Abstract
As technology continues to improve, surgeons must regularly re-evaluate techniques to improve efficacy and outcomes. The Bankart repair for shoulder instability has evolved from open reconstruction to minimally invasive arthroscopic techniques, which have the benefit of less pain and morbidity. This technical description and video present a modern arthroscopic technique for Bankart repair used at our institution with high success in an athletic population.
Bankart repair techniques have improved significantly over the last 90 years since Bankart initially described this lesion. The open Bankart repair was the gold standard for years, with success rates ranging from 75% to 100%1, 2, 3; however, postoperative problems such as restriction to external rotation and secondary osteoarthritis were concerns.4 Arthroscopic Bankart repair gained popularity since it began almost 30 years ago because of improved arthroscopic equipment and increased experience of surgeons.5, 6, 7 Compared with open Bankart repair, arthroscopic Bankart repair gives the potential advantages of smaller skin incisions, shorter surgical times, less postoperative pain, decreased blood loss, decreased narcotic usage, decreased rates of complications, and improved shoulder motion.8, 9, 10, 11 First-generation arthroscopic techniques demonstrated higher recurrence rates than the more modern arthroscopic techniques,11, 12, 13, 14 but as techniques and implants continued to improve, results have become comparable to the open gold standard.1, 12, 15, 16, 17 Initial arthroscopic fixation was performed by staple capsulorrhaphy, which resulted in unacceptable levels of recurrent instability. Other methods of fixation have included transosseous suturing and bioabsorbable tacks, both of which have had lower success rates than open repairs.11 As technology evolved, modern day suture anchors were developed that have improved the success of arthroscopic repair. We present here a modern arthroscopic technique for Bankart repair used at our institution.
Surgical Technique
Step 1: Preoperative Planning
Obtaining a thorough history is the first step in evaluating a patient with shoulder instability. It is important to inquire about the mechanism of injury, the direction of the instability, and the method of reduction. The surgical plan and workup may change depending on the chronicity of the problem. The surgeon will want to know if this is an acute first-time dislocator or a chronic dislocator who has had numerous subluxation or dislocation events. If the instability is recurrent, we will inquire about activities or events that may lead to an instability episode. In general, chronic, recurrent dislocators are more likely to have more significant pathology, including bone loss, which may make arthroscopic repair ill advised.
The history is followed by a comprehensive upper extremity examination. The standard components include inspection, palpation, range of motion, strength, and stability testing. A good neurologic exam is also important to look for axillary nerve or brachial plexus injuries. In the acute setting, some of the examination may be limited because of guarding. For instability patients, we routinely include the apprehension/relocation test and look for a sulcus sign, which may indicate multidirectional instability.
Radiographs are routinely obtained and should include an axillary lateral, true anteroposterior, and scapular Y views. The Stryker-Notch view is also helpful for visualizing Hill-Sachs lesions. Magnetic resonance imaging with arthrogram is part of the standard workup for evaluating the typical injuries associated with a shoulder dislocation and also shows concomitant associated injuries, which are commonly present. Computed tomographic scans of the shoulder are not routinely obtained but are useful if there is evidence or suspicion of glenoid bone loss.
Step 2: Anesthesia and Positioning
A preoperative interscalene block and continuous catheter is used for postoperative pain control and is placed while the patient is in the preoperative holding area. The patient is then taken to the operating room, where general anesthesia is administered. Preoperative antibiotics are administered within 1 hour of the start of the procedure. With the patient supine, both shoulders are examined under anesthesia. Range of motion and laxity are evaluated and documented. Patients are then placed in the lateral decubitus position with a beanbag. All bony prominences are padded and protected. Fifteen pounds of traction is applied to the operative extremity using a traction boom to help with intraoperative glenohumeral distraction.
Step 3: Portal Placement and Diagnostic Arthroscopy
A standard posterior portal is established (Video 1). This is placed 2 cm distal and 1 cm medial to the posterolateral corner of the acromion, parallel to the glenohumeral joint. A spinal needle is used to insufflate the shoulder with 60 mL of arthroscopic fluid. An incision is made and an arthroscopic cannula is used to enter the shoulder joint. A 30° arthroscope (Arthrex, Naples, FL) is placed into the cannula for viewing. Two anterior working portals are then established in the rotator interval from outside in using spinal needle localization (Fig 1). An 8-mm-diameter corkscrew cannula (Smith & Nephew, London, England) is placed lower, just superior to the subscapularis tendon. This cannula is placed low in order to reach the most inferior portion of the glenoid. A 5-mm-diameter corkscrew cannula (Smith & Nephew) is placed higher, just anterior to the biceps tendon (Fig 2). Diagnostic arthroscopy is performed and the pathology is assessed (Fig 3, Fig 4, Fig 5).
