Abstract
Irreducible shoulder dislocation is an uncommon event. When it does occur, blocks to reduction can include bone, labrum, rotator cuff musculature, or tendon. Concomitant rotator cuff tear at the time of initial dislocation is not an exclusive complication of anterior shoulder dislocation in the older population. Indeed, rotator cuff tear should not be excluded based solely on the patient's age. Rotator cuff interposition is not an uncommon complication after anterior dislocation of the shoulder. It should be suspected when there is incongruency of the joint and persistent subluxation on postreduction radiographs. If such incongruence or subluxation is seen, a computed tomographic (CT) or magnetic resonance imaging (MRI) scan must then be obtained to determine the nature of the interposed soft tissues. The key to treatment is early diagnosis and adequate imaging. Open reduction and repair of the rotator cuff should be performed. We present a technique for treating irreducible anterior shoulder dislocation caused by interposition of the subscapularis tendon. Both CT and MRI observations, along with intraoperative findings and surgical technique, are discussed.
Dislocation of the shoulder joint is a common presenting complaint in emergency departments, with anterior dislocation representing more than 95% of cases.1 Closed reduction of an acutely dislocated shoulder is usually successful, and failure of closed reduction is rare and usually due to a structural block within the joint.2 Mechanical blocks leading to successful reduction are many and can include bone,3 labrum, rotator cuff,4 or the long head of biceps tendon.5
Rotator cuff tear is not an exclusive complication of anterior shoulder dislocations in the older population. Indeed, rotator cuff tear should not be excluded based solely on the patient's age.6
Although many cases have been reported in the literature, the surgical techniques were not described clearly.7 We present technical notes on the treatment of an irreducible glenohumeral dislocation caused by interposition of the subscapularis tendon and posteriorly displaced biceps tendon.
Indication and Preoperative Evaluation
Many young patients present to the emergency department with an anterior shoulder dislocation, the prereduction plain radiograph showing anterior dislocation with avulsion fracture of the tuberosities (Fig 1). After closed reduction, however, the postreduction film shows the head of the humerus to be still subluxed (Fig 2), with the patient reporting significant pain and a limited range of abduction and flexion. In such cases, postreduction computed tomographic (CT) and magnetic resonance imaging (MRI) should be ordered to exclude the following: any bony block to complete reduction and persistent anterior-superior subluxation of the glenohumeral joint (Fig 3); complete tears of the subscapularis or rotator cuff tendons, which may be incarcerated into the glenohumeral joint and thus impeding reduction; or biceps tendon dislocation and incarceration into the glenohumeral joint (Figs 4 and 5).
Fig 1.
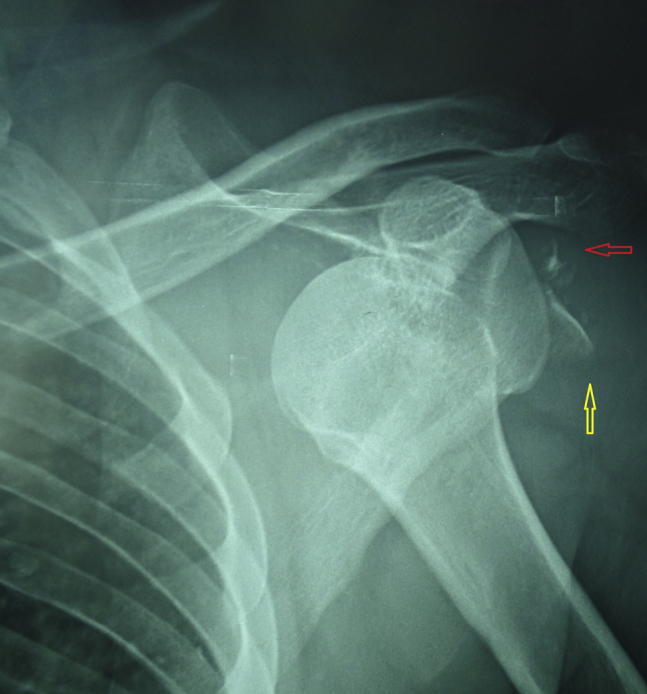
Prereduction plain radiograph: anteroposterior view of the left shoulder showing dislocated shoulder joint with avulsion fracture of tuberosities (red and yellow arrows).
