Abstract
Introduction
The Tobacco Control Act requires public disclosure of information about toxic constituents in cigarette smoke. To inform these efforts, we studied public understanding of cigarette smoke constituents.
Methods
We conducted phone surveys with national probability samples of adolescents (n=1125) and adults (n=5014) and an internet survey with a convenience sample of adults (n=4137), all in the USA. We assessed understanding of cigarette smoke constituents in general and of 24 specific constituents.
Results
Respondents commonly and incorrectly believed that harmful chemicals in cigarette smoke mostly originate in additives introduced by cigarette manufacturers (43–72%). Almost all participants had heard that nicotine is in cigarette smoke, and many had also heard about carbon monoxide, ammonia, arsenic and formaldehyde. Less than one-quarter had heard of most other listed constituents being in cigarette smoke. Constituents most likely to discourage respondents from wanting to smoke were ammonia, arsenic, formaldehyde, hydrogen cyanide, lead and uranium. Respondents more often reported being discouraged by constituents that they had heard are in cigarette smoke (all p<0.05). Constituents with names that started with a number or ended in ‘ene’ or ‘ine’ were less likely to discourage people from wanting to smoke (all p<0.05).
Discussion
Many people were unaware that burning the cigarette is the primary source of toxic constituents in cigarette smoke. Constituents that may most discourage cigarette smoking have familiar names, like arsenic and formaldehyde and do not start with a number or end in ene/ine. Our findings may help campaign designers develop constituent messages that discourage smoking.
INTRODUCTION
Smoking cigarettes is one of the leading causes of preventable deaths in the USA and globally.1,2 Inhalation of smoke directly from cigarettes and secondhand smoke exposes people to scores of toxic constituents (chemicals), many of which have been directly implicated in the cardiovascular, respiratory and carcinogenic health effects of smoking.3–5 Tobacco products and cigarette smoke have at least 93 harmful and potentially harmful constituents.5 In the USA, the Family Smoking Prevention and Tobacco Control Act requires tobacco companies to provide information about cigarette smoke constituents by brand and subbrand to the Food and Drug Administration (FDA).6,7 The law also requires FDA to disclose this information to the public in a way that is understandable and not misleading to a layperson.6
Research exploring how to most effectively communicate about tobacco and tobacco product constituents is at an early stage. Our recent review of the literature found low awareness and knowledge about cigarette smoke constituents other than nicotine and tar.8–14 Additionally, our review also found that people are interested in learning more about these constituents.8,15,16 However, the literature has large gaps. While studies have examined awareness of a handful of constituents, we know little about the public’s understanding of many other harmful constituents.15 We also know little about how people think about constituents, including their origins or how cigarette filters affect exposure to constituents.9,17,18
The goal of our paper is to identify ways to improve communication about cigarette smoke constituents in order to improve tobacco prevention and control efforts. In our prior qualitative research, familiar-sounding constituents appeared to elicit concern, while unfamiliar constituent names led people to search for meaning by using any available clues, including making associations to other words that sound or look similar.19,20 We hypothesised that constituent names that are more familiar to people or have less technical sounding names (ie, no numerical prefix, shorter) would elicit more discouragement from wanting to smoke. Since we noticed that many constituent names have similar endings (eg, ine/ene as in nicotine or ide/yde as in formaldehyde), we sought to examine whether certain constituent name endings elicited more discouragement. Finally, smokers are well known to express less concern about the harms of smoking. Thus, we hypothesised constituents would elicit less discouragement among smokers and among groups with higher smoking prevalence, such as men, individuals with lower levels of education and gay, lesbian and bisexual (GLB) respondents.
METHODS
Participants
Adult phone survey sample
The Carolina Survey Research Laboratory (CSRL) at the University of North Carolina recruited a probability sample of 5014 adults living in the USA. From September 2014 to May 2015, CSRL recruited participants through random-digit-dial landline and cell phone frames, resulting in about 98% coverage of the US population. Geographic and household-based oversampling in areas with higher rates of poverty and smoking, as well as oversampling respondents with certain characteristics at the household level, resulted in a sample that had higher rates of smoking, poverty and young adults than the US population. To be eligible for study participation, adults had to be 18 years or older and speak English or Spanish. Elsewhere, we provide additional details on sampling design, survey methods and sample characteristics.21 The response rate among adults was 42%, calculated using American Association for Public Opinion Research formula 4.22
Adolescent phone survey sample
From November 2014 to June 2015, CSRL recruited a separate probability sample of 1125 adolescents living in the USA, using random-digit-dial and list-assisted sampling frames. As with the adult sample, CSRL oversampled counties with higher prevalence of smokers and poverty. To be eligible for study participation, adolescents had to be ages 13–17 and speak English or Spanish. Interviewers obtained verbal consent from adolescents’ parents or guardians and verbal assent from the adolescents. The response rate among adolescents was 66%, calculated using American Association for Public Opinion Research formula 4.22
Adult internet survey sample
Through Amazon Mechanical Turk, an online recruitment tool, our staff recruited a national convenience sample of 4137 adults (ages 18 or older who spoke English or Spanish) living in the USA, in December 2014. The online advertisement for the survey encouraged current smokers to participate.
The University of North Carolina’s institutional review board approved all three studies.
Measures
Phone and internet surveys used the same question order, wording and response scales, with small adjustments as needed for the internet survey. As part of an iterative measures development process intended to verify that participants assigned the meaning to surveys items that we intended, we conducted cognitive interviews and a survey pilot among diverse samples of adolescents and adults, including adults with low and high education.
