Abstract
The most common procedure to address transverse glenoid fractures that are characterized by intra-articular step-off or gapping is open reduction and internal fixation. Disadvantages of open surgery are delay in regaining full range of motion, increased approach morbidity, neurovascular complications, and the need for capsulotomy, which delays healing and increases the risk of stiffness. An arthroscopically assisted fracture fixation, as described in this article, is characterized by better visualization of the glenoid articular surface and reduction of the intra-articular fragments under direct vision, which diminishes the chances of residual step-off after fixation. Furthermore, arthroscopic fixation provides the advantages of minimal surgical trauma, which speeds up the recovery time, decreased morbidity as there is less blood loss compared with the open technique, lower chance of neurologic injury as there is less dissection around the spinoglenoid or suprascapular notch, less trauma to the joint capsule, and lower chances of stiffness and capsulorrhaphy arthropathy.
Fractures of the glenoid that extend to the body of the scapula are usually the result of high-energy trauma. Most of these fractures can be treated in a nonoperative fashion with good outcomes if there is no involvement of the articular surface of the glenoid, no displacement of the glenoid fragments, and no intra-articular step-off or gapping. Posterior or anterior approaches to the scapular body, glenoid neck, or articular surface are characterized by soft tissue trauma, disruption of blood flow to the fracture site, risk of neurovascular injury, and delayed recovery. In addition, there is a risk of weakness and stiffness after open capsulotomies through a posterior or anterior approach to the glenoid. The open exposure and anatomic reduction as well as visualization of the glenoid articular surface can be challenging, especially in obese or muscular individuals. There are reports of arthroscopic treatment of glenoid fractures that are characterized by a transverse fracture line that separates the glenoid fossa from the rest of the scapula with superior to inferior screw fixation.1, 2
We report on an arthroscopic surgical technique for fixation of transverse intra-articular glenoid fractures with or without scapular extension. This technique allows fixation of the intra-articular component of the scapular fracture and permits through superior inferior lag screw insertion, fixation of the glenoid fracture, and conversion to an extra-articular scapular fracture.
Technique
Preoperative Workup
Patient selection and appropriate workup of the trauma victim are key components for successful treatment. The scapular body and glenoid fractures are the result of high-energy trauma, and initial workup of the fracture requires anterior-posterior, Grashey, scapular Y, and axillary views of the affected shoulder. Computed tomography with 3D reconstruction and possible segmentation of any free bony fragments that may be interposed between the articular superior and inferior glenoid fossa are helpful in preoperative planning.
Patient Positioning and Setup
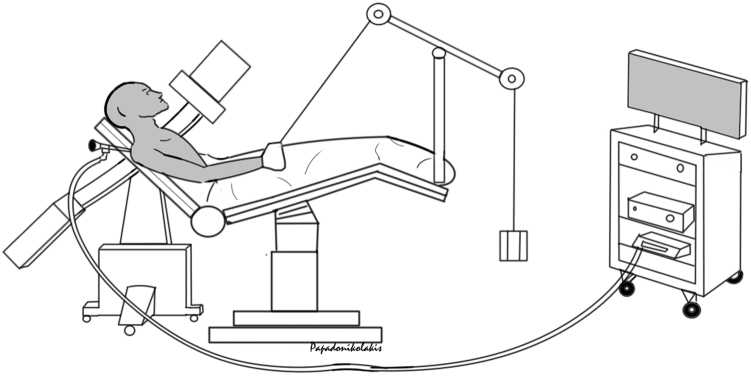
The patient is placed in the beach chair position, which permits easier fluoroscopic imaging during the procedure or conversion to open technique should that be required. Fluoroscopic images are taken prior to prepping and draping the patient to verify visualization of the fracture. The C-arm is brought into the field from the opposite site. Ten to 15 pounds of traction is applied to the affect extremity with a traction arm device (Fig 1).
Fig 1.
The patient is placed in the beach chair position; the arthroscopy tower should be away from the C-arm. The C-arm is introduced in the field from the opposite side. Ten to 15 pounds of traction are applied to the affected arm with a traction device during the arthroscopic procedure. The traction should be eliminated when obtaining Grashey radiographs; this maneuver will allow the scapula to “fall back” and make the radiographic Grashey view of the glenoid more accurate.
