Abstract
Isolated fractures of the greater tuberosity of the humerus are an uncommon and frequently missed diagnosis. Mistreated and unrecognized, these fractures can cause chronic pain and diminished shoulder range of motion and function. Operative treatment options include open reduction and internal fixation, as well as arthroscopic-assisted reduction and internal fixation. The purpose of this Technical Note is to describe a bridging arthroscopic technique for the treatment of bony avulsions of the supraspinatus tendon.
Isolated fractures of the greater tuberosity (GT) of the humerus account for 19% of all proximal humerus fractures1, 2 and are mainly associated with acute glenohumeral dislocation or with direct trauma to the lateral shoulder.3 The incidence of isolated GT fractures is approximately 12 to 14 cases per 100,000 patients annually.4, 5 This particular fracture pattern occurs most frequently in middle-aged adults and can be easily missed when only minimally displaced.1, 2 The rationale for surgery of a GT fracture is to achieve anatomical reduction to prevent nonoutlet impingement and to restore the function of the rotator cuff. The decision to proceed with surgery is dependent on both patient-specific and fracture-specific factors, including demographics, comorbidities, physical goals, and the expected outcomes. Regarding fracture-specific variables, nondisplaced and minimally displaced (<3 mm) fractures do not necessarily require surgery; however, fractures with displacement greater than 3 mm in athletes and overhead workers and with displacement of more than 5 mm in active patients3 should be treated with surgery. Although open procedures are preferred for comminuted, widely displaced fractures, arthroscopic procedures can be used for multifragment bony avulsions of the supraspinatus tendon and isolated one-part GT fractures with minimal displacement.4, 5 The advantages of arthroscopic procedures are less soft-tissue trauma and blood loss, less peri- and postoperative morbidity, and decreased scar tissue adhesions.6 In addition, concomitant lesions such as labral tears and rotator cuff tears are often associated with fractures of the GT and can be easily diagnosed and addressed arthroscopically.3, 7, 8 In this Technical Note and Video 1, we describe a bridging, knotless arthroscopic technique for the treatment of bony avulsions of the supraspinatus tendon. The advantages and disadvantages of this technique are outlined in Table 1.
Table 1.
Advantages and Disadvantages of the Arthroscopic Surgical Technique
| Advantages | Disadvantages |
|---|---|
| Minimally invasive | Technically challenging |
| Can visualize and address concomitant intra-articular pathology | Limited visibility in cases with significant bleeding |
| Faster recovery | |
| No hardware removal when using a SpeedBridge system (Arthrex, Naples, FL) |
Surgical Technique
Preoperative Imaging
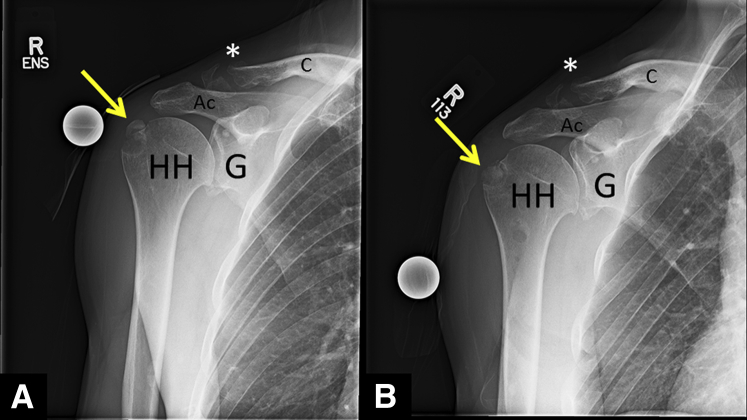
Preoperative evaluation with anteroposterior, Grashey, scapular-Y, and axillary radiographs is obtained and reviewed (Fig 1). Careful attention should be paid to elucidating fracture characteristics and associated fractures, including those of the scapular neck and clavicle. Magnetic resonance imaging evaluation of the shoulder assesses the integrity of the rotator cuff and other soft tissue glenohumeral and subacromial structures. Computed tomography scan can help evaluate humeral head bone stock and defects.
