Abstract
Iliotibial (IT) band syndrome is a common cause of lateral knee pain in runners and cyclists. Many can be treated nonoperatively; however, some may require surgical lengthening of their IT band to achieve optimal pain relief and a return to preinjury level of activity. Several studies have been published detailing surgical lengthening procedures and satisfactory outcomes after these procedures. However, it is important to continue to improve on and optimize outcomes. We present our arthroscopic IT band–lengthening procedure.
Iliotibial (IT) band syndrome in a common condition that causes lateral knee pain in runners, with a reported incidence rate of 1% to 12%.1, 2, 3, 4 It was first described in 1975 by Renne5 as a condition affecting active-duty marines. The proposed cause involves friction of the IT band on the lateral femoral condyle during repetitive extension and flexion at the knee.1, 6 Hence, patients will often complain of pain during activity and will often have crepitus palpated at the lateral femoral condyle during flexion and extension (positive Noble compression test).6, 7, 8 Nonoperative management is the standard of care for this condition, often consisting of rest from pain-inciting activities with a gradual return to activities as tolerated, oral anti-inflammatories, physical therapy focused on stretching the IT band, and corticosteroid injections.1, 3, 9, 10
However, if symptoms persist for greater than 6 months despite these conservative modalities, some patients may require surgical intervention to achieve pain relief and return to preinjury activity levels.6 It has been seen that by surgically lengthening the IT band, one can achieve satisfactory pain relief and a quick return to activity.11, 12, 13 Although there have been surgical techniques for this particular condition published, it is critical that techniques continue to be improved to achieve optimal results.14, 15, 16, 17 Therefore, our purpose was to describe an arthroscopic surgical technique for IT band lengthening in patients with IT band syndrome refractory to conservative treatment modalities.
Surgical Technique
Step 1: Preparation
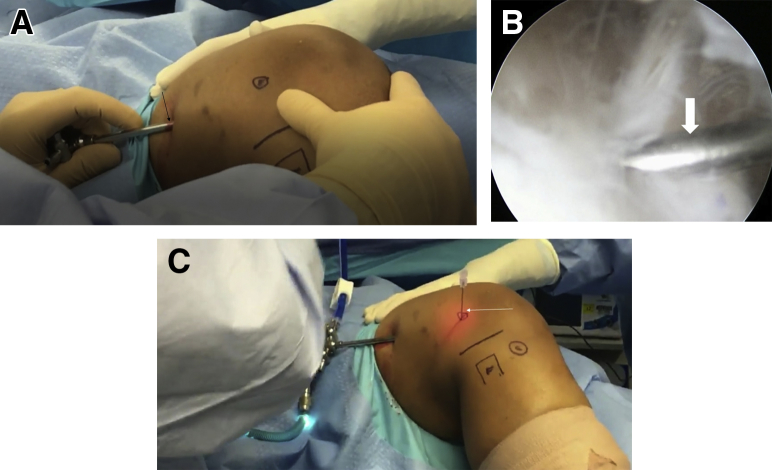
The patient is placed in the supine position and the affected knee (right side) flexed to 30°. This is critical because inadequate flexion may lead to the inability to appropriately visualize the IT band. The lateral femoral condyle, the fibular head, and the Gerdy tubercle are identified and marked (Fig 1).
Fig 1.
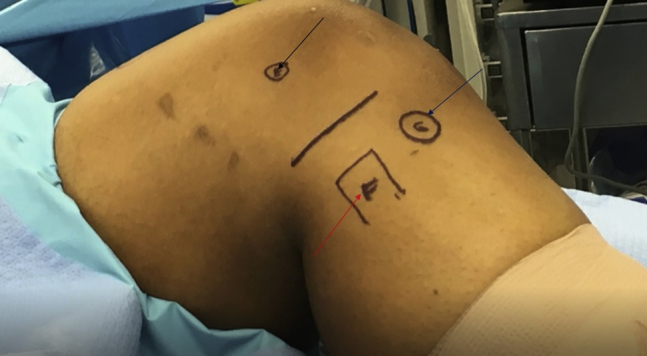
The patient is placed in the supine position and the right knee is flexed to 30°. We have marked the lateral femoral epicondyle (black arrow), the head of the fibula (red arrow), and the Gerdy tubercle (blue arrow).
