Abstract
Purpose
Breast cancer incidence and survival is high, which results in high prevalence of breast cancer survivors. The risk of (death from) cardiovascular disease (CVD) is higher in patients exposed to cardiotoxic treatments, in particular if they have pre-existing CVD risk factors. This study systematically summarized the risk of death from CVD following breast cancer.
Methods
Databases of Medline, Embase, and the Cochrane Library were systematically searched using the following terms and synonyms: breast cancer, cardiovascular disease, and cause of death. Articles reporting on both risk and risk factors of CVD mortality following breast cancer were eligible for inclusion. The methodological quality of each article was assessed using the Newcastle Ottawa quality assessment scale for cohort studies.
Results
Fourteen articles were included assessing the risk of CVD mortality among 1,217,910 women with breast cancer. The methodological quality was high for the majority of the studies. Studies were heterogeneous in design, study population, length of follow-up, CVD outcomes, and risk factors. 1.6–10.4% of all women with breast cancer died of CVD. Women with breast cancer had a higher risk of CVD mortality than women from the general population. The risk of CVD mortality was higher among women with breast cancer with older age at diagnosis, left-sided tumor, diagnosis in an earlier calendar period, and black ethnic origin.
Conclusions
CVD is an important cause of death following breast cancer. Identification of patients at high risk of CVD is important to optimize CVD prevention and tailor breast cancer treatment.
Keywords: Breast cancer, Cardiovascular disease, Absolute risk, Risk factors
Introduction
Breast cancer incidence has increased substantially over the last decades [1, 2], which, in combination with improved survival rates attributable to the availability of screening methods and effective treatments of early and more advance breast cancer [3, 4], leads to an increasing number of breast cancer survivors. Cardiovascular disease (CVD) is an important cause of death among these women as the risk of CVD may be increased by cardiotoxic treatments and CVD risk factors [5–8].
The risk of (death from) CVD following breast cancer is increased in women exposed to cardiotoxic treatments such as mediastinal and left-sided radiotherapy, anthracycline-based chemotherapy, and trastuzumab, and is even higher in patients with pre-existing CVD risk factors such as diabetes and hypertension [9–12]. With the current high breast cancer survival rates, especially for women with lower stages, and the large number of women with breast cancer receiving intensive treatment regimens, it is increasingly important to identify patients at high risk of CVD, and to balance the benefits of breast cancer treatment for achieving tumor control with the risks of cardiac toxicity inducing CVD.
As an overview of the available evidence on the risk of dying of CVD in women with breast cancer is currently lacking, we systematically reviewed the literature on the risk and risk factors of death from CVD following breast cancer.
Methods and materials
This systematic review was conducted in accordance with the Preferred Reporting Item for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13].
A systematic search was performed, and last updated on April 1, 2017, to identify all studies reporting on the risk and risk factors of death from CVD following breast cancer. Databases of Medline (via PubMed), Embase, and the Cochrane Library were systematically searched using the following terms and their synonyms in the search strategy: breast cancer, cardiovascular disease, and cause of death (Table 1). No limits were used.
Table 1.
Search strategy performed in Medline (via Pubmed)
| Search strategy (Medline via Pubmed) | |
|---|---|
| #1 | (Breast Neoplasms[Mesh Terms] OR cancer[Title/Abstract] OR cancers[Title/Abstract] OR carcinoma[Title/Abstract] OR carcinomas[Title/Abstract] OR tumor[Title/Abstract] OR tumors[Title/Abstract] OR tumor[Title/Abstract] OR tumors[Title/Abstract] OR malignancy[Title/Abstract] OR malignancies[Title/Abstract] OR neoplasm[Title/Abstract] OR neoplasms[Title/Abstract] OR neoplasms[Mesh Terms]) AND (breast[Title/Abstract] OR breasts[Title/Abstract] OR mamma[Title/Abstract] OR mamma*[Title/Abstract]) |
| #2 | (Cardiovascular Diseases[Mesh] OR heart[Title/Abstract] OR cardiac[Title/Abstract] OR cardio[Title/Abstract] OR cardiovascular[Title/Abstract] OR coronary[Title/Abstract] OR ventricular[Title/Abstract] OR valvular[Title/Abstract] OR circulatory[Title/Abstract]) AND (disease[Title/Abstract] OR diseases[Title/Abstract] OR complication[Title/Abstract] OR complications[Title/Abstract] OR failure[Title/Abstract] OR failures[Title/Abstract] OR dysfunction[Title/Abstract] OR dysfunctions[Title/Abstract] OR mortality[Title/Abstract] OR mortalities[Title/Abstract] OR death[Title/Abstract] OR deaths[Title/Abstract] OR arrhythmias[Title/Abstract] OR arrhythmia[Title/Abstract] OR cardiomyopathy[Title/Abstract] OR cardiomyopathies[Title/Abstract] OR Ischemia[Title/Abstract] OR Ischemia’s[Title/Abstract] OR all[Title/Abstract]) AND (cause[Title/Abstract] or causes[Title/Abstract] OR other[Title/Abstract]) |
| #3 | (Cause of death[Mesh Terms] OR mortality[Title/Abstract] OR mortalities[Title/Abstract] OR death[Title/Abstract] OR deaths[Title/Abstract] OR fatality[Title/Abstract] OR fatalities[Title/Abstract] OR dying[Title/Abstract]) |
| #4 | #1 AND #2 AND #3 |
Comparable search strategies have been conducted for Embase and the Cochrane Library
Articles reporting on both risk and risk factors of CVD mortality in breast cancer patients were eligible for inclusion. Articles with the following criteria were excluded: (1) published before 1990, (2) written in another language than English or Dutch, (3) case reports, reviews, or abstracts. Cross-referencing was performed.
Selection of studies and data extraction
After removal of duplicates, all titles and abstracts of the remained retrieved articles were screened. Abstracts that seemed potentially relevant, based on the in- and exclusion criteria, were screened for full text. The full text of these articles were assessed for eligibility by three investigators independently (S.A.M. Gernaat, P.J. Ho, and N. Rijnberg). Data were extracted using standardized data extraction forms and any disagreements were resolved by discussion. We extracted data on study size, characteristics of breast cancer patients (age, ethnic origin, year of diagnosis, years of follow-up), study design, International Classification of Diseases (ICD) codes for CVD mortality, absolute risk of death from CVD, absolute risk of death from breast cancer, absolute risk of death from any cause, statistical methods used to assess which factors increase the risk of death from CVD, and the risk of CVD mortality per risk factor.
Quality assessment
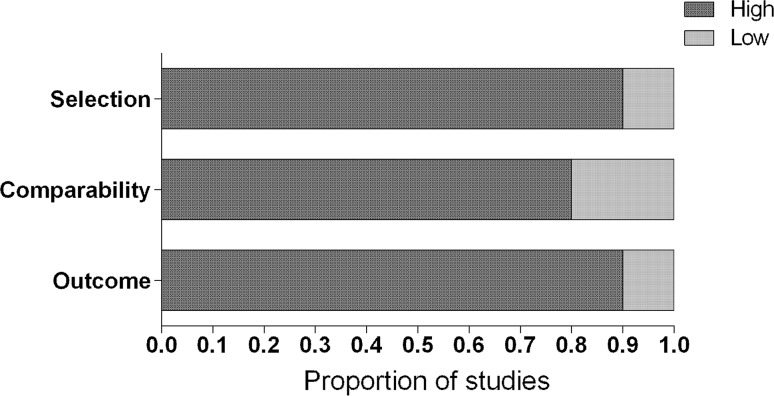
The methodological quality for each article was assessed by two authors independently (S.A.M. Gernaat and P.J. Ho) using the Newcastle Ottawa Quality Assessment Scale (NOS) for cohort studies [14]. The NOS consists of six multiple-choice questions that address subject selection, comparability, and the assessment of the outcome (i.e. CVD mortality), which sum up to a maximum score of seven. In the present study, a high score on one of these sections indicated that the maximum score (i.e. two for selection and comparability, and three for outcome) was achieved. In all other cases, the study received a low score on that particular section.