Fig 2.
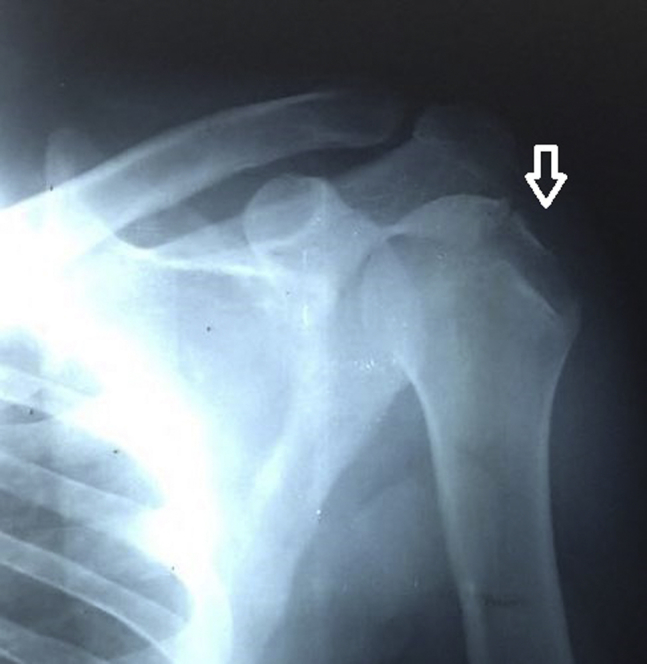
Initial postreduction plain radiograph: anteroposterior view of the left shoulder showing subluxed shoulder joint with avulsion fracture of the greater tuberosity (white arrow).
Fig 3.
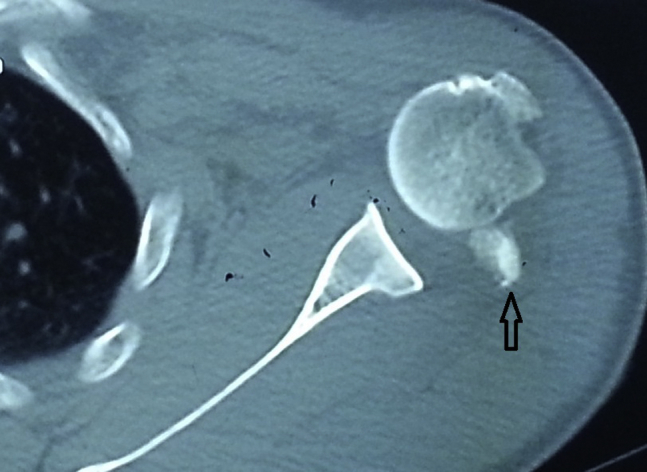
Axial computed tomographic scan of the left shoulder showing a persistent anterior subluxation of the humeral head with the lesser tuberosity lying behind it (black arrow).
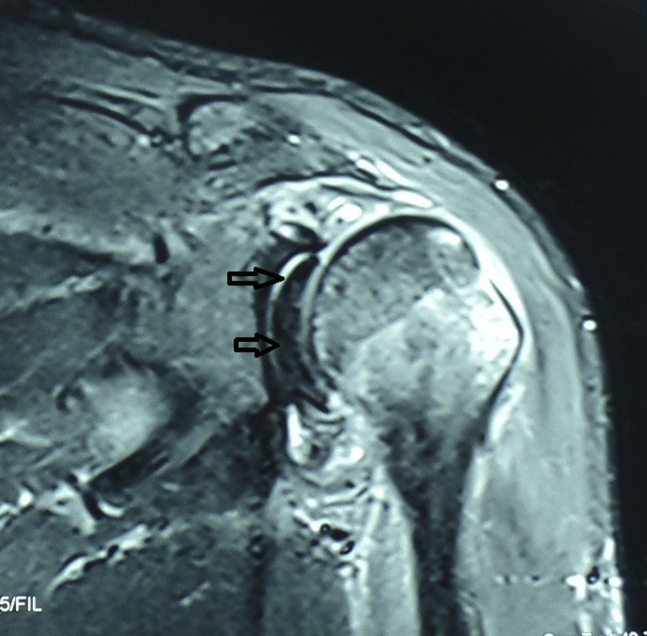
Fig 4.