Procedure
Step 1: Portal Placement
The arthroscopic procedure is initiated by establishment of the posterior portal first. This is placed 1.5 to 3 cm distal and 1 to 2 cm medial to the posterolateral tip of the acromion. Avoid placement of this portal too far laterally, which makes visualization of the glenoid articular surface more difficult. A 30° arthroscope is inserted through the posterior portal. At this point of the procedure, the articular fracture will be visualized (Fig 2). The anterior portal is established using an outside-in technique. This is accomplished through the rotator cuff interval between the inferior edge of the supraspinatus and the superior edge of the subscapularis muscle/tendon. A spinal needle is used first for identification of the insertion point. The insertion point is usually halfway between the anterior inferior edge of the acromion and the most superior axillary skin fold, which can be identified with internal rotation of the shoulder and adduction. It is recommended to place this anterior portal as superior as possible and close to the supraspinatus tendon, which will allow enough space for placement of a second anterior portal. The second anterior portal is placed in a similar fashion inferior to the first anterior portal and just superior to the superior edge of the subscapularis in the rotator cuff interval to permit maximum spacing between the 2 anterior portals. The increased space between the 2 anterior portals allows ease of instrument insertion and manipulation within the joint.
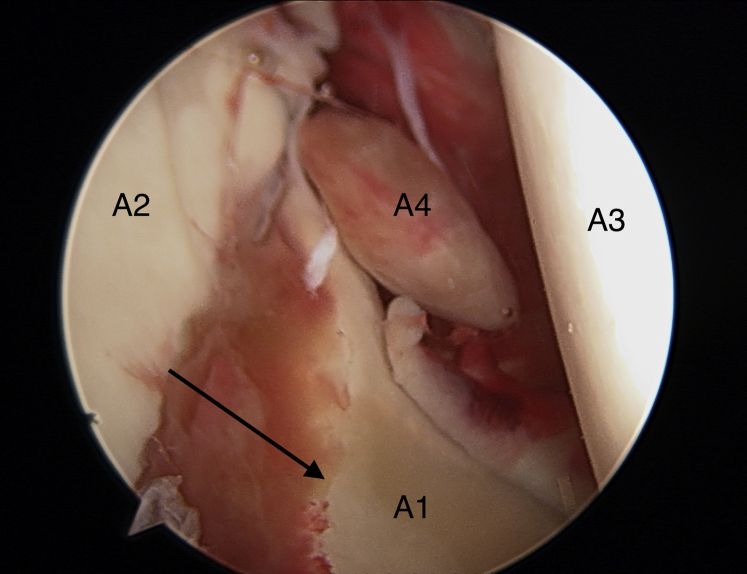
Fig 2.
Right shoulder. Viewing from the posterior portal the glenoid fossa and the transverse fracture with 5 mm of gapping (arrow). A1 indicates the inferior glenoid fragment and A2 the superior fragment. A3 represents the humeral head and A4 a loose body.
Step 2: Fracture Evaluation and Debridement of Fracture Hematoma
Any loose intra-articular fragments are removed using an arthroscopy shaver or tissue grasper that is inserted over a cannula through the anterior portal as the joint is viewed through the posterior portal. The diagnostic arthroscopy is completed by assessment of the orientation and position of the fracture. This is accomplished by viewing from the posterior portal and then inserting the 30° arthroscope through the anterior portal for better understanding of the fracture orientation. With the arthroscope in the posterior portal, the fracture hematoma is debrided with the use of a 4.0- or 3.5-mm arthroscopy shaver (Arthrex, Naples, FL) and/or electrocautery (ArthroCare; Smith & Nephew, London, England) through the anterior portal (Fig 3). Sometimes, a portion of the labrum anteriorly may need to be debrided to allow for complete visualization, taking care not to remove any labrum in the anterior inferior area of the glenoid rim, which may cause an iatrogenic Bankart lesion. Any interposed bony fragments that may be blocking reduction of the glenoid fracture are removed with a tissue grasper (Fig 4). Mobilization of any interposed bony fragments prior to removal can be achieved with a probe. In subacute fractures, a Bankart elevator inserted through the anterior portal can be used to mobilize the bony fragments.