Results
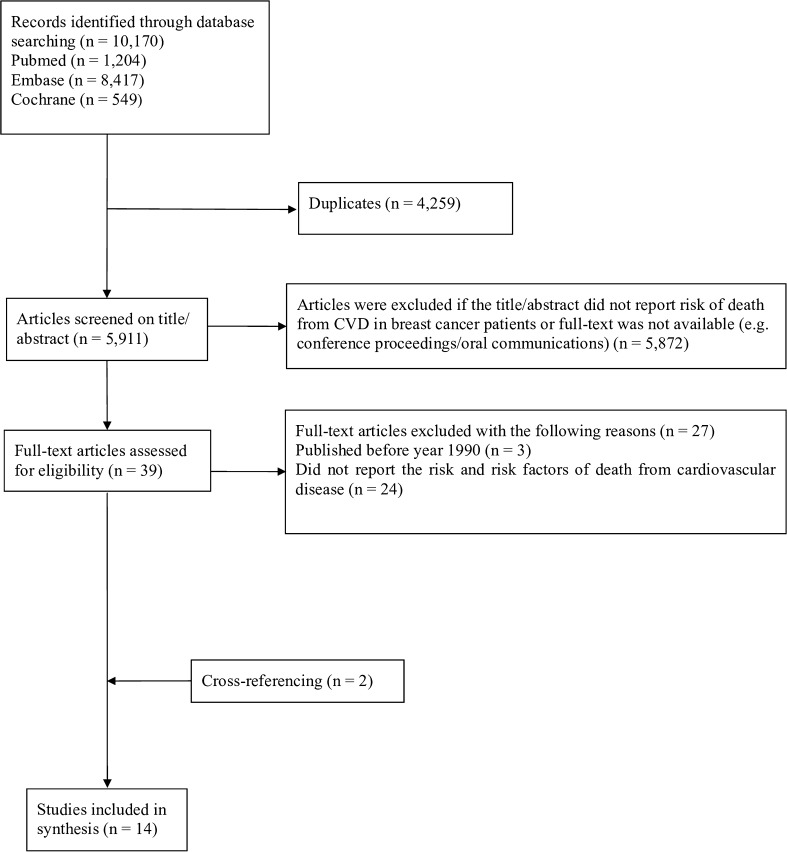
The systematic search yielded 10,170 citations including 5911 unique articles, which were screened for title and abstract using the predefined inclusion and exclusion criteria (Fig. 1). After screening the full text of 39 articles, 27 were excluded for the following reasons: published before the calendar year 1990 (n = 3) or articles that did not report the risk and risk factors of death from CVD (n = 24). Cross-referencing identified two additional papers. In total, 14 articles were included in the current systematic review, including 4,773,576 women of which 1,217,910 were diagnosed with breast cancer [5, 6, 8, 15–25].
Fig. 1.
Flowchart of the systematic review on the risk of death from cardiovascular disease in breast cancer patients
Quality assessment
The majority of the studies had the maximum score on the quality assessment for selection, comparability, and outcome [5, 8, 17, 18, 20–22, 26] (Fig. 2). The study by Nichols et al. [15] had a low score on selection as the study population was a selected group of in situ or invasive breast cancer patients and breast cancer ascertainment was by written self-report. The studies by Berkman et al. [6], Darby et al. [23], and Giordano et al. [24] had low scores on comparability as the hazard ratios (HRs) were not adjusted for factors other than age at diagnosis, the CVD mortality rates were unadjusted, and the HRs were only adjusted for other factors than age at diagnosis, respectively. The studies by Hooning et al. [25] and McCullough et al. [16] had low scores on the outcome attainment as the assessment of CVD deaths was by hospital records and subjects were lost to follow-up or the follow-up rate was less than 70%, respectively.
Fig. 2.
Quality assessment by the Newcastle Ottawa Quality Assessment Scale Selection was based on the representativeness of the breast cancer cohort and ascertainment of breast cancer. Comparability was based on the comparability of cohorts on the basis of the design or analysis. Outcome was based on the assessment of death from cardiovascular disease, on the length of follow-up (≥10 years), and adequacy of follow-up of the cohorts. A high score on one of these sections indicated that the maximum score on that particular section (i.e. two for selection and comparability, and three for outcome) was achieved. In all other cases, the study received a low score on that particular section
Cardiovascular disease mortality in breast cancer patients compared with the general population
Bradshaw et al. [8] included 1413 women with primary in situ or invasive breast cancer diagnosed in the United States (U.S.) between 1996 and 1997, and 1411 age-matched women from the general population (Table 2). Mean age at breast cancer diagnosis and reference date for women from the general population were 59 and 57 years, respectively. During the follow-up time, which ranged between 0.2 and 13.5 years for both groups, 9.4% of women with breast cancer and 7.4% of women from the general population died of CVD. After adjusting for age, menopausal status, and other CVD risk factors, women with breast cancer had a 1.9 (95% confidence interval (CI) = 1.4–2.7) times higher risk to die of CVD after at least 7 years post diagnosis than women from the general population (Table 3).
Table 2.
Characteristics and risk of cardiovascular disease mortality of the fourteen articles included in the systematic review
| First author, publication year, country | Type of breast cancer, number of patients | Age at diagnosis or reference date, y | Year of diagnosis, years of follow-up | ICD-9 and/or ICD-10 codes of CVD mortality outcomes | Percentage of deaths due to any cause, CVD, and BC (percentage of total) | |
|---|---|---|---|---|---|---|
| CVD mortality in breast cancer patients compared with the general population | ||||||
| Bradshaw, 2016, USa | Primary in situ or invasive; 1413 | 59 or 57d | 1996–1997, 13.5e | ICD-9: 394.9, 402.9, 410, 414.0, 427.5 | Women with BC | Women without BC |
| Any cause: 29.4 | Any cause: 17.2 | |||||
| ICD-10: I10, I11.9, I21.9, I25.1, I25.4, I46.9 | ||||||
| Without BC; 1411c | CVD: 9.4 BC: 9.6 |
CVD: 7.4 BC: 0.1 |
||||
| Riihimäki, 2012, Swedena | Primary invasive; 122,217 | – | 1987–2006, 19e | ICD-9: 410, 411–414, 420–427, 428, 430–438, 440–448 | Women with BC | Women without BC |
| Any cause: 39.3 | Any cause: 16.7 | |||||
| Women without BC; 3,554,255h | ||||||
| ICD-10: I20, I21–I22, I23–I25, I30–I50, I52, I60–I79 | CVD: 10.4 | CVD: 7.5 | ||||
| BC: 18.1 | BC: - | |||||
| CVD mortality in breast cancer patients by patient, tumor, and treatment characteristics | ||||||
| Colzani, 2011, Swedena | Primary invasive I-III; 12,850 | <75 | 1990–2006, 10e | ICD-9: 390–459 | Any cause: | 14.4 |
| ICD-10: I00–I99 | CVD: | 1.8 | ||||
| BC: | 9.2 | |||||
| Hooning, 2006, the Netherlandsf | Primary invasive I-IIIA; 7425 | ≤70 | 1970–1986, 13.8b | ICD-9: 410–459 | Any cause: | 56.0 |
| CVD: | 5.3 | |||||
| BC: | 42.6 | |||||
| CVD mortality in patients with left-sided breast cancer compared to right-sided breast cancer | ||||||
| Bouchardy, 2009, Switzerlanda | Primary invasive lymph node-negative; 1245 | 57.4d | 1980–2004, 7.7d | ICD-10: I00-I99 | Any cause: | 12.4 |
| CVD: | 2.2 | |||||
| BC: | 7.3 | |||||
| Darby, 2005, USa | Primary in situ or invasive; 308,861 | 20–79 | 1973–2001, 29e | ICD-9: 390–398, 402, 404, 410, 411–414, 415–429 | Any cause: | 29.5 |
| CVD: | 4.2 | |||||
| BC: | 16.8 | |||||
| Giordano, 2005, USa | Primary in situ or invasive; 24,785 | 56.9 ± 13.2d | 1973–1988, 9.3b | ICD-9: 410-414 | Any cause: | – |
| ICD-10: I20–I25 | CVD: | – | ||||
| BC: | – | |||||
| Haque, 2017, USa | DCIS, 140,914 | ≤60 & >60 | 1973–2002, 11.5 | – | Any cause: | – |
| (IQR: 6.8–15.1)b | CVD: | – | ||||
| BC: | – | |||||
| Merzenich, 2016, Germanyg | Primary in situ or invasive; 11,982 | 59d | 1998–2008, 6.5 (0–15)b | ICD-10: I20–I25, I34–I37, I44–I50 | Any cause: | 20.6 |
| (range: 18–101) | CVD: | 2.3 | ||||
| BC: | 10.2 | |||||
| CVD mortality in breast cancer patient with ethnic differences | ||||||
| Berkman, 2014, USa | Primary DCIS; 54,518 white women; 6113 black women | ≥40 | 1978–2010, 9.2b | ICD-10: I00–I09, I11, I13, I20–I51, I60–I69, I70, I72–178 | Any cause: | 18.0 |
| CVD: | 6.0 | |||||
| BC: | 1.5 | |||||
| Solanki, 2016, USa | Primary in situ or invasive I-III; 462,005 NHW; 44,531 API | NHW: 61.2 ± 13.7d | 1991–2011, | ICD-9: 390–459 | Non-Hispanic white | Asian and Pacific Islander |
| API: 56.3 ± 13.1d | NHW: 6.8 ± 4.9d, | Any cause: 23.8 | Any cause: 15.4 | |||
| 4 (2–6) b | CVD: 5.5 | CVD: 2.6 | ||||
| API: 6.7 ± 5.0d, | BC: 10.0 | BC: 8.2 | ||||
| 3 (2–5)b | ||||||
| CVD mortality in breast cancer patients by diet, body weight, and health behaviors | ||||||
| McCullough, 2016, Switzerlandg | Primary invasive I-III; 4452 for pre-diagnostic of which 2152 were included in the ≥1-year post- diagnostic analysis | 70.7 ± 7.2d | 1992–2011, pre-diagnostic diet assessment 9.8 ± 4.9, post-diagnostic analyses 9.9 ± 3.3d | ICD-9: 390-459 | Any cause: | 27.0 |
| ICD-10: I00-I99 | CVD: | 5.2 | ||||
| BC: | 8.9 | |||||
| Nichols, 2009, USa | Primary in situ or invasive; 5791 | 58.4 ± 10.0d | 1988–1999, 6.4 ± 1.2d | ICD-10: I00-99 | Any cause: | 7.3 |
| CVD: | 1.6 | |||||
| BC: | 2.1 | |||||
| Veal, 2017, USg | Primary DCIS; 1925 | 20–74 | 1997–2006, 6.7d | ICD-10: I00-I09, I11, I13, I20-I51, I60-I69, I70, I72-I78 | Any cause: | 10.2 |
| CVD: | 1.8 | |||||
| BC: | 4.5 | |||||
BC breast cancer, CVD cardiovascular disease, DCIS ductal carcinoma in situ, ICD-9 International Classification of Diseases version 9, ICD-10 International Classification of Diseases version 10, y years, US United States of America
aPopulation-based registry
bMedian with (range if described by the article)
cWomen without breast cancer were matched on age and the expected distribution of survivors in 5-year age groups with women with breast cancer
dMean with (±standard deviation if described by the article)
eMaximum
fHospital-based registry
gProspective cohort study
hAll women who were born before 1977 who resided in Sweden were included; women without breast cancer were part of the reference group
Table 3.