Oblique coronal magnetic resonance image of the left shoulder shows an avulsion of the supraspinatus tendon (the 2 black arrows), which is draped over the superior labrum. The humeral head is subluxated superolaterally.
Fig 5.
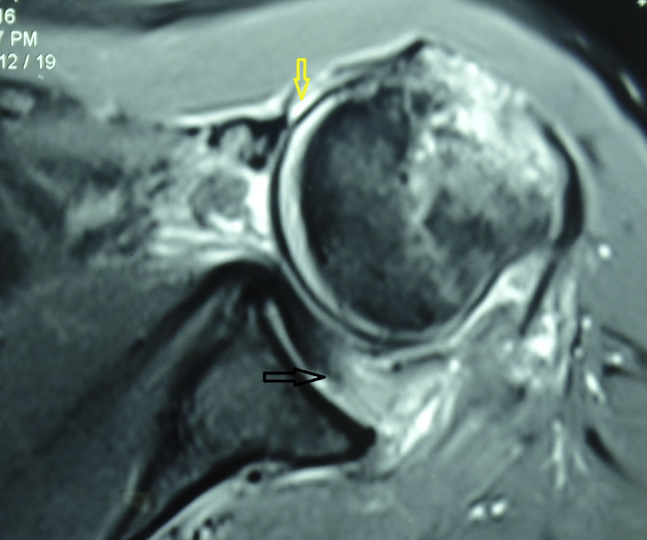
Axial magnetic resonance image of the left shoulder shows avulsion of the subscapularis tendon (black arrow) and its entrapment into the glenohumeral joint. In addition, there is interposition of the long head of the biceps tendon (yellow arrow).
Surgical Technique
This note focuses on the technique of delivery of incarcerated subscapularis tendon in cases of irreducible anterior shoulder dislocation.
Preoperative Setup
There is no role for arthroscopy in this technique as the joint space is occupied by the subscapularis tendon. In any trial for entering the joint, the arthroscope will need to pass through the tendon substance, and further attempts to improve the field of view by using a shaver will lead to injury of the cuff tendon itself.
Regarding anesthesia and preparation for the operation and the operating room setup, the same materials apply as with any regular open rotator cuff repair, with the patient in beach chair position.
Exposure
The shoulder is approached through the deltopectoral and deltoid splitting approaches to expose both the anterior shoulder joint and cuff tendon insertion. In this technique (Video 1), a skin incision is made to allow surgical access to the deltopectoral interval as well as for deltoid splitting (the upper end of skin incision is directed toward the anterolateral border of the acromion). During the skin incision, care should be taken to avoid cephalic vein injury as it is usually displaced very superficially by the dislocated head.
After skin and subcutaneous incisions, splitting the deltopectoral interval will reveal the traumatically exposed humeral head directly under the deltoid (as a result of rotator cuff tendon disruption), which usually tent the conjoined tendon medially. This closes the space to gain access to the glenoid (Fig 6).
Fig 6.
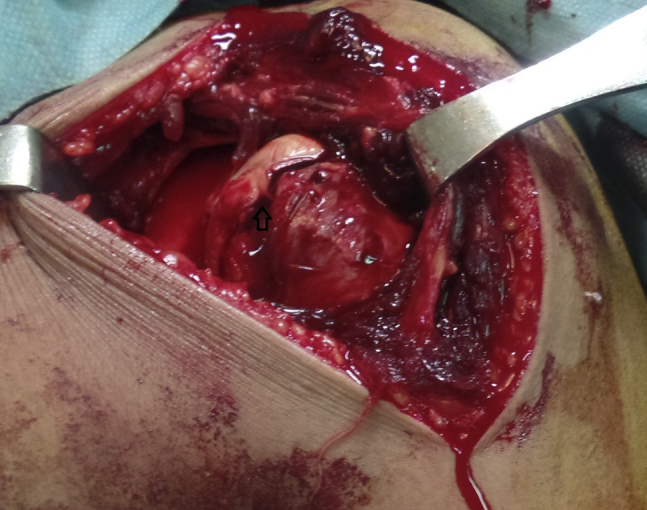
Beach chair position, left shoulder, showing the incision through the deltopectoral interval, which reveals the traumatically exposed humeral head.