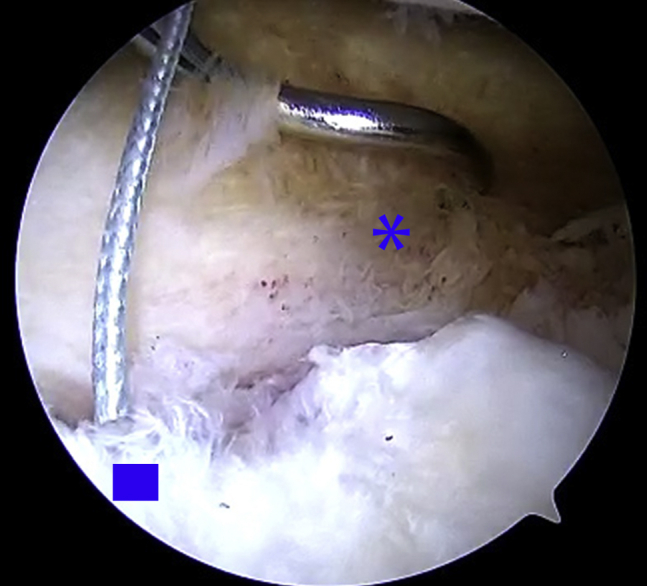
Fig 1.
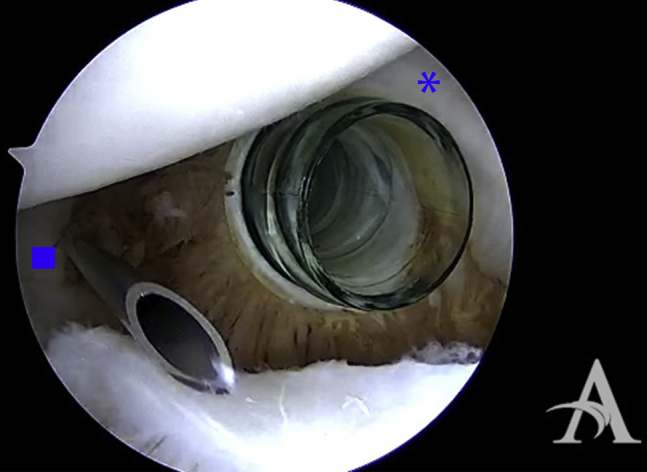
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows placement of the two corkscrew cannulas on either end of the rotator interval. The anterior inferior cannula is in place just superior to the subscapularis tendon (asterisk). A spinal needle is used to find the ideal position for the anterior superior cannula just anterior to the biceps tendon (square). Cannulas are placed to aid in suture management.
Fig 2.
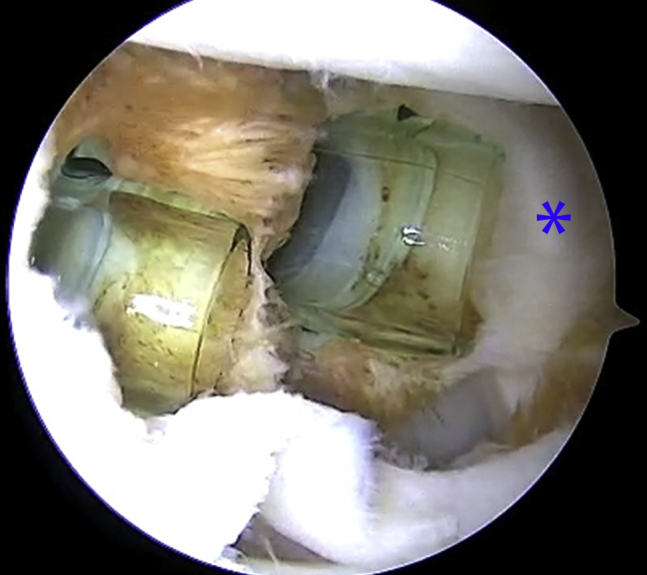
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the cannulas in final position between the subscapularis tendon (asterisk) and the biceps tendon.
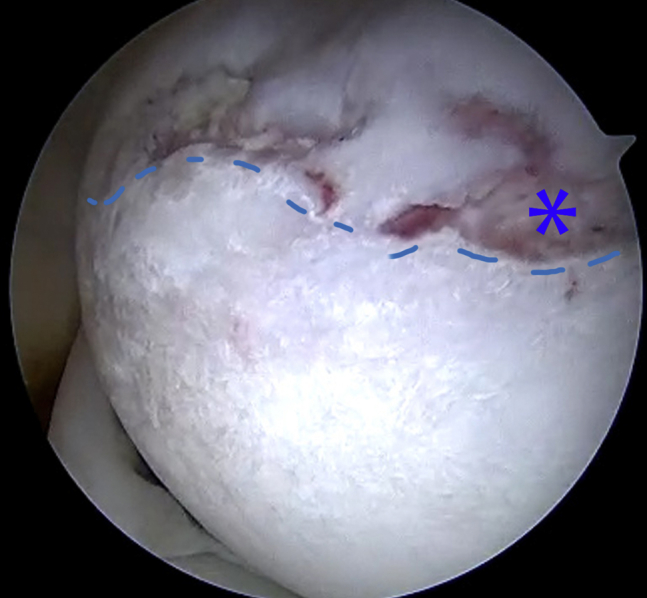
Fig 3.
