low resistance, the main resistance in the system comes from the interface between the electrodes and the biological tissue located between the electrodes. Ohm’s law dictates that a greater voltage will be needed to pass a current through tissue with higher resistance. During tCS, higher resistance (and hence higher voltage) can result in patient discomfort and may lead to skin burns under the electrodes (reviewed in Section 3) (6). Typical reasons for heightened resistance are poor electrode contact with skin, or use of electrodes made from materials that do not conduct well. Devices that enforce a maximum upper limit of voltage mitigate this risk. Safe delivery of tCS requires low resistance for the duration of a stimulation session; this is achieved through steps taken to ensure 1) use of electrodes with good conductive properties, 2) good contact between electrodes and skin, and 3) integrity of connections between electrodes, lead wires, and the stimulator.
Spatial Targeting: Electrode Montages
The spatial positioning of stimulation electrodes on the scalp can generate the misleading perception that only the brain underneath the electrodes, and no other area, is stimulated. This notion is mostly incorrect since the human head exhibits heterogeneous electrical properties. For example, when delivered through scalp electrodes, a large fraction of current is shunted away through the skin and does not penetrate the skull. Current may also travel through the orbits, foramen magnum or cranial nerve foramina, as low-resistance interstitial fluid creates electrical shunts at these sites. Several tCS devices deliver stimulation through one or more electrodes placed on the ears, face, or elsewhere below the head and neck. It is possible that nonspecific cranial nerve stimulation plays an important part in the effects of tCS. Once the electric field reaches the brain, tCS has a certain strength and direction; both are relevant for modulating the activity of individual neurons or networks of neurons. Similar to antennae, neurons must be positioned so they are aligned with the direction of an oncoming electrical field if the field is to influence them. When this happens, a series of events leads to a change in the voltage across the neuron’s membrane (7); stronger electrical fields (i.e., those with greater amplitude) have greater effects on the neuronal membrane. Spatial targeting using computer simulations of the electric field distribution, as a function of electrode number, size and location has been proposed (8), but lacks validation as an approach to guide clinical tCS. Moreover, given the distributed and complex deficits in neuronal networks associated with psychiatric disorders, identifying the correct target area(s) for therapeutic stimulation of a specific disorder or symptom remains an important challenge for the field.
Neurophysiological Effects of tCS
The electrical fields used in tDCS are generally considered a subthreshold perturbation, meaning that tDCS, by itself, is not thought to cause neuronal depolarization (Figure 1A). However, the net effect of tDCS does not occur in isolation. Communication between individual neurons and neuronal networks is nonlinear and complex, with a large number of inputs influencing the activity of any individual neuron. Therefore, even a small change in the membrane voltage may impact neuronal firing.
Figure 1A. Sub- and Suprathreshold Energy Input on Neuronal Action Potentials.
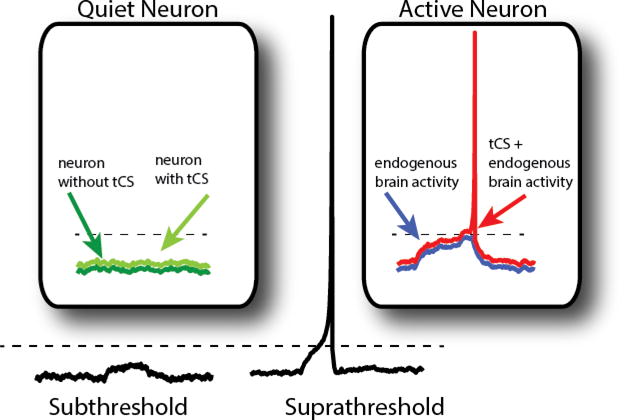
Subthreshold membrane fluctuations are not sufficient to generate an action potential (left). However, if intrinsic fluctuations in a neuron’s membrane voltage move it closer to its threshold, application of an inherently subthreshold input, such as tCS, can trigger an action potential (right). Dashed line indicates threshold.
Variation in the direction of current flow also impacts neuronal firing. As described above, when current travels in one direction, the effect is to depolarize or enhance chance of firing. However, current traveling in the opposite direction causes hyperpolarization of the membrane, making the neuron less likely to fire relative to its resting state. Unfortunately, this neurophysiological principle is associated with the unproven model wherein “anodal tDCS” excites brain activity in the region under that electrode, and “cathodal tDCS” inhibits brain activity in the region beneath that electrode. While application of this simplistic, and likely incorrect, model (9) has been used to support montages implemented in clinical trials (reviewed in Section 2), further research is needed to characterize the relationship between cellular physiology and clinical outcomes.
The potential therapeutic benefit of tCS arises because the neurophysiological effect of current applied during a single session is durable, to some extent, over time after the stimulation ceases. This phenomenon was demonstrated by a series of experiments wherein motor cortex neurons were stimulated with tDCS, and their excitability was measured after stimulation stopped (10). It is important to recognize that much of what we know about tDCS comes from studies of the motor cortex, and it remains unclear if the same principles apply to other brain regions, such as the prefrontal cortex. Furthermore, since neuronal organization may differ across the brain, it is possible that the same stimulation can result in varied effects when applied to different regions. Nevertheless, a number of experiments have now demonstrated enduring functional effects of tDCS on (non-motor) cortical activity, persisting in the hour after stimulation ceases (e.g.,(11–13)).
SECTION 2: REVIEW OF PUBLISHED RANDOMIZED CONTROLLED TRIALS
To describe the current evidence base for therapeutic effects of tCS in psychiatry, we performed a focused review of published clinical trial data, extracted from Pubmed, recent review articles (14–16), and meta-analyses (17; 18). Based on the known limitations of open-label pilot studies (19), we included only treatment-based, randomized, controlled trials (RCTs). Where there were no clinical RCTs, we included key proof of concept studies to illustrate the status of the field. The literature search was performed on 3/24/2016 and updated 11/21/2016. Search terms included tDCS, CES, tACS, tRNS, and several emerging tCS approaches such as external trigeminal nerve stimulation (eTNS) and transcutaneous vagus nerve stimulation (tVNS). Each modality term was searched separately, with words spelled out and in abbreviated form, and searched in combination with each reviewed psychiatric disorder (major depressive disorder (MDD), bipolar disorder, schizophrenia, anxiety, obsessive-compulsive disorder, substance use, and dementia). Primary outcomes of the trials for MDD, schizophrenia, dementia/cognitive disorders, and substance use disorders appear below. Details of administration, such as anatomical target, stimulation strength and duration, are included in corresponding tables. Meta-analyses are also summarized below.
Consensus scores were generated to review quality of the evidence base supporting tCS for several therapeutic areas by evaluating scientific rigor of the published RCTs. A list of 21 quality indicators (see Supplemental information) was developed by the authors, based on the GRADE scoring guidelines (20) that reflecting elements required for a well-designed tDCS RCT. These indicators incorporated standard elements of clinical trial design, and those unique to studying clinical effects of tCS, such as standardization of the environment during stimulation. Furthermore, it was noted that most while pharmacotherapy RCTs use a double-blind design (i.e., patients and raters blind to treatment assignment), tCS studies typically also need a blinded treatment administrator (i.e., triple-blind) to ensure the nature of the investigational treatment remains concealed. In light of possible tCS interactions with psychotropic medications, we evaluated the extent to which investigators gathered and reported data on participants’ concurrent medication use. A percentage score (0–100%; rounded to the nearest whole number) was calculated for each trial, based on the number of indicators present, with 100% reflecting the highest quality rating. Each report was independently reviewed and scored by at least two coauthors; group discussion took place to resolve discrepancies and achieve consensus scoring.
Randomized Controlled Trials and Meta-Analyses of tCS for Major Depression
Efficacy studies for depression represent the largest group of available tCS RCT data. tDCS is the dominant modality (Table 1), typically with the anode placed over the left dorsolateral prefrontal cortex (DLPFC). Some studies restricted enrollment to (unipolar) MDD and others included participants with unipolar or bipolar major depressive episodes (MDE). Some of these studies allowed participants to remain on stable regimens of psychotropic medications while others required medication-free participants.
Table 1.
