Abstract
Objective
There is a growing demand for interpreters in the cancer setting. Interpreters, the link to quality care for limited English proficiency patients, face many psychosocial stressors in their work. This project assessed interpreters’ experiences of stress and piloted a resiliency program to help interpreters cope with stressors.
Methods
From 2013–2014, we pilot tested a targeted resiliency program with interpreters from 3 Boston-based hospitals. In Phase 1, we conducted 5 focus groups (n=31) to identify interpreters’ psychosocial needs. In Phase 2, we developed and tested a 4-hour group program with 29 interpreters (response rate= 90%; 69% female, 54% Hispanic, 85% born outside of the U.S.).
Results
Phase 1. Stressors were patient-based (seeing young patients decline), interactions with medical team (unsure of role), and systems-based (appointment unpredictability). Phase 2. At baseline interpreters reported low abilities to cope with stress (measured by the Measure of Current Status (MOCS-A)). At 4 week follow-up we found improvements in job satisfaction (p=.02; Cohen’s d=.41) and declines in sick days (p=.08; Cohen’s d=.38). Stress reactivity (MOCS-A) improved; specifically participants reported feeling more assertive about their needs (p=.10; Cohen’s d=.30) and more able to relax at will (p=.10; Cohen’s d=.35)—important mechanisms to lower distress.
Conclusions
We piloted a resiliency program for medical interpreters in cancer care. We found that interpreters experience distress and have low coping skills. This program resulted in improved work factors and stress reactivity. Future research should include further implementation and testing in a larger, randomized trial.
Keywords: interpreter, Relaxation Response, resiliency, stress, burnout, coping
INTRODUCTION
Over the past two decades the number of people in the United States with Limited English Proficiency (LEP), persons who are unable to communicate effectively by speaking English, has grown tremendously. In the U.S. in 2011, 25 million adults., 9% of the. population, were LEP [1]. As a result, there is a high, and increasing, demand for medical interpreters nationwide [2]. The number of cancer patients in the U.S. is also increasing [3], and providing quality comprehensive cancer care in the context of an increasingly ethnically and linguistically diverse patient population is challenging. The provision of quality care in the cancer setting involves complex discussions between doctors and patients, which rely on patients’ understanding of their diagnosis and treatment plan as well as ongoing involvement of the physician in their care [4]. Indeed, language barriers have been evidenced to influence patients’ trust in providers, compliance with medical recommendations, and receipt of regular medical care [5–7].
Patients with LEP are at risk for lower quality cancer preventive care [8–11] and treatment [12,13] and at high risk for medical errors due to poor communication with their physicians [11]. Medical interpreters play an essential role in the treatment of cancer patients with LEP. Cancer patients are dependent on medical interpreters, and information conveyed through them, to make complex cancer care decisions.
The value of professional medical interpreters is well-established [14]. The use of professional medical interpreters has been associated with improved clinical outcomes, health care utilization, greater diagnostic comprehension, and treatment adherence [14–18]. However, the demands of providing care to patients with cancer can be overwhelming. Studies have documented the presence and consequence of burnout, on oncology clinicians [19–21]. Burnout has been associated with widespread negative outcomes for both patients and providers, being linked to more medical errors, greater work dissatisfaction, and withdrawal from the workforce by oncology clinicians [22,23]. These research findings emphasize the importance of identifying, and intervening upon, burnout early.
As members of the oncology care team, interpreters are at risk for burnout. There are preliminary [24] and anecdotal [7] data suggesting that stress levels are high among medical interpreters working in the cancer setting. One qualitative study [25] found that interpreters expressed feelings of distress and burnout. Another qualitative study, conducted in Australia, reported that interpreters’ causes for distress were related to managing patient boundaries and personal emotions in difficult interpretation encounters [26]. Ongoing stress may negatively impact both the interpreters and the patients who rely on the interpreter in the clinical setting. Stress can lead to cognitive dysfunction or inflexibility, impairing working memory, and behavioral flexibility [27] - all skills critical to the work of medical interpreters.
Professional medical interpreters are required to undergo training to assure fluency in medical terminology, awareness of cultural differences, and competency in specialized medical setting; psychosocial training, however, is generally not required. Once employed, interpreters do not consistently receive training or support to cope with psychosocial stressors encountered, particularly in cancer care encounters. To our knowledge, no research has been conducted in the U.S. to identify the primary sources of interpreters’ stress, particularly in working with cancer patients, or interventions conducted to address interpreters’ psychosocial needs.
Resiliency, a multidimensional construct that refers to the ability to maintain adaptation and effective functioning under adversity and challenges, provides a framework for understanding the adjustment to stress as a dynamic process. Research is warranted to examine the sources of interpreter stressors and to develop trainings to promote resilience among these professionals who play key roles in securing quality cancer care for LEP patients. In order to develop a resiliency program targeted to the needs of medical interpreters, we conducted a two-phase study to (1) identify the needs of medical interpreters working with cancer patients and (2) develop and test a psychoeducational resiliency program intended to enhance interpreters’ skills to effectively manage stressful encounters and cope with the personal effects of encounters. In Phase 1, we conducted focus groups and individual interviews to learn about stressors shared by medical interpreters working in cancer care. In Phase 2, we adapted an existing resiliency program and conducted a pilot trial to assess its feasibility, acceptability, and potential efficacy. IRB approval was obtained from the Dana-Farber Harvard Cancer Center and University of Massachusetts Boston prior to the conduct of the study.