Constituents in general
The survey first assessed perceived source of cigarette smoke constituents: ‘Where do you think most of the harmful chemicals in cigarettes and cigarette smoke come from?’ with response options ‘tobacco before it is made into cigarettes’, ‘tobacco additives’ or ‘burning the cigarettes’. The survey next assessed the perceived impact of cigarette filters using the question, ‘Do you think the cigarette filter traps…’ with response options ‘all of the harmful chemicals in cigarette smoke’ (coded as 1), ‘a lot of them’ (2), ‘some of them’ (3) or ‘none of them’ (4).
Specific constituents
We randomised participants to 1 of 6 survey panels, each of which had questions about four different cigarette smoke constituents (see online supplementary table S1). The 24 selected constituents included the 18 on FDA’s abbreviated list, 5 from the FDA’s complete list of 93 constituents and ‘nitrosamine’.5,7 We added ‘nitrosamine’ as it is a more accessible term to refer to N-nitrosonornicotine (NNN) and nicotine-derived nitrosamine ketone (NNK), two of the most harmful constituents in cigarette smoke.23 To examine the effect of using an acronym for the nitrosamines, the surveys used ‘NNK’ when referring to nicotine-derived nitrosamine ketone.
The surveys assessed awareness that each of the four constituents from the assigned panel are in cigarette smoke: ‘Before today, had you ever heard that [constituent] is in cigarette smoke?’. We coded responses of yes as 1 and other responses as 0. The survey next assessed perceived harmfulness for each constituent the respondent had heard is in cigarette smoke with the measure, ‘As far as you know, how harmful is [constituent] in cigarette smoke?’. The four-point response scale ranged from ‘not at all’ (coded as 1) to ‘extremely harmful’ (4). Finally, the survey assessed, ‘How much does [constituent] being in cigarette smoke discourage you from wanting to smoke?’. The four-point response scale ranged from ‘not at all’ (coded as 1) to ‘a lot’ (4).24 We chose discouragement from wanting to smoke because smokers could interpret this as quitting smoking and non-smokers as not starting to smoke. We coded constituent names for three characteristics: beginning, ending and length. Beginnings were either a number or not. Endings were ‘ene’/‘ine’, ‘ide’/‘yde’ and other. Length was the number of characters in the constituent name.
Demographics
The survey assessed participant characteristics, including age, sex, sexual orientation (or sexual interest, among adolescents), race, Hispanic ethnicity, education (or education of mother, among adolescents), numeracy and smoking status.25 Numeracy was assessed with the item, ‘In general, which of these numbers shows the biggest risk of getting disease?’.26 The three response options were ‘one in 10’, ‘one in 100’ and ‘one in 1000’, with only the first response coded as correct (ie, high numeracy). We defined being a current smoker as smoking some days or every day and having smoked 100 or more cigarettes in one’s lifetime among adults, and among adolescents as having smoked during at least 1 of the past 30 days.27,28
Data analysis
We used χ2 tests to compare smokers’ and non-smokers’ beliefs about where constituents originate and t-tests to compare their beliefs about the impact of cigarette filters. We report percentages or means for awareness, perceived harm and discouragement for each of the 24 constituents. For analyses of data from the adult and adolescent phone surveys, we used sample design and sample weights to account for study design and generate nationally representative estimates (percentages and means), and we report unweighted frequencies.
We examined correlates of discouragement from wanting to smoke after hearing that a particular constituent is present in cigarette smoke. We dichotomised the outcome of discouragement from wanting to smoke, so that we could compare responses of ‘a lot’ (coded as 1) to other responses (0), in order to address skewing. One set of predictors were the participant characteristics shown in table 1, with age mean-centred and scaled in decades to make the estimate more interpretable. Another set of predictors were characteristics of constituents: awareness that the constituent is in cigarette smoke; and constituent name beginning (did or did not start with a number), ending (‘ene’/‘ine’, ‘ide’/‘yde’, other) and length (number of characters). The multilevel analyses used the SAS PROC GLIMMIX procedure with quasi-likelihood estimation, a log link function specified with a binary distribution, a random intercept and random effects, where appropriate; used the Newton-Raphson algorithm for the optimisation technique; controlled for constituent panel; and did not use survey weights. Models treated constituent characteristics as random effects and then, if not statistically significant, as fixed effects. We conducted sensitivity analyses by repeating the analyses without data for nicotine to see whether it accounted for the study findings for constituent name ending. We analysed data separately for the three surveys. We conducted analyses in SAS V.9.3 (SAS Institute, 2011) and used two-tailed statistical tests with a critical α of 0.05.
Table 1.