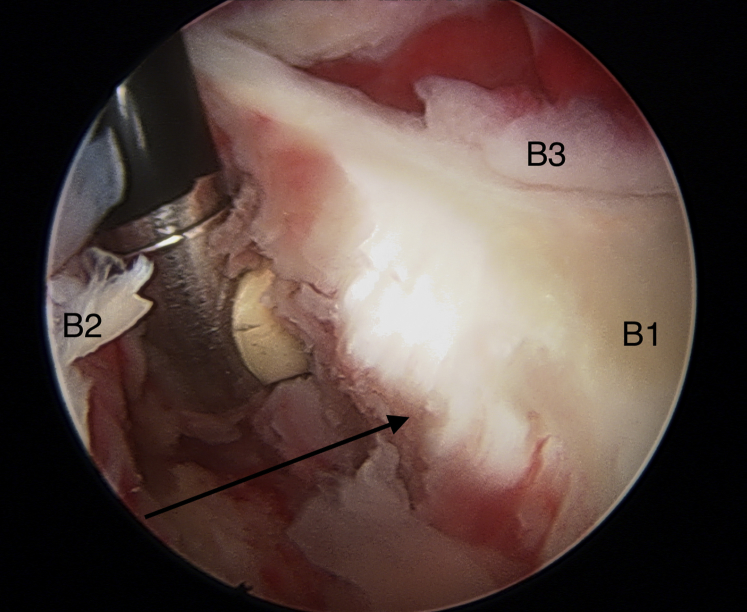
Fig 3.
Right shoulder. Viewing from the posterior portal the ArthroCare wand is inserted through the anterior portal in the fracture site (arrow) between the superior (B2) and inferior (B1) fragments for debridement of the hematoma and exposure of the interposed bony fragment. The anterior labrum is indicated (B3).
Fig 4.
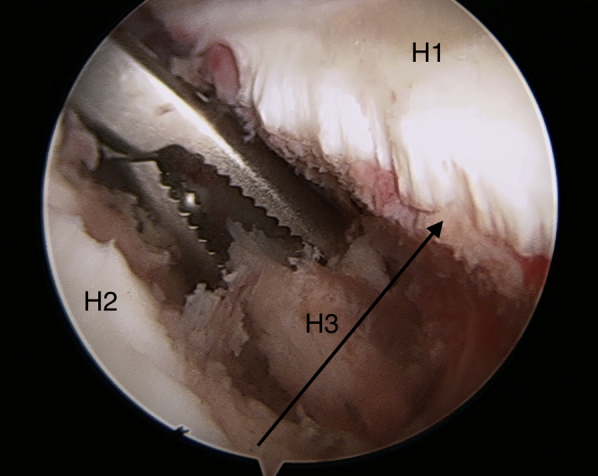
Right shoulder. The fracture site (arrow) is viewed from the posterior portal, and the superior (H2) and inferior glenoid bony fragments (H1) are indicated. The interposed fracture fragments (H3) in the fracture site (arrow) are removed with a tissue grasper.
Step 3: Fracture Manipulation, Reduction, and Insertion of Cannulated Screw Guidewires
Through an arthroscopy cannula, a threaded K-wire is inserted through the anterior portal in the superior and then in the inferior glenoid bony fragment to identify the most mobile fragment (Fig 5). The K-wire is inserted and advanced 1 to 2 cm at the rim of the glenoid. The K-wire should be threaded to usually 0.045 inch in size to avoid pullout during manipulation. By applying traction to the K-wire that is inserted first on the superior and then on the inferior glenoid fragment, the most mobile fragment will be identified. The K-wire is left in place in the most mobile fragment and the Neviaser portal is used for insertion of a spinal needle and selection of the proper trajectory for cannulated screw fixation. The assistant holds the reduction by the pull or manipulation of the threaded K-wire with the main goal to eliminate any step-off or fragment rotation and not necessarily the gapping. The closure of the gapping is usually achieved by the later lag screw insertion. Two cannulated screw guidewires are placed from the posterior superior glenoid rim through the Neviaser portal to the anterior inferior glenoid. At this point, the arthroscope is in the posterior portal and the fracture site is visualized. The cannulated screw guidewires crossing the fracture site will be visualized (Fig 6). Minimal advancement of the guidewires to the inferior glenoid fragment is recommended (Fig 7). The arthroscope is then removed from the joint and the C-arm is brought in the field from the opposite site. A Grashey radiograph of the shoulder is obtained. At this stage of the procedure, removal of the arm from the traction arm device will allow the scapula to “fall back.” This maneuver facilitates in obtaining a true Grashey view of the shoulder. Final advancement of the 2 guidewires to the inferior glenoid fragment is performed under fluoroscopic guidance, which will allow avoidance of penetration of the far or inferior glenoid cortex, which minimizes the risk for injury to the axillary nerve or artery. In addition, the fluoroscopy facilitates to verify a proper insertion point lateral to the suprascapular notch and away from the articular margin of the glenoid rim to prevent the screw head from abrading the humeral head articular cartilage (Video 1). The 2 guidewires provide rotational control of the fracture. The C-arm is then removed from the field and the arthroscope is inserted through the posterior portal to assess the reduction of the fracture.