METHODS
The study was conducted from November 2013 to May 2014. Three Boston-based academic medical centers, affiliated with the Dana-Farber Harvard Cancer Center, participated: Brigham and Women’s Hospital (BWH), Massachusetts General Hospital (MGH), and Dana-Farber Cancer Institute (DFCI). BWH and MGH are general hospitals that treat cancer patients; DFCI is a tertiary cancer center. The three hospitals are staffed by professional interpreters. Professional medical interpreters receive certificates from programs, which include medical content (e.g., medical terminology, anatomy, and pathophysiology), interpreting skills (e.g., memory retention, sight-translation), and professional standards of practice and code of ethics. Additionally, some professional interpreters get “certified” by an accreditation agency, which involves a two-part examination consisting of current standards and codes of ethics and performance interpretation role plays. Certification requires ongoing continuing education credits.”
Phase 1: Qualitative Study
The aim of this phase was to identify the psychosocial needs of medical interpreters working with cancer patients, specifically the types of cancer care communications that are the most difficult or stressful, areas of need for education and skills training, and preferred program modality.
Participants and recruitment
Medical interpreters from one of the three participating hospitals who worked ≥20 hours/week, were at least 18 years old, and were able to provide informed consent were eligible to participate.
Interpreter directors from the three hospitals sent a study flyer via email to interpreters. Interpreters were screened for eligibility, consented prior to group participation and received $25 remuneration. All participants were also asked to complete an exit interview.
Data Collection
Semi-structured interview guides, for the group and individual interviews, were developed and piloted. The focus guide consisted of the following domains: 1) stress definitions/conceptualization, 2) types of work stressors experienced, particularly with cancer encounters, 3) types of skills training desired, and 4) barriers to participation and preferences for intervention delivery modality. In the individual interviews, interpreters were queried about additional work stressors that they had not shared in the group.
Focus groups lasted approximately 90 minutes, and individual interviews lasted approximately 20 minutes. All interviews were recorded and transcribed; transcripts were reviewed by study investigators for quality. Two members of the study team independently coded all data using NVivo 10, applying framework thematic analyses, to identify themes and to develop a coding structure. Through an iterative process of coding and review, the coders (GP, CF) and lead investigator (EP) developed the coding framework and categories; all data were coded, and an excellent level of coder reliability was achieved (Kappa=.98).
Results
Five focus groups were conducted, with a total of 31 participants; 29 participants also completed an exit interview. Groups began with an exploratory question about what interpreters’ enjoyed about their work. In particular, interpreters’ expressed satisfaction in being able to aid patients directly by facilitating their understanding of medical information and empowering patients to ask questions. Interpreters voiced that they felt they made a difference in patients’ experiences of care by helping vulnerable patients better navigate the health care system, and making all participating parties feel more at ease during clinical encounters. Interpreters also voiced that they found their jobs to be stimulating, since medical interpreting offers opportunities for learning and job diversity.
Interpreter stressors
Overall, interpreters shared experiences of powerful, salient stressors. High levels of distress were observed as interpreters emoted during the group and individual interviews. Relatedly, many participants were very thankful that we were eliciting their opinions and experiences. Expressions of gratitude were voiced; there was a shared sentiment that, otherwise, “no one notices us.”
Repeated themes emerged about the types of stressors interpreters experience on a daily basis, grouped into: patient-based, interactions with medical team, role challenges, and systems based (See Table 1). While the types of stressors discussed in the focus group and the individual interviews were similarly shared, in the individual interviews participants were more likely to share how they were affected by witnessing patient suffering and attachment to patient, and in the focus groups additional system based stressors were elicited.
Table 1.
Interpreter Stressors
| Patient-Based Stressors | |
|---|---|
| Theme | Quote |
| Patients Who are Declining | Or when you see that a patient’s health is declining, the visual effect, especially if you’ve worked with that patient over time. And unfortunately we just keep seeing the patients that aren’t getting better. |
| Older and Younger Patients |
They come home from radiation oncology in the Dora the Explorer bed, and it’s so sad, because they are so little and yet they are so powerful and they are fighting this thing. It is difficult for me when there aren’t other people taking care of the patient, especially when you know it’s an elderly patient and no one’s really going to follow-up on their medicines like it should be done. |
| Impoverished patients |
It’s also stressful to be present for somebody who lacks health literacy and so seems to think that there’s an infinite number of drugs down the road… that the three that haven’t worked so far so there’ll be a fourth, fifth and so on. And I know that that’s not true but they want to believe that. … you see the patient that does not have the resources to get the care that he or she needs. Also, especially for a patient… sometimes they need to go to rehab, or they cannot have access to rehab, or they don’t have the money to buy the medication, or they need a ride. Those kinds of things that sometimes are kind of frustrating. |
| Developing attachments and relationships to patients | Some of the patients that I interpret for over a long time and all the time they have told me stuff about themselves… And that’s tough when they pass away, because sometimes when you get the page saying “this patient passed away” it is tough to hear. |
| Identifying with patient and family member |
He was very young, almost like my age and also the thing that touched me personally because …he was like my age too. So I kind of identify with the patient. And then I just, I fell apart…I thought of my mother with Alzheimer’s and if this were to happen to her. Not to have people to take care of her… It was very frightening to me and I actually had to leave the appointment and calm down. |
| English speaking patients and family members |
Sometimes the patients know some English but insist on using only English. That’s a lot of pressure on us! Because we have to sometimes interrupt a little bit “oh- you can use (your native language), maybe that will be faster”. The doctor would probably prefer if they spoke in (their native language), too… “…family members who actually are fully bilingual really make it sometimes very difficult for us to interpret because a lot of times people don’t fully understand what interpreting is, and think that we have to say the exact words that the doctor used.” |
| Don’t want patient to know diagnosis |
Before they come to me as an interpreter the family has been interpreting and not letting them know everything that’s going on. “particularly, one case, there was a patient who came who was late stage and still doesn’t know. The patient does feel something going on, but they keep telling him it’s something else.” |
| Interactions with Medical Team | |
|---|---|
| Theme | Quote |