Step 2: Portal Creation
A No. 11 blade scalpel is used to make a proximal-lateral portal, and a blunt trocar and sheath are inserted under the IT band with the trocar angled toward the lateral femoral condyle, where an arthroscopic camera is inserted (Fig 2A). A spinal needle is then used to localize the insertion point for the distal-lateral portal directly over the lateral epicondyle at the site of the patient's pathology (Fig 2 B and C). It is imperative to ensure adequate visualization of the spinal needle before the procedure continues. A No. 11 blade is then used to create the portal over the lateral condyle and incise the IT band longitudinally.
Fig 2.
(A) While the patient remains supine with the right knee flexed to 30°, the right proximal-lateral portal is made with a No. 11 blade scalpel. The trocar (arrow) is then inserted with angulation in the direction of the right lateral femoral condyle. The arthroscopic camera is inserted into this proximal portal and remains there for the duration of the procedure. (B, C) A spinal needle (arrows) is inserted directly over the right lateral femoral epicondyle. It is visualized by the arthroscopic camera, which is located in the right proximal portal. A No. 11 blade scalpel is used to create the working distal portal directly over the right lateral epicondyle.
Step 3: Bursectomy
With the arthroscopic camera in the proximal-lateral portal, the shaver is inserted into the distal-lateral portal and a bursectomy is performed deep to the IT band (Fig 3A). Care is taken to ensure a complete bursectomy is performed for appropriate visualization of the IT band. Once completed, hemostasis is achieved with an Arthrocare-1 wand (Smith & Nephew, Austin, TX) (Fig 3B).
Fig 3.
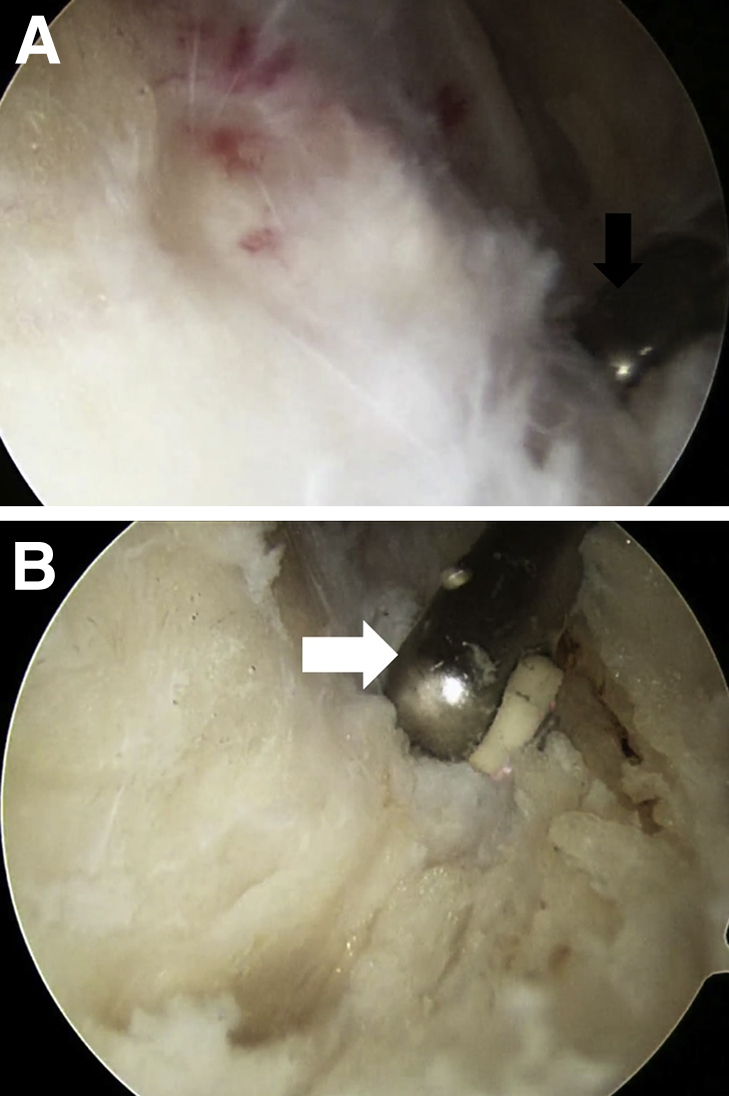
(A) A bursectomy is performed deep to the iliotibial band with an arthroscopic shaver (Smith & Nephew) (arrow) in the right distal-lateral portal and the arthroscopic camera in the right proximal-lateral portal. (B) The bursectomy is completed with hemostasis being achieved by the Arthrocare-1 wand (arrow) in the right distal-lateral portal. The camera remains in the proximal portal during this step.