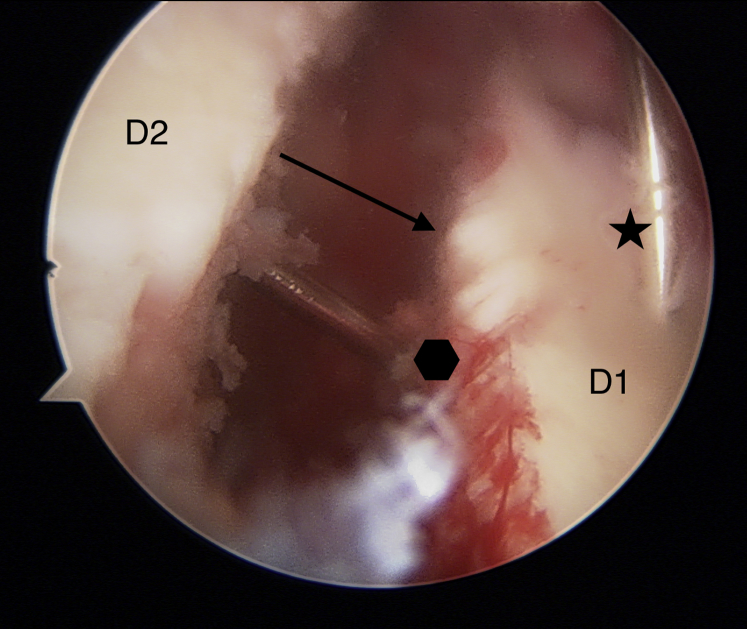
Fig 5.
Right shoulder, viewing from the posterior portal. The fracture site (arrow) is depicted, with the lag screw guidewire (polygon) being advanced from the superior (D2) to the inferior (D1) glenoid bony fragment. The asterisk shows the K-wire, which is inserted in the anterior rim of the glenoid and is used for rotational control of the fragments.
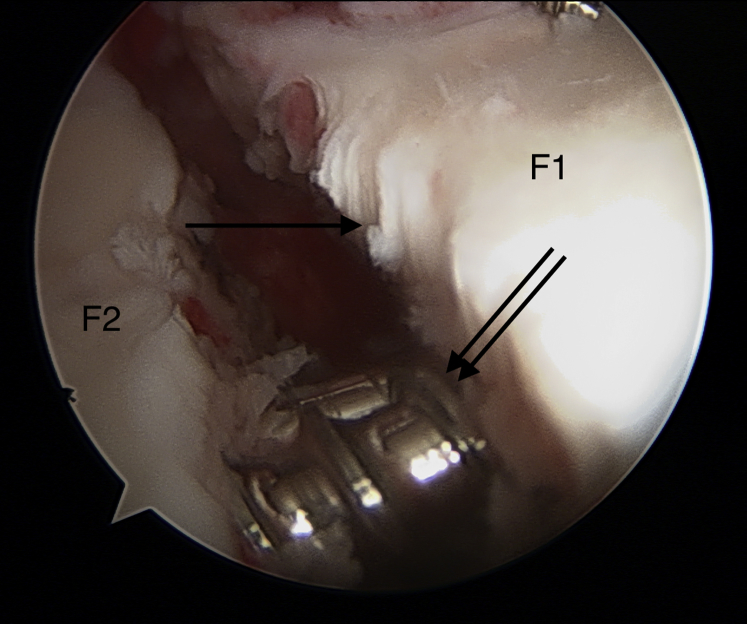
Fig 6.