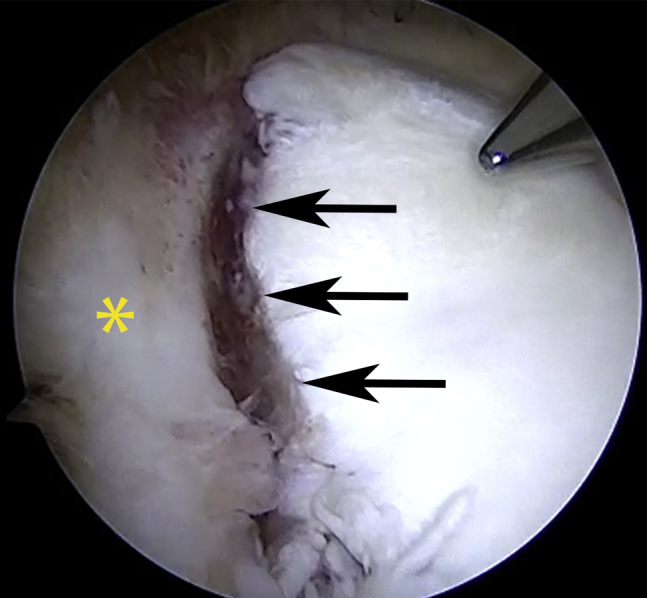
Right shoulder in the lateral decubitus position (viewing from the anterior superior portal) shows the capsulolabral complex (asterisk) avulsed from the anterior inferior glenoid rim (arrows) consistent with a Bankart Lesion.
Fig 4.
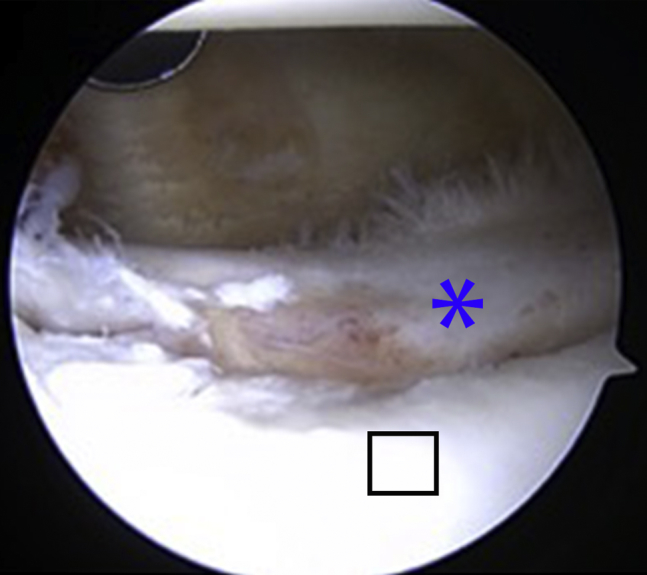
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the labral tear (asterisk) torn away from the anterior glenoid (black square).
Fig 5.
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows a Hill-Sachs lesion (asterisk) on the posterior aspect of the humeral head. The dotted line shows the demarcation of normal cartilage to the impacted portion superiorly.
Step 4: Glenoid Preparation
A 30° arthroscopic tissue liberator (Arthrex) is used to elevate and free up the labrum from the anterior glenoid, which is often scarred down in a nonanatomic, medialized position (Fig 6). This is an important step as incomplete mobilization of the anterior labrum from the glenoid neck may result in a nonanatomic, less functional repair. The subscapularis muscle can be seen anteriorly when this tissue is sufficiently elevated off the anterior glenoid neck. An arthroscopic rasp (Arthrex) is used to prepare the anterior capsular tissue for better healing after plication (Fig 7). A small 3.5-mm burr (Smith & Nephew) is then used to create a bleeding bed of bone along the neck of the glenoid (Fig 8). This completes glenoid and soft tissue preparation (Fig 9).
Fig 6.
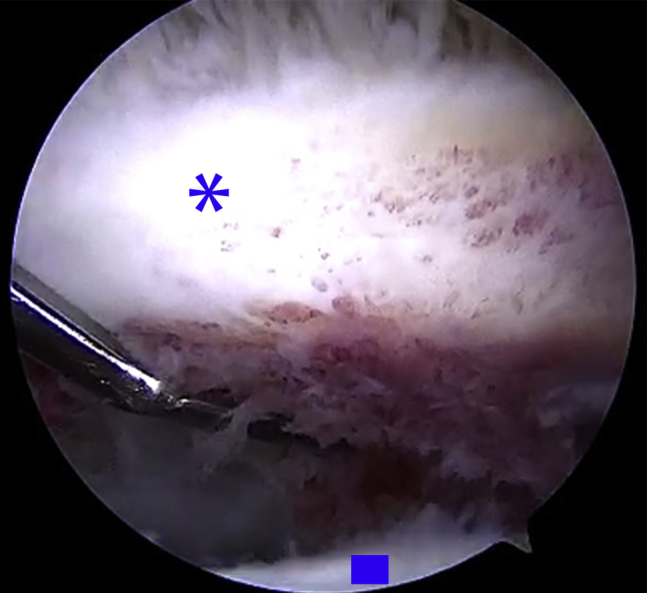
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the 30° elevator being used to free the capsulolabral complex (asterisk) from its healed medial position on the glenoid (square) from the anterior portal. Sufficient release is critical to reposition this tissue back to its anatomic position. The pink hue of the subscapularis muscle can be seen deep in the lower left of the image in the cleft deep to the capsule.