Step 4: Protection of Skin
Metzenbaum scissors (Smith & Nephew) are inserted into the distal-lateral portal used to spread the tissue over the IT band, creating separation between the skin and the IT band, thus protecting the overlying skin until completion of the procedure (Fig 4).
Fig 4.
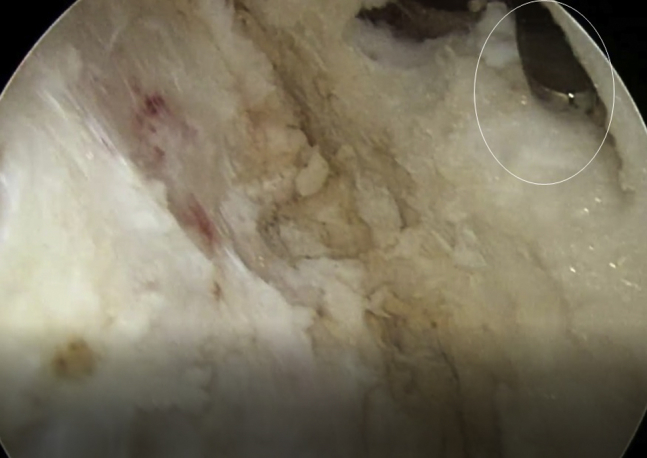
By use of the right distal-lateral portal, Metzenbaum scissors (oval) are used to spread the tissue of the overlying skin of the iliotibial band, thus protecting the skin during lengthening. Visualization using the arthroscopic camera occurs through the proximal portal.
Step 5: Lengthening of IT Band
Cruciate IT band lengthening is then performed (Fig 5). The arthroscopic camera remains in the proximal-lateral portal, and scissors are inserted into the distal portal. Metzenbaum scissors are used to incise the band proximally (Fig 5A) and distally (Fig 5B), as well as anteriorly (Fig 5C) and posteriorly (Fig 5D), from the point of initial insertion. A complete lengthening must be performed to minimize the risk of recurrent IT band syndrome. The Arthrocare-1 wand is then used to complete the lengthening (Fig 5E). Care is taken not to damage the overlying skin (Fig 6). Video 1 shows the complete technique.
Fig 5.