Risk factors of death from cardiovascular disease in women diagnosed with breast cancer
| First author, year of publication | Statistical analysis | Categories | Cause of death (outcome) | Risk of death HR (95% CI) | Covariates | ||
|---|---|---|---|---|---|---|---|
| CVD mortality in breast cancer patients compared with the general population | |||||||
| Bradshaw, 2016 | Competing risk | General population | CVD | 1.0 (ref) | Age, menopausal status, CVD risk factors | ||
| Breast cancer patients diagnosed 0–7 years ago | 0.59 (0.4–0.9) | ||||||
| General population | CVD | 1.00 (ref) | |||||
| Breast cancer patients diagnosed >7 years ago | 1.9 (1.4–2.7) | ||||||
| General population | CVD | 1.0 (ref) | |||||
| Breast cancer patients treated with RT | 1.1 (0.8–1.6) | ||||||
| General population | CVD | 1.0 (ref) | |||||
| Breast cancer patients treated without RT | 1.3 (0.9–2.0) | ||||||
| General population | CVD | 1.0 (ref) | |||||
| Breast cancer patients treated with CT | 1.4 (1.0–2.2) | ||||||
| General population | CVD | 1.0 (ref) | |||||
| Breast cancer patients treated without CT | 1.1 (0.8–1.5) | ||||||
| General population | CVD | 1.0 (ref) | |||||
| Breast cancer patients treated with HT | 1.2 (0.9–1.7) | ||||||
| General population | CVD | 1.0 (ref) | |||||
| Breast cancer patients treated without HT | 1.2 (0.8–1.8) | ||||||
| Riihimäki, 2012 | Cox proportional hazard | General population | CVA | 1.00 (ref) | Age, socioeconomic index, geographical region of residence | ||
| Breast cancer patients | 1.03 (1.00–1.07) | ||||||
| General population | AMI | 1.00 (ref) | |||||
| Breast cancer patients | 1.01 (0.98–1.0) | ||||||
| General population | Other CHD | 1.00 (ref) | |||||
| Breast cancer patients | 1.14 (1.10–1.19) | ||||||
| General population | Heart failure | 1.00 (ref) | |||||
| Breast cancer patients | 1.29 (1.22–1.37) | ||||||
| General population | Other heart disease | 1.00 (ref) | |||||
| Breast cancer patients | 1.24 (1.17–1.32) | ||||||
| General population | Arterial disease | 1.00 (ref) | |||||
| Breast cancer patients | 0.95 (0.89–1.02) | ||||||
| General population | Complications of CVD | 1.00 (ref) | |||||
| Breast cancer patients | 1.12 (0.99–1.2) | ||||||
| CVD mortality in breast cancer patients by patient, tumor, and treatment characteristics | |||||||
| Colzani, 2011 | Flexible parametric survival models | Age at diagnosis | <45 | CVD | 0.3 (0.0–2.5) | Clinical, tumor, treatment characteristics | |
| 45–54 | 1.00 (ref) | ||||||
| 55–64 | 6.5 (2.8–14.6) | ||||||
| 65–74 | 17.9 (8.0–39.7) | ||||||
| Calendar time at diagnosis | 1990–1994 | CVD | 2.1 (1.2–3.6) | ||||
| 1995–1999 | 1.6 (0.9–2.9) | ||||||
| 2000–2006 | 1.00 (ref) | ||||||
| Treatment | Surgery | CVD | 2.1 (1.2–3.8) | ||||
| Surgery + RT + HT | 1.00 (ref) | ||||||
| Surgery + RT | 1.4 (0.7–2.5) | ||||||
| Surgery + RT + CT | 0.6 (0.1–2.5) | ||||||
| Surgery + CT | 2.0 (0.6–6.8) | ||||||
| Surgery + RT + CT + HT | 0.7 (0.3–1.9) | ||||||
| Surgery + HT | 2.2 (1.5–3.2) | ||||||
| Surgery + CT + HT | 1.0 (0.2–4.5) | ||||||
| No. of positive lymph nodes | 0 | CVD | 1.00 (ref) | ||||
| 1–3 | 2.0 (1.4–2.9) | ||||||
| ≥4 | (1.0-3.4) | ||||||
| Estrogen receptor | Negative | CVD | 1.00 (ref) | ||||
| Status | Positive | 0.8 (0.5–1.3) | |||||
| Tumor size in mm | 1–20 | CVD | 1.00 (ref) | ||||
| >20 | 1.5 (1.1–2.1) | ||||||
| Hooning, 2006 | Cox proportional hazard | Total study population | Clinical, tumor, treatment, characteristics | ||||
| Age at diagnosis (continuous) | CVD | 1.12 (1.10–1.14) | |||||
| Treatment | Surgery | CVD | 1.00 (ref) | ||||
| Surgery + RT | 2.03 (1.33–3.10) | ||||||
| Surgery + RT + CT | 1.47 (0.81–2.67) | ||||||
| Surgery + RT + HT | 1.70 (0.99–2.93) | ||||||
| Calendar time at diagnosis | 1970–1975 | CVD | 1.34 (0.93–1.92) | ||||
| 1976–1980 | 1.54 (1.11–2.14) | ||||||
| 1981–86 | 1.00 (ref) | ||||||
| 10-year survivors | |||||||
| Age at diagnosis (continuous) | CVD | 1.11 (1.09–1.13) | |||||
| Treatment | Surgery | CVD | 1.00 (ref) | ||||
| Surgery + RT | 2.08 (1.25–3.47) | ||||||
| Surgery + RT + CT | 2.38 (1.18–4.77) | ||||||
| Surgery + RT + HT | 2.42 (1.27–4.61) | ||||||
| Calendar time at diagnosis | 1970–1975 | CVD | 1.38 (0.89–2.14) | ||||
| 1976–1980 | 1.62 (1.07–2.46) | ||||||
| 1981–1986 | 1.00 (ref) | ||||||
| CVD mortality in breast cancer patients by laterality of the tumor | |||||||
| Bouchardy, 2016 | Cox proportional hazard | RT and right-sided tumor | CVD | 1.00 (ref) | Clinical, tumor, and treatment characteristics | ||
| RT and left-sided tumor | 0.52 (0.24–1.12) | ||||||
| RT and outer quadrant | CVD | 1.00 (ref) | |||||
| RT and inner quadrant | 2.46 (1.13–5.37) | ||||||
| RT and right-sided tumor and outer quadrant | CVD | 1.00 (ref) | |||||
| RT and right-sided tumor and inner quadrant | 2.51 (0.88–7.18) | ||||||
| RT and left-sided tumor and outer quadrant | CVD | 1.00 (ref) | |||||
| RT and left-sided tumor and inner quadrant | 2.17 (0.65–7.25) | ||||||
| RT and outer quadrant and right-sided tumor | CVD | 1.00 (ref) | |||||
| RT and outer quadrant and left-sided tumor | 0.70 (0.21–2.32) | ||||||
| RT and inner quadrant and right-sided tumor | CVD | 1.00 (ref) | |||||
| RT and inner quadrant and left-sided tumor | 0.52 (0.18-1.48) | ||||||
| Darby, 2005 | Poisson regression for mortality rates | RT on right-sided tumor | CVD | 1.00 (ref) | No covariates | ||
| RT on left-sided tumor | 1.44 (1.26–1.65) | ||||||
| RT on right-sided tumor | AMI | 1.00 (ref) | |||||
| RT on left-sided tumor | 1.43 (1.10–1.87) | ||||||
| RT on right-sided tumor | Other | 1.00 (ref) | |||||
| Ischemic | |||||||
| CVD | |||||||
| RT on left-sided tumor | 1.60 (1.26–2.02) | ||||||
| RT on right-sided tumor and aged 20–49 years at diagnosis | CVD | 1.00 (ref) | |||||
| RT on left-sided tumor and aged 20–49 years at diagnosis | 1.54 (1.08–2.19) | ||||||
| RT on right-sided tumor and aged 50–59 years at diagnosis | CVD | 1.00 (ref) | |||||
| RT on left-sided tumor and aged 50–59 years at diagnosis | 1.53 (1.19–1.98) | ||||||
| RT on right-sided tumor and aged 60–69 years at diagnosis | CVD | 1.00 (ref) | |||||
| RT on left-sided tumor and aged 60–69 years at diagnosis | 1.40 (1.15–1.70) | ||||||