Participant characteristics
| Adolescents in phone survey (n=1125) | Adults in phone survey (n=5014) | Adults in internet survey (n=4137) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | Weighted % | n | Weighted % | n | % | |
| Age | ||||||
| 13–17 | 1124 | 100 | 0 | 0 | 0 | 0 |
| 18–25 | 0 | 0 | 809 | 15 | 1010 | 24 |
| 26–64 | 0 | 0 | 3397 | 68 | 3077 | 75 |
| 65+ | 0 | 0 | 789 | 17 | 39 | 1 |
| Sex | ||||||
| Female | 564 | 49 | 2640 | 51 | 2093 | 51 |
| Male | 561 | 51 | 2372 | 49 | 2042 | 49 |
| Race | ||||||
| African-American | 119 | 13 | 978 | 18 | 313 | 8 |
| American Indian | 18 | 2 | 135 | 2 | 39 | 1 |
| Asian | 25 | 3 | 125 | 3 | 218 | 5 |
| White | 901 | 73 | 3473 | 67 | 3433 | 83 |
| Other | 61 | 8 | 281 | 9 | 131 | 3 |
| Hispanic | ||||||
| No | 1040 | 90 | 4568 | 86 | 3787 | 92 |
| Yes | 85 | 10 | 432 | 14 | 340 | 8 |
| Gay, lesbian or bisexual | ||||||
| No | 1041 | 96 | 4730 | 97 | 3656 | 88 |
| Yes | 42 | 4 | 192 | 3 | 478 | 12 |
| Attended college | ||||||
| No | 218 | 21 | 1756 | 43 | 559 | 14 |
| Yes | 731 | 79 | 3241 | 57 | 3577 | 86 |
| Numeracy | ||||||
| Low | 307 | 27 | 1599 | 32 | 344 | 8 |
| High | 818 | 73 | 3401 | 68 | 3791 | 92 |
| Smoking status | ||||||
| Non-smoker | 1083 | 97 | 3856 | 82 | 2687 | 65 |
| Smoker | 41 | 3 | 1151 | 18 | 1441 | 35 |
| Constituent panel | ||||||
| 1 | 188 | 16 | 790 | 16 | 663 | 16 |
| 2 | 192 | 16 | 849 | 17 | 718 | 17 |
| 3 | 171 | 16 | 837 | 17 | 692 | 17 |
| 4 | 182 | 17 | 779 | 15 | 685 | 17 |
| 5 | 191 | 17 | 897 | 17 | 703 | 17 |
| 6 | 201 | 18 | 862 | 17 | 676 | 16 |
Percentages for phone surveys are weighted. For adolescents, attended college is based on mother’s highest level of education. For adults, smoking status is defined as having smoked at least 100 lifetime cigarettes, and currently smoke every day or some days; for adolescents, it is defined as having smoked during at least 1 of the past 30 days. GLB for adults was defined as sexual orientation; for adolescents, it was defined as sexual attraction. Alaska natives are included in the American Indian race category. Pacific Islanders are included in Asian race category.
RESULTS
Respondents represented diverse demographic groups, including African-Americans (range 8–18% across the three surveys), Hispanics (8–14%) and GLBs (3–12%) as shown in table 1. Current smokers were present in all samples but most common in the internet sample (35%) and least common in the adolescent sample (3%).
Perceived source of constituents
Adults commonly believed that most of the constituents in cigarette smoke come from chemicals added by cigarette manufacturers (phone 61%; internet 72%). Relatively few adults believed that constituents come from burning the cigarette (phone 31%; internet 24%) or from tobacco before it is made into a cigarette (phone 8%; internet 4%). Adult smokers were more likely than non-smokers to believe that constituents come from additives and less likely to believe that constituents came from burning the cigarette (all p<0.05, table 2). Adolescents believed, in roughly equal measure, that constituents in cigarette smoke come from additives (43%) or from burning the cigarette (46%). Adolescent smokers and non-smokers showed few differences, perhaps due to the adolescent sample having few smokers.
Table 2.
Source of most dangerous things in cigarette smoke
| Adolescents in phone survey | Adults in phone survey | Adults in internet survey | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Non-smoker (n=1059) | Smoker (n=41) | Non-smoker (n=3759) | Smoker (n=1135) | Non-smoker (n=2684) | Smoker (n=1483) | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Tobacco before made into cigarettes | 11 (9 to 13) | 0** | 8 (7 to 10) | 7 (4 to 9) | 4 (4 to 5) | 3 (2 to 4)* |
| Additives | 43 (40 to 46) | 50 (34 to 67) | 58 (56 to 61) | 75 (70 to 80)** | 70 (68 to 72) | 77 (75 to 79)** |
| Burning the cigarette | 46 (43 to 50) | 50 (33 to 66) | 33 (30 to 36) | 18 (14 to 23)** | 26 (24 to 28) | 20 (18 to 22)** |
Percentages for phone surveys are weighted. Data missing for 3% of adolescent non-smokers.
p<0.05,
p<0.001.
The belief that cigarette filters trap all of the harmful chemicals in cigarette smoke was held by many adults (phone 33%; internet 22%) and adolescents (27%). Adult smokers believed that cigarette filters remove more harmful chemicals from cigarette smoke than non-smokers (weighted means: 1.81 (SE=0.02) vs 1.90 (SE=0.04), p=0.04) in the phone survey. Beliefs about the filter’s effectiveness did not differ between smokers and non-smokers in the adult online sample or in the adolescent sample.
Awareness and perceived harmfulness of constituents
The constituent that most participants had heard is in cigarette smoke was nicotine (89–95%) (table 3). Other commonly heard-of constituents were carbon monoxide (59–70%), ammonia (39–53%), arsenic (42–66%) and formaldehyde (41–68%). Fifteen constituents had awareness levels below 25% in all three samples. Awareness of NNN showed the most variability across the samples, with relatively high awareness in the phone survey (39% of adults, 62% of adolescents) and low awareness in the internet survey (15% of adults), perhaps because hearing the constituent name read aloud drew attention to its ‘nicotine’ ending. Perceived harmfulness exhibited no clear pattern of results across the samples, other than acrylonitrile, hydrogen cyanide and uranium having higher perceived harmfulness ratings in two of the three samples (table 3).
Table 3.