Fig 7.
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows an arthroscopic rasp being used from the anterior inferior cannula to prepare the redundant capsular tissue prior to plication. This will stimulate a healing response. The asterisk marks the labral tissue that has been freed from its previous medialized position on the glenoid.
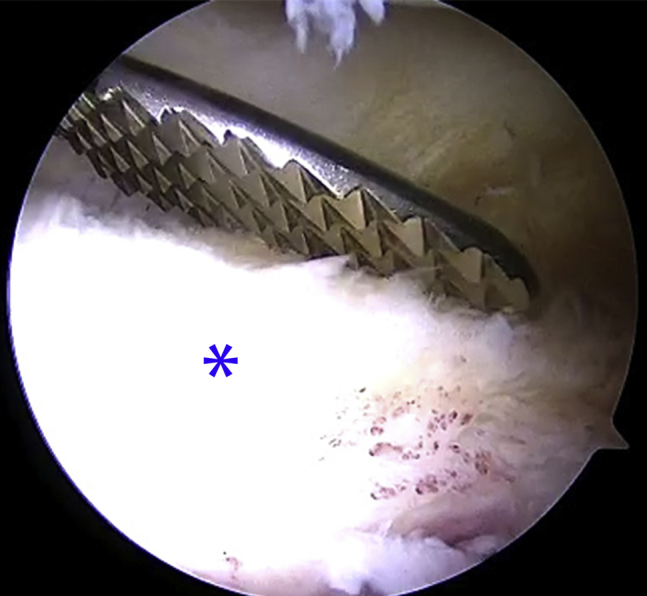
Fig 8.

Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the 3.5-mm sheathed burr used to prepare the anterior glenoid rim from the anterior portal. The goal is to gently abrade the bone to create bleeding and stimulate a repair response. The sheath protects the capsulolabral complex (asterisk) from being damaged by the burr.
Fig 9.

Right shoulder in the lateral decubitus position (viewing from the anterior superior portal) shows the prepared glenoid surface to promote healing to the capsulolabral complex (asterisk) once it is reduced and stabilized.
Step 5: Anchor Placement and Capsulolabral Plication
While viewing from the posterior portal, the drill guide for the suture anchor (SutureTac biocomposite 3 mm × 14.5 mm, Arthrex) is introduced through the inferior cannula and is positioned onto the face of the glenoid as close to the 6 o'clock position as possible (Fig 10). The stout metal drill guide can be used to lever the humeral head slightly out of the way to get the best possible angle in the glenoid to prevent skiving and cartilage injury. If the most inferior position on the glenoid cannot be reached from the anterior cannula, a percutaneous portal through the subscapularis tendon can be used. A drill is used to create a pilot hole, and the anchor is then tapped into the glenoid. A suture-retrieving grasper (Arthrex) is used to grasp one limb of suture from the anchor and pull it out through the 5-mm cannula. A curved suture passer (Spectrum, ConMed, Utica, NY) loaded with a no. 1 polydioxanone (PDS) suture is used to pierce the capsule and is advanced under the capsule and labrum in 1 pass (Fig 11). The goal is to get a healthy capsular bite, grabbing inferior to the anchor in an effort to shift the tissue superiorly, reducing capsular volume. The PDS is advanced out of the passer and into the joint, where it is grasped and pulled out of the 5 mm cannula. The suture passer is removed from the shoulder. A simple loop is then made with the PDS that was pulled out of the 5-mm cannula. This loop is loaded with the anchor suture and cinched down (Fig 12). The PDS limb that is in the 8-mm cannula is pulled, shuttling the suture limb through the tissue and out of the cannula.
Fig 10.
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the drill guide being placed low on the glenoid face (asterisk) around the 5:30 position. A pilot hole is drilled and a suture anchor is placed. If the angle to drill the anchor is not possible from the anterior superior portal, a percutaneous portal through the subscapularis tendon must be created.