| RT on right-sided tumor and aged 70–79 years at diagnosis | CVD | 1.00 (ref) | |||||
| RT on left-sided tumor and aged 70–79 years at diagnosis | 1.28 (0.87–1.90) | ||||||
| RT on right-sided tumor and white ethnic origin | CVD | 1.00 (ref) | |||||
| RT on left-sided tumor and white ethnic origin | 1.39 (1.21–1.61) | ||||||
| RT on right-sided tumor and black ethnic origin | CVD | 1.00 (ref) | |||||
| RT on left-sided tumor and black ethnic origin | 2.25 (1.36–3.72) | ||||||
| RT on right-sided tumor and other/ unknown ethnic origin | CVD | 1.00 (ref) | |||||
| RT on left-sided tumor and other/ unknown ethnic origin | 1.30 (0.71–2.39) | ||||||
| Giordano, 2005 | Cox proportional hazard | Right-sided tumor and diagnosed in 1979 | CVD | 1.00 (ref) | No covariates | ||
| Left-sided tumor and diagnosed in 1979 | 1.50 (1.19–1.87) | ||||||
| Right-sided tumor and diagnosed in 1988 | CVD | 1.00 (ref) | |||||
| Left-sided tumor and diagnosed in 1988 | 0.79 (0.52–1.18) | ||||||
| Haque, 2016 | Cox proportional hazard | Diagnosed 1973–1982 | Clinical, tumor, treatment characteristics | ||||
| Right-sided tumor | CVD | 1.00 (ref) | |||||
| Left-sided tumor | 1.30 (1.18–1.42) | ||||||
| Race | White | CVD | 1.00 (ref) | ||||
| African American | 1.14 (0.94–1.36) | ||||||
| American Indian/ | 0.83 (0.66–1.02) | ||||||
| Asian/ Pacific | |||||||
| Islander | |||||||
| Unspecified | 0.47 (0.03–2.06) | ||||||
| Age at diagnosis | ≤60 | CVD | 1.00 (ref) | ||||
| >60 | 5.87 (5.30–6.50) | ||||||
| Marital status | Married | CVD | 1.00 (ref) | ||||
| Unmarried | 1.87 (1.70–2.05) | ||||||
| Unknown | 1.77 (1.29–2.37) | ||||||
| Right-sided tumor and <10 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and <10 years since diagnosis | 1.14 (0.99–1.32) | ||||||
| Right-sided tumor and 10–19 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and 10–19 years since diagnosis | 1.32 (1.12–1.57) | ||||||
| Right-sided tumor and ≥20 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and ≥20 years since diagnosis | 1.30 (1.10–1.54) | ||||||
| Region | Pacific | CVD | 1.00 (ref) | ||||
| Alaska | – | ||||||
| East | 0.97 (0.86-1.09) | ||||||
| Northern Plains | 1.35 (1.21-1.51) | ||||||
| Southwest | 1.51 (0.98-1.34) | ||||||
| Diagnosed 1983–1992 | |||||||
| Right-sided tumor | CVD | 1.00 (ref) | |||||
| Left-sided tumor | 1.02 (0.95–1.10) | ||||||
| Race | White | CVD | 1.00 (ref) | ||||
| African American | 1.14 (0.98–1.32) | ||||||
| American Indian/ | 0.68 (0.56–0.82) | ||||||
| Asian/ Pacific | |||||||
| Islander | |||||||
| Unspecified | 0.39 (0.02–1.74) | ||||||
| Age at diagnosis | ≤60 | CVD | 1.00 (ref) | ||||
| >60 | 10.16 (9.62–11.30) | ||||||
| Marital status | Married | CVD | 1.00 (ref) | ||||
| Unmarried | 2.25 (2.08–2.42) | ||||||
| Unknown | 1.65 (1.28–2.08) | ||||||
| Right-sided tumor and <10 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and <10 years since diagnosis | 1.01 (0.90–1.13) | ||||||
| Right-sided tumor and 10–19 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and 10–19 years since diagnosis | 0.98 (0.88–1.10) | ||||||
| Right-sided tumor and ≥ 20 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and ≥20 years since diagnosis | 0.94 (0.77–1.15) | ||||||
| Region | Pacific | CVD | 1.00 (ref) | ||||
| Alaska | 0.00 (0.00–14.13) | ||||||
| East | 1.09 (0.99–1.20) | ||||||
| Northern Plains | 1.42 (1.30–1.56) | ||||||
| Southwest | 1.13 (0.97–1.30) | ||||||
| Diagnosed 1993–1902 | |||||||
| Right-sided tumor | CVD | 1.00 (ref) | |||||
| Left-sided tumor | 0.99 (0.93–1.05) | ||||||
| Race | White | CVD | 1.00 (ref) | ||||
| African American | 1.32 (1.20–1.45) | ||||||
| American Indian/ | 0.53 (0.46–0.61) | ||||||
| Asian/ Pacific | |||||||
| Islander | |||||||
| Unspecified | 0.11 (0.01–0.47) | ||||||
| Age at diagnosis | ≤60 | CVD | 1.00 (ref) | ||||
| >60 | 10.73 (9.86–11.70) | ||||||
| Marital status | Married | CVD | 1.00 (ref) | ||||
| Unmarried | 2.21 (2.28–2.55) | ||||||
| Unknown | 1.90 (1.60–2.24) | ||||||
| Right-sided tumor and <10 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and <10 years since diagnosis | 1.00 (0.98–1.03) | ||||||
| Right-sided tumor and ≥20 years since diagnosis | CVD | 1.00 (ref) | |||||
| Left-sided tumor and ≥20 years since diagnosis | 1.01 (0.91–1.11) | ||||||
| Region | Pacific | CVD | 1.00 (ref) | ||||
| Alaska | 0.24 (0.01–1.07) | ||||||
| East | 1.06 (0.99–1.13) | ||||||
| Northern Plains | 1.25 (1.16–1.35) | ||||||
| Southwest | 0.87 (0.76–0.99) | ||||||
| Merzenich, 2016 | Cox proportional hazard | RT and right-sided tumor | CVD | 1.0 (ref) | Clinical, tumor, treatment characteristics | ||
| RT and left-sided tumor | 0.94 (0.64–1.38) | ||||||
| No RT and right-sided tumor | CVD | 1.0 (ref) | |||||
| No RT and left-sided tumor | 1.07 (0.79–1.46) | ||||||
| RT without a history of cardiac disease | CVD | 1.0 (ref) | |||||
| RT with a history of cardiac disease | 1.73 (1.11–2.68) | ||||||
| RT without chemotherapy | CVD | 1.0 (ref) | |||||
| RT with chemotherapy | 0.66 (0.37–1.19) | ||||||
| CVD mortality in breast cancer patients with different ethnic origins | |||||||
| Berkman, 2014 | Kaplan– Meier with log-rank statistics |
White and diagnosed between 1990 and 2010 | CVD | 1.00 (ref) | No covariates | ||
| Black and diagnosed between 1990 and 2010 | 6.43 (3.61–11.45) | ||||||
| White and age at diagnosis 40–49 years | CVD | 1.00 (ref) | |||||
| Black and age at diagnosis 40–49 years | 9.83 (4.56–21.17) | ||||||
| White and age at diagnosis 50–59 years | CVD | 1.00 (ref) | |||||
| Black and age at diagnosis 50–59 years | 3.35 (2.14–5.24) | ||||||
| White and age at diagnosis 60–69 years | CVD | 1.00 (ref) | |||||
| Black and age at diagnosis 60–69 years | 2.13 (1.65–2.74) | ||||||
| White and age at diagnosis ≥70 years | CVD | 1.00 (ref) | |||||
| Black and age at diagnosis ≥70 years | 1.07 (0.93–1.23) | ||||||
| Solanki, 2016 | Cox proportional hazard | Non-Hispanic white | CVD | 1.00 (ref) | Age, birthplace, SEER registry, AJCC stage | ||