Right shoulder, viewing from the posterior portal. The crossing (double arrow) of the lag screws is seen in the fracture site (single arrow) from the superior (F2) to the inferior (F1) glenoid fragment.
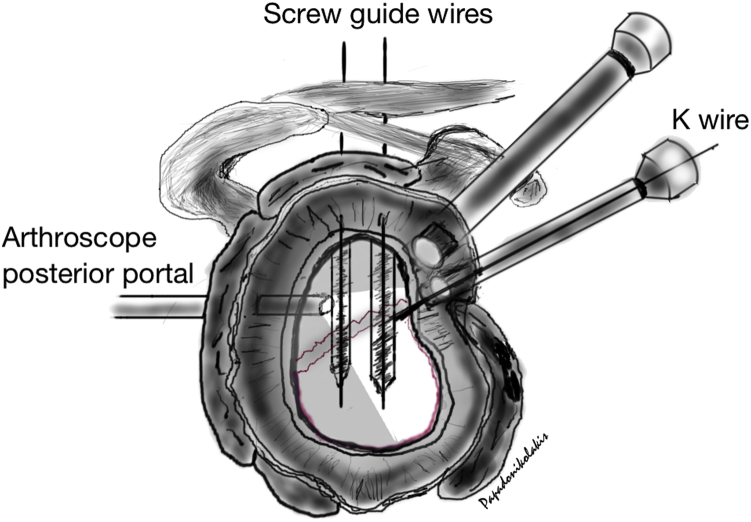
Fig 7.
Drawing of the glenoid showing the insertion point of the lag screw guidewires, the arthroscope is inserted in the posterior viewing portal, the anterior portals are established, and 2 arthroscopy cannulas are inserted. The threaded K-wire is inserted through the anterior portal for manipulation of the articular glenoid bony fragment.
Step 4: Insertion of the Cannulated Lag Screws
The guidewires exiting the Neviaser portal is measured to determine the appropriate screw length before a 2.7-mm cannulated drill bit is used to drill the outer cortex of the superior glenoid fracture fragment only. Further advancement of the drill bit is not recommended as this maneuver may lead to advancement of the screw guidewire and penetration of the inferior or far glenoid cortex in the axilla endangering the axillary nerve or artery. During measurement of the screw length, fluoroscopic confirmation may be needed to verify seating of the measuring device on the bone. The screw length is selected based on the measured guidewire length and is shortened by 2 mm to prevent screw penetration through the far or inferior glenoid cortex. The partially threaded 4.0-mm cannulated screws (Smith & Nephew) are then inserted, and under direct visualization through the posterior portal the screws are advanced sequentially to the inferior glenoid fragment to avoid loss of reduction. Compression of the articular surface and closure of the intra-articular gap is usually seen during this step of the procedure as shown in Video 1 and Figure 8. Final confirmation of the correct placement of the screws is completed with fluoroscopy (Fig 9). It is recommended to remove the guidewires before the final fluoroscopic images are obtained. The arthroscope is then inserted again through the posterior portal for verification of removal of all loose intra-articular fragments and irrigation of the shoulder joint. The procedure is completed by closure of the skin portals and placement of a sling.
Fig 8.
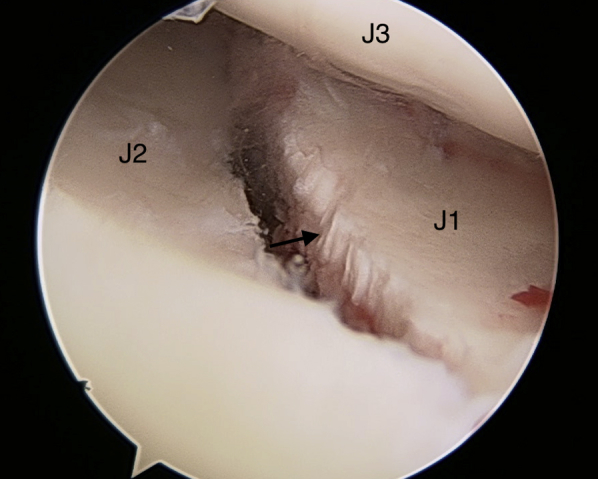
Viewing from the posterior portal—right shoulder. The fracture gap (arrow) is closed down to 1 mm, between the superior (J2) and inferior (J1) glenoid fragments after advancement of the lag screws. The articular surface of the humeral head is also depicted (J3).