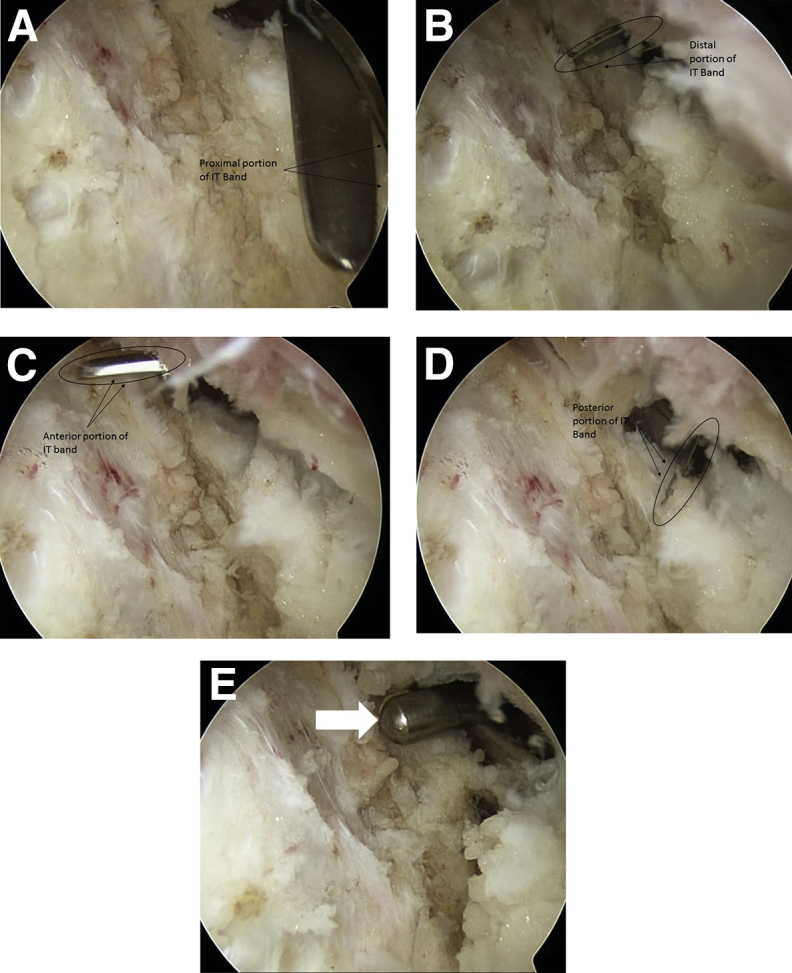
(A-D) With the arthroscopic camera still in the right proximal portal, by use of the Metzenbaum scissors (ovals) inserted into the distal-lateral portal, the lengthening is performed proximally (A), distally (B), anteriorly (C), and posteriorly (D) from its point of insertion at the Gerdy tubercle. The arrows with labels are used to show the orientation at each dimension of the lengthening. (IT, iliotibial.) (E) The Arthrocare-1 wand (arrow) is inserted into the right distal portal and is used to complete the lengthening with care taken not to damage the overlying skin. The arthroscopic camera remains in the right proximal portal for appropriate visualization.
Fig 6.
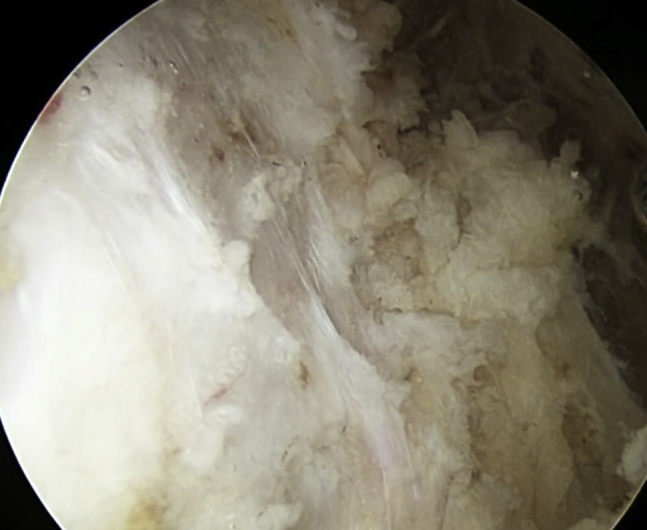
Completed iliotibial band lengthening.
Discussion
IT band syndrome is a painful condition that is often seen in persons who participate in activities such as running or cycling.4, 9, 18 Despite the well-described techniques with satisfactory outcomes that have been reported in the literature, it is imperative that different surgical lengthening techniques are clearly described to optimize outcomes and return to activity.11, 12, 13, 17 Hence, we have presented our arthroscopic IT band–lengthening procedure that we believe allows for a complete lengthening of the IT band. Table 1 shows pearls and pitfalls.