Quality of tCS RCTs (n=16) for Major Depressive Episodes
| Study | N per Group | Type | Anatomical Target(s) | Stimulation Strength | Session Duration, Number of Sessions (Total) | Main Findingsa | Quality Metric Score (%)b |
|---|---|---|---|---|---|---|---|
| Barclay et al., 2014 (33) | Sham: 55 Active: 60 Total: 115 |
CES | Cortex | 100 μA 0.5 Hz |
1 hour daily, 5 days/week for 5 weeks (25) | Active stimulation reduced anxiety and depressive symptoms | 63 |
| Bennabi et al., 2015 (27) | Sham: 12 Active: 12 Total: 24 |
tDCS | L DLPFC | 2 mA | 30 min, twice per day, for 5 days (10) | No difference between active and sham stimulation on depression | 68 |
| Blumberger et al., 2012 (26) | Sham: 11 Active: 13 Total: 24 |
tDCS | L DLPFC | 2 mA | 20 min/day, 5 times per week for 3 weeks (15) | No difference in remission from depression between active and sham stimulation | 74 |
| Boggio et al., 2008 (22) | Sham: 10 Active Control: 9 Active: 21 Total: 40 |
tDCS | L DLPFC | 2 mA | 20 min/day, 5 times per week for 10 days (10) | Active stimulation reduced depressive symptoms | 68 |
| Brunoni et al., 2013 (4) | PBO/Sham: 30 Sert/Sham: 30 PBO/Active: 30 Sert/Active: 30 Total: 120 |
tDCS | L DLPFC | 2 mA | 30 min/day, 5 times per week for 2 weeks, then 2 sessions every other week (12) | Sert/Active Stimulation was superior to Sert/Sham, PBO/Active, and PBO/Sham group | 89 |
| Brunoni et al., 2014 (28) | Therapy/Sham: 17 Therapy/Active: 20 Total: 37 |
tDCS | L DLPFC | 2 mA | 30 min/day for 10 days (10) | No difference between active and sham stimulation on depression | 79 |
| Fregni et al., 2006 (21) | Sham: 5 Active: 5 Total: 10 |
tDCS | L DLPFC | 1 mA | 20 min/day for 5 alternate days (5) | Active stimulation reduced depressive symptoms | 32 |
| Loo et al., 2010 (23) | Sham: 20 Active: 20 Total: 40 |
tDCS | L DLPFC | 1 mA | 20 min/day, 3 times per week (M/W/F), for 5 sessions (5) | No difference in between active and sham on depression | 79 |
| Loo et al., 2012 (24) | Sham: 31 Active: 33 Total: 64 |
tDCS | L DLPFC | 2 mA | 20 min/day, 5 days per week, for 3 weeks (15) | Active stimulation reduced depressive symptoms | 89 |
| Lyon et al., 2015 (34) | Sham: 81 Active: 82 Total: 163 |
CES | Cortex | 100 μA, 0.5Hz | 1 hour/day, 7 days per week, for 2 weeks (14) | No difference between active and sham on depression | 63 |
| Mischoulon et al., 2015 (35) | Sham: 13 Active: 17 Total: 30 |
CES | DLPFC | 1–4 μA | 20 min/day, 5 days per week, for 3 weeks (15) | No difference between active and sham on depression | 84 |
| McClure et al., 2015 (36) | Sham: 9 Active: 7 Total: 16 |
CES | Cortex | 2mA, 5Hz, 500Hz, 15,000Hz | 20 min/day, 5 days per week, for 2 weeks (10) | Active stimulation reduced depressive symptoms | 67 |
| Palm et al., 2012 (25) | Sham: 11 Active: 11 Total: 22 |
tDCS | L DLPFC | 1–2mA | 20 min/day, 5 days per week, for 4 weeks (20) | No difference between active and sham on depression | 74 |
| Segrave et al., 2014 (5) | Therapy/Active: 9 Therapy/Sham: 9 Sham Therapy/Active: 9 Total: 27 |
tDCS | L DLPFC | 2 mA | 24 min/day for 5 sessions (5) | Active stimulation reduced depressive symptoms | 68 |
| Shiozawa et al., 2015 (37) | Sham: 20 Active: 20 Total: 40 |
TNS | Trigeminal Nerve | 120 hz 250 μs |
30 min/day, for 10 days (10) | Active stimulation reduced depressive symptoms | 74 |
| Vanderhasselt et al., 2015 (29) | Sham: 14 Active: 19 Total: 33 |
tDCS | L DLPFC | 2 mA | 30 min/day for 10 sessions (10) | No difference between active and sham on depression | 53 |
Key: mA, milliamps; tDCS, transcranial direct current stimulation; CES, cranial electrotherapy; TNS, trigeminal nerve stimulation; L, left; R, right; DLPFC, dorsolateral prefrontal cortex; Sert, sertraline.
Some studies included unblinded components; only double-blind outcomes are reported here.
21-item quality checklist was developed (see supplements 1 and 2), based on GRADE scoring guidelines (Kavanagh 2009). The same criteria were applied to all clinical RCTs reviewed. Quality Metric Score is a summary score (0–100%; rounded to the nearest whole number) calculated for each trial, based on the number of quality indicators that were present, with 100% reflecting the highest quality rating. Each published report was independently reviewed and scored by at least two coauthors; group discussion took place to resolve discrepancies and achieve consensus scoring for all indicators on all studies.
Initial studies of tDCS generated mixed results regarding potential efficacy. Fregni et al. (21) performed the first clinical trial of tDCS for MDD (n=10) and found efficacy of active over sham treatment (p<.05). This was followed by a larger study (n=40) by Boggio et al. (22) that also showed superiority of active stimulation. Subsequently, Loo and colleagues (23) found no difference between active and sham tDCS (n=40)(p>.1). However, when they conducted a larger study (24)(n=64) with more treatment sessions, they found a significant advantage of active tDCS (p<.05) but no difference in response rates; one bipolar patient receiving active tDCS became hypomanic. Palm et al. (25)(n=22), and Blumberger et al. (26)(n=24), also found no difference between active and sham tDCS. Bennabi et al. (27)(n=24) tested tDCS+escitalopram (10–20mg) and found no difference between active and sham.
In the largest (n=120) study of tDCS to date, Brunoni et al. (4) gave twelve 30-minute sessions of 2 mA tDCS (10 consecutive workday sessions followed by a single session delivered every other week) and/or a low-dose of sertraline (50mg/d) in a 2×2 factorial design; two of the groups (each n=30) were randomized to groups with active tDCS. This approach enabled comparisons of active versus sham tDCS, placebo pill versus sertraline, and a combination drug + stimulation. They observed greater reduction of depression in the combined sertraline+active tDCS group compared to sertraline monotherapy (p=.002), tDCS monotherapy (p=.03), and both inactive treatments (placebo+sham tDCS; p<.001). Treatment with tDCS monotherapy was superior to placebo+sham tDCS (p=.01) but comparable to sertraline monotherapy (p=.35). When comparing response rates, tDCS monotherapy (43.3%; p<.001) and tDCS+sertraline (63.3%; p=.03) did better than placebo+sham stimulation (16.7%). Remission followed a similar pattern, with worse outcomes for the placebo+sham (13.3%) group compared to tDCS monotherapy (40.0%, p=.02) and to active tDCS+sertraline (46.7%, p=.007). Sertraline monotherapy did not statistically separate from placebo+sham on any outcome measure. Seven episodes of treatment-emergent mania or hypomania were observed, with the majority (n=5; 17%) in the combined (active tDCS+sertraline) group.
Several groups have evaluated the combined effect of tDCS plus psychotherapy for depression, an approach informed by data indicating that tDCS can facilitate neuronal firing in the context of appropriate environmental cues (10). Segrave et al. (5)(n=27) reported improved depressive symptoms when tDCS was combined with cognitive control therapy, although both Brunoni et al. (28)(n=37), and Vanderhasselt et al. (29)(n=33) found no difference between active and sham combined with therapy. Some have identified the timing of stimulation relative to therapy as a possible limitation of these studies, theorizing that “online” stimulation, occurring concurrent with therapy might be superior to “offline” stimulation that precedes the session (30).
The anxiolytic/antidepressant effects of other types of tCS have also been investigated. Over a dozen CES devices received FDA clearance for treatment of “insomnia, depression, or anxiety,” based on technical features that were considered substantially equivalent to older CES devices already on the market before Congress introduced the Medical Device Regulation Act in 1976. While an older literature (31)(32) suggested clinical efficacy of CES, that body of evidence is comprised by trials that would not be considered rigorous by modern standards of clinical trial design. A 1995 meta-analyses of CES therapy raised questions regarding data reporting bias and adequacy of blinding (32). While the use of proprietary waveforms by most CES devices has created an obstacle for independent evaluation of efficacy and potential mechanisms of action, Barclay et al. (33)(n=115) conducted a investigation of CES efficacy using the Alpha-Stim device in patients with a primary anxiety disorder and some (unspecified) degree of comorbid depressive symptoms, reported significantly improved depression (p<.001) and anxiety (p<.001) outcomes. However, subsequent studies by Lyon et al. (34)(n=167), and Mischoulon et al. (35)(n=30) found no advantage of CES over sham on depressive symptoms (all p>.1). One recent pilot study of Bipolar II Depression by McClure et al. (36)(n=16) indicated that two weeks of CES could reduce depressive symptoms (p<.003).