| Asian and Pacific islander | 0.77 (0.71–0.83) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Chinese | 0.66 (0.56–0.78) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Japanese | 0.71 (0.62–0.81) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Filipino | 0.90 (0.78–1.03) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Hawaiian | 1.43 (1.17–1.75) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Korean | 0.68 (0.46–0.99) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Vietnamese | 0.46 (0.28–0.76) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Asian Indian and Pakistani | 0.98 (0.70–1.37) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Pacific Islander | 1.33 (0.83–2.15) | ||||||
| Non-Hispanic white | CVD | 1.00 (ref) | |||||
| Other Asian | 0.61 (0.45–0.83) | ||||||
| Non-U.S. born Asian and Pacific Islander | CVD | 1.00 (ref) | |||||
| U.S. born Asian and Pacific Islander | 1.29 (1.08–1.54) | ||||||
| Non-U.S. born Chinese | CVD | 1.00 (ref) | |||||
| U.S. born Chinese | 1.33 (0.81–2.20) | ||||||
| Non-U.S. born Japanese | CVD | 1.00 (ref) | |||||
| U.S. born Japanese | 1.04 (0.74–1.48) | ||||||
| Non-U.S. born Filipino | CVD | 1.00 (ref) | |||||
| U.S. born Filipino | 0.99 (0.57–1.72) | ||||||
| Non-U.S. born Hawaiian | CVD | 1.00 (ref) | |||||
| U.S. born Hawaiian | 0.97 (0.13–7.38) | ||||||
| Non-U.S. born Korean | CVD | 1.00 (ref) | |||||
| U.S. born Korean | 0.17 (0.02–1.69) | ||||||
| Non-U.S. born Asian Indian and Pakistani | CVD | 1.00 (ref) | |||||
| U.S. born Asian Indian and Pakistani | 0.94 (0.11–8.13) | ||||||
| Non-U.S. born Pacific Islander | CVD | 1.00 (ref) | |||||
| U.S. born Pacific Islander | 4.27 (0.68–26.7) | ||||||
| Non-U.S. born Other Asian | CVD | 1.00 (ref) | |||||
| U.S. born Other Asian | 2.06 (0.84–5.10) | ||||||
| CVD mortality in breast cancer patients by diet, body weight, and health behaviors | |||||||
| McCullough, 2016 | Cox proportional hazard | Pre-diagnostic diet score (continuous) | CVD | 0.96 (0.84–1.10) | Clinical, tumor, and treatment characteristics, CVD risk factors | ||
| Pre-diagnostic diet score 0–2 | CVD | 1.00 (ref) | |||||
| Pre-diagnostic diet score 3–5 | 0.95 (0.68–1.32) | ||||||
| Pre-diagnostic diet score 6–9 | 0.94 (0.63–1.39) | ||||||
| Post-diagnostic diet score (continuous) | CVD | 0.95 (0.79–1.14) | |||||
| Post-diagnostic diet score 0–2 | CVD | 1.00 (ref) | |||||
| Post-diagnostic diet score 3–5 | 0.96 (0.60–1.54) | ||||||
| Post-diagnostic diet score 6–9 | 0.81 (0.47–1.39) | ||||||
| Nichols, 2009 | Cox proportional hazard | One to 5 year before diagnosis a BMI <18.5 | CVD | 4.15 (1.44–12.0) | Age, menopausal status, and other CVD risk factors | ||
| One to 5 year before diagnosis a BMI 18.5−24.9 | 1.00 (ref) | ||||||
| One to 5 year before diagnosis a BMI 25.0−29.9 | 1.05 (0.63–1.74) | ||||||
| One to 5 year before diagnosis a BMI ≥30 | 2.45 (1.46–4.11) | ||||||
| BMI after diagnosis <18.5 | CVD | 0.58 (0.08–4.34) | |||||
| BMI after diagnosis 18.5−24.9 | 1.00 (ref) | ||||||
| BMI after diagnosis 25.0−29.9 | 0.99 (0.59–1.66) | ||||||
| BMI after diagnosis ≥30 | 1.65 (0.97–2.83) | ||||||
| Weight (kg) change −50.0 to −10.1 | CVD | 1.08 (0.42–2.78) | |||||
| Weight (kg) change −10.0 to −2.1 | 1.02 (0.58–1.80) | ||||||
| Weight (kg) change −2.0 to 2.0 | 1.00 (ref) | ||||||
| Weight (kg) change 2.1–6.0 | 0.79 (0.43–1.44) | ||||||
| Weight (kg) change 6.1–10.0 | 0.64 (0.29–1.44) | ||||||
| Weight (kg) change 10.1 | 1.73 (0.83–3.62) | ||||||
| Veal, 2017 | Cox proportional hazard | Pre-diagnosis behaviors | Demographic, clinical, tumor, and treatment characteristics | ||||
| BMI | Continuous | CVD | 1.01 (0.95–1.07) | ||||
| 18.5–24.9 | CVD | 1.0 (ref) | |||||
| 25.0–29.9 | 0.88 (0.37–2.07) | ||||||
| 30.0–34.9 | 1.21 (0.45–3.24) | ||||||
| ≥35.0 | 1.85 (0.59–5.85) | ||||||
| Physical activity (hours per week) | Continuous | CVD | 0.83 (0.70–0.98) | ||||
| No activity | CVD | 1.0 (ref) | |||||
| 0–1.9 | 0.52 (0.22–1.23) | ||||||
| 2.0–4.9 | 0.38 (0.15–1.00) | ||||||
| ≥5.0 | 0.29 (0.08–1.04) | ||||||
| Alcohol (drinks per week) | Continuous | CVD | 1.01 (0.94–1.08) | ||||
| Non-drinker | CVD | 1.0 (ref) | |||||
| 0–1.9 | 0.68 (0.29–1.60) | ||||||
| 2.0–6.9 | 1.22 (0.47–3.14) | ||||||
| ≥7.0 | 0.49 (0.13–1.86) | ||||||
| Smoking | Non-smoker | CVD | 1.0 (ref) | ||||
| Former smoker | 0.96 (0.43–2.15) | ||||||
| Current smoker | 2.07 (0.84–5.11) | ||||||
| Post-diagnosis behaviors | Pre-diagnosis health behavior and demographic, clinical, tumor, and treatment characteristics | ||||||
| BMI | Continuous | CVD | 0.96 (0.85–1.08) | ||||
| 18.5–24.9 | CVD | 1.0 (ref) | |||||
| 25.0–29.9 | 0.90 (0.32–2.51) | ||||||
| 30.0–34.9 | 0.63 (0.15–2.70) | ||||||
| ≥35.0 | 0.36 (0.05–2.74) | ||||||
| Physical activity (hours per week) | Continuous | CVD | 1.04 (0.91–1.18) | ||||
| No activity | CVD | 1.0 (ref) | |||||
| 0–1.9 | 0.35 (0.04–2.97) | ||||||
| 2.0–4.9 | 0.42 (0.05–3.60) | ||||||
| ≥5.0 | 2.27 (0.40–12.76) | ||||||
| Alcohol (drinks per week) | Continuous | CVD | 0.90 (0.67–1.22) | ||||
| Non-drinker | CVD | 1.0 (ref) | |||||
| 0–1.9 | 1.43 (0.37–5.62) | ||||||
| 2.0–6.9 | 1.53 (0.24–9.89) | ||||||
| ≥7.0 | 0.57 (0.04–8.52) | ||||||
| Smoking | Non-smoker | CVD | 1.0 (ref) | ||||
| Former smoker | 0.92 (0.41–2.08) | ||||||
| Current smoker | 1.27 (0.22–6.86) | ||||||
AJCC American Joint Committee on Cancer, AMI acute myocardial infarction, BMI body mass index; kg/m2, CHD Coronary heart disease, CI confidence interval, CT chemotherapy, CVA cerebrovascular accident, CVD cardiovascular disease, DCIS ductal carcinoma in situ, HR hazard ratio, HT hormonal therapy, MR mortality ratio, ref reference category, RT radiotherapy, SD standard deviation, SEER Surveillance, Epidemiology, and End Results, US United States
Riihimäki et al. [5] included all 3,676,472 female Swedish residents born before 1977 (Table 2). Of these, 122,217 were diagnosed with primary invasive breast cancer between 1987 and 2006. During a maximum follow-up of 19 years, 10.4% and 7.5% of women died of CVD, respectively. Women with breast cancer had a 1.14 (95% CI 1.10–1.19) times higher risk to die of coronary heart disease, a 1.29 (95% CI 1.22–1.37) times higher risk to die of heart failure, and a 1.24 (95% CI 1.17–1.32) times higher risk to die of other heart disease than women from the general population, independent of age, socioeconomic index, and geographical region of residence in Sweden (Table 3).