| Multiple doctors or caregivers talking at the same time | You know sometimes when doctors are talking all at the same time, everyone is talking, you know they are developing new things or treatment, they talk to each other… there are many disturbances in the encounter, phone ringing, a lot of noises around.. and all these factors together it makes you feel stress. So you are the only one, the only connector so you need to listen well, to pay attention, but you cannot… |
| Having responsibility but no control | You don’t want to take charge of the situation because you are not the top guy there, from the interpreting point of view you are the person who links them together…At the same time you have no control; the doctor is the one able to control the situation. |
| Not feeling part of a team | We are usually one of the most important pieces when you are having an appointment…at the same time, we’re the forgotten ones. |
| Abilities not respected | So a lot of times the lack of respect among the professionals is there… And that’s besides having to deal with patient’s families and lack of respect there, you also have to deal with your own groups. |
| Role Challenges | |
|---|---|
| Theme | Quotes |
| Bridging communication between the doctor, patient and family |
When I see that kinds of cases…when the provider is like, “I want this.” Is demanding. And that patient is not getting and she cannot understand that the patient in that moment is in another world and I am there trying to make them communicate together. But another stress for me is when the doctor tells the patient “you have terminal [cancer]”. And children understand the word and they cry. And then I don’t know what to say to get them to [calm down] like “please calm down, let’s hear the doctor first”, but they keep crying and keep crying. And it’s like- What should I do now? Should I be silent? Or should I tell the doctor “please give them some time and then come back and start from the beginning”? |
| Translating cultures | It’s two cultures and you learn at the same time the cross cultural, the diversity part is important because you have to understand the culture that you are interpreting and at the same time the mainstream here. |
| Making cultural adaptations | Maybe the way Hispanics talk sometimes, sometimes is not that it’s a dialect or something like that, but they have their own way of speaking and leaving sentences unfinished and take it for granted that you understand what they mean. And often they keep on talking. They don’t take any breaks and you have to really stop them and say, “wait a minute. I don’t quite understand what you mean.” And even when you say that several times, they continue to do the same. It’s like it doesn’t compute in their minds that it’s not easy to translate or to interpret when they are talking so continuously and taking for granted that you know what is in their minds… It is very stressful… |
| Maintaining professionalism and accuracy | And I have always tried to register when I interpret the same or a similar tone that the people talk. So inevitably if someone’s screaming, well I won’t scream but I raise the pitch of my voice or I’ll speak stronger. If somebody is crying or very sad I would go to that level also. And those things together with everything else makes me also feel all of those. I mean, I’m not made of stone. So all of those little things someway or another always get to me at some point. So I, while trying to maintain always that professional appearance, I’m usually, not usually, but in situations like this I’m usually struggling to keep my composure until the end. And then at the end I usually feel drained… |
| Breaking bad news | She came here, she didn’t, she thought she was cured. So she didn’t know the reason they transferred her here was because she was terminal. So that difficult for me to realize that she didn’t know the severity of her case and I was the one to tell her. She thought that it was something different or another disease that they could cure. So that was very very hard to let her know that she was at the final stage and that there wasn’t anything that they could do for her. |
| System Based | |
|---|---|
| Theme | Quotes |
| Lack of resources | Sometimes being short of help-- not knowing which people to answer first. Sometimes it’s hard. |
| Lack of time |
So you get one page after another and you try to explain “I am going to help you but I am already tied up and I am going to be seeing another patient” [they respond] “oh I need you right now”. Time management is an issue. I think it’s an issue especially for this kind- you really have to triage and go with your gut- what goes first, figuring out what the situation is…when you get a page from the same person over and over again… I almost had 10 pages… every time they paged me I had to excuse myself and use the phone. |
| Scheduling |
And (the doctors) will say something like ‘I booked you!”. [I respond] “yeah- you booked me at 2. It is now 4. I have somebody at 4.”…I have had nurses question me: “What do you mean you can’t come here. Where is it that you’re going next? “ I was about to say in addition to that about how they tell me “oh- I already booked the patient and the patient is here waiting for you. The doctor is waiting for you.” And no, it’s not on my schedule. The doctor was not ready. So I tell them I will take care of the patient now and I will be there in 15 minutes. And 15 minutes later I was there and the doctor was still not ready. |
Patient-based
An overarching stressor of witnessing patient suffering – physical and emotional – was identified. Many shared stories of particularly salient cases that they had witnessed. The most frequently reported patient-based stressor expressed was interpreting for patients, young and old, who were declining. Participants explained that they frequently worked with severely ill patients and thus witness patients’ hopefulness turn into despair when they deliver the news about hospice care recommendations.
Interpreters reported that certain types of patients were particularly distressing or challenging to work with. Interpreters were disturbed by older patients were often alone and lonely. Many interpreters also expressed the difficulty of interpretations that involved young patients and their families. Interpreters were particularly stressed by socioeconomically vulnerable patients. Interpreters explained that their patients with poor health literacy are often naïve to how treatments work and when they have exhausted all possible treatment options. Interpreters also noted difficulties interpreting for patients who switched between English and their native language.
Interactions with the medical team
Interpreters shared the logistical challenges of serving as an intermediary between the doctor, patient, and families, including multiple doctors and caregivers talking at the same time and problematic physician behavior (e.g., talking for long periods, proceeding when patient doesn’t understand). Interpreters highlighted an incongruency between the amount of responsibility they carried compared to the amount of control they had in a clinical encounter. Sentiments of not feeling a part of the medical team were voiced; often interpreters expressed not feeling respected or perceived as medically trained.
Role challenges
Role challenges consisted of two areas: being a liaison between patients, families and providers and managing complex patient and family interactions. Bridging communication between the doctor, patient and family is challenging, for example, when a provider is unaware of a patient’s lack of understanding or response to information. Interpreters are cultural brokers and have to incorporate culturally-mediated meanings, as well as emotional expressions and tones, into their interpretations between clinicians and patients. Interpreters also have to manage complex family member dynamics, in particular when family members don’t want a patient to be told a diagnosis, want to speak English themselves or, relatedly, express that interpreters are not necessary.