Subscapularis Tendon Identification and Delivery
Just medial to the traumatically exposed humeral head, the subscapularis muscle firmly adheres to the glenoid surface, and its insertion is displaced posteriorly within the glenohumeral joint. To widen the joint space under the tented conjoined tendon, maximal external rotation and/or abduction is recommended to redislocate the subluxed humeral head to expose the incarcerated subscapularis tendon. At this point, No. 2 Ethibond stay suture (Ethicon/Johnson&Johnson, Cincinnati, OH) is applied to the subscapularis at its myotendinous junction to allow easy extraction of the tendon. Once extraction of the subscapularis tendon occurs, the joint can be reduced very easily (Fig 7).
Fig 7.
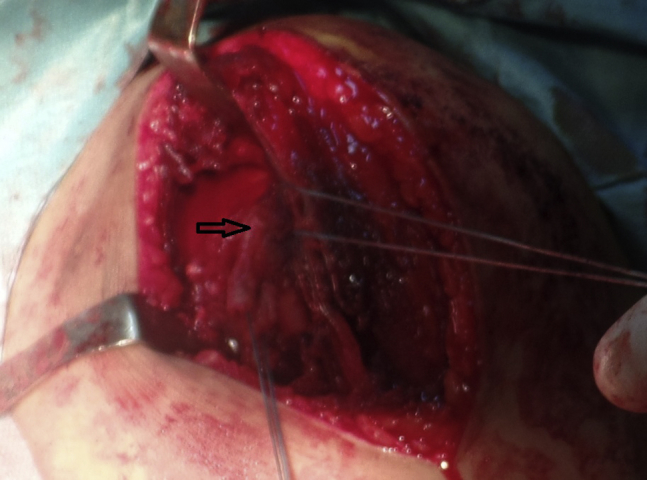
Beach chair position, left shoulder, showing the distal end of the subscapularis tendon (black arrow) held by 2 nonabsorbable sutures after its delivery from within the joint.
Recognition of Associated Tendon Entrapment and Injury
In most cases, the long head of the biceps is usually dislocated and entrapped inside the joint, adding to the difficulty of reduction, so it should be cut as high as possible. (Usually, cutting it at this step at the level of the glenoid is not possible.) Also, associated supraspinatus tendon avulsion may be found, and it has to be identified and repaired through the deltoid splitting approach.
After complete reduction and removal of any incarcerated bony or soft tissue, repair of the cuff tendons and tenodesis of the biceps can be carried out either with suture anchors or transosseous sutures in the regular manner (Figs 8 and 9). The reduction is assessed clinically by improvement in severe pain symptoms with passive shoulder movement in internal and external rotation, along with restoration of the acromiohumeral space in postoperative radiogaphs (Fig 10).
Fig 8.
Beach chair position, left shoulder, showing the biceps tendon tenotomy being tenodesed to the subscapularis tendon (black arrow).
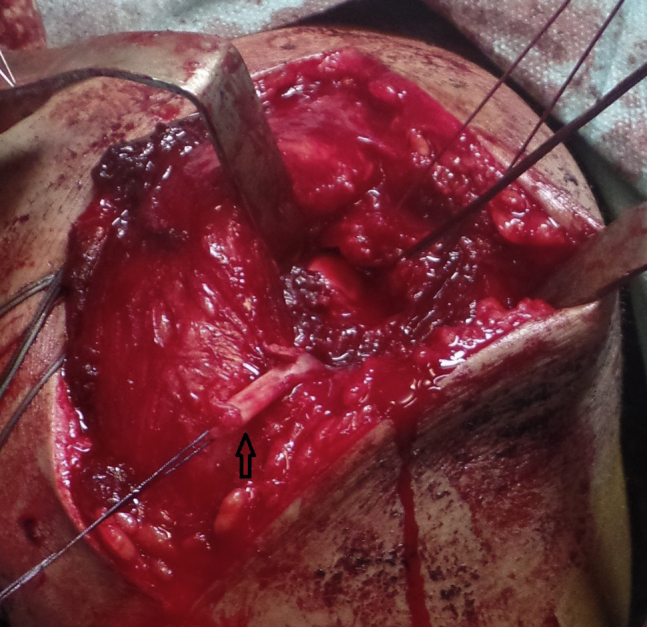
Fig 9.