Table 1.
Pearls and Pitfalls
| Step | Pearls | Pitfalls |
|---|---|---|
| 1. Preparation | The surgeon should ensure that the knee is flexed to 30°. | Inadequate flexion leads to difficulty visualizing the IT band. |
| 2. Portal creation | Creation of the distal portal over the lateral femoral condyle becomes critically important because this will be the working portal of the procedure. | The surgeon should ensure visualization of the spinal needle before proceeding. |
| 3. Bursectomy | Bursectomy should be completed with the Arthrocare-1 wand to ensure hemostasis. | The IT band may not be completely and appropriately visualized if the bursectomy is not complete. |
| 4. Skin protection | Metzenbaum scissors allow for the appropriate separation of the skin from the IT band. | The overlying skin is at risk of being damaged during the lengthening without separation. |
| 5. Lengthening | The surgeon should be aware of the overlying skin. | If the surgeon does not release proximally, distally, anteriorly, and posteriorly, there is an increased risk of recurrence of IT band syndrome. |
IT, iliotibial.
There have been several small studies that have shown that IT band lengthening can appropriately treat chronic IT band syndrome refractory to conservative treatment modalities with a minimal risk of complications and a quick return to play (Table 2).11, 12, 13, 15, 18 Hariri et al.13 evaluated this in a series of 11 patients in whom a 6-month course of nonoperative treatment failed. The operation was performed with an open technique after a diagnostic arthroscopy. After a mean follow-up period of 38 months (range, 20-66 months), the cohort showed a substantial improvement in postoperative visual analog scale scores (from 8 to 2 points, P < .001). However, there was no difference between the preoperative and postoperative Tegner activity scores (6 points vs 5 points, P = .47). Yet, when further analyzed, 8 of the 11 patients had Tegner scores that were equal to or better than their preinjury scores. Similarly, Michels et al.11 reported on a series of patients who underwent IT band lengthening performed by a completely intra-articular arthroscopic technique (34 lengthening procedures). After a mean 28-month follow-up period, all of the patients had returned to running activities within 3 months of the operation. Furthermore, by use of the scale created by Drogset et al.,12 the authors found that 80% of the cohort achieved excellent results, with 17% having good results. Hence, different techniques may result in satisfactory outcomes.
Table 2.
Studies Detailing Outcomes of Surgical Iliotibial Band Lengthening
| Authors | N | Mean Age, yr | Mean Follow-Up, mo | Return to Preinjury Activity, % | Complication Rate, % |
|---|---|---|---|---|---|
| Hariri et al.,13 2009 | 11 | 32 (range, 24-41) | 38 (range, 20-66) | 72 | 0 |
| Michels et al.,11 2009 | 34 | 31 (range, 19-44) | 28 (minimum, 6) | 100 | 3 |
| Drogset et al.,12 1999 | 45 | 27 (range, 14-46) | 25 (range, 2-108) | — | 2 |
| Holmes et al.,18 1993 | 21 | — | — (minimum, 3) | 81 | — |
| Martens et al.,15 1989 | 19 | 25 (range, 19-33) | 45 (range, 24-132) | 100 | 5 |
Although the outcomes appear to not be solely dependent on the chosen surgical technique, there are potential advantages and disadvantages for each technique (Table 3). Our technique uses arthroscopy, whose less invasive nature may potentially lead to less pain, decreased blood loss, and a smaller incision with less dissection required, as opposed to its open counterparts, which could potentially lead to more pain, greater blood loss, and larger incisions with a greater dissection required. Furthermore, our technique allows for direct lengthening specifically at the area of pathology. Conversely, conventional open techniques offer the potential for a greater lengthening of the IT band with a larger Z-plasty technique. Given these advantages and disadvantages, we believe that our arthroscopic technique maximizes efficacy and safety.
Table 3.