Cranial nerve stimulation is another tCS approach under investigation. Shiozawa et al. (37)(n=40) reported the first RCT evaluating efficacy of externally-applied trigeminal nerve stimulation (eTNS), and reported that active stimulation significantly reduced depressive symptoms (p<.01). Rong et al. (38)(n=160) conducted a pseudo-RCT of transcutaneous VNS (tVNS) for MDD. While active tVNS was associated with greater reduction in depressive symptoms (p<.001), no differences in response or remission were observed at endpoint.
To date, there are four meta-analyses of tDCS for depression. Although earlier reports were negative (14, 38), recent analyses (incorporating larger studies) are positive. Shiozawa et al. (18)(n=259) found a significant advantage of active tDCS over sham (g=0.37; 95% CI 0.04–0.7). Odds Ratios (OR) for response and remission were 1.63 (95% CI 1.26–2.12) and 2.50 (95% CI 1.26–2.49). Most recently, Brunoni et al. (39)(n=289) found similar results for response (OR = 2.44, 95% CI 1.38–4.32) and remission (OR = 2.38, 95% CI 1.22–4.64), and also reported that treatment resistance predicted nonresponse, whereas higher tDCS dose (longer duration and higher current density) predicted response.
Questions remain about potential side effects or synergistic therapeutic effects when tCS is combined with psychotropic medications, since no large studies have investigated the use of tDCS concurrent with adequate doses of antidepressant medication. The currently available data does not support the use of tDCS as a method to accelerate or enhance the short-term effects of psychotherapy. While risk of adverse events appears modest, the incidence of (hypo)manic induction in larger RCTs is noteworthy and deserves greater study.
Taken together, the available RCT evidence generally supports the use of tDCS to relieve symptoms of depression, with other stimulation modalities yielding mixed results. To date there is no defined regulatory pathway for tDCS devices, and none are approved or cleared for treating psychiatric disorders. On the other hand, despite having an FDA indication for depression, CES devices have not consistently demonstrated clinical efficacy.
Randomized Controlled Trials of tCS for Schizophrenia
tCS has been investigated as a treatment approach for schizophrenia (Table 2), mostly utilizing tDCS. Montages typically utilized placement of the anode over the left DLPFC, with cathode over the temporo-parietal junction (TPJ) or over the supraorbital area. Brunelin et al (40)(n=30) conducted the first RCT and observed that active tDCS reduced auditory hallucinations acutely (p<.001) and over 3 months (p<.001), and reduced negative symptoms (p=.01). This was followed by a study by Smith et al. (41)(n=37) that found active stimulation improved cognition (p=.008), but had no effect on positive or negative symptoms (all p >.1), whereas Palm et al. (42) found tDCS reduced negative symptoms (p=.016) and Mondino et al. (43) found tDCS reduced hallucinations (p<.001). Several studies for schizophrenia (Fitzgerald et al. (n=24)(44) and Frohlich et al. (45)(n=26)) and tVNS (Hasan et al. (46)(n=20) found no difference between active and sham stimulation.
Table 2.
Quality of tCS RCTs (n=7) for Schizophrenia
| Study | N per Group | Type | Anatomical Target(s) | Stimulation Strength | Session Duration, Number of Sessions (Total) | Main Findingsa | Quality Metric Score (%)b |
|---|---|---|---|---|---|---|---|
| Brunelin et al., 2012 (40) | Sham: 15 Active: 15 Total: 30 |
tDCS | L DLPFC, L TPJ | 2 mA | 20 min twice a day for 5 days (10) | Active stimulation reduced auditory and verbal hallucinations | 63 |
| Fitzgerald et al., 2014c (44) | Sham: 12 Active: 12 Total: 24 |
tDCS | Bilateral (n=11): L+R (both anodal) to DLPFC with L+R TPJ (both cathodal); Unilateral (n=13): L DLPFC, L TPJ | 2 mA | 20 min/day, 5 days per week, for 3 weeks (15) | No difference between active and sham stimulation on hallucinations or negative symptoms | 37 |
| Frohlich et al., 2016 (45) | Sham: 13 Active: 13 Total: 26 |
tDCS | L DLPFC, L TPJ | 2 mA | 20 min/day for 5 days (5) | No difference between active and sham on auditory hallucinations | 74 |
| Hasan et al., 2015 (46) | Sham: 10 Active: 10 Total: 20 |
eVNS | Vagus Nerve | 25Hz, 250 μsec pulse width, 0.1–10mA | Morning to bedtime, daily, for 12 weeks (84) | No difference between active and sham on schizophrenia symptoms | 84 |
| Mondino et al., 2016c (43) | Sham: 12 Active: 11 Total: 23 |
tDCS | L DLPFC, L TPJ | 2 mA | 20 min, twice a day for 5 days (10) | Active stimulation reduced auditory and verbal hallucinations | 42 |
| Palm et al., 2016 (42) | Sham: 10 Active: 10 Total: 20 |
tDCS | L DLPFC, | 2mA | 10 min/day for 5 days (10) | Active stimulation reduced negative symptoms | 81 |
| Smith et al., 2015 (41) | Sham: 16 Active: 17 Total: 33 |
tDCS | L DLPFC | 2 mA | 20 min/day for 5 days (5) | Active stimulation improved cognition; no effects on psychiatric symptoms or smoking | 84 |
Key: tDCS, transcranial direct current stimulation, L, left; R, right; DLPFC, dorsolateral prefrontal cortex; TPJ, temporoparietal junction; mA, milliamps; eVNS, external vagus nerve stimulation
Some studies included unblinded components; only double-blind outcomes are reported here.
21-item quality checklist was developed (see supplements 1 and 2), based on GRADE scoring guidelines (Kavanagh 2009). The same criteria were applied to all clinical RCTs reviewed. Quality Metric Score is a summary score (0–100%; rounded to the nearest whole number) calculated for each trial, based on the number of quality indicators that were present, with 100% reflecting the highest quality rating. Each published report was independently reviewed and scored by at least two coauthors; group discussion took place to resolve discrepancies and achieve consensus scoring for all indicators on all studies.
This study describes two pilot studies, reported together; the first used unilateral and the second utilized bilateral stimulation, in both cases with goal for inhibition of TPJ and stimulation of DLPFC
This study included participants (8 active, 7 sham) previously described in another clinical trial report by Brunelin et al., 2012
The currently available data does not support use of tCS for schizophrenia. The evidence base comprises a small number of RCTs with conflicting results. More work is clearly needed to develop tCS for treatment of patients with schizophrenia.
Randomized Controlled Trials of tCS for Dementia or Cognitive Deficits
Dementia and cognitive deficits are other therapeutic areas of investigation (Table 3), inspired by the potential for tDCS to enhance attention, learning, and memory in healthy adults (reviewed in (47)). While meta-analyses of single-session tCS (48; 49) indicate benefit in patient samples, most clinical RCTs have been negative (50; 51), although Manenti et al. (52)(n=20) found that tDCS improved cognition in patients with Parkinson’s disease. Based on these results, the available data does not support the use of tDCS for patients with dementia or cognitive deficits.
Table 3.
Quality of tCS RCTs (n=3) for Dementia
| Study | N per Group | Type | Anatomical Target(s) | Stimulation Strength | Session Duration, Number of Sessions (Total) | Dementia Type | Main Findingsa | Quality Metric Score (%)b |
|---|---|---|---|---|---|---|---|---|
| Boggio et al., 2012 (50) | Total: 15e | tDCS | Temporal cortex | 2 mA | 30 min for 5 days (5) | AD | No difference on most measures; active stimulation improved visual recognition | 52 |
| Manenti et al., 2016 (52) | Sham: 10 Active: 10 Total: 20 |
tDCS | DLPFCf | 2 mA | 25 min/day, 5 days per week, for 2 weeks (10) | PD | No difference between active and sham on motor ability or depressive symptoms | 42 |
| Suemoto et al., 2014 (51) | Sham: 20 Active: 20 Total: 40 |
tDCS | L DLPFC | 2 mA | 20 min/day, 3 days per week, for 2 weeks (6) | AD | No difference between active and sham on apathy | 68 |
Key: tDCS, transcranial direct current stimulation; L, left; R, right; DLPFC, dorsolateral prefrontal cortex; mA, milliamps; PD, Parkinson’s disease; AD, alzheimers disease; FTD, frontotemporal dementia
Some studies included unblinded components; only double-blind outcomes are reported here.