Systems-based
Systems-based stressors included lack of interpreter resources and time as well as unpredictability of scheduling. Interpreters described common situations of being called, and expected by, multiple clinicians simultaneously. Interpreters were often frustrated juggling and accommodating physicians’ and nurses’ variable schedules.
Barriers and preferences for participation
Interpreters were interested in learning skills that were aligned with content in our resiliency training (i.e., stress awareness, relaxations skills). Barriers to participating included: 1) logistical issues (e.g., availability, scheduling), 2) concerns about group size and confidentiality, and 3) disinterest in a support-group. Thus, when recruiting interpreters for the trial we emphasized program preferences that interpreters had responded were important, including small group sizes, confidential exchanges, and skills-based (vs. a support group) learning. We offered sessions during weekend hours to try to accommodate weekday scheduling conflicts. Interpreters who wished to obtain CEUs for their National Board certification received CEU credits, from the International Medical Interpreters Association (IMIA), for participating in the resiliency training. Based on scheduling and logistical preferences, it was determined that the resiliency training program would be delivered in a format comprising one 4-hour session block.
Phase 2: Pilot Study
Program development
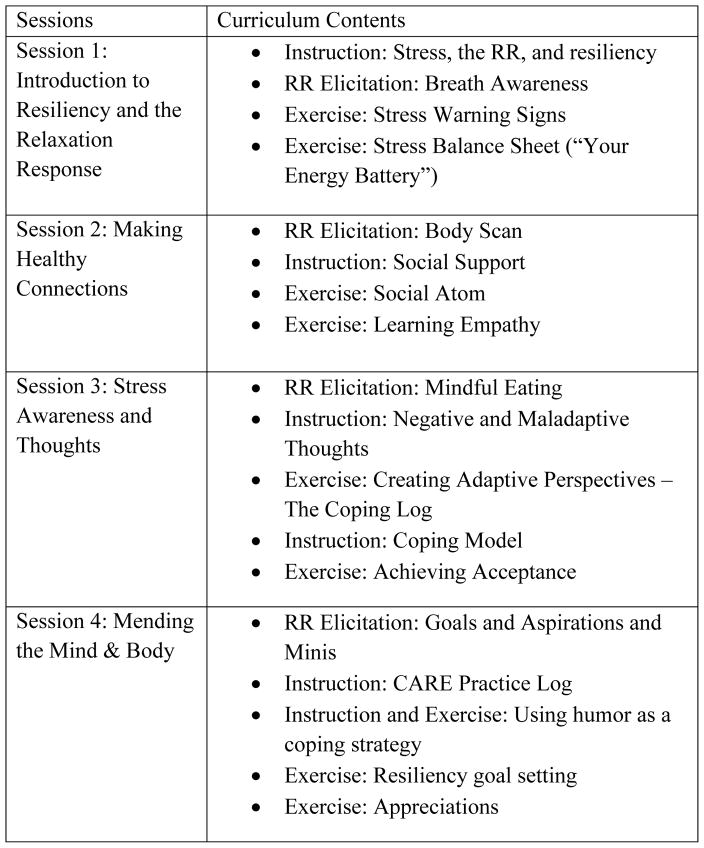
The Relaxation Response Resiliency Program (3RP) [28], is an 8-week group treatment to promote adaptation to stress and enhance resiliency. There are three essential components to the 3RP program: relaxation response (RR) elicitation, Stress Awareness, and Adaptive Strategies (Figure 1). The 3RP has been shown to be efficacious among palliative care clinicians in decreasing stress reactivity [29].
Figure 1.
3RP Theory
Using qualitative participants’ idioms/vernacular for stress, stress awareness examples, and work stressors experienced, we modified the 3RP into the Coping and Resiliency Enhancement (CARE) program for medical interpreters (Figure 2 in Appendix). The intervention program guide was developed at an 8th grade reading level. Qualitative findings were used to create case-based learning, including creating examples of stressful interpreter encounters to be used for interactive exercises. Given the need to consolidate the 3RP into a 4-session program, qualitative results guided the selection and content of CARE coping skill interactive exercises, including 1) selected RR elicitation techniques (breath awareness, mindful awareness), 2) restructuring negative thoughts (using a common example of thoughts of inadequacy (e.g., “I am not trained to handle this kind of conflict”) or isolation (i.e., “none of the clinicians are asking me for my impressions of this patient”), 3) stress awareness (awareness of how one’s stress directly affects interactions with patients), and 4) empathy (feelings of connectedness to a particular family).
Figure 2.
CARE PROGRAM OVERVIEW
Participants and Recruitment
Eligibility criteria and recruitment procedures were the same as in Phase 1.
Data Collection
Survey data were collected via REDCap (a secure, web-based application designed to support data capture for research studies) at baseline and 4-weeks post intervention.
Intervention Delivery
Five 4-hour CARE treatment groups were delivered (EP). Participants were given a CARE manual to write-in during the group. The program was delivered in one 4-hour block, each of which included an RR elicitation exercise, a didactic component, and interactive components (Figure 1). Participants were instructed to practice relaxation response elicitation techniques daily; a CD was given to facilitate this practice, and participants were encouraged to document their daily practice (type and duration) with a weekly practice note. Following treatment completion, the group leader called each participant to check in.
Measures
Sociodemographics
Sociodemographics included gender, age, country of origin, number of years living in the U.S., native language, marital status, level of education, and race/ethnicity. Work characteristics: Work characteristics included length of time working as an interpreter, languages in which interpretation services are provided, number of hours worked per week and number of cancer patients seen each week.