Advantages and Disadvantages of Open and Arthroscopic Iliotibial Band Lengthening
| Technique | Advantages | Disadvantages |
|---|---|---|
| Conventional open technique | Potential for greater lengthening using Z-plasty | Theoretically more pain |
| Theoretically greater blood loss | ||
| Larger incision with greater dissection required | ||
| Our arthroscopic technique | Theoretically less pain | Inability to perform greater lengthening |
| Theoretically less blood loss | ||
| Smaller incision with decreased dissection required | ||
| Localized lengthening that directly addresses pathology |
In conclusion, our IT band–lengthening technique may be used in patients with chronic IT band syndrome. We believe it may be easily replicated and allows for an appropriate lengthening that will greatly minimize the risk of recurrence. Future studies should analyze the outcomes of this surgical lengthening procedure and compare it with other techniques in the hope of definitively establishing an operative standard of care for this condition.
Footnotes
The authors report the following potential conflict of interest or source of funding: T.P.P. receives support from Shaklee. Paid distributer. V.K.M. receives support from MD Advantage. A.J.S. receives support from MD Advantage, Mitek.
Supplementary Data
The patient is in the supine position with the right knee flexed to 30°. Inadequate flexion may lead to the inability to completely visualize the iliotibial (IT) band. The right lateral femoral epicondyle, the right head of the fibula, and the right Gerdy tubercle are marked. The right proximal-lateral portal, which will be used for the camera, is created with a No. 11 blade scalpel, and the trocar is inserted with angulation toward the lateral femoral condyle. The distal portal, which will be the working portal, is created over the lateral femoral condyle with a spinal needle and the No. 11 blade scalpel. The spinal needle is visualized by the arthroscopic camera located in the proximal portal before proceeding. At this time, a complete bursectomy is performed deep to the IT band with the arthroscopic shaver (Smith & Nephew) inserted into the distal portal to ensure appropriate IT band visualization. Hemostasis is achieved with the Arthrocare-1 wand. Metzenbaum scissors are used to spread the tissue of the overlying skin and thereby protect it. The lengthening is then performed proximally, distally, anteriorly, and posteriorly with the Metzenbaum scissors in the distal-lateral portal. It is then completed by use of the Arthrocare-1 wand. During these steps, the camera remains in the proximal portal. Care is taken to ensure a complete lengthening is performed to minimize the risk of recurrent IT band syndrome.
References
- 1.Lavine R. Iliotibial band friction syndrome. Curr Rev Musculoskelet Med. 2010;3:18–22. doi: 10.1007/s12178-010-9061-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van der Worp M.P., van der Horst N., de Wijer A., Backx F.J., Nijhuis-van der Sanden M.W. Iliotibial band syndrome in runners: A systematic review. Sports Med. 2012;42:969–992. doi: 10.2165/11635400-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 3.Ellis R., Hing W., Reid D. Iliotibial band friction syndrome—A systematic review. Man Ther. 2007;12:200–208. doi: 10.1016/j.math.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Tenforde A.S., Sayres L.C., McCurdy M.L., Collado H., Sainani K.L., Fredericson M. Overuse injuries in high school runners: Lifetime prevalence and prevention strategies. PM R. 2011;3:125–131. doi: 10.1016/j.pmrj.2010.09.009. quiz 131. [DOI] [PubMed] [Google Scholar]
- 5.Renne J.W. The iliotibial band friction syndrome. J Bone Joint Surg Am. 1975;57:1110–1111. [PubMed] [Google Scholar]
- 6.Strauss E.J., Kim S., Calcei J.G., Park D. Iliotibial band syndrome: Evaluation and management. J Am Acad Orthop Surg. 2011;19:728–736. doi: 10.5435/00124635-201112000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Noble C.A. Iliotibial band friction syndrome in runners. Am J Sports Med. 1980;8:232–234. doi: 10.1177/036354658000800403. [DOI] [PubMed] [Google Scholar]