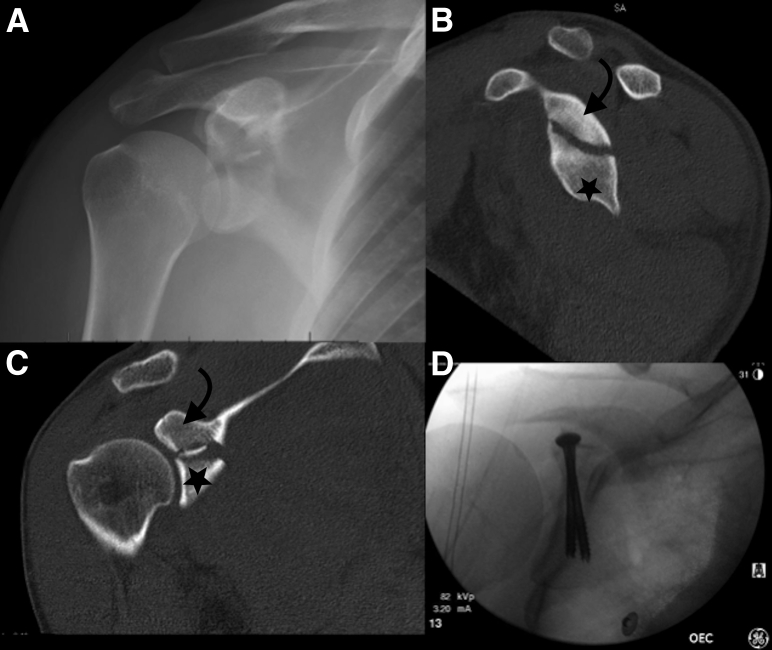
Fig 9.
Preoperative anteroposterior radiograph (A), sagittal CT image (B), coronal CT image (C), and postoperative Grashey view (D) after fixation of the transverse glenoid fracture using two 4.0-mm cannulated lag screws. The arrow indicates the superior and the asterisk the inferior glenoid bony fragment. After fixation, there is no intra-articular step-off, and there is closure of the gapping that is seen on the preoperative radiograph. (CT, computed tomographic.)
Rehabilitation Protocol
Postoperatively, the affected shoulder is placed in a sling for 3 weeks. Active and passive range of motion to the elbow and wrist is permitted. Active range of motion to the shoulder is not permitted at this stage. Pendulum exercises are allowed. At 4 weeks, passive range of motion to the shoulder or assistive forward elevation to 140° is permitted. At 6 weeks postoperatively, active range of motion to the shoulder is allowed with a weight lifting restriction of 5 to 7 pounds. Strengthening exercises are allowed at 3 months after surgery. Return to contact sports is permitted at 6 months after surgery if there is radiographic healing of the fracture.
Discussion
Glenoid fracture fixation requires technical skill because of the proximity of the neurovascular structures around the glenoid. The arthroscopic fixation of transverse glenoid fractures is characterized by minimal soft tissue dissection and disruption of the blood flow to the fractured fragments, easier evaluation of the articular surface of the glenoid, and direct visualization of fracture reduction2 when compared to open surgery. The direct visualization of the articular surface of the glenoid permits more accurate reduction of the step-off and elimination of the gapping at the fracture site. Fixation of a transverse fracture of the glenoid that extends to the body of the scapula has the benefit of conversion of an articular fracture to a nonarticular fracture of the body of the scapula that can be approached conservatively. This minimally invasive approach allows for faster mobilization with the theoretically lower risk of postoperative infection compared with open surgical techniques.