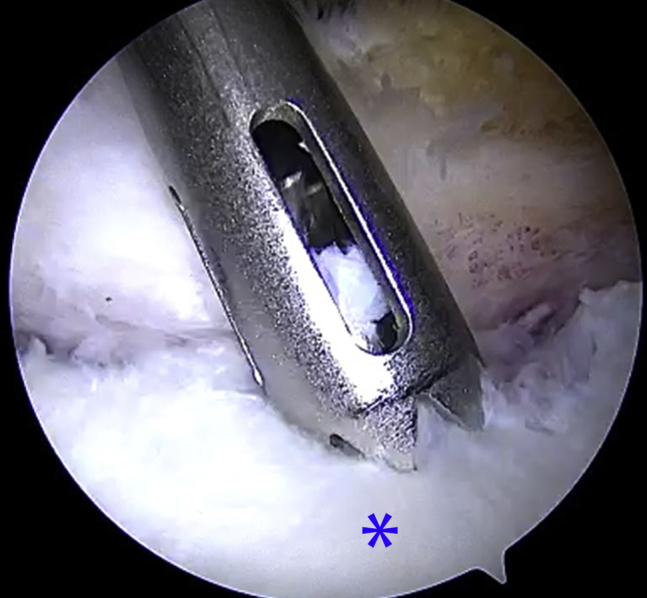
Fig 11.
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the Spectrum curved suture passer (ConMed, Utica, NY) being used through the anterior inferior portal to pierce the capsule (asterisk) approximately 1 cm distal and 5 to 10 mm anterior to the drilled anchor (square). When the suture is tied, this will shift the capsular tissue superiorly and plicate redundant capsular tissue.
Fig 12.

Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the grasper being used through the anterior superior portal to grab the PDS suture and one limb of the passed FiberWire suture (Arthrex, Naples, FL). The PDS is then tied around the FiberWire suture outside of the body and the PDS is pulled back through the tissue, bringing the FiberWire suture into position for knot tying. (PDS, polydioxanone.)
Step 6: Knot Tying and Sequential Anchor Placement
Knots are tied arthroscopically using low-profile sliding locking Westin knots followed by half hitches with care to keep the knots away from the glenoid face, in an effort to prevent articular cartilage injury from the suture (Fig 13). Suture tails are cut with the arthroscopic cutters, leaving a small 2-mm tail. Subsequent anchors are placed in similar fashion, working superiorly on the glenoid (Fig 14). Previous studies have demonstrated that the use of fewer than 4 anchors will increase the likelihood of recurrent instability.18, 19 Therefore, a minimum of 4 to 6 anchors are used depending on the size of the patient. Anchors are placed as close to each other as possible without compromising fixation of the previous anchor. This re-creates a stabilizing “bumper” effect on the anterior glenoid and ensures multiple points of fixation (Figs 15 and 16).
Fig 13.
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows both limbs of the FiberWire suture (Arthrex, Naples, FL) being pulled out of the anterior inferior cannula. The suture that has been passed through the tissue should act as the post, which keeps the knot off the glenoid. Sliding locking arthroscopic knots with half hitches are used to stabilize the capsulolabral complex (asterisk) to the front of the glenoid, creating a “bumper” effect.
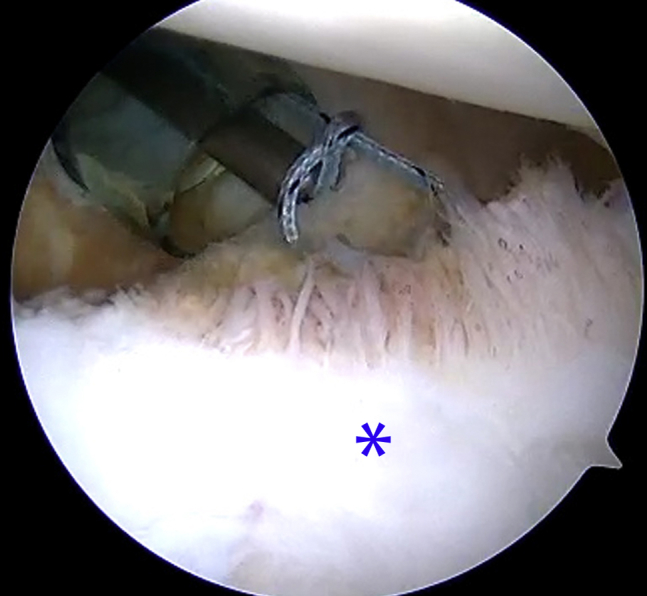
Fig 14.

Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the next anchor being drilled 3 to 4 mm proximal to the previous anchor (asterisk) with the proper 45° angle. The anchor is placed and steps are repeated to pass and tie sutures.
Fig 15.
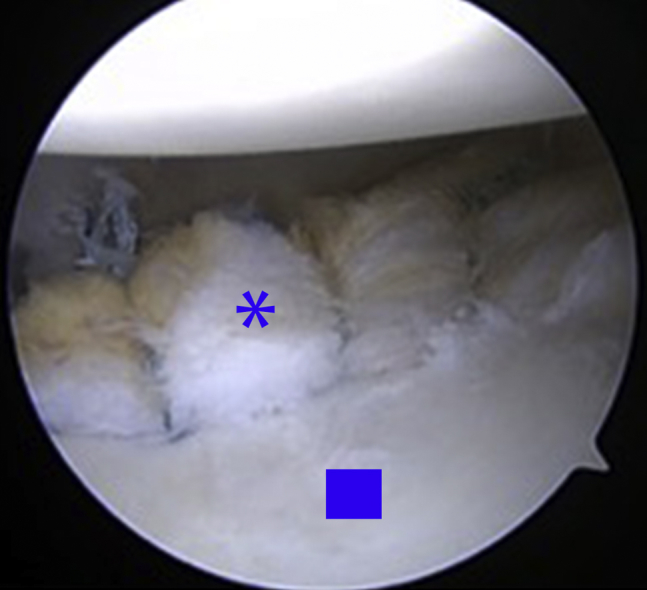
Right shoulder in the lateral decubitus position (viewing from the posterior portal) shows the final construct with multiple anchors (4-6) used to reduce and stabilize the capsulolabral complex (asterisk) back to its anatomic position on the glenoid (square) while creating a sufficient “bumper” to prevent recurrent dislocation.