Cardiovascular disease mortality in breast cancer patients by patient, tumor, and treatment characteristics
Colzani et al. [18] included 12,850 Swedish women younger than 75 years of age at diagnosis with primary invasive stage I to III breast cancer between 1990 and 2006 (Table 2). During a maximum follow-up of ten years, 1.8% of all women died of CVD. After adjusting for clinical, tumor, and treatment characteristics, except the one of interest, women with breast cancer were at increased risk of CVD mortality if they were older at diagnosis (65–74 years vs. 45–54 years: hazard ratio (HR) = 17.9, 95% CI 8.0–39.7), if diagnosed in an earlier calendar period (1990–1994 vs. 2000–2006: HR = 2.1, 95% CI 1.2–3.6), and treated with only surgery (HR = 2.1, 95% CI 1.2–3.8) or surgery in combination with hormonal therapy (HR = 2.2, 95% CI 1.5–3.2) compared with surgery in combination with radiotherapy and hormonal therapy (Table 3).
Hooning et al. [25] included 7425 women younger than 71 years of age at diagnosis with primary invasive stage I to IIIA breast cancer in the Netherlands between 1970 and 1986 (Table 2). During a median follow-up of 13.8 years, 5.3% of all women died of CVD. After adjusting for clinical, tumor, and treatment characteristics, women with breast cancer were at increased risk of CVD mortality with each year increase in age at diagnosis (HR = 1.12, 95% CI 1.10–1.14), if diagnosed in an earlier calendar period (1976–1980 vs. 1981–1986: HR = 1.54, 95% CI 1.11–2.14), and treated with a combination of surgery and radiotherapy compared with only surgery (HR = 2.03, 95% CI 1.33–3.10) (Table 3).
Cardiovascular disease mortality in breast cancer patients by laterality of the tumor
Bouchardy et al. [20] included 1245 women with a mean age of 57.4 years at diagnosis with primary lymph node-negative breast cancer in Switzerland between 1980 and 2004 (Table 2). During a mean follow-up of 7.7 years, 2.2% of all women died of CVD. Among women treated with radiotherapy, an inner quadrant tumor was associated with a 2.46 (95% CI 1.13–5.37) higher risk of dying of CVD, adjusted for clinical, tumor, and treatment characteristics (Table 3).
Darby et al. [23] included 308,861 women between 20 and 79 years of age at diagnosis with primary in situ or invasive breast cancer in the USA between 1973 and 2001 (Table 2). During a maximum follow-up of 29 years, 4.2% of all women died of CVD. In women treated with radiotherapy and diagnosed between 1973 and 1982, left-sided breast cancer led to higher mortality ratios (MR) ten to 14 years post diagnosis (unadjusted MR = 1.42, 95% CI 1.11–1.82) and over 15 years post diagnosis (unadjusted MR = 1.58, 95% CI 1.29–1.95) compared with right-sided breast cancer (Table 3). More than ten years post diagnosis, women with left-sided breast cancer had a higher risk of death from CVD (unadjusted MR = 1.44, 95% CI 1.26–1.65), acute myocardial infarction (unadjusted MR = 1.43, 95% CI 1.10–1.87), and other ischemic CVD (unadjusted MR = 1.60, 95% CI 1.26–2.02) compared with women with right-sided breast cancer.
Giordano et al. [24] included 24,785 women with primary in situ or invasive breast cancer diagnosed in the US between 1973 and 1988 (Table 2). Mean age at diagnosis was 56.9 years (standard deviation (SD) = 13.2) at diagnosis. Eight years post diagnosis, women with left-sided breast cancer who were diagnosed in 1979 had a (unadjusted) 1.50 (95% CI 1.15–1.87) times higher risk to die of CVD compared with women with right-sided breast cancer diagnosed in the same year (Table 3).
Haque et al. [26] included 140,914 women of all ages with ductal carcinoma in situ (DCIS) in the US between 1973 and 2002 (Table 2).The median follow-up was 11.5 years (interquartile range = 6.8–15.1). Among women diagnosed between 1973 and 1982, a left-sided tumor was associated with a 1.30 (95% CI 1.18–1.42) higher risk of dying of CVD than a right-sided tumor, independent of clinical, tumor, and treatment characteristics. This association was not found for women diagnosed in a more recent calendar period.
Merzenich et al. [21] included 11,982 women with a mean age of 59 years (range = 18–101) at primary diagnosis of in situ or invasive breast cancer in Germany between 1998 and 2008 (Table 2) [21]. During a median follow-up of 6.5 years (range = 0–15), 2.3% of all women died of CVD. Women with left-sided breast cancer did not have a higher risk of dying of CVD than women with right-sided breast cancer, irrespectively of radiotherapy treatment (Table 3). Among women treated with radiotherapy, women with a history of CVD had a 1.73 times (95% CI 1.11–2.68) higher risk of dying of CVD than women without a history of CVD.
CVD mortality in breast cancer patient by ethnic origin
Berkman et al. [6] included 54,518 white and 6113 black women over 40 years of age at diagnosis with primary DCIS in the US between 1978 and 2010 (Table 2). During a median follow-up of 9.2 years, 6.0% of all women died of CVD. Among women diagnosed with breast cancer between 1990 and 2010, black women had a (unadjusted) 6.43 (95% CI 3.61–11.45) times higher risk of death from CVD compared to white women (Table 3). Unadjusted HRs of CVD death in black compared to white women decreased with increasing age at diagnosis: 9.83 (95% CI 4.56–21.17), 3.35 (95% CI 2.14–5.24), 2.13 (95% CI 1.65–2.74), and 1.07 (95% CI 0.93–1.23) for women of ages 40–49, 50–59, 60–69, and ≥ 70 years, respectively.
Solanki et al. [17] included 462,005 non-Hispanic white and 44,531 Asian and Pacific Islander women diagnosed with breast cancer in the US between 1991 and 2001 (Table 2). Median age at breast cancer diagnosis was 61.2 years (SD = 13.7) for non-Hispanic white women and 56.3 years (SD = 13.1) for Asian and Pacific Islander women. The median follow-up for non-Hispanic white women was 4 years (range = 2-6), during which 5.5% of women died of CVD. The median follow-up for Asian and Pacific Islander women was 3 years (range 2–5), during which 2.6% of women died of CVD. After adjusting for patient, tumor, and registry characteristics, Asian and Pacific Islander women with breast cancer had a HR of 0.77 (95% CI 0.71–0.83) for death from CVD compared to non-Hispanic white women with breast cancer (Table 2). Furthermore, US born Asian and Pacific Islander women with breast cancer had a 1.29 (95% CI 1.08–1.54) times higher risk of death from CVD compared to non-US born Asian and Pacific Islander women with breast cancer.
CVD mortality in breast cancer patients by diet, body weight, and health-behaviors
McCullough et al. [16] included 4452 women diagnosed with primary invasive breast cancer in Switzerland between 1992 and 2011 who had scored their diet according to the American Cancer Society (AMC) guidelines before breast cancer diagnosis, and of these, 2152 women scored their diet also at least one year after breast cancer diagnosis (Table 2). The AMC guidelines recommend following the general food-based guidelines for primary cancer prevention, which includes eating a plant-based diet rich in vegetables and fruits, whole grains, and which is limited in red and processed meats [27]. Mean age at diagnosis was 70.7 years (SD = 7.2). During a mean follow-up of 9.8 years (SD = 4.9), 5.2% of all women died of CVD. After adjusting for tumor, treatment, and patient characteristics, both pre-diagnostic and post-diagnostic higher AMC diet scores, indicating an unhealthier diet, were not associated with a higher risk of CVD mortality following breast cancer compared with the lowest diet score category (0–2), indicating a healthier diet (Table 3).
Nichols et al. [15] included 5791 women with primary in situ or invasive breast cancer diagnosed in the US between 1988 and 1999 (Table 2). Mean age at diagnosis was 58.4 years (SD = 10.0). During a mean follow-up of 6.4 years (SD = 1.2), 1.6% of all women died of CVD. After correcting for age, menopausal status, and CVD risk factors, Nichols et al. found a 4.15 (95% CI 1.44–12.0) and 2.45 (95% CI 1.46–4.11) times higher risk of death from CVD in women with a pre-diagnosis underweight (body mass index (BMI; kg/m2): <18.5) and obesity (BMI: ≥ 30), respectively, compared with women with a pre-diagnosis normal weight (BMI: 18.5–24.9) (Table 3).
Veal et al. [22] included 1925 women aged between 20 and 74 years at diagnosis of DCIS in the US between 1997 and 2006 (Table 2). During a mean follow-up of 6.7 years, 1.8% of all women died of CVD. More hours per week of physical activity before the breast cancer diagnosis was associated with 0.83 (95% CI 0.70–0.98) lower risk of dying of CVD (Table 3).
Discussion
In this review, we systematically summarized the evidence on the risk and risk factors of death from CVD following breast cancer.