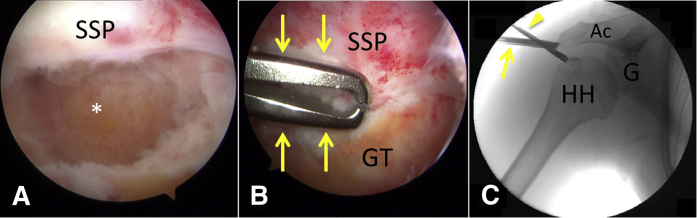
Fig 1.
(A) Anteroposterior view of a right shoulder with a minimally displaced right-sided greater tuberosity fracture nonunion (arrow) and associated mildly displaced distal clavicle fracture (*). (B) Postoperative anteroposterior radiograph of the same shoulder showing the reduction of the fragment (arrow). (Ac, acromion; C, clavicle; G, glenoid; HH, humeral head.)
Anesthesia and Patient Positioning
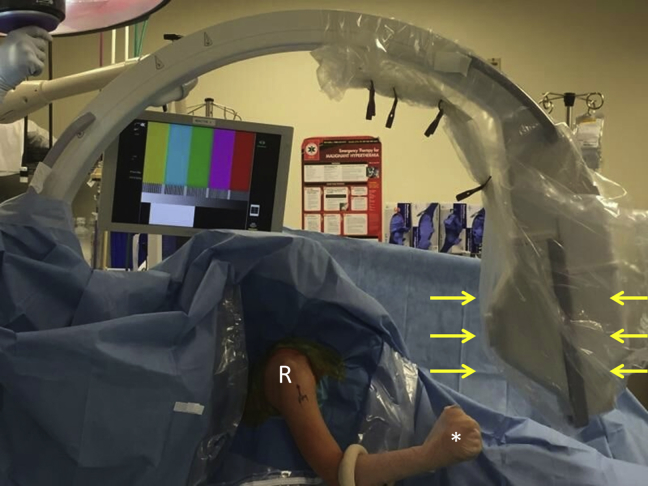
Anesthesia is a combination of general endotracheal anesthesia and interscalene block for postoperative pain control. We use the beach chair position, as it allows the surgeon to address associated injuries (e.g., clavicle fracture), if present, while also allowing the surgeon to conveniently switch to open procedures, if necessary (Fig 2). Beach chair positioning also facilitates C-arm positioning. We prefer to place the bow of the C-arm superiorly with the x-ray tube anterior to the patient's shoulder (Fig 2). The arm is then prepped and draped in a sterile fashion and the operative extremity is situated in a pneumatic arm holder (Tenet T-Max Beach Chair and Spider arm positioner; Smith & Nephew, Memphis, TN).
Fig 2.
Patient prepped and draped in the beach chair position with the right-sided operative upper extremity (R) in a pneumatic arm holder (*). The beach chair position facilitates the use of intraoperative fluoroscopy; the bow of the C-arm is placed superiorly with the x-ray tube (arrows) anterior to the patient's shoulder.
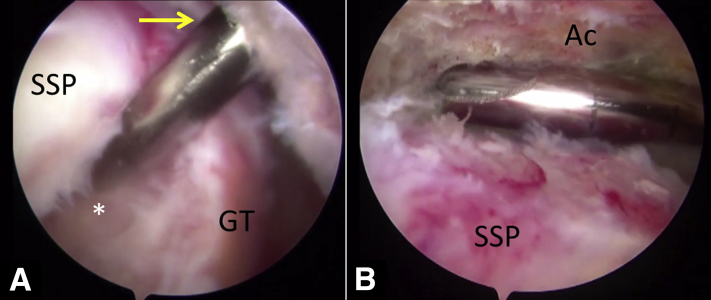
Diagnostic Arthroscopy
The complete surgical technique is shown in Video 1. A standard posterior viewing portal is then created 2 cm inferior and 2 cm medial to the posterolateral corner of the acromion. A standard 30° arthroscope is used to conduct a diagnostic arthroscopy. Afterward, an anterior working portal is established through the rotator interval. All intra-articular pathology is addressed at this time. The arthroscope is then placed in the subacromial space through the posterior portal, and an anterolateral working portal is established 2 cm lateral to the anterolateral corner of the acromion (Fig 3A). All subacromial space pathology is addressed at this time (Fig 3B).