21-item quality checklist was developed (see supplements 1 and 2), based on GRADE scoring guidelines (Kavanagh 2009). The same criteria were applied to all clinical RCTs reviewed. Quality Metric Score is a summary score (0–100%; rounded to the nearest whole number) calculated for each trial, based on the number of quality indicators that were present, with 100% reflecting the highest quality rating. Each published report was independently reviewed and scored by at least two coauthors; group discussion took place to resolve discrepancies and achieve consensus scoring for all indicators on all studies.
All participants received active and sham stimulation in a counterbalanced design.
Stimulation was delivered contralaterally to the most affected side
Randomized Controlled Trials of tCS for Treating Substance Use Disorders
A number of studies evaluated tCS for substance use disorders (Table 4). Da Silva et al. (53)(n=13) investigated tDCS for alcohol dependence, and reported significant reductions in depressive symptoms (p<.001) and craving (p=.015), although also reported a statistical trend towards higher relapse rate (p=.053). Klauss et al. (54)(n=15) found active tDCS improved alcohol abstinence (p=.02). Regarding nicotine, two studies, Boggio et al. (55)(n=27), and Fecteau et al. (56)(n=12), found tDCS reduced nicotine craving and cigarette consumption (p<.05). Findings in cocaine use are mixed; Conti et al. (57)(n=13) found no effect of tDCS on cocaine use (p>.1), whereas Batista et al. (58)(n=36) found tDCS reduced cocaine craving (p=.028). There are some proof-of-concept studies of tDCS for other substances, with potentially concerning results. Boggio et al. (59)(n=25) found tDCS increased risk-taking behaviors in chronic cannabis users (p<.001), and Shahbabaie et al. (60)(n=22) found tDCS increased cue-induced methamphetamine craving (p=.012).
Table 4.
Quality of tCS RCTs (n=6) for Substance Use Disorders
| Study | N per Group | Type | Anatomical Target(s) | Stimulation Strength | Session Duration, Number of Sessions (Total) | Substance Type | Main Findingsa | Quality Metric Score (%)b |
|---|---|---|---|---|---|---|---|---|
| Batista et al., 2015 (58) | Sham: 19 Active: 17 Total: 36 |
tDCS | L DLPFC | 2 mA | 20 min/day, every other day, for 5 days (5) | Cocaine | Active stimulation reduced craving | 62 |
| Boggio et al., 2009 (59) | Total: 27g | tDCS | L & R DLPFC | 2 mA | 20 min/day, for 5 days (5) | Smoking | Active stimulation reduced craving | 42 |
| Conti et al., 2014 (57) | Sham: 6 Active: 7 Total: 13 |
tDCS | Frontopolar cortex | 2 mA | 20 min/day, every other day (5) | Cocaine | Active stimulation reduced craving | 58 |
| Da Silva et al., 2013 (53) | Sham: 7 Active: 6 Total: 13 |
tDCS | L DLPFC | 2 mA | 20 min, once a week, for 5 weeks (5) | Alcohol | Active stimulation reduced depressive symptoms and and craving | 58 |
| Fecteau et al., 2014 (56) | Total: 12f | tDCS | R DLPFC | 2 mA | 30 min/day, for 5 days (5) | Smoking | Active stimulation reduced number of cigarettes smoked | 58 |
| Klauss et al., 2014 (54) | Sham: 17 Active: 16 Total: 33 |
tDCS | L & R DLPFC | 2 mA | 13 min, twice a day, for 5 days (10) | Alcohol | Active stimulation reduced relapse | 68 |
Key: tDCS, transcranial direct current stimulation; L, left; R, right; DLPFC, dorsolateral prefrontal cortex; mA, milliamps
Some studies included unblinded components; only double-blind outcomes are reported here.
21-item quality checklist was developed (see supplements 1 and 2), based on GRADE scoring guidelines (Kavanagh 2009). The same criteria were applied to all clinical RCTs reviewed. Quality Metric Score is a summary score (0–100%; rounded to the nearest whole number) calculated for each trial, based on the number of quality indicators that were present, with 100% reflecting the highest quality rating. Each published report was independently reviewed and scored by at least two coauthors; group discussion took place to resolve discrepancies and achieve consensus scoring for all indicators on all studies.
Stimulation was delivered contralaterally to the most affected side
All participants received active and sham stimulation in a crossover design
While the available data appear to provide some support for the use of tDCS for some substance use disorders, there are very few clinical trials, and several suggest potential harms, such as increased relapse (53), greater risk-taking (59; 61), and heightened craving (60).
Proof of Concept Studies of tCS for Treating Other Neuropsychiatric Disorders
Data describing tCS for therapeutic areas beyond those reviewed here are quite limited. For example, one study (62)(n=60) did not find efficacy of a single tDCS session for ADHD, and several case series or open label studies suggested potential efficacy of tCS for working memory in PTSD (63), and symptoms of comorbid PTSD and MDD (64). There are also a growing number of studies for nonpsychiatric conditions that may be of interest to psychiatrists, described elsewhere (14; 65).
SECTION 3: POTENTIAL RISKS OF tCS
The majority of tCS devices used in the RCTs we reviewed are not FDA-cleared for psychiatric disorders, except CES devices that are FDA-cleared for insomnia, depression, and anxiety. Purchase of CES devices requires a written authorization from a licensed healthcare practitioner (which may include acupuncturists, chiropractors, or pharmacists). CES devices should be safe when used according to the manufacturer’s instructions, although CES device instructions may lack detail regarding aspects of use. Regarding tDCS risks, a recent review found no evidence of brain injury when applied using conventional parameters (≤40 min, ≤4 mA, ≤7.2 C) (66). However, this review included only data from published tDCS clinical research trials, and therefore excludes information from unsupervised use outside of research protocols.
The perceived safety of tCS has led to both direct to consumer (DTC) sales and do-it-yourself (DIY) construction kits for tCS systems. DTC devices are commercial systems marketed and sold to consumers without requirement for any involvement by a health professional, whereas DIY devices are made by an individual for private use (i.e., with store bought or homemade components), although where one category ends and the other begins is not clear (67). Because they have electronic components, DTC devices for tCS must conform to certain regulatory standards regarding protections against shock and radiofrequency interference. However, the FDA regulates neither DTC nor DIY devices, as these devices are not intended (at least explicitly) to provide specific medical benefits. Described in popular press as “jumper cables for the mind” and by companies as a way to “overclock your brain” (68), many DTC tCS systems priced in the $100–400 USD range are advertised as capable of promoting general “brain health” benefits. Discussed below are the three major risks associated with unsupervised tCS: device-related injury, cognitive effects, and treatment interference.
Device-Related Risks
The classic risk when stimulating the brain is seizure generation, although the energy used in tCS is orders of magnitude lower than in ECT (e.g., 800mA) or rTMS (66). Therefore, seizures would be very unlikely in the absence of intracranial pathology. Additionally, the interaction between tCS and metal in the head/neck represents a major unknown risk. Most tCS studies excluded participants with head/neck metal, which could divert and adversely focus applied currents. While tCS in patients with head/neck metal may be safe in some cases, it should not routinely be considered outside of specialized research-based settings.
Perhaps the greatest device-related risk is skin burns from excess energy, though these are generally preceded by pain and redness as a warning sign (6). Recent studies, with experienced investigators using devices with adequate safety features, have not observed skin burns (e.g., Brunoni et al. (4)). Self-administration of tCS by untrained individuals may present greater burn risk. A closely related risk is delivering more (or less) current than desired. DTC devices typically do not include instructions for the consumer to calibrate or other otherwise assess the function of the device. Of concern, a growing community of DIY enthusiasts is building and using their own devices for noninvasive brain stimulation. For example, a 2015/2016 internet search by the authors yielded five DIY device designs that could be constructed for $50–100 USD and would likely be capable of delivering 1–2 mA. DIY interest is growing; a user-support websites with 2,700 registered users in 2013 (69) had grown to over 8,700 in 2016. Purported uses range from improving mood/anxiety symptoms, to enhanced exercise endurance, to gaining an edge in online gaming. Accessible plans for DIY devices did include multiple statements about safety precautions in building and using the device. Such disclaimers may protect DIY proponents from liability (69), but the information is likely insufficient for patients. Furthermore, since the FDA does not regulate DTC devices or DIY device construction documents, serious adverse events may be occurring, yet not reported: one DIY tCS website included subjective descriptions of migraines, photophobia, vivid dreams, increased anxiety, and possible mania. Such reports represent important safety information that is otherwise not recorded.