Reactions to cigarette smoke constituents
| Constituent | Aware constituent is in cigarette smoke % | Perceived harm Mean | Discouragement Mean | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Adol. phone | Adult phone | Adult internet | Adol. phone | Adult phone | Adult internet | Adol. phone | Adult phone | Adult internet | |
| 1,3-Butadiene | 8 | 8 | 11 | 3.11 | 3.06 | 2.92 | 3.63 | 3.43 | 2.79 |
| 1-Aminonaphthalene | 14 | 11 | 10 | 2.92 | 2.95 | 2.91 | 3.57 | 3.41 | 2.74 |
| 2-Aminonaphthalene | 13 | 13 | 5 | 2.86 | 3.01 | 2.92 | 3.57 | 3.30 | 2.60 |
| 4-Aminobiphenyl | 13 | 9 | 7 | 3.33 | 3.37 | 3.00 | 3.61 | 3.43 | 2.81 |
| Acetaldehyde | 18 | 20 | 21 | 3.22 | 3.48 | 2.86 | 3.62 | 3.49 | 2.87 |
| Acrolein | 6 | 6 | 7 | 3.41 | 3.27 | 2.70 | 3.48 | 3.29 | 2.61 |
| Acrylonitrile | 14 | 9 | 7 | 3.16 | 3.44 | 3.10 | 3.69 | 3.42 | 2.94 |
| Ammonia | 47 | 39 | 53 | 3.18 | 3.27 | 2.76 | 3.78 | 3.58 | 3.16 |
| Arsenic | 42 | 50 | 66 | 3.19 | 3.14 | 2.95 | 3.70 | 3.57 | 3.30 |
| Benzene | 37 | 39 | 41 | 3.08 | 3.13 | 2.76 | 3.52 | 3.41 | 2.81 |
| Benzo(a)pyrene | 15 | 19 | 19 | 3.38 | 3.38 | 2.93 | 3.62 | 3.39 | 2.83 |
| Carbon monoxide | 59 | 61 | 70 | 3.34 | 3.12 | 2.77 | 3.74 | 3.46 | 3.04 |
| Crotonaldehyde | 20 | 17 | 5 | 3.22 | 3.21 | 2.91 | 3.63 | 3.47 | 2.76 |
| Formaldehyde | 41 | 49 | 68 | 3.35 | 3.29 | 2.95 | 3.78 | 3.52 | 3.28 |
| Hydrogen cyanide | 33 | 31 | 34 | 3.33 | 3.54 | 3.18 | 3.69 | 3.50 | 3.22 |
| Isoprene | 18 | 13 | 9 | 3.33 | 3.34 | 2.82 | 3.61 | 3.44 | 2.93 |
| Lead | 33 | 23 | 27 | 3.30 | 3.44 | 2.94 | 3.76 | 3.55 | 3.31 |
| Naphthalene | 20 | 14 | 19 | 3.20 | 3.19 | 2.72 | 3.59 | 3.35 | 2.83 |
| Nicotine | 92 | 89 | 95 | 3.34 | 3.26 | 2.56 | 3.67 | 3.32 | 2.54 |
| Nitrosamine | 21 | 11 | 8 | 3.26 | 3.26 | 2.76 | 3.60 | 3.46 | 2.81 |
| N-nitrosonornicotine | 62 | 39 | 15 | 3.28 | 3.24 | 2.73 | 3.67 | 3.50 | 2.76 |
| NNK | 13 | 5 | 3 | 3.18 | 3.27 | 2.71 | 3.66 | 3.36 | 2.74 |
| Toluene | 11 | 13 | 21 | 3.01 | 3.11 | 2.81 | 3.55 | 3.41 | 2.79 |
| Uranium | 19 | 7 | 10 | 3.58 | 3.41 | 3.11 | 3.72 | 3.53 | 3.23 |
Percentages for phone surveys are weighted. Three constituents with the highest values for each survey sample in bold. Response scale for perceived harm and discouragement ranged from ‘not at all’ (coded as 1) to ‘a lot’ (coded as 4). For awareness, the median SEs were 2%/3%/1% in adult phone/adol. phone/internet surveys. For perceived harm, the median SEs were 0.10/0.08 in phone/internet surveys. For discouragement, the median SEs were 0.06/0.04 in phone/internet surveys. Perceived harm assessed only for participants aware the constituent was in cigarette smoke. Percentages and means for phone survey were weighted.
Adol., adolescent.
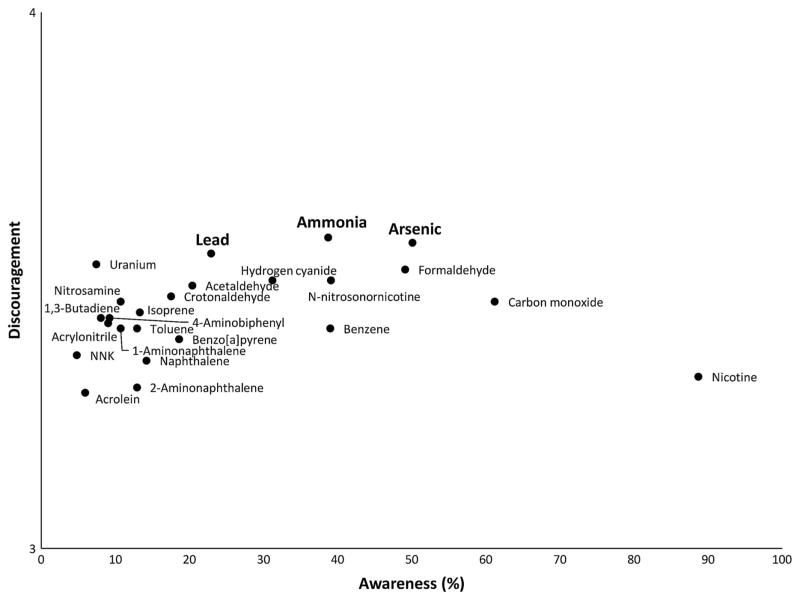
Discouragement from wanting to smoke
Across all three samples, ammonia, arsenic, formaldehyde, hydrogen cyanide, lead and uranium elicited the highest discouragement from wanting to smoke (table 3). The most discouraging constituents represented a range from low to moderate awareness, as shown in figure 1 and online supplementary figures S1 and S2. Acrolein was the least discouraging constituent for all samples. Nicotine and 2-aminonaphthalene were least discouraging among adults, and benzene and toluene were least discouraging among adolescents.