Environmental characteristics
Environmental characteristics included perceived support, respect and treatment at work, as measured by the 5-item Esteem Reward subscale of the Effort-Reward Imbalance Scale [30]. Responses are measured on a four point scale (1 = strongly agree to 4 = strongly disagree.); scores range from 5–20 with lower scores indicating a more favorable work environment.
Feasibility and Acceptability
Feasibility was measured by the proportion of interpreters who attended the training and completed the assessments. Acceptability was measured by the participants’ satisfaction with the program as indicated in a feedback questionnaire. Questions inquired about the amount of time sessions lasted, whether participants continued to practice the intervention techniques during follow-up, and interest in delivery modalities.
Efficacy outcome measures
Study outcomes included stress reactivity and coping (primary), perceived stress and burnout, and work-related stress.
Stress Reactivity and Coping
Measure of Current Status (MOCS-A)
The MOCS-A [31] is a 13-item self-report measure developed to assess participants’ current self-perceived status on several skills that are targeted by the CARE intervention, including the ability to relax at will, recognize stress-inducing situations, restructure maladaptive thoughts, be assertive about their needs, and choose appropriate coping responses. Statements are rated from 0 (I cannot do this at all) to 4 (I can do this extremely well). Scores range from 0–52; higher scores suggest better coping skills.
Perceived stress and burnout
Perceived Stress Scale (PSS-10)
The PSS-10 [32] is a 10-item scale designed to measure the degree to which situations in one’s life are appraised or considered stressful, and how unpredictable, uncontrollable, and overloaded respondents find their lives. Responses are measured on a five-point scale (0 = never, 1 = almost never, 2 =sometimes, 3 = fairly often, 4 = very often). Scores range from 0–40; high scores suggest a higher degree and longer duration of self-perceived stress.
Maslach Burn Out Inventory (MBI), Human Services Survey
The MBI-Human Services Survey [33] is a 22-item self-report instrument that measures three areas of job-related feelings. Questions are grouped into 3 subscales: Emotional Exhaustion, Depersonalization, and Personal Achievement. It is considered the standard for assessing burn out. Statements are rated as occurring “never” (0) to “every day” (6); range=0–52. Higher levels of burnout are indicated by higher scores on emotional exhaustion and depersonalization subscales, and by lower scores on personal achievement. We received permission from Mind Garden, Inc. to reproduce this scale for the purposes of use in this study.
Work-related stress measures
Job Satisfaction
For the interpreter pilot trial we modified scale items from the 2006 MGH staff survey to capture job satisfaction levels of interpreters; Dr. Donelan created this survey and modifications were made to this scale with input from DF/HCC interpreter directors. The result was a 10-item scale evaluating satisfaction with aspects of one’s job (job on the whole, interactions with patients, recognition received, working relationship with doctors and nurses and support staff, opportunity to learn new skills, support from supervisors, and understanding of role in the patient care team). Responses are measured on a five-point scale (1 = Very Dissatisfied to 5 = Very Satisfied); higher scores indicate greater job satisfaction.
Sick days
A single self-report indicates days taken off of work during the previous 12 weeks, due to feeling sick or stressed.
Analysis
Standard univariate statistics were used to describe the sample. Efficacy was assessed as changes in outcomes scores subsequent to completion of the CARE program as assessed at a 4-week follow-up. Significance of change in the outcome measures was evaluated based on the non-parametric Wilcoxon signed rank test using conservative (p<0.05) and liberal (p<0.10) critical values. Strength of effect was evaluated using Cohen’s d. For the few cases having missing data, mean substitution was used. Analyses were conducted with SPSS version 22.0. Feasibility was assessed with reference to the percentage of interpreters completing the assessments. Acceptability was evaluated from participant satisfaction feedback questions at 4 week follow-up.
Results
A total of 29 medical interpreters enrolled in the resiliency training program; 26 participants completed the 4-week follow-up survey (90% response rate).
Baseline Characteristics (Table 2)
Table 2.
Baseline Characteristics of CARE participants (n=26)
| Female Gender (%) | 69.0 |
| Age (M, SD) | 47.4 (11.0) |
| Country of Origin (%) | |
| Born in the U.S. | 15.0 |
| Born Outside the U.S. | 85.0 |
| Native Language (%) | |
| Spanish | 53.8 |
| English | 19.2 |
| Other | 27.0 |
| Marital Status (%) | |
| Married | 65 |
| Divorced/Separated | 11.5 |
| Never Married | 11.5 |
| Other | 11.5 |
| Education (%) | |
| Less than some college | 11.5 |
| College Degree | 50.0 |
| Graduate Degree | 38.5 |
| Race/Ethnicity (%) | |
| Asian | 11.5 |
| White, non-Hispanic | 30.8 |
| Hispanic | 53.8 |
| Other | 3.8 |
| Years as an Interpreter (M,SD) | 11.4 (9.5) |
| Spanish Language Interpretation (%) | 61.5 |
| Hours worked per week (M, SD) | 32.9 (10.3) |
| Cancer Patients seen per week (M,SD) | 6.1 (4.3) |
| Environmental Characteristics (M,SD) | 9.07 (2.5) |
A majority of the medical interpreters participating in the training were female (69%), and had at least a college degree (88%). 85% of the participants were born outside of the US; and those individuals had lived in the U.S. for an average of 20 years. Half were Hispanic (54%), and more than half provided interpreter services in the Spanish language (62%). Participants had worked as medical interpreters for an average of 11 years, worked for an average of 33 hours per week, and provided medical interpreting services for an average of six cancer patients weekly; each participant interpreted for cancer patients on a weekly basis. Participants’ environmental characteristics scores on the Esteem Reward subscale of the Effort-Reward Imbalance Scale were an average rating of 9, indicating a generally favorable work environment.