Risk of Adverse Cognitive Effects
Though claims that tCS improves brain function have been made (47)(48; 49), stimulation may also impair cognition (70). It may induce a functional “trade-off”, improving a single cognitive function at the cost of impairing another. For example, one study of healthy individuals found tDCS improved learning new associations, at the cost of performing old ones (71). Another reported tDCS increased mathematics performance but reduced executive function (72). These effects may be greater in psychiatric patients, where the cognitive reserve may be reduced as a consequence of illness. Specific electrode configurations may also be associated with adverse cognitive effects. Several studies described learning and working memory impairments when the tDCS cathode was applied over the parietal lobe or cerebellum (73; 74), and another found reduced cognitive performance when the tDCS anode was placed over the DLPFC (i.e., the configuration used by the vast majority of tDCS studies) (70). Worsened working memory has also been reported after use of a commercial tDCS device (75).
Risk of Interference with Psychiatric Treatment
The ostensibly benign profile of tCS could lead patients with mental illness to substitute stimulation for evidence-based care. In a large-scale survey of the DIY community, depressive symptoms were cited as a common reason for trying tCS. Less than half (44%) of those using tCS for a medical condition were seeing a physician for that same condition (69). As reviewed in Section 2, only a small handful of studies systematically evaluated the effects of stimulation concurrent with psychopharmacology or therapy. Given that tCS effects are likely state-dependent, the field should expect to find significant, unexpected, and potentially harmful interactions between tCS and other interventions. As described above, Brunoni et al. (4) described an elevated rate of conversion from depression to hypomania in participants receiving tDCS and sertraline. As tCS becomes widely available to consumers, more patients with a bipolar diathesis may try it and switch into a (hypo)manic state. Clinicians might erroneously attribute the change in mood state to pharmacology, thereby removing a potential treatment option. Several of the reviewed substance abuse studies showed an increase in cravings or related symptoms (53; 59–61), suggesting that occult tCS could attenuate the efficacy of substance abuse treatment. Therefore, unreported or unsupervised tCS may pose a significant risk to patients by interfering with evidence-based psychiatric treatments.
Supplementary Material
Figure 1B. Model of Anode vs. Cathode Stimulation.
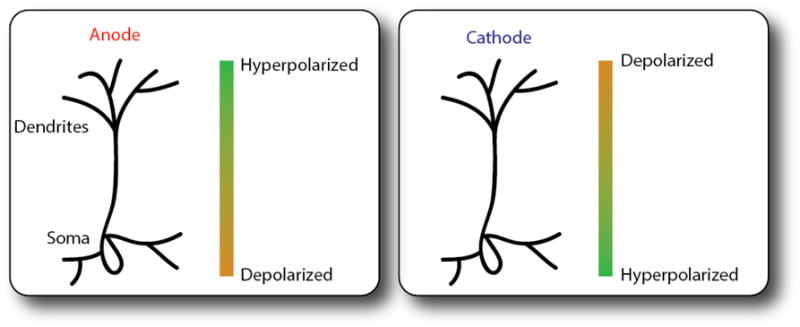
Schematized representation of anode and cathode stimulation on neuron resting potentials. Placement of the anode over a brain region leads a depolarization that increases the likelihood of neuronal firing in the cell body (left). In contrast, placement of the cathode leads to hyperpolarization, which decreases the likelihood of neuronal firing (right).
SUMMARY: EFFICACY AND SAFETY OF tCS IN PSYCHIATRIC DISORDERS.
Our review of tCS RCTs pointed to many cases of inadequate blinding and lack of standardized environment. Only tDCS for MDD has consistently demonstrated positive therapeutic effects, with the caveats that risk of (hypo)mania needs to be studied further, and longer-term outcomes have yet to be evaluated. It is important to note that positive tCS studies require replication, and the precise interactions between stimulation, antidepressant medication and psychotherapy (or other cognitive states surrounding stimulation) are unknown. Data regarding tCS for other psychiatric disorders demonstrate negative or mixed results, with some evidence of harm in individuals with substance use disorders. One potential explanation for these outcomes is the over-application of simplistic neurophysiologic principles. Expectations that a specific tCS electrode montage will be “excitatory” or “inhibitory” to a given brain region or cognitive function may not be appropriate for the more complicated neural pathology that characterizes psychiatric disorders.
The majority of tCS clinical trials in this review utilized tDCS, which, when delivered by experienced research teams to medically healthy patients, is associated with a relatively benign side effect profile. However, in a recently published letter, a group of researchers with extensive experience in noninvasive brain stimulation summarized concerns about unknown risks of tDCS, emphasizing: 1) “Stimulation affects more of the brain than a user may think;” 2) “Stimulation interacts with ongoing brain activity, so what a user does during tDCS changes tDCS effects;” 3) “Enhancement of some cognitive abilities may come at the cost of others;” 4) “Changes in brain activity (intended or not) may last longer than a user may think;” 5) “Small differences in tDCS parameters can have a big effect;” 6) “tDCS effects are highly variable across different people;” and 7) “The risk/benefit ratio is different for treating diseases versus enhancing function” (76).
It is possible that future tCS modalities may demonstrate clinical efficacy (or greater potential for harm) for psychiatric disorders. A search of clinicaltrials.gov found over 450 registered studies using tCS for psychiatric disorders, dwarfing the number of studies in this review. Burgeoning research activity demonstrates a significant interest in the therapeutic potential of tCS and the rapid development of this field. Research into mechanisms of action, findings generated in other types of clinical samples, and a variety of sources of clinical information will continue to shape the evidence base surrounding tCS.
At this point in time, enthusiasm for tCS in clinical practice settings should be mitigated by the fact that there are no tDCS devices with FDA clearance for treatment of psychiatric disorders. Devices cleared for other indications (e.g., iontophoresis) were utilized in some clinical tDCS studies, while other trials used devices that are only available for purchase and use in research protocols. Translating the tDCS literature into guidelines for tCS in clinical practice is thus complex. Further, tCS devices that do have FDA clearance (e.g., CES devices manufactured by Fisher-Wallace, Alpha-Stim) have either not shown efficacy in recent published trials or have only limited support arising from low quality data. While conclusions from this review reflect the perspective of clinicians working and practicing in the USA, other considerations may exist for our international colleagues. If eventually proven safe and effective, with appropriate regulatory controls and guidelines for clinical monitoring, the relative ease of use and abundant access to devices could render tCS a broad-reaching and important advance in mental health care.
Acknowledgments
The authors report the following sources of support for their time working on this project: U.S. Department of Veterans Affairs grant IK2 CX000724 (Dr. Philip); Brain and Behavior Research Foundation grant (Dr. Nelson); Grants from National Institute of Mental Health (NIMH) R01 MH101547, Foundation of Hope, Brain and Behavior Research Foundation, and Human Frontier Science Program (Dr. Frohlich); National Institute on Drug Abuse (NIDA) grant R01 DA038984 and U.S. Department of Veterans Affairs (Dr. Lim); Grants from the Harvard Brain Science Initiative, Brain & Behavior Research Foundation, and the Picower Family Foundation (Dr. Widge); and the Brown Institute for Brain Sciences/Brown Department of Psychiatry and Human Behavior (Dr. Carpenter).
Commercial financial relationships reported by the coauthors include research equipment and clinical trials contracts support from Neuronetics, Cervel Neurotech, and Neosync (Drs. Philip and Carpenter); research funding from Tal Medical (Dr. Frohlich); in-kind device donations from Medtronic (Dr. Widge); and consulting income from Magstim LTD (Dr. Carpenter) and Strata Solar (Dr. Frohlich). Dr. Frohlich is the chief science officer, founder, and majority owner of Pulvinar Neuro, LLC, a company that is involved in the design and manufacture of low intensity stimulation devices. Dr. Nelson was president and co-owner of AgileMedicine, LLC, a company that produced clinical trial and health data management systems, until May 2016. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or National Institutes of Health.
The authors wish to acknowledge Sarah Albright, B.A. (previously employed at the Center of Excellence for Neurorestoration and Neurotechnology, Providence VA Medical Center, Providence RI), for her assistance with manuscript preparation.