Figure 1.
Adults in national phone study: discouragement from wanting to smoke and awareness of cigarette smoke constituents.
Discouragement from wanting to smoke was greater for constituents that adults had heard are in cigarette smoke than for ones they had not (71% vs 68% phone survey, aOR=1.19, 95% CI 1.04 to 1.35; 46% vs 34% internet survey, aOR=2.02, 95% CI 1.79 to 2.27) in adjusted analyses (table 4). The same was true for adolescents (82% vs 74%, aOR=1.84, 95% CI 1.41 to 2.41). Among adults, discouragement was lower for constituent names that started with a number than those that did not start with a number (66% vs 70% phone survey, aOR=0.76 95% CI 0.64 to 0.91; 30% vs 39% internet survey, aOR=0.76, 95% CI 0.64 to 0.90). Adolescents showed a similar pattern that was not statistically significant.
Table 4.
Correlates of discouragement from smoking
| Adolescents in phone survey (n=863) | Adults in phone survey (n=4445) | Adults in internet survey (n=4024) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| % | aOR (95% CI) | % | aOR (95% CI) | % | aOR (95% CI) | |
| Constituent characteristics | ||||||
| Respondent aware constituent is in cigarette smoke | ||||||
| No | 73.7 | Ref | 68.0 | Ref | 34.2 | Ref |
| Yes | 81.5 | 1.84 (1.41 to 2.41)** | 71.3 | 1.19 (1.04 to 1.35)* | 45.5 | 2.02 (1.79 to 2.27)** |
| Constituent name starts with number | ||||||
| No | 77.9 | Ref | 69.9 | Ref | 39.3 | Ref |
| Yes | 71.2 | 0.88 (0.60 to 1.29) | 65.7 | 0.76 (0.64 to 0.91)* | 29.7 | 0.76 (0.64 to 0.90)* |
| Constituent name ending | ||||||
| ‘ene’ or ‘ine’ | 72.8 | Ref | 66.5 | Ref | 30.5 | Ref |
| ‘ide’ or ‘yde’ | 80.8 | 1.79 (1.27 to 2.52)** | 71.9 | 1.43 (1.23 to 1.68)** | 43.5 | 2.21 (1.92 to 2.55)** |
| Other | 80.4 | 1.95 (1.44 to 2.64)** | 71.7 | 1.78 (1.54 to 2.06)** | 45.8 | 2.89 (2.55 to 3.28)** |
| Constituent name length | 0.99 (0.95 to 1.03) | 1.02 (1.00 to 1.04)* | 0.99 (0.97 to 1.01) | |||
| Person characteristics | Ref | Ref | Ref | |||
| Age | 0.23 (0.07 to 0.81)* | 1.21 (1.15 to 1.27)** | 1.39 (1.30 to 1.49)** | |||
| Sex | ||||||
| Female | 81.2 | Ref | 74.7 | Ref | 43.5 | Ref |
| Male | 72.6 | 0.52 (0.37 to 0.73)** | 63.1 | 0.47 (0.40 to 0.56)** | 31.9 | 0.50 (0.43 to 0.57)** |
| Gay, lesbian or bisexual† | ||||||
| No | 76.9 | Ref | 69.7 | Ref | 38.6 | Ref |
| Yes | 75.5 | 1.02 (0.43 to 2.42) | 56.8 | 0.64 (0.42 to 0.96)* | 31.4 | 0.72 (0.57 to 0.91)* |
| Race | ||||||
| White | 82.0 | 0.60 (0.38 to 0.95)* | 75.6 | 0.51 (0.42 to 0.62)** | 45.0 | 0.63 (0.52 to 0.77)** |
| Other | 75.7 | Ref | 66.7 | Ref | 36.3 | Ref |
| Hispanic | ||||||
| No | 77.3 | Ref | 68.6 | Ref | 37.1 | Ref |
| Yes | 70.3 | 0.53 (0.27 to 1.02) | 76.0 | 1.38 (1.01 to 1.89)* | 45.2 | 1.67 (1.27 to 2.18)** |
| Attended college† | ||||||
| No | 75.3 | Ref | 70.4 | Ref | 37.7 | Ref |
| Yes | 82.2 | 1.99 (1.29 to 3.06)* | 66.8 | 1.35 (1.12 to 1.62)* | 38.2 | 1.54 (1.24 to 1.92)** |
| Numeracy | ||||||
| Low | 75.6 | Ref | 66.0 | Ref | 30.7 | Ref |
| High | 77.2 | 1.11 (0.75 to 1.63) | 70.5 | 1.34 (1.12 to 1.60)* | 38.4 | 1.59 (1.21 to 2.08)** |
| Smoking status | ||||||
| Non-smoker | 78.7 | Ref | 78.3 | Ref | 48.6 | Ref |
| Smoker | 37.1 | 0.08 (0.04 to 0.17)** | 38.3 | 0.09 (0.07 to 0.11)** | 17.8 | 0.12 (0.11 to 0.15)** |
Outcome was being ‘a lot’ discouraged from wanting to smoke. Adjusted models controlled for all variables in table and constituent panel. The intraclass correlation was 0.45 for adolescents, 0.55 for adults in the phone survey and 0.48 for adults in the internet survey.
p<0.05,
p<0.001.
For analyses of adolescent data, attended college was whether mother attended college and sexual orientation was sexual attraction to people of the same sex.
aOR, adjusted OR; Ref, reference group.