In addition, there is less blood loss than in open surgery and less soft tissue dissection around the glenoid rim, which has a lower theoretical risk of capsulorrhaphy arthropathy. Alternative arthroscopically assisted techniques that require a mini open or open approach for manipulation of the fragments or placement of reduction clamps on the coracoid increase the complexity of surgery, may result in poor arthroscopic visualization due to bleeding within the shoulder joint, or increased fluid outflow and loss of shoulder joint distention from the large-sized surgical wounds. Although the technique described in this paper may not be suitable for multifragmentary intra-articular fractures, simple articular glenoid fractures can be fixed in a minimally invasive approach that shortens the recovery time associated with the surgical trauma of open surgery. The avoidance of large incisions minimizes postoperative pain from soft tissue dissection that is required in the open or mini open arthroscopically assisted approaches. Arthroscopic surgery is expensive compared with open surgery; however, the cost can be balanced from the faster recovery and shortened period of postoperative physical therapy.
Appropriate placement of the portals around the shoulder requires understanding of the 3-dimensional alignment of the fracture, which can be facilitated with a preoperative 3-dimensional computed tomographic scan. Wrong placement of the portals or long arthroscopy cannulas that may be required for obese or muscular patients may complicate the surgery. The complexity lies in the difficulty to manipulate the bony fragments with the K-wires as there is limited freedom for cannula movement within the shoulder joint. Caution is advised to avoid bending of the wires in those situations. Guidewire bending can also happen as they enter the shoulder through the Neviaser portal. This is usually the result of manipulation or removal of arm from traction to allow the scapula to “fall back” in order to obtain a true Grashey radiograph, which assists in the assessment of the fracture reduction or provisional fracture fixation.
Another critical aspect of this surgical technique is to downsize the screw length, because it is difficult to accurately assess the screw length during arthroscopy. Downsizing by 2 or 4 mm from the measured screw length minimizes the risk of far cortex penetration, which can result in vascular or nerve injury. Furthermore, it is preferred to use partially threaded cannulated lag screws that achieve better compression across the fracture site. To avoid loss of rotational control of the fragments, it is recommended to advance one screw at a time sequentially and use 2 screws instead of 1. The insertion point of the cannulated screw guidewire must be under the labrum, away from the articular surface, to avoid prominence of the head screws and contact with the humeral head, which can cause cartilage abrasion.
The beach chair position is preferred because it makes fluoroscopy easier and conversion to open surgery faster and easier compared to the lateral decubitus position. This is critical because in the event of vascular injury there is an interval time between skin incision for conversion to open surgery, soft tissue dissection, and control of the bleeding with a vascular clamp. Cautious advancement of the cannulated drill bit over the guidewires under fluoroscopy, especially when the tip of the guidewire aims toward the axilla, is essential for safety and avoidance of vascular injury from the tip of the guidewire. In addition, it is preferred to stop drilling and advancement of the cannulated drill bit over the guidewire 5 mm proximal to the guidewire tip. This maneuver reduces the risk of accidental removal of the guidewire when the drill bit is withdrawn from the drill hole. In the event of suspected vascular injury, palpation of the axilla is suggested for possible fullness and of the radial artery at the wrist bilaterally to evaluate for asymmetry in the pulses. During the early phases of the learning curve, vascular surgery availability is suggested depending on the arthroscopy skills of the orthopaedic surgeon performing the procedure (Tables 1 and 2).
Table 1.
Advantages and Disadvantages of Arthroscopic Fixation of Glenoid Fractures
| Advantages | Disadvantages |
|---|---|
| Minimal surgical trauma to soft tissues | More expensive than open technique |
| Lower infection rate, less dissection | Technically demanding for multifragmentary articular fractures |
| Lower risk of stiffness because of scar tissue | |
| Direct visualization and fracture reduction | Not suitable for scapular body fractures |
| Less pain than open surgery | Arthritis from prominent head of the screws |
| Faster recovery than open surgery | Risk of suprascapular nerve injury |
| Less blood loss than open surgery | Risk of axillary nerve or artery injury |
| Lower chances of arthritis | Not suitable for obese patients |
Table 2.