Beach chair position, left shoulder, showing the subscapularis repaired to the trough on its lesser tuberosity (arrows).
Fig 10.

Postoperative radiograph of the left shoulder showing restoration of the acromiohumeral space with anchors fixing the cuff tendons.
The patient is managed in a sling for 6 weeks. During this time, pendular exercises as well as wrist and elbow exercises are allowed. Passive abduction is allowed at 4 weeks and active abduction at 12 weeks. At 3 months' follow-up, the patient will have a stable shoulder with abduction up to 60° and a functional range of flexion, extension, and rotation. Patients are allowed to return to sport when active abduction more than 110° with full flexion is observed.
Discussion
Shoulder dislocation is a common presenting complaint in the emergency department,6 with the incidence of first-time anterior dislocation ranging from 8 to 8.2 per 100,000 population/year, and the prevalence is about 2%.8 The consequences of shoulder dislocations in different age groups are well known to orthopedic surgeons.9 Rarely, however, is attention paid to the possibility of interposed soft tissue after shoulder dislocation.10
Closed reduction of an acutely dislocated shoulder is usually successful.5 And irreducibility of the acutely dislocated shoulder is rare, but well described.6 The reported causes of irreducible dislocation include bowstringing of the subscapularis or biceps tendon,7, 8 impaction of the greater tuberosity into a Hill-Sachs lesion,9 and interposition of a ruptured subscapularis in the glenoid rim.11
Rotator cuff tear is commonly associated with anterior shoulder dislocations, especially in older patients. In patients older than 40 years, they are present in up to 30%, and among those older than 60 years, up to 80% have rotator cuff tear. However, persistent subluxation due to cuff interposition is quite rare, and only a few operative reports of irreducible dislocation due to the subscapularis tendon have been described. Torn subscapularis can interpose between the glenoid and humeral head and prevent reduction.6
Preoperative evaluations with CT scans and MRI allow to detect these associated problems and aid the surgeon during the operation. Although CT identifies associated bone injuries and persistent joint subluxation, it fails to adequately image the associated soft tissue injury and possibly delays definitive management. MRI is a very useful adjunct in evaluating the shoulder post dislocation in any age group and is particularly useful for imaging the rotator cuff.8
There is no consensus regarding the gold standard imaging tool for diagnosis, the most suitable surgical approach, postoperative management, or probable complications.9 This Technical Note highlights the importance of CT and MRI after failure of reduction of anterior shoulder dislocation, especially if associated with any bony avulsion.
The key to treatment is early identification and management. These injuries initially may be misdiagnosed as brachial plexus neurapraxia or cuff contusions. Open reduction and repair of the rotator cuff is preferable to arthroscopic repair as the subscapularis tendon is entrapped within the joint, and any trial for improving the field of the arthroscope by using a shaver may lead to fraying of the tendon.
This note calls attention to the possibility of massive cuff tear in any age group and would help prevent misdiagnosis and mismanagement of this potentially devastating injury. When this injury is recognized and treated appropriately, good outcomes can be achieved. Table 1 shows the pearls and pitfalls of this technique.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Postreduction MRI in doubtful cases helps in excluding any soft tissue entrapment. | There is a possibility of injury of the cephalic vein by the scalpel due to the displaced humeral head. |
| The traumatically exposed humeral head in open technique indicates complete cuff tear. | It is difficult to completely evaluate labral injuries. |
| External rotation and abduction of the humeral head allow widening of the joint space to allow easy extraction of the entrapped tendon. | |
| Any methods of cuff repair can be used easily. |
MRI, magnetic resonance imaging.
The familiarity with a deltopectoral approach, the ability to address and repair any associated cuff tears, and the versatility of this technique in repairing the associated tears are considered its advantages; however, failure to completely address the associated labral tear and difficulty of biceps tenotomy near its labral attachment (no use for arthroscopy) are the limitations and disadvantages of this technique (Table 2).