Fig 16.
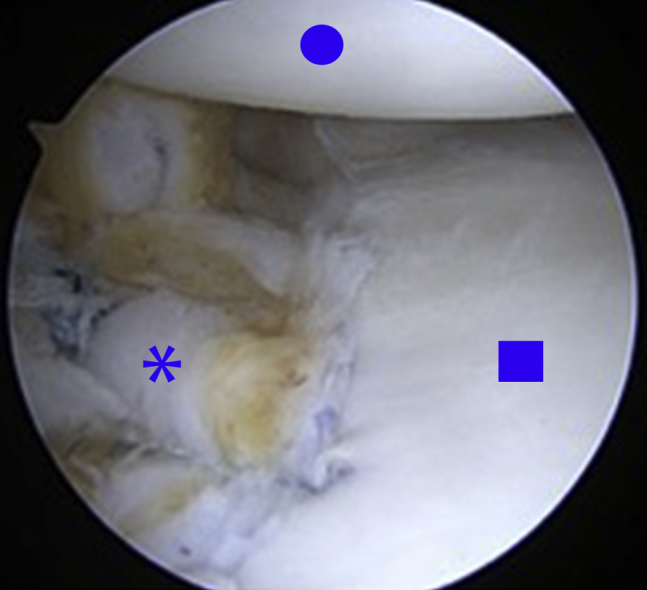
Right shoulder in the lateral decubitus position (viewing from the anterior superior portal) shows the final construct. The capsulolabral complex (asterisk) has been reduced and stabilized back to the anterior glenoid (square) with superior capsular shift and plication. The humeral head is seen in the upper portion of the image (circle).
Step 7: Skin Closure and Shoulder immobilization
Nonabsorbable sutures are used to close the skin. Sterile dressings are applied to the surgical incisions. Patients are placed in a shoulder immobilizer and rolled to the recovery area. Standard postoperative assessment in the recovery room is performed on all patients. The patients are discharged home with an indwelling perineural catheter for postoperative pain control. The catheter is typically removed by the patient in 3 to 4 days.
Postoperative Rehabilitation
A shoulder immobilizer is worn for 6 weeks. Phase 1 (weeks 0-6) goals include protecting the anatomic repair, preventing the negative effects of immobilization, promoting dynamic stability and proprioception, and diminishing pain and inflammation. Passive and gentle active assistive range of motion (ROM) exercises are begun, but no active external rotation, extension, or abduction is allowed. During weeks 5 to 6, the patient works to gradually improve ROM with gentle stretching exercises. Phase 2 (weeks 7-14) goals include working to gradually restore full ROM (ideally by week 10), restoring muscular strength and balance, and enhancing neuromuscular control. More aggressive strengthening and ROM are progressed to meet functional demands (i.e., overhead athlete). Phase 3 (weeks 15-20) goals include improving muscular strength, power, and endurance and gradually initiating functional activities. Next, the advanced strengthening phase (weeks 21-24) goals include enhancing muscular strength, power, and endurance, progressing functional activities, and maintaining shoulder mobility. Lastly, the return to activity phase (months 7-9) goals include a gradual return to sport activities while maintaining strength, mobility, and stability. The protocol may be modified slightly based on the athlete's goals, revision versus primary cases, and the tissue quality at the time of surgery.
Discussion
We recently published data on 94 shoulders undergoing Bankart repair using this technique.12 This athletic population included collegiate and professional athletes. At an average follow-up of 5 years (range 3-9 years), the success rate was 93.6%, with only 6 recurrences. 82.5% of athletes were able to return to the same level of sport. There were no recurrences in the collegiate or professional athletes, including National Football League players. There were no recurrences in the revision cases.