Discouragement was lower for constituents that ended in ‘ene’ or ‘ine’ than for constituents that ended in ‘ide’ or ‘yde’, among adults (67% vs 72% phone survey, aOR=1.43, 95% CI 1.23 to 1.68; 31% vs 44% internet survey, aOR=2.21, 95% CI 1.92 to 2.55) and adolescents (73% vs 81%, aOR=1.79 95% CI 1.27 to 2.52), or for any other endings (table 4). The same pattern of findings appeared in sensitivity analyses that omitted data for nicotine (data not shown).
Shorter constituent names were more discouraging for all samples in unadjusted analyses (see online supplementary table S2), but adjusting only for constituent awareness caused these findings to lose statistical significance (table 4). In the fully adjusted models, longer names were more discouraging for the adult phone sample. Sensitivity analyses dropping constituent name length from the adjusted models showed roughly identical findings for the other variables.
With respect to participant characteristics, discouragement elicited by constituents was much higher among non-smokers than smokers across the three samples in adjusted analyses. For example, in the phone survey, 78% of adult non-smokers but only 38% of adult smokers said the constituents would discourage them from wanting to smoke (aOR=0.09, 95% CI 0.07 to 0.11), numbers that were nearly identical for adolescents (79% vs 37%, aOR=0.08, 95% CI 0.04 to 0.17). Discouragement was also more common among women and whites in all three samples as well as adult Hispanics and less common among adult GLBs. In addition, discouragement was higher among adults who attended college and adolescents whose mothers had attended college and more numerate adults than among those with lower education or numeracy. Finally, discouragement was highest at younger ages among adolescents and older ages among adults.
DISCUSSION
Across three national samples that included a total of over 10 000 US adults and adolescents, we found that many people lacked a basic understanding of the origin of harmful chemicals in cigarette smoke. Many people did not understand that most toxic constituents in cigarette smoke come from burning the cigarette rather than from cigarette manufacturer additives. Many also incorrectly believed that cigarette filters trap the toxic chemicals in cigarette smoke. On a more positive note, we identified several principles that could inform communications about cigarette smoke constituents. People were most discouraged by familiar constituents with names that started with letters rather than numbers, but were less discouraged by ones ending with ‘ine’ as in the familiar constituent nicotine.
Most toxic chemicals develop as the cigarette burns and do not primarily come from cigarette additives.23 The tobacco industry has invested heavily in promoting ‘additive-free’ cigarettes.29 We speculate that exposure to this advertising may have contributed to the finding that people believe added chemicals, not chemicals inherent to the tobacco leaf and burning of cigarettes, are responsible for cigarettes’ toxicity. Another misconception noted in our study is the belief that cigarette filters trap most of the harmful substances in cigarette smoke. Future public health communications about cigarette smoke constituents should consider that many people hold erroneous beliefs. Educational campaigns and other communication vehicles such as cigarette pack constituent disclosures could attempt to address these misunderstandings.
One of the most important constituent communication principles that we identified is that familiar constituents appear to discourage more people from wanting to smoke than less familiar ones. This finding confirms and extends the previous findings of Hall et al and is consistent with other research on constituents.8,15 Health communication campaigns may still be able to productively focus on less familiar constituents; however, more research is needed on how to best address low understanding of these unfamiliar cigarette smoke constituents. Campaigns with substantial resources could improve the public’s knowledge of one or two specific constituents, with the goal of simultaneously increasing awareness and discouraging smoking. For example, nitrosamines and acrolein had low awareness and were least discouraging, but research shows these are two of the most harmful constituents in cigarette smoke.30–32 Informing the public about these harmful chemicals in cigarette smoke may be particularly important.
Other important constituent communication principles that we identified relate to constituent name characteristics. Constituent names that started with a number elicited less discouragement, perhaps because these names seemed technical, which may have prevented participants from creating meaning.20 Constituent names ending with text that sounded like ‘ene’ were also less discouraging. We speculate that this may be due in part to an association with nicotine, a constituent that is widely associated with cigarettes but is among the least discouraging. It could also be that endings that sounded like ‘ide’ benefit from associations with highly discouraging constituent names like formaldehyde. This insight follows from some of our previous qualitative research, indicating that unfamiliar constituents lead people to find similar sounding words to establish meaning.20 These speculations on the mechanism driving constituent name effects require further study.
Demographic differences in discouragement from wanting to smoke followed disparities in smoking prevalence and sequelae. Differences by smoking status were the most dramatic, with smokers being consistently much less discouraged than non-smokers. This finding may be an example of rejection of risk information by smokers, a common finding, or it may be a realistic self-assessment that health information on its own may not be enough to counteract the potent, addictive hold that cigarettes have on smokers.33 Other disparities, found even after controlling for smoking status, followed patterns of smoking prevalence or risk. Discouragement was lower among respondents with lower education, sexual minorities, younger adults and older teens. The findings for smoking status, age (among adults) and education mirror previous findings reported by Hall et al.15 The findings for race and sex are similar to the ‘white male effect’, a general pattern of findings in which this group minimises their risks for many potential harms.34 Mode of constituent information delivery, read aloud or in print, may also affect constituent perceptions.35 Our findings for phone and internet studies were largely concordant, but larger differences for constituent names endings in the online sample merit further exploration. Demographic disparities and mode effects merit special attention in the design and implementation of future research on the impact of constituent messages that could be delivered via communication campaigns, disclosures on cigarette packs, or through other means.
Our study’s strengths include the use of probability sampling for adults and adolescents in the phone survey; careful survey development and testing through cognitive interviews and pilot testing; and replication of many of our findings across three different samples. Limitations to the study include the use of cross-sectional studies that limit causal inferences about many of the associations we report. We relied on single-item measure for most constructs. The impact of constituent information on behaviour may differ, though these perceived effectiveness measures are often good correlates of intentions and behaviour and useful in the early stages of message development.36,37 We focused on the 18 constituents in the FDA’s abbreviated list, but as measurement approaches become more refined and widely available, other constituents may be important to study as well. Though we weighted point estimates for phone survey participants, we did not use weights in our multilevel analyses of discouragement as these methods are not yet well developed. Point estimates differed across the survey modes, but the pattern of associations with other variables showed many similarities. The fixed order of constituent names within panels and different composition of constituents across panels may have had some effect. Future work could include randomisation to more evenly distribute order effects and constituent names artificially created to reflect the dimensions we examined.