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages and Limitation |
|---|---|
| The approach used is familiar. | Arthroscopy cannot be used. |
| Any associated cuff tear can be addressed. | There is a risk of injury to the cephalic vein. |
| Any technique of cuff repair can be easily used. | It is difficult to assess the subacromial space. |
It is important to carry out a meticulous clinical and radiologic evaluation prior to closed reduction of an anteriorly dislocated shoulder to assess any possible blocks to reduction. Manipulative reduction should be done with caution. When there is a case of difficult closed reduction, the possibility of interposition of soft tissues should be considered, especially in the absence of an obvious bony block to reduction, and surgical intervention may be required. The necessary equipment and skilled surgeons must be available to manage the patient properly.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Video of a cadaver left shoulder shows the steps discussed in the Technical Note. A deltopectoral approach is used, and after skin incision the traumatically exposed humeral head is seen pushing the cephalic vein more superficially. The subscapularis tendon entrapped within the joint can be seen hindering the reduction of the humeral head. By gentle traction on the tendon with maximal external rotation and abduction, the subscapularis tendon is dislodged from the joint and the humeral head easily reduced to the glenohumeral joint. Finally, the subscapularis and associated cuff tendon are repaired at the insertion.
References
- 1.Cutts S., Prempeh M., Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl. 2009;91:2–7. doi: 10.1308/003588409X359123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aiyenuro O.D., Zadeh H.G. Irreducible acute anterior shoulder dislocation due to rotator cuff tear and associated fracture of the greater tuberosity: A method of open reduction and rotator cuff repair. Inj Extra. 2007;38:74–77. [Google Scholar]
- 3.Mihata T., Doi M., Abe M. Irreducible acute anterior dislocation of the shoulder caused by interposed fragment of the anterior glenoid rim. J Orthop Sci. 2000;5:404–406. doi: 10.1007/pl00021457. [DOI] [PubMed] [Google Scholar]
- 4.Connolly S., Ritchie D., Sinopidis C., Brownson P., Aniq H. Irreducible anterior dislocation of the shoulder due to soft tissue interposition of subscapularis tendon. Skeletal Radiol. 2008;37:63–65. doi: 10.1007/s00256-007-0370-y. [DOI] [PubMed] [Google Scholar]
- 5.Day M.S., Epstein D.M., Young B.H., Jazrawi L.M. Irreducible anterior and posterior dislocation of the shoulder due to incarceration of the biceps tendon. Int J Shoulder Surg. 2010;4:83–85. doi: 10.4103/0973-6042.76970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gudena R., Iyengar K.P., Nadkarni J.B., Loh W. Irreducible shoulder dislocation: A word of caution. Orthop Traumatol Surg Res. 2011;97:451–453. doi: 10.1016/j.otsr.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Throckmorton T., Albright J. Case report: Concurrent anterior shoulder dislocation and rotator cuff tear in a young athlete. Iowa Orthop J. 2001;21:76–79. [PMC free article] [PubMed] [Google Scholar]
- 8.Khiami F., Gérometta A., Loriaut P. Management of recent first-time anterior shoulder dislocations. Orthop Traumatol Surg Res. 2015;101:51–57. doi: 10.1016/j.otsr.2014.06.027. [DOI] [PubMed] [Google Scholar]
- 9.Neviaser R., Neviaser T., Neviaser J. Concurrent rupture of the rotator cuff and anterior dislocation of the shoulder in the older patient. J Bone Joint Surg Am. 1988;70:1308–1311. [PubMed] [Google Scholar]
- 10.Miles Z.E., Gordon R.J., Wilkinson M.P.R. Irreducible traumatic anterior shoulder dislocation—A case report. Open J Orthop. 2012;2:51–55. [Google Scholar]
- 11.Amroodi M.N. Irreducible anterior shoulder dislocation associated with displaced fracture of the greater tuberosity: An analysis of seven cases. Shafa Ortho J. 2015;2:10–14. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video of a cadaver left shoulder shows the steps discussed in the Technical Note. A deltopectoral approach is used, and after skin incision the traumatically exposed humeral head is seen pushing the cephalic vein more superficially. The subscapularis tendon entrapped within the joint can be seen hindering the reduction of the humeral head. By gentle traction on the tendon with maximal external rotation and abduction, the subscapularis tendon is dislodged from the joint and the humeral head easily reduced to the glenohumeral joint. Finally, the subscapularis and associated cuff tendon are repaired at the insertion.