Risk factors for recurrent instability include recurrent trauma, younger age, male sex, increased number of dislocations, prior procedures, bone defects of the glenoid or humeral head, humeral avulsion of the glenohumeral ligament lesions, and capsular laxity.20 Technical errors such as excessive medialization of anchors, “high” placement of the most inferior anchor, insufficient number of anchors, and improper suture configuration are other factors that may lead to failure of repair.20
Advantages of arthroscopic Bankart repair include smaller skin incisions, shorter surgical times, less postoperative pain, decreased blood loss, decreased narcotic usage, decreased rates of complications, and improved shoulder motion (Table 1).8, 9, 10, 11 Disadvantages include relatively long learning curve to master this technique, expensive instrumentation, and lack of long-term data on modern day implants.21 Pearls for successful execution of an arthroscopic Bankart repair include precise portal placement and adequate mobilization of the capsulolabral sleeve so that it can be placed onto the face of the glenoid in an anatomic position. Preparation of the glenoid is also important. Sufficient burring of the anterior glenoid generates healthy bleeding bone to stimulate a healing response. It is also important to use a sufficient number of anchors to create multiple points of fixation and the strongest repair possible. Previous studies have demonstrated that the use of fewer than 4 anchors will increase the likelihood of recurrent instability.18, 19 Therefore, our goal is to use a minimum of 4 to 6 anchors, depending on the size of the patient (Table 2).
Table 1.
Advantages and Disadvantages of Arthroscopic Versus Open Bankart Repair
| Advantages: |
| - Smaller incisions |
| - Less postoperative pain |
| - Shorter surgical times |
| - Decreased complications |
| - Improved shoulder range of motion |
| Disadvantages: |
| - Technically difficult |
| - Long learning curve |
| - Expensive equipment |
| - Higher recurrent instability rates with older techniques/devices |
Table 2.
Pearls for Successful Arthroscopic Bankart Repair
| - Perform thorough diagnostic arthroscopy of the shoulder to confirm concomitant pathology that may alter the surgical plan. |
| - Place anterior portals on opposite ends of the rotator interval. The anterior inferior portal should be at the superior edge of the subscapularis tendon so that the most inferior area of the glenoid can be reached. Place the anterior superior portal just anterior to the biceps tendon to allow an accessory portal for viewing and passing or tying sutures. Use a spinal needle to confirm location before creating the portals. |
| - Adequate mobilization of the capsulolabral sleeve from the medialized position on the glenoid neck to fixate onto the face of the glenoid, creating a “bumper” of tissue along the rim. |
| - Adequate preparation of the anterior glenoid rim with a burr to stimulate a healing response. Do not remove bone; only remove scar and periosteal tissue to expose the underlying bleeding bone. |
| - Grab a healthy capsular bite, shifting the tissue superiorly and plicating the tissue to decrease the capsular volume. |
| - Use 4-6 anchors with a simple suture configuration, starting as low on the glenoid as possible and working superiorly. Tie stable arthroscopic knots away from the articular surface. |
Pitfalls include failure to recognize pathology that may make arthroscopic repair unsuccessful, such as excessive bone loss or humeral avulsion of the glenohumeral ligament lesions (Table 3). Technical pitfalls include placing anchors too far medially on the glenoid neck, resulting in a nonanatomic, ineffective repair. Failure to plicate and superiorly shift the capsule may lead to excessive capsular volume and recurrent instability. Arthroscopic knots should stay off the glenoid to avoid erosion of the humeral head cartilage.
Table 3.
Pitfalls to Avoid When Performing Arthroscopic Bankart Repair
| - Failure to address concomitant pathology (i.e., glenoid bone loss or Hill-Sachs lesions) |
| - Place anchors on the glenoid face, not along the anterior glenoid rim. |
| - Failure to shift and plicate tissue will lead to excessive capsular volume |
| - Failure to use multiple points of fixation (<4-6) will lead to a weak repair |
| - Return to play before proper healing and rehabilitation (around 6-9 months depending on quality of tissue and repair) |
The arthroscopic Bankart repair, when using modern and current techniques and implants, is a successful option for shoulder instability, even with the higher-risk contact athlete. Although current arthroscopic techniques are significantly more successful than first-generation techniques, there is still room for improvement as surgical skill, technology, and implants evolve.
Acknowledgment
The authors acknowledge Jim Sims for his assistance with the video production.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.O. receives support from Mitek, OnQ (consultancy fees) and research and fellowship support from Arthrex.
Supplementary Data
Right shoulder viewed from a standard posterior portal (and some shots from the anterior portal) shows the steps of repair of a Bankart Lesion using multiple suture anchors along the anterior glenoid rim. The capsulolabral complex is freed from its medialized position on the glenoid neck with the elevator. The rasp is used to stimulate a healing response along the redundant capsule during later plication. The burr is used to prepare the anterior glenoid rim. Multiple anchors are drilled and placed along the anterior glenoid rim. The sutures are passed through the capsular tissue shifting it superiorly and decreasing capsular volume. Arthroscopic sliding knots are tied to reduce and stabilize this tissue back to its anatomic position.