The absolute risk of dying of CVD following breast cancer ranges from 1.6% [15] to 10.4% [5], and the risk of CVD mortality is higher in women with breast cancer than women from the general population [5, 8]. Older age at diagnosis [6, 18, 19, 25], left-sided tumor [23, 24, 26], diagnosis in an earlier calendar period [18, 25], and black ethnic origin [6] are risk factors of CVD mortality following breast cancer.
Several mechanisms are proposed for the increased risk of CVD mortality in women with breast cancer. CVD risk factors, such as obesity and diabetes, may be more present among breast cancer survivors than women from the general population as breast cancer and CVD have shared risk factors [28]. Also, cardiotoxic effects of breast cancer treatments, specifically mediastinal and left-sided radiotherapy, anthracycline-based chemotherapy, and trastuzumab, are well documented to increase the risk of CVD [29–32].
In the current review, studies with longer follow-up, i.e. over 10 years [5, 6, 8], reported higher absolute risks of CVD mortality. The risk of CVD increases with time since diagnosis probably due to increasing age and cardiotoxicity of breast cancer treatments that become apparent after several years [29]. Age is a well-known risk factor for CVD [33–36], and therefore, expected to be found as a risk factor in women with breast cancer [6, 18, 19, 25]. Schonberg et al. [14] found that 26–40% of older women diagnosed with early-stage breast cancer died of CVD, indicating that the risk of CVD is high in specific subgroups and particularly in older women.
The association between left-sided breast cancer and radiotherapy treatment with a higher risk of CVD mortality was found among women diagnosed in the early 1980’s [23, 24, 26]. Radiotherapy treatment was more cardiotoxic in these years as it usually involved higher doses with large irradiation fields irradiating parts of the heart [37, 38]. This may also explain the increased risk of CVD mortality among breast cancer patients diagnosed in an earlier calendar period [18, 25]. Colzani et al. [18] did not find an increased risk of CVD mortality among women treated with radiotherapy and/or chemotherapy. Although the baseline risk of CVD was not reported, this result is probably due to patient selection, i.e. women who did not undergo radiotherapy and/or chemotherapy probably had a higher risk of CVD at baseline. The lower risk of CVD in Asian populations [17] and the higher risk of CVD in black populations [6] are reported by several studies and can be explained by the lower and higher presence of CVD risk factors, respectively, such as high blood pressure, obesity, and lipid levels [39–42].
The present systematic review shows that there are only a limited number of studies investigating the risk and risk factors of CVD mortality following breast cancer, and that these studies are heterogeneous in design, study population, and length of follow-up. Also, the determinants and outcomes, in terms of CVD risk factors and death due to CVD, respectively, vary. We acknowledge that, due to the heterogeneous designs of the included studies, we were unable to perform a meta-analysis, which limited the strength of evidence. Besides limitations, the current review has strengths. This is the first study that systematically summarized the literature on the risk and risk factors of death from CVD following breast cancer. Furthermore, the current systematic review includes a large variety of risk factors of death from CVD in women with breast cancer.
To conclude, the combination of high breast cancer incidence, improved breast cancer survival, presence of CVD risk factors, and cardiotoxic breast cancer treatments has resulted into many breast cancer survivors at risk of CVD. Therefore, it is important to understand the incidence and etiology of CVD in these survivors. Furthermore, identification of women with breast cancer at high risk of CVD is important to minimize the number of women suffering and/or dying of CVD after breast cancer treatment and improve quality of life and long-term prognosis. Clinicians should be able to identify breast cancer patients at increased risk of CVD and provide accurate recommendations for CVD risk reduction strategies specifically for breast cancer survivors at high risk of CVD. The current systematic review, in combination with a recent guideline by Armenian et al. [29] on the prevention and monitoring of cardiac dysfunction in survivors of adult cancers, may help clinicians with such a recommendation. In addition, there are studies investigating the identification of women with breast cancer at high risk of CVD using other measurements, for example, by measuring the coronary artery calcification on radiotherapy planning computed tomography scans [43]. This may further help clinicians with identification of breast cancer patients at high risk of CVD. Identification of breast cancer patients at high risk of CVD is important to optimize CVD prevention of (irreversible) cardiac damage, by adjusting breast cancer treatments accordingly and initializing CVD (preventative) treatment. Furthermore, a tailored individual approach with early and late monitoring of cardiac dysfunction in breast cancer survivors should be implemented in routine care [44].
Acknowledgments
Funding
The current project was conducted within the framework ‘Strategic PhD Partnership Program’ from the Board of Directors of the University Medical Center Utrecht.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study format, informed consent is not required. This article does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Integraal Kankercentrum Nederland Cijfers over kanker. http://cijfersoverkanker.nl/. Accessed 10 Aug 2016
- 2.Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabe E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castaneda-Orjuela C, Catala-Lopez F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HM, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Soreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabares-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BS, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki ME, Zenebe ZM, Murray CJ, Naghavi M (2016) Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. doi: 10.1001/jamaoncol.2016.5688 [DOI] [PMC free article] [PubMed]
- 3.Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Mandelblatt JS, Yakovlev AY, Habbema JD, Feuer EJ, Cancer Intervention and Surveillance Modeling Network (CISNET) Collaborators Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784–1792. doi: 10.1056/NEJMoa050518. [DOI] [PubMed] [Google Scholar]
- 4.Nakano M, Fujisue M, Tashima R, Okumura Y, Nishiyama Y, Ohsako T, Toyozumi Y, Arima N, Nishimura R. Survival time according to the year of recurrence and subtype in recurrent breast cancer. Breast. 2015;24:588–593. doi: 10.1016/j.breast.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Riihimaki M, Thomsen H, Brandt A, Sundquist J, Hemminki K. Death causes in breast cancer patients. Ann Oncol. 2012;23:604–610. doi: 10.1093/annonc/mdr160. [DOI] [PubMed] [Google Scholar]
- 6.Berkman A, Cole BF, Ades PA, Dickey S, Higgins ST, Trentham-Dietz A, Sprague BL, Lakoski SG. Racial differences in breast cancer, cardiovascular disease, and all-cause mortality among women with ductal carcinoma in situ of the breast. Breast Cancer Res Treat. 2014;148:407–413. doi: 10.1007/s10549-014-3168-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taunk NK, Haffty BG, Kostis JB, Goyal S. Radiation-induced heart disease: pathologic abnormalities and putative mechanisms. Front Oncol. 2015;5:39. doi: 10.3389/fonc.2015.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradshaw PT, Stevens J, Khankari N, Teitelbaum SL, Neugut AI, Gammon MD. Cardiovascular disease mortality among breast cancer survivors. Epidemiology. 2016;27:6–13. doi: 10.1097/EDE.0000000000000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bird BR, Swain SM. Cardiac toxicity in breast cancer survivors: review of potential cardiac problems. Clin Cancer Res. 2008;14:14–24. doi: 10.1158/1078-0432.CCR-07-1033. [DOI] [PubMed] [Google Scholar]
- 10.Borger JH, Hooning MJ, Boersma LJ, Snijders-Keilholz A, Aleman BM, Lintzen E, van Brussel S, van der Toorn PP, Alwhouhayb M, van Leeuwen FE. Cardiotoxic effects of tangential breast irradiation in early breast cancer patients: the role of irradiated heart volume. Int J Radiat Oncol Biol Phys. 2007;69:1131–1138. doi: 10.1016/j.ijrobp.2007.04.042. [DOI] [PubMed] [Google Scholar]
- 11.McGale P, Darby SC, Hall P, Adolfsson J, Bengtsson NO, Bennet AM, Fornander T, Gigante B, Jensen MB, Peto R, Rahimi K, Taylor CW, Ewertz M. Incidence of heart disease in 35,000 women treated with radiotherapy for breast cancer in Denmark and Sweden. Radiother Oncol. 2011;100:167–175. doi: 10.1016/j.radonc.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 12.Pinder MC, Duan Z, Goodwin JS, Hortobagyi GN, Giordano SH. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol. 2007;25:3808–3815. doi: 10.1200/JCO.2006.10.4976. [DOI] [PubMed] [Google Scholar]