- 8.Fredericson M., Wolf C. Iliotibial band syndrome in runners: Innovations in treatment. Sports Med. 2005;35:451–459. doi: 10.2165/00007256-200535050-00006. [DOI] [PubMed] [Google Scholar]
- 9.Wanich T., Hodgkins C., Columbier J.A., Muraski E., Kennedy J.G. Cycling injuries of the lower extremity. J Am Acad Orthop Surg. 2007;15:748–756. doi: 10.5435/00124635-200712000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Gunter P., Schwellnus M.P. Local corticosteroid injection in iliotibial band friction syndrome in runners: A randomised controlled trial. Br J Sports Med. 2004;38:269–272. doi: 10.1136/bjsm.2003.000283. discussion 272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Michels F., Jambou S., Allard M., Bousquet V., Colombet P., de Lavigne C. An arthroscopic technique to treat the iliotibial band syndrome. Knee Surg Sports Traumatol Arthrosc. 2009;17:233–236. doi: 10.1007/s00167-008-0660-5. [DOI] [PubMed] [Google Scholar]
- 12.Drogset J.O., Rossvoll I., Grontvedt T. Surgical treatment of iliotibial band friction syndrome. A retrospective study of 45 patients. Scand J Med Sci Sports. 1999;9:296–298. doi: 10.1111/j.1600-0838.1999.tb00249.x. [DOI] [PubMed] [Google Scholar]
- 13.Hariri S., Savidge E.T., Reinold M.M., Zachazewski J., Gill T.J. Treatment of recalcitrant iliotibial band friction syndrome with open iliotibial band bursectomy: Indications, technique, and clinical outcomes. Am J Sports Med. 2009;37:1417–1424. doi: 10.1177/0363546509332039. [DOI] [PubMed] [Google Scholar]
- 14.Cowden C.H., III, Barber F.A. Arthroscopic treatment of iliotibial band syndrome. Arthrosc Tech. 2014;3:e57–e60. doi: 10.1016/j.eats.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martens M., Libbrecht P., Burssens A. Surgical treatment of the iliotibial band friction syndrome. Am J Sports Med. 1989;17:651–654. doi: 10.1177/036354658901700511. [DOI] [PubMed] [Google Scholar]
- 16.Sangkaew C. Surgical treatment of iliotibial band friction syndrome with the mesh technique. Arch Orthop Trauma Surg. 2007;127:303–306. doi: 10.1007/s00402-006-0152-3. [DOI] [PubMed] [Google Scholar]
- 17.Richards D.P., Alan Barber F., Troop R.L. Iliotibial band Z-lengthening. Arthroscopy. 2003;19:326–329. doi: 10.1053/jars.2003.50081. [DOI] [PubMed] [Google Scholar]
- 18.Holmes J.C., Pruitt A.L., Whalen N.J. Iliotibial band syndrome in cyclists. Am J Sports Med. 1993;21:419–424. doi: 10.1177/036354659302100316. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is in the supine position with the right knee flexed to 30°. Inadequate flexion may lead to the inability to completely visualize the iliotibial (IT) band. The right lateral femoral epicondyle, the right head of the fibula, and the right Gerdy tubercle are marked. The right proximal-lateral portal, which will be used for the camera, is created with a No. 11 blade scalpel, and the trocar is inserted with angulation toward the lateral femoral condyle. The distal portal, which will be the working portal, is created over the lateral femoral condyle with a spinal needle and the No. 11 blade scalpel. The spinal needle is visualized by the arthroscopic camera located in the proximal portal before proceeding. At this time, a complete bursectomy is performed deep to the IT band with the arthroscopic shaver (Smith & Nephew) inserted into the distal portal to ensure appropriate IT band visualization. Hemostasis is achieved with the Arthrocare-1 wand. Metzenbaum scissors are used to spread the tissue of the overlying skin and thereby protect it. The lengthening is then performed proximally, distally, anteriorly, and posteriorly with the Metzenbaum scissors in the distal-lateral portal. It is then completed by use of the Arthrocare-1 wand. During these steps, the camera remains in the proximal portal. Care is taken to ensure a complete lengthening is performed to minimize the risk of recurrent IT band syndrome.