Feasibility and Acceptability
At 4-week follow-up, participants were asked about their CARE experiences. All participants indicated that they were comfortable during the group. 77% (n=20) of participants felt the program was the right length, while 15% (n=4) felt it was too short. Participants also reported that they continued to utilize the exercises they learned in the intervention; 62% of participants reported practicing relaxation a few times a week or daily. The use of media tools (i.e., CDs) also allowed the participants to create space and time for the exercises when it best fit their schedule.
Efficacy (Table 3)
Table 3.
CARE Outcomes
| Range: Pre | Range: Post | Pre-Mean | Pre-SD | Post-Mean | Post-SD | Difference | z score* | P value for difference | Cohen’s d | |
|---|---|---|---|---|---|---|---|---|---|---|
| Job satisfaction | 1.1–5.0 | 3.5–5.0 | 4.11 | 0.99 | 4.50 | 0.44 | 0.39 | 2.31 | 0.02 | .41 |
| PSS-10 | 5–23 | 1–30 | 13.73 | 5.66 | 12.62 | 6.56 | −1.11 | 0.92 | 0.36 | .17 |
| MBI: Emotional exhaustion | 1–51 | 1–40 | 15.79 | 12.15 | 14.12 | 10.8 | −1.67 | 1.27 | 0.20 | 0.33 |
| MBI: Depersonalization | 0–18 | 0–14 | 4.13 | 4.79 | 3.44 | 3.59 | −0.69 | 0.93 | 0.35 | 0.19 |
| MBI: Personal accomplishment | 11–47 | 2–47 | 36.58 | 8.02 | 35.96 | 10.01 | −0.62 | 0.10 | 0.92 | 0.43 |
| MOCS: Assertive | 1–5 | 2–5 | 3.37 | 0.97 | 3.59 | 0.98 | 0.22 | 1.63 | 0.10 | .30 |
| MOCS: Awareness | 1.67–4 | 2.0–4.67 | 3.13 | 0.69 | 3.26 | 0.68 | 0.13 | 1.08 | 0.28 | .23 |
| MOCS: Relax | 1–4 | 1.5–4.5 | 2.63 | 0.86 | 2.90 | 0.87 | 0.27 | 1.67 | 0.10 | .35 |
| MOCS: Coping | 2–4 | 2–4.2 | 3.24 | 0.72 | 3.28 | 0.67 | 0.04 | 0.56 | 0.58 | .08 |
| MOCS-A Total | 24–52 | 29–56 | 40.96 | 8.45 | 42.77 | 8.21 | 1.81 | 1.53 | 0.13 | .33 |
| Sick Days | 0–7 | 0–9 | 1.76 | 1.88 | 1.31 | 1.98 | −0.45 | 1.75 | 0.08 | .38 |
Job Satisfaction Mean on 10 Items scored 1–5, higher= greater job satisfaction.
PSS range=0–40; higher =greater perceived stress.
MBI Emotional Exhaustion range 0–54; lower= less emotional exhaustion.
MBI Depersonalization range 0–30; lower= less depersonalization.
MBI: Personal accomplishment range 0–48; higher= greater sense of accomplishment.
MOCS: Assertive Mean on 3 items scored 1–5, higher= more assertive.
MOCS: Awareness Mean on 3 items scored 1–5, higher= more aware.
MOCS: Relax Mean on 2 items scored 1–5, higher= more able to relax.
MOCS: Mean on 5 items scored 1–5, higher= better coping.
MOCS-A Total: Sum score on 13 items, higher is better.
At enrollment, perceived stress was rated relatively low (mean 13.73, sd=5.66). Four week follow-up indicated measurable improvements in job satisfaction (p=0.02; Cohen’s d=0.41). Improvements were also observed in stress reactivity (MOCS-A (Measure of Current Status); specifically, participants reported feeling more assertive about their needs (p=0.10; Cohen’s d=0.30), and more able to relax at will (p=0.10; Cohen’s d=0.35)—important mechanisms by which training can result in lower levels of distress. Sick days declined at four weeks post-training compared to baseline (p=0.08; Cohen’s d=0.38). Post-training scores on perceived stress (PSS-10) and burnout (MBI) were not significantly different from baseline.
Conclusion
To address an unmet need for psychosocial support for medical interpreters working with cancer patients, we developed a resiliency training program, targeted to the needs of medical interpreters. To date, there has been a paucity of research examining interpreter work stress, and no programs have been developed to address the psychosocial needs of interpreters working with cancer patients. Previous research has shown that oncology healthcare providers experience significant work-specific stress. The high demands and pressures of caring for oncology patients affect providers’ mental and physical health, which in turn result in negative impacts including medical errors, work dissatisfaction, and provider turnover as well as increased sick days from work [22,23]. In the case of interpreters, the quality of their work, for example the accuracy of their interpretations, can suffer. Yet these effects have not been explored among interpreters working with oncology patients.
Pilot findings suggest that this targeted resiliency program was accessible, in terms of readability and appeal, feasible to administer and evaluate, and valuable for participants. After completion of this resiliency program, interpreters reported improvements in their ability to cope with stress— in particular, to relax and assert themselves as needed. Improvements in work-related variables were also documented, including improvements in interpreters’ satisfaction with their work and a decrease in the number of sick days taken. These improvements are meaningful given that clinician wellness has been found to enhance the quality of patient care, such as enhancing providers’ empathy, [34] and that clinician job satisfaction can positively influence patients’ treatment and disease management [35].
In the development phase of this project, we identified areas of interpreter stress and integrated this information into the resiliency program’s didactic and interactive content. Overarching themes of effects of witnessing patient suffering and interpreting for “sad” patients and difficult requests, as well as complex patient-family dynamics were heard. Interpreters expressed frustrations with their intermediary role, unclear identity, and low position within the medical team’s hierarchy. Lastly, pragmatic system logistics added burdens. Qualitative findings also highlighted stressors related to interpreters’ interactions with oncology team members. These data were incorporated into interactive exercises (e.g., stressor examples specific to oncology clinician communication challenges) and findings were shared with interpreter directors of the participating institutions, which may be helpful in guiding clinician training to enhance their communication with interpreters.