References
- 1.Heidland A, Fazeli G, Klassen A, Sebekova K, Hennemann H, Bahner U, Di Iorio B. Neuromuscular electrostimulation techniques: historical aspects and current possibilities in treatment of pain and muscle wasting. Clin Nephrol. 2013;79(Suppl 1):S12–23. [PubMed] [Google Scholar]
- 2.Fink M. Meduna and the origins of convulsive therapy. Am J Psychiatry. 1984;141:1034–1041. doi: 10.1176/ajp.141.9.1034. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin S, Widge A, Shaw K. Neuropsychiatry and neuroscience milestones for general psychiatry trainees. Acad Psychiatry. 2014;38:275–282. doi: 10.1007/s40596-014-0112-0. [DOI] [PubMed] [Google Scholar]
- 4.Brunoni AR, Valiengo L, Baccaro A. The sertraline vs. electrical current therapy for treating depression clinical study: results from a factorial, randomized, controlled trial. JAMA Psychiatry. 2013;70:383–391. doi: 10.1001/2013.jamapsychiatry.32. [DOI] [PubMed] [Google Scholar]
- 5.Segrave RA, Arnold S, Hoy K, Fitzgerald PB. Concurrent cognitive control training augments the antidepressant efficacy of tDCS: a pilot study. Brain Stimul. 2014;7:325–331. doi: 10.1016/j.brs.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Loo CK, Martin DM, Alonzo A, Gandevia S, Mitchell PB, Sachdev P. Avoiding skin burns with transcranial direct current stimulation: preliminary considerations. Int J Neuropsychopharmacol. 2011;14:425–426. doi: 10.1017/S1461145710001197. [DOI] [PubMed] [Google Scholar]
- 7.Tranchina D, Nicholson C. A model for the polarization of neurons by extrinsically applied electric fields. Biophys J. 1986;50:1139–1156. doi: 10.1016/S0006-3495(86)83558-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahman A, Lafon B, Bikson M. Multilevel computational models for predicting the cellular effects of noninvasive brain stimulation. Prog Brain Res. 2015;222:25–40. doi: 10.1016/bs.pbr.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Kronberg G, Bridi M, Abel T, Bikson M, Parra LC. Direct Current Stimulation Modulates LTP and LTD: Activity Dependence and Dendritic Effects. Brain Stimul. doi: 10.1016/j.brs.2016.10.001. Available from: http://www.sciencedirect.com/science/article/pii/S1935861X16302595. [DOI] [PMC free article] [PubMed]
- 10.Nitsche Ma, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(Pt 3):633–639. doi: 10.1111/j.1469-7793.2000.t01-1-00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohn SH, Park C-I, Yoo W-K, Ko M-H, Choi KP, Kim G-M, Lee YT, Kim Y-H. Time-dependent effect of transcranial direct current stimulation on the enhancement of working memory. Neuroreport. 2008;19:43–47. doi: 10.1097/WNR.0b013e3282f2adfd. [DOI] [PubMed] [Google Scholar]
- 12.Clark VP, Coffman BA, Mayer AR, Weisend MP, Lane TDR, Calhoun VD, Raybourn EM, Garcia CM, Wassermann EM. TDCS guided using fMRI significantly accelerates learning to identify concealed objects. Neuroimage. 2012;59:117–128. doi: 10.1016/j.neuroimage.2010.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuo H-I, Paulus W, Batsikadze G, Jamil A, Kuo M-F, Nitsche MA. Chronic Enhancement of Serotonin Facilitates Excitatory Transcranial Direct Current Stimulation-Induced Neuroplasticity. Neuropsychopharmacology. 2016;41:1223–1230. doi: 10.1038/npp.2015.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fregni F, Nitsche MA, Loo CK, Brunoni AR, Marangolo P, Leite J, Carvalho S, Bolognini N, Caumo W, Paik NJ, Simis M, Ueda K, Ekhitari H, Luu P, Tucker DM, Tyler WJ, Brunelin J, Datta A, Juan CH, Venkatasubramanian G, Boggio PS, Bikson M. Regulatory Considerations for the Clinical and Research Use of Transcranial Direct Current Stimulation (tDCS): review and recommendations from an expert panel. Clin Res Regul Aff. 2015;32:22–35. doi: 10.3109/10601333.2015.980944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuo M-F, Paulus W, Nitsche MA. Therapeutic effects of non-invasive brain stimulation with direct currents (tDCS) in neuropsychiatric diseases. Neuroimage. 2014;85(Pt 3):948–960. doi: 10.1016/j.neuroimage.2013.05.117. [DOI] [PubMed] [Google Scholar]
- 16.Tortella G, Casati R, Aparicio LVM, Mantovani A, Senço N, D’Urso G, Brunelin J, Guarienti F, Selingardi PML, Muszkat D. Transcranial direct current stimulation in psychiatric disorders. World J Psychiatry. 2015;5:88–102. doi: 10.5498/wjp.v5.i1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berlim MT, Van den Eynde F, Daskalakis ZJ. Clinical utility of transcranial direct current stimulation (tDCS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. J Psychiatr Res. 2013;47:1–7. doi: 10.1016/j.jpsychires.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 18.Shiozawa P, Fregni F, Benseñor IM, Lotufo PA, Berlim MT, Daskalakis JZ, Cordeiro Q, Brunoni AR. Transcranial direct current stimulation for major depression: an updated systematic review and meta-analysis. Int J Neuropsychopharmacol. 2014;17:1443–1452. doi: 10.1017/S1461145714000418. [DOI] [PubMed] [Google Scholar]
- 19.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63:484. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- 20.Kavanagh BP. The GRADE system for rating clinical guidelines. PLoS Med. 2009;6:e1000094. doi: 10.1371/journal.pmed.1000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fregni F, Boggio PS, Nitsche MA, Marcolin MA, Rigonatti SP, Pascual-Leone A. Treatment of major depression with transcranial direct current stimulation. Bipolar Disord. 2006;8:203–204. doi: 10.1111/j.1399-5618.2006.00291.x. [DOI] [PubMed] [Google Scholar]
- 22.Boggio PS, Rigonatti SP, Ribeiro RB, Myczkowski ML, Nitsche MA, Pascual-Leone A, Fregni F. A randomized, double-blind clinical trial on the efficacy of cortical direct current stimulation for the treatment of major depression. Int J Neuropsychopharmacol. 2008;11:249–254. doi: 10.1017/S1461145707007833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loo CK, Sachdev P, Martin D, Pigot M, Alonzo A, Malhi GS, Lagopoulos J, Mitchell P. A double-blind, sham-controlled trial of transcranial direct current stimulation for the treatment of depression. Int J Neuropsychopharmacol. 2010;13:61–69. doi: 10.1017/S1461145709990411. [DOI] [PubMed] [Google Scholar]
- 24.Loo CK, Alonzo A, Martin D, Mitchell PB, Galvez V, Sachdev P. Transcranial direct current stimulation for depression: 3-week, randomised, sham-controlled trial. Br J Psychiatry. 2012;200:52–59. doi: 10.1192/bjp.bp.111.097634. [DOI] [PubMed] [Google Scholar]
- 25.Palm U, Schiller C, Fintescu Z, Obermeier M, Keeser D, Reisinger E, Pogarell O, Nitsche MA, Möller H-J, Padberg F. Transcranial direct current stimulation in treatment resistant depression: a randomized double-blind, placebo-controlled study. Brain Stimul. 2012;5:242–251. doi: 10.1016/j.brs.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 26.Blumberger DM, Tran LC, Fitzgerald PB, Hoy KE, Daskalakis ZJ. A randomized double-blind sham-controlled study of transcranial direct current stimulation for treatment-resistant major depression. Front Psychiatry. 2012;3:74. doi: 10.3389/fpsyt.2012.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bennabi D, Nicolier M, Monnin J, Tio G, Pazart L, Vandel P, Haffen E. Pilot study of feasibility of the effect of treatment with tDCS in patients suffering from treatment-resistant depression treated with escitalopram. Clin Neurophysiol. 2015;126:1185–1189. doi: 10.1016/j.clinph.2014.09.026. [DOI] [PubMed] [Google Scholar]
- 28.Brunoni AR, Boggio PS, De Raedt R, Benseñor IM, Lotufo PA, Namur V, Valiengo LCL, Vanderhasselt MA. Cognitive control therapy and transcranial direct current stimulation for depression: a randomized, double-blinded, controlled trial. J Affect Disord. 2014;162:43–49. doi: 10.1016/j.jad.2014.03.026. [DOI] [PubMed] [Google Scholar]