Pearls and Pitfalls of Arthroscopic Fixation of Glenoid Fractures
| Pearls | Pitfalls |
|---|---|
| Appropriate planning of portal placement is essential: wrong portal placement complicates the K-wire trajectories, extends surgical time, and increases risk for neurovascular injury. In the beach chair position, one can convert to open surgery easier than the lateral position. Downsizing the length of the screws is essential to avoid injury to the neurovascular structures. Partially threaded cannulated screws achieve better fracture compression than fully threaded. Tightening of the screws sequentially, one at a time, results in better control and alignment of the fracture. |
Exact screw length is difficult to judge arthroscopically. Muscular or obese patients may require long cannulas, which makes fragment manipulation challenging. Excessive manipulation of the shoulder during fluoroscopy and after placement of the cannulated screw guidewires may result in bending of the guidewires. Revision surgery usually requires an open approach. Vascular injuries may not be seen immediately. Conversion to open surgery adds to the time required for bleeding control. During the learning curve, vascular surgery backup may be required depending on the arthroscopy skills of the orthopaedic surgeon. |
Tao et al.1 reported a similar technique for fixation of these fractures and proposed manipulation of the fracture using a reduction clamp that is placed on the coracoid. Our experience has been that occasionally Type 4 or 5 Ideberg glenoid fractures that extend to the body of the scapula have an intra-articular inferior glenoid fossa fragment that is more mobile than the superior glenoid fragment, which may be in continuity with the coracoid. In addition, our technique requires less arthroscopic dissection. Yang et al.2 reported good outcomes at 2 years for glenoid fractures without extension to the body of the scapula (Ideberg 3). A similar technique to ours has been reported by Tuman et al.3; however, a posterior inferior portal was used for visualization of the fracture, which can be helpful when the transverse fracture line is in the lower one-third of the glenoid.
Safe placement of the guidewires and knowledge of the anatomy of the neurovascular structures located around the glenoid rim are imperative for good outcomes free of complications. It has been shown that superior placement of the guidewires through the Neviaser portal or anteromedial to the AC joint are safe techniques with minimal risk of suprascapular nerve injury. More specifically, it has been shown that the superior portion of the glenoid is accessible by percutaneous screw insertion between the clock times 7:40 and 2:50, apart from positions occupied by the coracoid (1:05-2:00) and acromion (9:35-10:55).4 Long-term outcomes of arthroscopic fixation of glenoid fractures with extension to the scapular body are lacking; however, this approach is promising in reducing complications and the morbidity associated with open surgery.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Preoperative evaluation, technique, and final imaging after arthroscopic fixation of the transverse glenoid fracture. Viewing from the posterior portal throughout the video demonstration—right shoulder. The patient is in the beach-chair position. The glenoid is seen at the bottom left of the screen (7 o'clock position) and the humeral head at the top right of the screen (1 o’ clock position). The surgical instruments are inserted through the anterior portals as well as the K-wire needed for rotational control of the inferior articular glenoid fragment.
References
- 1.Tao M.A., Garrigues G.E. Arthroscopic-assisted fixation of Ideberg type III glenoid fractures. Arthrosc Tech. 2015;4:e119–e125. doi: 10.1016/j.eats.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang H.B., Wang D., He X.J. Arthroscopic-assisted reduction and percutaneous cannulated screw fixation for Ideberg type III glenoid fractures: A minimum 2-year follow-up of 18 cases. Am J Sports Med. 2011;39:1923–1928. doi: 10.1177/0363546511408873. [DOI] [PubMed] [Google Scholar]
- 3.Tuman J.M., Bishop J.A., Abrams G.D. Arthroscopic reduction and internal fixation of an inferior glenoid fracture with scapular extension (Ideberg V) Arthrosc Tech. 2015;4:e869–e872. doi: 10.1016/j.eats.2015.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marsland D., Ahmed H.A. Arthroscopically assisted fixation of glenoid fractures: A cadaver study to show potential applications of percutaneous screw insertion and anatomic risks. J Shoulder Elbow Surg. 2011;20:481–490. doi: 10.1016/j.jse.2010.08.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preoperative evaluation, technique, and final imaging after arthroscopic fixation of the transverse glenoid fracture. Viewing from the posterior portal throughout the video demonstration—right shoulder. The patient is in the beach-chair position. The glenoid is seen at the bottom left of the screen (7 o'clock position) and the humeral head at the top right of the screen (1 o’ clock position). The surgical instruments are inserted through the anterior portals as well as the K-wire needed for rotational control of the inferior articular glenoid fragment.