As our studies are among the first to identify elements of constituent names that discourage smoking, future research should aim to replicate our findings and further fill gaps in our understanding of how best to communicate about cigarette smoke constituents. The widespread misunderstandings that constituents come from tobacco additives highlight the importance of banning the use of ‘additive-free’ and similar terms that falsely suggest healthfulness and risk reduction; however, educational campaigns may more effectively improve understanding of constituents than dispel myths about additives.38 Given the current public understanding of constituents, arsenic and formaldehyde are promising topics for campaigns. We had hoped that useful topics would include nitrosamines and acrolein, two particularly harmful cigarette smoke constituents, but they had low awareness and generally elicited less discouragement than other constituents.23,32 If campaigns can invest resources to remedy low awareness, nitrosamines and acrolein may be important topics for health messages. Even though these constituents had low awareness and elicited less discouragement and have the ‘ine’ ending, they are important because they are particularly harmful. However, it may be more beneficial to develop awareness around acrylonitrile or various aldehydes as they do not have the less discouraging ‘ine’ ending reminiscent of nicotine. Research on messages and delivery channels to effectively communicate with the public about harmful constituents are an important next step for the field.
Supplementary Material
What this paper adds.
US Food and Drug Administration is required to inform the public about toxic constituents (chemicals) in cigarette smoke.
Prior research suggests that many US adults are not aware of cigarette smoke constituents other than nicotine and tar.
Little research describes how the public understands constituents, particularly lesser known constituents, and their origins.
These 3 national surveys of more than 10 000 US adults and adolescents found that most respondents mistakenly believed that constituents come from tobacco additives rather than burning the cigarette.
Participants were more discouraged from smoking by constituents that they had heard of (eg, arsenic and formaldehyde) and less discouraged by constituents that started in a number or ended in ‘ene’/‘ine’ (eg, 1-aminonapthalene).
In order to reduce smoking, future public health communications might focus on the constituents that are most discouraging or attempt to raise awareness of lesser known but highly toxic constituents.
Acknowledgments
Funding Research reported in this publication was supported by grant number P50CA180907 from the National Cancer Institute and FDA Center for Tobacco Products (CTP).
Footnotes
Contributors NTB and JKP led instrument development. RPA and MHB led and oversaw data collection. JCM, MHB and RPA conducted data analysis. NTB led writing. All authors made significant contributions to the interpretation of data reported here and the manuscript’s conceptualisation, writing and revision.
Publisher's Disclaimer: Disclaimer The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Competing interests KMR has served as an expert consultant in litigation against cigarette manufacturers and internet tobacco vendors.
Ethics approval The University of North Carolina Institutional Review Board approved study protocol and materials.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Rentería E, Jha P, Forman D, et al. The impact of cigarette smoking on life expectancy between 1980 and 2010: a global perspective. Tob Control. 2016;25:551–7. doi: 10.1136/tobaccocontrol-2015-052265. [DOI] [PubMed] [Google Scholar]
- 3.Talhout R, Schulz T, Florek E, et al. Hazardous compounds in tobacco smoke. Int J Environ Res Public Health. 2011;8:613–28. doi: 10.3390/ijerph8020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta, GA: Centers for Disease Control and Prevention (US); 2014. [accessed 22 Jul 2016]. http://www.ncbi.nlm.nih.gov/books/NBK179276/ [PubMed] [Google Scholar]
- 5.Food and Drug Administration. Harmful and Potentially Harmful Constituents in Tobacco Products and Tobacco Smoke; Established List. 2012 77 FR 20034. http://www.fda.gov/downloads/TobaccoProducts/Labeling/RulesRegulationsGuidance/UCM297981.pdf.
- 6. [accessed 22 Jul 2016];Family Smoking Prevention and Tobacco Control Act. 2009 https://www.gpo.gov/fdsys/pkg/PLAW-111publ31/pdf/PLAW-111publ31.pdf.
- 7.Food and Drug Administration. Draft Guidance for Industry: Reporting Harmful and Potentially Harmful Constituents in Tobacco Products and Tobacco Smoke Under the Federal Food, Drug, and Cosmetic Act. 2012 77 FR 20030. http://www.fda.gov/downloads/TobaccoProducts/Labeling/RulesRegulationsGuidance/ucm297828.pdf.
- 8.Morgan JC, Byron MJ, Baig SA, et al. How people think about the chemicals in cigarette smoke: a systematic review. J Behavioral Med. doi: 10.1007/s10865-017-9823-5. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cummings KM, Hyland A, Giovino G, et al. Are smokers adequately informed about the health risks of smoking and medicinal nicotine? Nicotine Tob Res. 2004;6:333–40. doi: 10.1080/14622200412331320734. [DOI] [PubMed] [Google Scholar]
- 10.Ipsos-Eureka. Public Health Value of Disclosed Cigarette Ingredients and Emissions Data. 2009 http://www.ipsos.com/public-affairs/sites/www.ipsos.com.public-affairs/files/documents/Australia-tobacco-emissions.pdf.