- 29.Vanderhasselt M-A, De Raedt R, Namur V, Lotufo PA, Bensenor IM, Boggio PS, Brunoni AR. Transcranial electric stimulation and neurocognitive training in clinically depressed patients: a pilot study of the effects on rumination. Prog Neuropsychopharmacol Biol Psychiatry. 2015;57:93–99. doi: 10.1016/j.pnpbp.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 30.Martin DM, Liu R, Alonzo A, Green M, Loo CK. Use of transcranial direct current stimulation (tDCS) to enhance cognitive training: effect of timing of stimulation. Exp Brain Res. 2014;232:3345–3351. doi: 10.1007/s00221-014-4022-x. [DOI] [PubMed] [Google Scholar]
- 31.de Felice EA. CRANIAL ELECTROTHERAPY STIMULATION (CES) IN THE TREATMENT OF ANXIETY AND OTHER STRESS-RELATED DISORDERS: A REVIEW OF CONTROLLED CLINICAL TRIALS. Stress Med. 1997;13:31–42. [Google Scholar]
- 32.Klawansky S, Yeung A, Berkey C, Shah N, Phan H, Chalmers TC. Meta-analysis of randomized controlled trials of cranial electrostimulation. Efficacy in treating selected psychological and physiological conditions. J Nerv Ment Dis. 1995;183:478–484. doi: 10.1097/00005053-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Barclay TH, Barclay RD. A clinical trial of cranial electrotherapy stimulation for anxiety and comorbid depression. J Affect Disord. 2014;164:171–177. doi: 10.1016/j.jad.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 34.Lyon D, Kelly D, Walter J, Bear H, Thacker L, Elswick RK. Randomized sham controlled trial of cranial microcurrent stimulation for symptoms of depression, anxiety, pain, fatigue and sleep disturbances in women receiving chemotherapy for early-stage breast cancer. Springerplus. 2015;4:369. doi: 10.1186/s40064-015-1151-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mischoulon D, De Jong MF, Vitolo OV, Cusin C, Dording CM, Yeung AS, Durham K, Parkin SR, Fava M, Dougherty DD. Efficacy and safety of a form of cranial electrical stimulation (CES) as an add-on intervention for treatment-resistant major depressive disorder: A three week double blind pilot study. J Psychiatr Res. 2015;70:98–105. doi: 10.1016/j.jpsychires.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 36.McClure D, Greenman SC, Koppolu SS, Varvara M, Yaseen ZS, Galynker II. A Pilot Study of Safety and Efficacy of Cranial Electrotherapy Stimulation in Treatment of Bipolar II Depression. J Nerv Ment Dis. 2015;203:827–835. doi: 10.1097/NMD.0000000000000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shiozawa P, da Silva ME, Netto GTM, Taiar I, Cordeiro Q. Effect of a 10-day trigeminal nerve stimulation (TNS) protocol for treating major depressive disorder: a phase II, sham-controlled, randomized clinical trial. Epilepsy Behav. 2015;44:23–26. doi: 10.1016/j.yebeh.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 38.Rong P, Liu J, Wang L, Liu R, Fang J, Zhao J, Zhao Y, Wang H, Vangel M, Sun S, Ben H, Park J, Li S, Meng H, Zhu B, Kong J. Effect of transcutaneous auricular vagus nerve stimulation on major depressive disorder: A nonrandomized controlled pilot study. J Affect Disord. 2016;195:172–179. doi: 10.1016/j.jad.2016.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brunoni AR, Moffa AH, Fregni F, Palm U, Padberg F, Blumberger DM, Daskalakis ZJ, Bennabi D, Haffen E, Alonzo A, Loo CK. Transcranial direct current stimulation for acute major depressive episodes: meta-analysis of individual patient data. Br J Psychiatry. 2016;208:522–531. doi: 10.1192/bjp.bp.115.164715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brunelin J, Mondino M, Gassab L, Haesebaert F, Gaha L, Suaud-Chagny M-F, Saoud M, Mechri A, Poulet E. Examining transcranial direct-current stimulation (tDCS) as a treatment for hallucinations in schizophrenia. Am J Psychiatry. 2012;169:719–724. doi: 10.1176/appi.ajp.2012.11071091. [DOI] [PubMed] [Google Scholar]
- 41.Smith RC, Boules S, Mattiuz S, Youssef M, Tobe RH, Sershen H, Lajtha A, Nolan K, Amiaz R, Davis JM. Effects of transcranial direct current stimulation (tDCS) on cognition, symptoms, and smoking in schizophrenia: A randomized controlled study. Schizophr Res. 2015;168:260–266. doi: 10.1016/j.schres.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 42.Palm U, Keeser D, Hasan A, Kupka MJ, Blautzik J, Sarubin N, Kaymakanova F, Unger I, Falkai P, Meindl T, Ertl-Wagner B, Padberg F. Prefrontal Transcranial Direct Current Stimulation for Treatment of Schizophrenia With Predominant Negative Symptoms: A Double-Blind, Sham-Controlled Proof-of-Concept Study. Schizophr Bull. 2016;42(5):1253–61. doi: 10.1093/schbul/sbw041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mondino M, Jardri R, Suaud-Chagny M-F, Saoud M, Poulet E, Brunelin J. Effects of Fronto-Temporal Transcranial Direct Current Stimulation on Auditory Verbal Hallucinations and Resting-State Functional Connectivity of the Left Temporo-Parietal Junction in Patients With Schizophrenia. Schizophr Bull. 2016;42:318–326. doi: 10.1093/schbul/sbv114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fitzgerald PB, McQueen S, Daskalakis ZJ, Hoy KE. A negative pilot study of daily bimodal transcranial direct current stimulation in schizophrenia. Brain Stimul. 2014;7:813–816. doi: 10.1016/j.brs.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 45.Fröhlich F, Burrello TN, Mellin JM, Cordle AL, Lustenberger CM, Gilmore JH, Jarskog LF. Exploratory study of once-daily transcranial direct current stimulation (tDCS) as a treatment for auditory hallucinations in schizophrenia. Eur Psychiatry. 2016;33:54–60. doi: 10.1016/j.eurpsy.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 46.Hasan A, Wolff-Menzler C, Pfeiffer S, Falkai P, Weidinger E, Jobst A, Hoell I, Malchow B, Yeganeh-Doost P, Strube W, Quast S, Müller N, Wobrock T. Transcutaneous noninvasive vagus nerve stimulation (tVNS) in the treatment of schizophrenia: a bicentric randomized controlled pilot study. Eur Arch Psychiatry Clin Neurosci. 2015;265:589–600. doi: 10.1007/s00406-015-0618-9. [DOI] [PubMed] [Google Scholar]
- 47.Coffman BA, Clark VP, Parasuraman R. Battery powered thought: enhancement of attention, learning, and memory in healthy adults using transcranial direct current stimulation. Neuroimage. 2014;85(Pt 3):895–908. doi: 10.1016/j.neuroimage.2013.07.083. [DOI] [PubMed] [Google Scholar]
- 48.Dedoncker J, Brunoni AR, Baeken C, Vanderhasselt M-A. A Systematic Review and Meta-Analysis of the Effects of Transcranial Direct Current Stimulation (tDCS) Over the Dorsolateral Prefrontal Cortex in Healthy and Neuropsychiatric Samples: Influence of Stimulation Parameters. Brain Stimul. 2016;9:501–517. doi: 10.1016/j.brs.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 49.Hill AT, Fitzgerald PB, Hoy KE. Effects of Anodal Transcranial Direct Current Stimulation on Working Memory: A Systematic Review and Meta-Analysis of Findings From Healthy and Neuropsychiatric Populations. Brain Stimul. 2016;9:197–208. doi: 10.1016/j.brs.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 50.Boggio PS, Ferrucci R, Mameli F, Martins D, Martins O, Vergari M, Tadini L, Scarpini E, Fregni F, Priori A. Prolonged visual memory enhancement after direct current stimulation in Alzheimer’s disease. Brain Stimul. 2012;5:223–230. doi: 10.1016/j.brs.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 51.Suemoto CK, Apolinario D, Nakamura-Palacios EM, Lopes L, Leite REP, Sales MC, Nitrini R, Brucki SM, Morillo LS, Magaldi RM, Fregni F. Effects of a non-focal plasticity protocol on apathy in moderate Alzheimer’s disease: a randomized, double-blind, sham-controlled trial. Brain Stimul. 2014;7:308–313. doi: 10.1016/j.brs.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 52.Manenti R, Brambilla M, Benussi A, Rosini S, Cobelli C, Ferrari C, Petesi M, Orizio I, Padovani A, Borroni B, Cotelli M. Mild cognitive impairment in Parkinson’s disease is improved by transcranial direct current stimulation combined with physical therapy. Mov Disord. 2016 May;31(5):715–24. doi: 10.1002/mds.26561. [DOI] [PubMed] [Google Scholar]