However, despite these stressors and challenges, interpreters’ endorsed levels of perceived stress and burnout were relatively low, which could explain the lack of improvements seen in levels of perceived stress and the negative indicators of burnout. Indeed, interpreters’ levels of perceived stress were on par with population norms[36], and lower than that reported by oncology providers [37]. Despite exposure to these many work-related stressors, interpreters in this study did not appear to be burned out. As with stress, scores on the Emotional Exhaustion and Depersonalization subscales of the MBI were lower than those reported by oncology employees in another study of burnout [21]. In fact, interpreters’ MBI scores indicated high levels of personal accomplishment, on par with published norms of physicians and nurses [38]. Additionally, there is the possibility that the stressors faced by interpreters may be distressing in the moment, but that this stress was not captured by our outcomes which assessed more chronic and persistent stress. Qualitative data suggested that interpreters have numerous meaningful experiences in their work, in which they glean a sense of fulfillment and altruism, which are factors of resiliency [39] that may buffer the stress encountered. In addition, participants scored their work environments favorably and worked in well resourced academic institutions, with support systems in place. Correspondingly, interpreters reported a high degree of emotional support and availability among their peers and the managers who oversee their work.
In contrast, and supporting the need for a resiliency program, interpreters endorsed low skill acquisition for coping with these stressors. Interpreters completed the MOCS-A at study enrollment. When comparing interpreters’ MOCS-A baseline subscale scores on Assertiveness, Awareness, Relaxation, and Coping to a group of nonmetastatic breast cancer patients [40], interpreters endorsed lower levels of stress coping skills.
This pilot work was successful across three academic centers but there are limitations of note. Specifically, the program was 1) delivered in one session, which precluded repeated practice and processing of skill acquisition, 2) available only to interpreters who could commit to a 4-hour work block or weekend block, and 3) conducted only with medical interpreters who were highly educated, very experienced, and were from academic institutions with copious resources and peer support. The small sample size precluded us from drawing meaningful conclusions about the effect of baseline sociodemographic and work characteristics on the outcome measures.
In summary, we developed a program that was feasible to deliver and acceptable to interpreters, improved interpreters’ perceptions of their work, and improved interpreters’ ability to cope. Despite high work demands, interpreters found their work meaningful, but they lacked skills needed to cope with multifaceted stressors. A resiliency program, targeted to the needs of interpreters, could promote needed skills development, particularly among practicing interpreters. This program could be offered as ongoing training, and, specifically, for continuing education training credit for “certified” interpreters. The interactive nature of the program and skills acquisition would allow practicing interpreters to focus on their own commonly experienced interpretation based stressors. Future programs should be delivered in a group-based format and be offered at convenient times with sessions delivered over multiple weeks.
Acknowledgments
Sources of Support: The study was funded by NIH/NCI 5U54CA156732-02
Katia Canenguez, Karen Burns-White, DF/HCC interpreter directors: Yilu Ma, Laura Nakazawa, and Anabela Nunes. We are grateful to the interpreters who participated in the pilot.
References
- 1.Batalova J, Whatley M. Limited English Proficient Population of the United States. [Accessed: 23-Dec-2014];migrationpolicy.org. [Online]. Available: http://www.migrationpolicy.org/article/limited-english-proficient-population-united-states.
- 2.U. S. Census Bureau. [Accessed: 06-Aug-2014];2010 American Community Survey. 2010 [Online]. Available: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_1YR_DP02&prodType=table.
- 3.Cancer Statistics. National Cancer Institute; [Accessed: 08-Jul-2015]. [Online]. Available: http://www.cancer.gov/about-cancer/what-is-cancer/statistics. [Google Scholar]
- 4.Epstein RM, Street RL., Jr . Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. National Cancer Institute; Bethesda, MD: 2007. NIH Publication No. 07-6225. [Google Scholar]
- 5.Arora NK, McHorney CA. Patient preferences for medical decision making: Who really wants to participate? Medical care. 2000;38:335–341. doi: 10.1097/00005650-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Medical care research and review: MCRR. 2005;62:255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 7.Schapira L, Vargas E, Hidalgo R, et al. Lost in translation: integrating medical interpreters into the multidisciplinary team. The oncologist. 2008;13:586–592. doi: 10.1634/theoncologist.2008-0042. [DOI] [PubMed] [Google Scholar]
- 8.Johnson-Kozlow M, Roussos S, Rovniak L, Hovell M. Colorectal cancer test use among Californians of Mexican origin: influence of language barriers. Ethn Dis. 2009;19:315–322. [PMC free article] [PubMed] [Google Scholar]
- 9.Karliner LS, Ma L, Hofmann M, Kerlikowske K. Language barriers, location of care, and delays in follow-up of abnormal mammograms. Med Care. 2012;50:171–178. doi: 10.1097/MLR.0b013e31822dcf2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nguyen GT, Shungu NP, Niederdeppe J, et al. Cancer-related information seeking and scanning behavior of older Vietnamese immigrants. Journal of health communication. 2010;15:754–768. doi: 10.1080/10810730.2010.514034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butow P, Bell M, Goldstein D, et al. Grappling with cultural differences; Communication between oncologists and immigrant cancer patients with and without interpreters. Patient Education and Counseling. 2011;84:398–405. doi: 10.1016/j.pec.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 12.Ayanian JZ, Zaslavsky AM, Guadagnoli E, et al. Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. 2005;23:6576–6586. doi: 10.1200/JCO.2005.06.102. [DOI] [PubMed] [Google Scholar]