- 11.Hammond D, Fong GT, McNeill A, et al. Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii19–25. doi: 10.1136/tc.2005.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swayampakala K, Thrasher JF, Hammond D, et al. Pictorial health warning label content and smokers’ understanding of smoking-related risks—a cross-country comparison. Health Educ Res. 2015;30:35–45. doi: 10.1093/her/cyu022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siahpush M, McNeill A, Hammond D, et al. Socioeconomic and country variations in knowledge of health risks of tobacco smoking and toxic constituents of smoke: results from the 2002 International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii65–70. doi: 10.1136/tc.2005.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bansal-Travers M, Cummings KM, Hyland A, et al. Educating smokers about their cigarettes and nicotine medications. Health Educ Res. 2010;25:678–86. doi: 10.1093/her/cyp069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall MG, Ribisl KM, Brewer NT. Smokers’ and nonsmokers’ beliefs about harmful tobacco constituents: implications for FDA communication efforts. Nicotine Tob Res. 2014;16:343–50. doi: 10.1093/ntr/ntt158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crawford MA, Balch GI, Mermelstein R Tobacco Control Network Writing Group. Responses to tobacco control policies among youth. Tob Control. 2002;11:14–19. doi: 10.1136/tc.11.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnett JJ. Winston’s ‘No Additives’ campaign: ‘straight up’? ‘no bull’? Public Health Rep. 1999;114:522. doi: 10.1093/phr/114.6.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Etter JF. Informing smokers on additives in cigarettes: a randomized trial. Patient Educ Couns. 2007;66:188–91. doi: 10.1016/j.pec.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Wiseman KD, Cornacchione J, Wagoner KG, et al. Adolescents’ and young adults’ knowledge and beliefs about constituents in novel tobacco products. Nicotine Tob Res. 2016;18:1581–7. doi: 10.1093/ntr/ntw009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moracco KE, Morgan JC, Mendel J, et al. ‘My first thought was croutons:’ perceptions of cigarettes and cigarette smoke constituents among adult smokers and nonsmokers. Nicotine Tob Res. 2016;18:1566–74. doi: 10.1093/ntr/ntv281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boynton MH, Agans RP, Bowling JM, et al. Understanding how perceptions of tobacco constituents and the FDA relate to effective and credible tobacco risk messaging: a national phone survey of U.S. adults, 2014–2015. BMC Public Health. 2016;16:516. doi: 10.1186/s12889-016-3151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 8. AAPOR; 2015. [Google Scholar]
- 23.Hecht SS. Research opportunities related to establishing standards for tobacco products under the Family Smoking Prevention and Tobacco Control Act. Nicotine Tob Res. 2012;14:18–28. doi: 10.1093/ntr/ntq216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Noar SM, Hall MG, Francis DB, et al. Pictorial cigarette pack warnings: a meta-analysis of experimental studies. Tob Control. 2016;25:341–54. doi: 10.1136/tobaccocontrol-2014-051978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Best practices for asking questions about sexual orientation on surveys. Los Angeles: The Williams Institute; 2009. http://williamsinstitute.law.ucla.edu/wp-content/uploads/SMART-FINAL-Nov-2009.pdf. [Google Scholar]
- 26.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 27.Davis S, Malarcher A, Thorne S, et al. State-specific prevalence and trends in adult cigarette smoking—United States, 1998–2007. JAMA. 2009;302:250–2. [Google Scholar]
- 28.Arrozola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2015;64:381–5. [PMC free article] [PubMed] [Google Scholar]
- 29.McDaniel PA, Malone RE. ‘I always thought they were all pure tobacco’: American smokers’ perceptions of ‘natural’ cigarettes and tobacco industry advertising strategies. Tob Control. 2007;16:e7–e7. doi: 10.1136/tc.2006.019638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.CDC. Immediately dangerous to life or health concentrations (IDLH): chemical listing and documentation of revised IDLH values. 2014 http://www.cdc.gov/niosh/idlh/intridl4.html.
- 31.Counts ME, Hsu FS, Laffoon SW, et al. Mainstream smoke constituent yields and predicting relationships from a worldwide market sample of cigarette brands: ISO smoking conditions. Regul Toxicol Pharmacol. 2004;39:111–34. doi: 10.1016/j.yrtph.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 32.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Personal habits and indoor combustions. Volume 100 E. A review of human carcinogens. IARC Monogr Eval Carcinog Risks Hum. 2012;100:1–538. [PMC free article] [PubMed] [Google Scholar]
- 33.Weinstein ND. Accuracy of smokers’ risk perceptions. Ann Behav Med. 1998;20:135–40. doi: 10.1007/BF02884459. [DOI] [PubMed] [Google Scholar]
- 34.Finucane ML, Slovic P, Mertz CK, et al. Gender, race, and perceived risk: the ‘White Male’ effect. Health Risk Soc. 2000;2:159–72. [Google Scholar]
- 35.Gallopel-Morvan K, Gabriel P, Le Gall-Ely M, et al. The use of visual warnings in social marketing: the case of tobacco. J Bus Res. 2011;64:7–11. [Google Scholar]
- 36.Brennan E, Durkin SJ, Wakefield MA, et al. Assessing the effectiveness of antismoking television advertisements: do audience ratings of perceived effectiveness predict changes in quitting intentions and smoking behaviours? Tob Control. 2014;23:412–18. doi: 10.1136/tobaccocontrol-2012-050949. [DOI] [PubMed] [Google Scholar]
- 37.Davis KC, Nonnemaker J, Duke J, et al. Perceived effectiveness of cessation advertisements: the importance of audience reactions and practical implications for media campaign planning. Health Commun. 2013;28:461–72. doi: 10.1080/10410236.2012.696535. [DOI] [PubMed] [Google Scholar]
- 38.FDA. FDA takes action against three tobacco manufacturers for making ‘additive-free’ and/or ‘natural’ claims on cigarette labeling. 2015 http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm459840.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.