- 53.da Silva MC, Conti CL, Klauss J, Alves LG, do Nascimento Cavalcante HM, Fregni F, Nitsche MA, Nakamura-Palacios EM. Behavioral effects of transcranial direct current stimulation (tDCS) induced dorsolateral prefrontal cortex plasticity in alcohol dependence. J Physiol Paris. 2013;107:493–502. doi: 10.1016/j.jphysparis.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 54.Klauss J, Penido Pinheiro LC, Silva Merlo BL, de Almeida Correia Santos G, Fregni F, Nitsche MA, Miyuki Nakamura-Palacios E. A randomized controlled trial of targeted prefrontal cortex modulation with tDCS in patients with alcohol dependence. Int J Neuropsychopharmacol. 2014;17:1793–1803. doi: 10.1017/S1461145714000984. [DOI] [PubMed] [Google Scholar]
- 55.Boggio PS, Liguori P, Sultani N, Rezende L, Fecteau S, Fregni F. Cumulative priming effects of cortical stimulation on smoking cue-induced craving. Neurosci Lett. 2009;463:82–86. doi: 10.1016/j.neulet.2009.07.041. [DOI] [PubMed] [Google Scholar]
- 56.Fecteau S, Agosta S, Hone-Blanchet A, Fregni F, Boggio P, Ciraulo D, Pascual-Leone A. Modulation of smoking and decision-making behaviors with transcranial direct current stimulation in tobacco smokers: a preliminary study. Drug Alcohol Depend. 2014;140:78–84. doi: 10.1016/j.drugalcdep.2014.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Conti CL, Nakamura-Palacios EM. Bilateral Transcranial Direct Current Stimulation Over Dorsolateral Prefrontal Cortex Changes the Drug-cued Reactivity in the Anterior Cingulate Cortex of Crack-cocaine Addicts. Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation. 2014;7:130–132. doi: 10.1016/j.brs.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 58.Batista EK, Klauss J, Fregni F, Nitsche MA, Nakamura-Palacios EM. A Randomized Placebo-Controlled Trial of Targeted Prefrontal Cortex Modulation with Bilateral tDCS in Patients with Crack-Cocaine Dependence. Int J Neuropsychopharmacol. 2015;18(12) doi: 10.1093/ijnp/pyv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boggio PS, Zaghi S, Villani AB, Fecteau S, Pascual-Leone A, Fregni F. Modulation of risk-taking in marijuana users by transcranial direct current stimulation (tDCS) of the dorsolateral prefrontal cortex (DLPFC) Drug Alcohol Depend. 2010;112:220–225. doi: 10.1016/j.drugalcdep.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 60.Shahbabaie A, Golesorkhi M, Zamanian B, Ebrahimpoor M, Keshvari F, Nejati V, Fregni F, Ekhtiari H. State dependent effect of transcranial direct current stimulation (tDCS) on methamphetamine craving. Int J Neuropsychopharmacol. 2014;17:1591–1598. doi: 10.1017/S1461145714000686. [DOI] [PubMed] [Google Scholar]
- 61.Gorini A, Lucchiari C, Russell-Edu W, Pravettoni G. Modulation of risky choices in recently abstinent dependent cocaine users: a transcranial direct-current stimulation study. Front Hum Neurosci. 2014;8:661. doi: 10.3389/fnhum.2014.00661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cosmo C, Baptista AF, de Araújo AN, do Rosário RS, Miranda JGV, Montoya P, de Sena EP. A Randomized, Double-Blind, Sham-Controlled Trial of Transcranial Direct Current Stimulation in Attention-Deficit/Hyperactivity Disorder. PLoS One. 2015;10:e0135371. doi: 10.1371/journal.pone.0135371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saunders N, Downham R, Turman B, Kropotov J, Clark R, Yumash R, Szatmary A. Working memory training with tDCS improves behavioral and neurophysiological symptoms in pilot group with post-traumatic stress disorder (PTSD) and with poor working memory. Neurocase. 2015;21:271–278. doi: 10.1080/13554794.2014.890727. [DOI] [PubMed] [Google Scholar]
- 64.Cook IA, Abrams M, Leuchter AF. Trigeminal Nerve Stimulation for Comorbid Posttraumatic Stress Disorder and Major Depressive Disorder. Neuromodulation. 2016;19(3):299–305. doi: 10.1111/ner.12399. [DOI] [PubMed] [Google Scholar]
- 65.O’Connell NE, Wand BM, Marston L, Spencer S, Desouza LH. Non-invasive brain stimulation techniques for chronic pain. Cochrane Database Syst Rev. 2014:CD008208. doi: 10.1002/14651858.CD008208.pub3. [DOI] [PubMed] [Google Scholar]
- 66.Bikson M, Grossman P, Thomas C, Zannou AL, Jiang J, Adnan T, Mourdoukoutas AP, Kronberg G, Truong D, Boggio P, Brunoni AR, Charvet L, Fregni F, Fritsch B, Gillick B, Hamilton RH, Hampstead BM, Jankord R, Kirton A, Knotkova H, Liebetanz D, Liu A, Loo C, Nitsche MA, Reis J, Richardson JD, Rotenberg A, Turkeltaub PE, Woods AJ. Safety of Transcranial Direct Current Stimulation: Evidence Based Update 2016. Brain Stimul. 2016;9(5):641–61. doi: 10.1016/j.brs.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wexler A. A pragmatic analysis of the regulation of consumer transcranial direct current stimulation (TDCS) devices in the United States. J Law Biosci. 2015;2:669–696. doi: 10.1093/jlb/lsv039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hurley D. Jumper Cables for the Mind. The New York Times; 2013. [cited 2016 Aug 6] Available from: http://www.nytimes.com/2013/11/03/magazine/jumper-cables-for-the-mind.html?pagewanted=all. [Google Scholar]
- 69.Jwa A. Early adopters of the magical thinking cap: a study on do-it-yourself (DIY) transcranial direct current stimulation (tDCS) user community. Int J Biosci Law. 2015;2:292–335. doi: 10.1093/jlb/lsv017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sellers KK, Mellin JM, Lustenberger CM, Boyle MR, Lee WH, Peterchev AV, Fröhlich F. Transcranial direct current stimulation (tDCS) of frontal cortex decreases performance on the WAIS-IV intelligence test. Behav Brain Res. 2015;290:32–44. doi: 10.1016/j.bbr.2015.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Iuculano T, Cohen Kadosh R. The mental cost of cognitive enhancement. J Neurosci. 2013;33:4482–4486. doi: 10.1523/JNEUROSCI.4927-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sarkar A, Dowker A, Cohen Kadosh R. Cognitive enhancement or cognitive cost: trait-specific outcomes of brain stimulation in the case of mathematics anxiety. J Neurosci. 2014;34:16605–16610. doi: 10.1523/JNEUROSCI.3129-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Berryhill ME, Wencil EB, Branch Coslett H, Olson IR. A selective working memory impairment after transcranial direct current stimulation to the right parietal lobe. Neurosci Lett. 2010;479:312–316. doi: 10.1016/j.neulet.2010.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ferrucci R, Marceglia S, Vergari M, Cogiamanian F, Mrakic-Sposta S, Mameli F, Zago S, Barbieri S, Priori A. Cerebellar transcranial direct current stimulation impairs the practice-dependent proficiency increase in working memory. J Cogn Neurosci. 2008;20:1687–1697. doi: 10.1162/jocn.2008.20112. [DOI] [PubMed] [Google Scholar]
- 75.Steenbergen L, Sellaro R, Hommel B, Lindenberger U, Kühn S, Colzato LS. “Unfocus” on foc.us: commercial tDCS headset impairs working memory. Exp Brain Res. 2016;234:637–643. doi: 10.1007/s00221-015-4391-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wurzman R, Hamilton RH, Pascual-Leone A, Fox MD. An open letter concerning do-it-yourself users of transcranial direct current stimulation. Ann Neurol. 2016;80:1–4. doi: 10.1002/ana.24689. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