- 13.Karliner LS, Hwang ES, Nickleach D, Kaplan CP. Language barriers and patient-centered breast cancer care. Patient education and counseling. 2011;84:223–228. doi: 10.1016/j.pec.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Gany FM, Gonzalez CJ, Basu G, et al. Reducing clinical errors in cancer education: Interpreter training. Journal of Cancer Education. 2010;25:560–564. doi: 10.1007/s13187-010-0107-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do Professional Interpreters Improve Clinical Care for Patients with Limited English Proficiency? A Systematic Review of the Literature. Health services research. 2007;42:727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graham EA, Jacobs TA, Kwan-Gett TS, Cover J. Health services utilization by low-income limited English proficient adults. Journal of Immigrant and Minority Health. 2008;10:207–217. doi: 10.1007/s10903-007-9069-3. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs EA, Shepard DS, Suaya JA, Stone E-L. Overcoming Language Barriers in Health Care: Costs and Benefits of Interpreter Services. Am J Public Health. 2004;94:866–869. doi: 10.2105/ajph.94.5.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of Interpreter Services on Delivery of Health Care to Limited–English-proficient Patients. Journal of General Internal Medicine. 2001;16:468–474. doi: 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eelen S, Bauwens S, Baillon C, Distelmans W, Jacobs E, Verzelen A. The prevalence of burnout among oncology professionals: oncologists are at risk of developing burnout. Psycho-Oncology. 2014 doi: 10.1002/pon.3579. [DOI] [PubMed] [Google Scholar]
- 20.Trufelli DC, Bensi CG, Garcia JB, et al. Burnout in cancer professionals: a systematic review and meta-analysis. European journal of cancer care. 2008;17:524–531. doi: 10.1111/j.1365-2354.2008.00927.x. [DOI] [PubMed] [Google Scholar]
- 21.Demirci S, Yildirim YK, Ozsaran Z, Uslu R, Yalman D, Aras AB. Evaluation of burnout syndrome in oncology employees. Medical Oncology. 2010;27:968–974. doi: 10.1007/s12032-009-9318-5. [DOI] [PubMed] [Google Scholar]
- 22.Barrett L, Yates P. Oncology/haematology nurses: a study of job satisfaction, burnout, and intention to leave the specialty. Australian Health Review. 2002;25:109–121. doi: 10.1071/ah020109. [DOI] [PubMed] [Google Scholar]
- 23.Grunfeld E, Whelan TJ, Zitzelsberger L, Willan AR, Montesanto B, Evans WK. Cancer care workers in Ontario: prevalence of burnout, job stress and job satisfaction. Canadian Medical Association Journal. 2000;163:166–169. [PMC free article] [PubMed] [Google Scholar]
- 24.Donelan K, Hobrecker K, Schapira L, Mailhot JR, Goulart BH, Chabner BA. Medical interpreter knowledge of cancer and cancer clinical trials. Cancer. 2009;115:3283–3292. doi: 10.1002/cncr.24377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDowell L, Messias DKH, Estrada RD. The work of language interpretation in health care: complex, challenging, exhausting, and often invisible. Journal of transcultural nursing: official journal of the Transcultural Nursing Society/Transcultural Nursing Society. 2011;22:137–147. doi: 10.1177/1043659610395773. [DOI] [PubMed] [Google Scholar]
- 26.Butow PN, Lobb E, Jefford M, et al. A bridge between cultures: interpreters’ perspectives of consultations with migrant oncology patients. Supportive Care in Cancer. 2012;20:235–244. doi: 10.1007/s00520-010-1046-z. [DOI] [PubMed] [Google Scholar]
- 27.Arnsten AFT. Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009;10:410–422. doi: 10.1038/nrn2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park ER, Traeger L, Vranceanu A-M, et al. The Development of a Patient-Centered Program Based on the Relaxation Response: The Relaxation Response Resiliency Program (3RP) Psychosomatics. 2013;54:165–174. doi: 10.1016/j.psym.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 29.Mehta D, Chittenden E, Denninger J, et al. Promoting Resiliency Among Palliative Care Clinicians: A Pilot Intervention. J Pain Symptom Manage. 2015 Epub ahead of print. [Google Scholar]
- 30.Siegrist J. Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- 31.Carver CS. [Accessed: 25-Aug-2015];Measure of Current Status (MOCS) 2006 Available: http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html.
- 32.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 33.Maslach C, Jackson SE. The measurement of experienced burnout. J Organiz Behav. 1981;2:99–113. [Google Scholar]
- 34.Shanafelt TD, West C, Zhao X, et al. Relationship Between Increased Personal Well-Being and Enhanced Empathy Among Internal Medicine Residents. J Gen Intern Med. 2005;20:559–564. doi: 10.1111/j.1525-1497.2005.0108.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robin M, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychology. 1993;12:93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 36.Cohen S. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Thousand Oaks, CA, US: Sage Publications, Inc; 1988. pp. 31–67. The Claremont Symposium on Applied Social Psychology. [Google Scholar]
- 37.Traeger L, Park ER, Sporn N, et al. Development and evaluation of targeted psychological skills training for oncology nurses in managing stressful patient and family encounters. Oncol Nurs Forum. 2013;40:E327–336. doi: 10.1188/13.ONF.E327-E336. [DOI] [PubMed] [Google Scholar]
- 38.Schaufeli WB, Leiter MP. The Maslach Burnout Inventory-Test Manual. 1996. The Maslach burnout inventory-test manual. [Google Scholar]
- 39.Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neurosci. 2013:7. doi: 10.3389/fnbeh.2013.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Antoni MH, Lechner SC, Kazi A, et al. How stress management improves quality of life after treatment for breast cancer. Journal of consulting and clinical psychology. 2006;74:1143. doi: 10.1037/0022-006X.74.6.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]