References
- 1.An V.V., Sivakumar B.S., Phan K., Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 2016;25:853–863. doi: 10.1016/j.jse.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Hubbell J.D., Ahmad S., Bezenoff L.S., Fond J., Pettrone F.A. Comparison of shoulder stabilization using arthroscopic transglenoid sutures versus open capsulolabral repairs: A 5-year minimum follow-up. Am J Sports Med. 2004;32:650–654. doi: 10.1177/0095399703258747. [DOI] [PubMed] [Google Scholar]
- 3.Freedman K.B., Romeo A.A., Cole B.J., Bach B.R. Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for recurrent anterior instability of the shoulder: A meta-analysis. Am J Sports Med. 2004;32:1520–1527. doi: 10.1177/0363546504265188. [DOI] [PubMed] [Google Scholar]
- 4.Owens B.D., Cameron K.L., Peck K.Y. Arthroscopic versus open stabilization for anterior shoulder subluxations. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115571084. 2325967115571084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green M.R., Christensen K.P. Arthroscopic versus open Bankart procedures: A comparison of early morbidity and complications. Arthroscopy. 1993;9:371–374. doi: 10.1016/s0749-8063(05)80308-1. [DOI] [PubMed] [Google Scholar]
- 6.Speer K.P., Deng X., Borrero S. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am. 1994;76:1819–1826. doi: 10.2106/00004623-199412000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Cole B.J., L'Insalata J., Irrgang J., Warner J.J. Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82:1108–1114. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Arciero R.A., Taylor D.C., Snyder R.J., Uhorchak J.M. Arthroscopic bioabsorbable tack stabilization of initial anterior shoulder dislocations: A preliminary report. Arthroscopy. 1995;11:410–417. doi: 10.1016/0749-8063(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 9.Bacilla P., Field L.D., Savoie F.H., 3rd Arthroscopic Bankart repair in a high demand patient population. Arthroscopy. 1997;13:51–60. doi: 10.1016/s0749-8063(97)90209-7. [DOI] [PubMed] [Google Scholar]
- 10.Kartus J., Ejerhed L., Funck E. Arthroscopic and open shoulder stabilization using absorbable implants. A clinical and radiographic comparison of two methods. Knee Surgery Sports Traumatol Arthrosc. 1998;6:181–188. doi: 10.1007/s001670050096. [DOI] [PubMed] [Google Scholar]
- 11.Levy D.M., Cole B.J., Bach B.R. History of surgical intervention of anterior shoulder. J Shoulder Elbow Surg. 2016;25:e139–e150. doi: 10.1016/j.jse.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 12.Milchteim C., Tucker S.A., Nye D.D. Outcomes of Bankart repairs using modern arthroscopic technique in an athletic population. Arthroscopy. 2016;32:1263–1270. doi: 10.1016/j.arthro.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 13.Arciero R.A., Ryan J.B., McBride J.T. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22:589–594. doi: 10.1177/036354659402200504. [DOI] [PubMed] [Google Scholar]
- 14.Gerometta A., Rosso C., Klouche S., Hardy P. Arthroscopic Bankart shoulder stabilization in athletes: Return to sports and functional outcomes. Knee Surg Sports Traumatol Arthrosc. 2016;24:1877–1883. doi: 10.1007/s00167-014-2984-7. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto N., Nagamoto H., Kurokawa D., Takahashi H., Sano H., Itoi E. Outcome of Bankart repair in contact versus non-contact athletes. Orthop Traumatol Surg Res. 2015;101:415–419. doi: 10.1016/j.otsr.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 16.McRae S., Leiter J., Subramanian K., Litchfield R., MacDonald P. Randomized controlled trial of arthroscopic electrothermal capsulorrhaphy with Bankart repair and isolated arthroscopic Bankart repair. Knee Surg Sports Traumatol Arthrosc. 2016;24:414–421. doi: 10.1007/s00167-015-3543-6. [DOI] [PubMed] [Google Scholar]
- 17.Mohtadi N.G., Chan D.S., Hollinshead R.M. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability. J Bone Joint Surg Am. 2014;96:353–360. doi: 10.2106/JBJS.L.01656. [DOI] [PubMed] [Google Scholar]
- 18.Boileau P., Hery J.V., Balg F., Ahrens P., Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.H., Ha K.I., Kim S.H. Bankart repair in traumatic anterior shoulder in-stability: Open versus arthroscopic technique. Arthroscopy. 2002;18:755–763. doi: 10.1053/jars.2002.31701. [DOI] [PubMed] [Google Scholar]
- 20.Ho A.G., Gowda A.L., Michael Wiater J. Evaluation and treatment of failed shoulder instability procedures. J Orthop Traumatol. 2016;17:187–197. doi: 10.1007/s10195-016-0409-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang L., Liu Y., Su X., Liu S. A meta-analysis of arthroscopic versus open repair for treatment of Bankart lesions in the shoulder. Med Sci Monit. 2015;21:3028–3035. doi: 10.12659/MSM.894346. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Right shoulder viewed from a standard posterior portal (and some shots from the anterior portal) shows the steps of repair of a Bankart Lesion using multiple suture anchors along the anterior glenoid rim. The capsulolabral complex is freed from its medialized position on the glenoid neck with the elevator. The rasp is used to stimulate a healing response along the redundant capsule during later plication. The burr is used to prepare the anterior glenoid rim. Multiple anchors are drilled and placed along the anterior glenoid rim. The sutures are passed through the capsular tissue shifting it superiorly and decreasing capsular volume. Arthroscopic sliding knots are tied to reduce and stabilize this tissue back to its anatomic position.