- 13.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 14.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
- 15.Nichols HB, Trentham-Dietz A, Egan KM, Titus-Ernstoff L, Holmes MD, Bersch AJ, Holick CN, Hampton JM, Stampfer MJ, Willett WC, Newcomb PA. Body mass index before and after breast cancer diagnosis: associations with all-cause, breast cancer, and cardiovascular disease mortality. Cancer Epidemiol Biomark Prev. 2009;18:1403–1409. doi: 10.1158/1055-9965.EPI-08-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCullough ML, Gapstur SM, Shah R, Campbell PT, Wang Y, Doyle C, Gaudet MM. Pre- and postdiagnostic diet in relation to mortality among breast cancer survivors in the CPS-II Nutrition Cohort. Cancer Causes Control. 2016 doi: 10.1007/s10552-016-0802-x. [DOI] [PubMed] [Google Scholar]
- 17.Solanki PA, Ko NY, Qato DM, Calip GS (2016) Risk of cancer-specific, cardiovascular, and all-cause mortality among Asian and Pacific Islander breast cancer survivors in the United States, 1991–2011. Springerplus. doi: 10.1186/s40064-016-1726-3 [DOI] [PMC free article] [PubMed]
- 18.Colzani E, Liljegren A, Johansson AL, Adolfsson J, Hellborg H, Hall PF, Czene K. Prognosis of patients with breast cancer: causes of death and effects of time since diagnosis, age, and tumor characteristics. J Clin Oncol. 2011;29:4014–4021. doi: 10.1200/JCO.2010.32.6462. [DOI] [PubMed] [Google Scholar]
- 19.Haque R, Yood MU, Geiger AM, Kamineni A, Avila CC, Shi J, Silliman RA, Quinn VP. Long-term safety of radiotherapy and breast cancer laterality in older survivors. Cancer Epidemiol Biomarkers Prev. 2011;20:2120–2126. doi: 10.1158/1055-9965.EPI-11-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bouchardy C, Rapiti E, Usel M, Majno SB, Vlastos G, Benhamou S, Miralbell R, Neyroud-Caspar I, Verkooijen HM, Vinh-Hung V. Excess of cardiovascular mortality among node-negative breast cancer patients irradiated for inner-quadrant tumors. Ann Oncol. 2010;21:459–465. doi: 10.1093/annonc/mdp341. [DOI] [PubMed] [Google Scholar]
- 21.Merzenich H, Bartkowiak D, Schmidberger H, Schmidt M, Schwentner L, Wiegel T, Woeckel A, Wollschlager D, Blettner M. 3D conformal radiotherapy is not associated with the long-term cardiac mortality in breast cancer patients: a retrospective cohort study in Germany (PASSOS-Heart Study) Breast Cancer Res Treat. 2017;161:143–152. doi: 10.1007/s10549-016-4042-2. [DOI] [PubMed] [Google Scholar]
- 22.Veal CT, Hart V, Lakoski SG, Hampton JM, Gangnon RE, Newcomb PA, Higgins ST, Trentham-Dietz A, Sprague BL. Health-related behaviors and mortality outcomes in women diagnosed with ductal carcinoma in situ. J Cancer Surviv. 2017 doi: 10.1007/s11764-016-0590-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Darby SC, McGale P, Taylor CW, Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 2005;6:557–565. doi: 10.1016/S1470-2045(05)70251-5. [DOI] [PubMed] [Google Scholar]
- 24.Giordano SH, Kuo YF, Freeman JL, Buchholz TA, Hortobagyi GN, Goodwin JS. Risk of cardiac death after adjuvant radiotherapy for breast cancer. J Natl Cancer Inst. 2005;97:419–424. doi: 10.1093/jnci/dji067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hooning MJ, Aleman BM, van Rosmalen AJ, Kuenen MA, Klijn JG, van Leeuwen FE. Cause-specific mortality in long-term survivors of breast cancer: a 25-year follow-up study. Int J Radiat Oncol Biol Phys. 2006;64:1081–1091. doi: 10.1016/j.ijrobp.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 26.Haque W, Verma V, Haque A, Butler EB, Teh BS. Trends in cardiac mortality in women with ductal carcinoma in situ. Breast Cancer Res Treat. 2017;161:345–351. doi: 10.1007/s10549-016-4045-z. [DOI] [PubMed] [Google Scholar]
- 27.Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, Gapstur S, Patel AV, Andrews K, Gansler T, American Cancer Society 2010 Nutrition and Physical Activity Guidelines Advisory Committee American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62:30–67. doi: 10.3322/caac.20140. [DOI] [PubMed] [Google Scholar]
- 28.Weaver KE, Foraker RE, Alfano CM, Rowland JH, Arora NK, Bellizzi KM, Hamilton AS, Oakley-Girvan I, Keel G, Aziz NM. Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal, and gynecologic cancers: a gap in survivorship care? J Cancer Surviv. 2013;7:253–261. doi: 10.1007/s11764-013-0267-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Armenian SH, Lacchetti C, Barac A, Carver J, Constine LS, Denduluri N, Dent S, Douglas PS, Durand JB, Ewer M, Fabian C, Hudson M, Jessup M, Jones LW, Ky B, Mayer EL, Moslehi J, Oeffinger K, Ray K, Ruddy K, Lenihan D. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2017;35:893–911. doi: 10.1200/JCO.2016.70.5400. [DOI] [PubMed] [Google Scholar]
- 30.EBCTCG (Early Breast Cancer Trialists’ Collaborative Group) McGale P, Taylor C, Correa C, Cutter D, Duane F, Ewertz M, Gray R, Mannu G, Peto R, Whelan T, Wang Y, Wang Z, Darby S. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383:2127–2135. doi: 10.1016/S0140-6736(14)60488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guenancia C, Lefebvre A, Cardinale D, Yu AF, Ladoire S, Ghiringhelli F, Zeller M, Rochette L, Cottin Y, Vergely C. Obesity as a risk factor for anthracyclines and trastuzumab cardiotoxicity in breast cancer: a systematic review and meta-analysis. J Clin Oncol. 2016;34:3157–3165. doi: 10.1200/JCO.2016.67.4846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vejpongsa P, Yeh ET. Prevention of anthracycline-induced cardiotoxicity: challenges and opportunities. J Am Coll Cardiol. 2014;64:938–945. doi: 10.1016/j.jacc.2014.06.1167. [DOI] [PubMed] [Google Scholar]
- 33.Fan J, Song Y, Chen Y, Hui R, Zhang W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;168:4761–4768. doi: 10.1016/j.ijcard.2013.07.230. [DOI] [PubMed] [Google Scholar]
- 34.Ringback Weitoft G, Eliasson M, Rosen M. Underweight, overweight and obesity as risk factors for mortality and hospitalization. Scand J Public Health. 2008;36:169–176. doi: 10.1177/1403494807085080. [DOI] [PubMed] [Google Scholar]
- 35.Wu CY, Chou YC, Huang N, Chou YJ, Hu HY, Li CP. Association of body mass index with all-cause and cardiovascular disease mortality in the elderly. PLoS ONE. 2014;9:e102589. doi: 10.1371/journal.pone.0102589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.D’Agostino RBS, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 37.Cuzick J, Stewart H, Rutqvist L, Houghton J, Edwards R, Redmond C, Peto R, Baum M, Fisher B, Host H. Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol. 1994;12:447–453. doi: 10.1200/JCO.1994.12.3.447. [DOI] [PubMed] [Google Scholar]
- 38.Darby SC, Bronnum D, Correa C, Ewertz M, Gagliardi G, Gigante B, McGale P, Nisbet A, Taylor C, Hall P. A dose-response relationship for the incidence of radiation-related heart disease. Int J Radiat Oncol Biol Phys. 2010;78:S49–S50. doi: 10.1016/j.ijrobp.2010.07.151. [DOI] [Google Scholar]
- 39.Valina-Toth AL, Zavodnik T, Seicean S, Plana J, Marwick T. African american race is a correlate of heart failure in breast cancer survivors: a study of 26,347 women identified with breast cancer from 1973 to 2007. J Am Coll Cardiol. 2013;61:E580. doi: 10.1016/S0735-1097(13)60580-X. [DOI] [Google Scholar]
- 40.Budoff MJ, Nasir K, Mao S, Tseng PH, Chau A, Liu ST, Flores F, Blumenthal RS. Ethnic differences of the presence and severity of coronary atherosclerosis. Atherosclerosis. 2006;187:343–350. doi: 10.1016/j.atherosclerosis.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 41.Sasayama S. Heart disease in Asia. Circulation. 2008;118:2669–2671. doi: 10.1161/CIRCULATIONAHA.108.837054. [DOI] [PubMed] [Google Scholar]
- 42.Tammemagi CM, Nerenz D, Neslund-Dudas C, Feldkamp C, Nathanson D. Comorbidity and survival disparities among black and white patients with breast cancer. JAMA. 2005;294:1765–1772. doi: 10.1001/jama.294.14.1765. [DOI] [PubMed] [Google Scholar]
- 43.Gernaat SA, Isgum I, de Vos BD, Takx RA, Young-Afat DA, Rijnberg N, Grobbee DE, van der Graaf Y, de Jong PA, Leiner T, van den Bongard DH, Pignol JP, Verkooijen HM. Automatic coronary artery calcium scoring on radiotherapy planning CT scans of breast cancer patients: reproducibility and association with traditional cardiovascular risk factors. PLoS ONE. 2016;11:e0167925. doi: 10.1371/journal.pone.0167925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maas AH, Ottevanger N, Atsma F, Cramer MJ, Leiner T, Poortmans P. Cardiovascular surveillance in breast cancer treatment: a more individualized approach is needed. Maturitas. 2016;89:58–62. doi: 10.1016/j.maturitas.2016.04.015. [DOI] [PubMed] [Google Scholar]