Fig 3.
View of the right shoulder with the arthroscope in the posterior viewing portal. (A) The anterolateral working portal is established (arrow). (B) After establishment of the anterolateral working portal, subacromial space pathology is addressed. The asterisk symbol (*) indicates greater tuberosity fracture. (Ac, acromion; GT, greater tuberosity; SSP, supraspinatus tendon.)
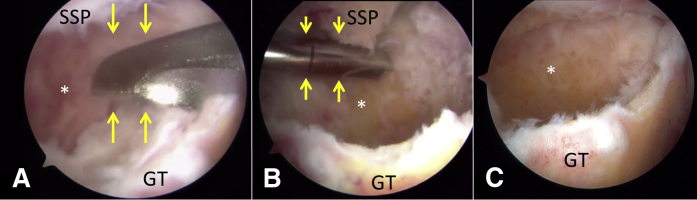
Arthroscopic Reduction and Internal Fixation
Next, the GT fracture is evaluated (Fig 4). If callus is present, it is removed with a combination of instruments, including the arthroscopic shaver and curettes (Fig 4 A and B). A combination of shaver and 5.5-mm burr (Arthrex, Naples, FL) is then used to debride the fracture site to a native anatomical contour (Fig 4C). This step also serves to create a bleeding bone surface conducive to healing. Thereafter, the fracture and torn rotator cuff tendon mobility are evaluated with an arthroscopic grasper (Fig 5). After an anatomic reduction is obtained using the grasper, fracture reduction is confirmed with fluoroscopy (Fig 5C).
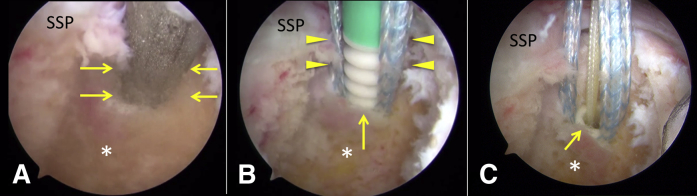
Fig 4.
The right-sided greater tuberosity fracture (*) is visualized with the arthroscope in the anterolateral portal. (A) Removal of the greater tuberosity callus with a curette (arrows). (B) Removal of the greater tuberosity callus with an arthroscopic shaver (arrows). (C) Greater tuberosity fracture after debridement to its native anatomic contour. (GT, greater tuberosity; SSP, supraspinatus.)
Fig 5.
Right shoulder, arthroscopic views of the subacromial space visualized through the anterolateral portal. (A) Arthroscopic view of the crescent-shaped supraspinatus tear and greater tuberosity fracture (*). (B) An arthroscopic grasper (arrows) introduced through the posterior portal is used to assess fracture and rotator cuff mobility. (C) Intraoperative fluoroscopic image confirming anatomic fracture reduction; the arthroscope (arrow) is in the anterolateral portal, whereas the grasper (arrowhead) is in the posterior portal. (Ac, acromion; G, glenoid; GT, greater tuberosity; HH, humeral head; SSP, supraspinatus tendon.)
Next, while the fracture fragment is held in an anatomically reduced position (Fig 5) with a grasper, a knotless self-reinforcing double-row repair with 4 anchors (2 medial and 2 lateral anchors) is performed.9, 10 This construct avoids over-reduction and under-reduction as the fragments are secured on both the medial and lateral sides. Additional anchors may be added when larger fractures need to be fixed.11 The appropriate positions of medial anchors at the cartilage-bone interface just medial to the fracture are first marked using a radiofrequency ablator. Depending on the size of the bony fragment, we recommend maintaining a bone bridge of at least 15 mm between each medial anchor in the anteroposterior direction. With the help of an arthroscopic punch, a bone socket to accommodate the first anchor approximately 1 to 2 mm lateral to the articular margin is created (Fig 6A). A vented 4.75-mm knotless suture anchor loaded with suture tape is placed in this anteromedial socket (BioComposite SwiveLock anchor with FiberTape; Arthrex) (Fig 6 B and C). With an arthroscopic grasper and suture passer (QuickPass SutureLasso; Arthrex), each limb of the suture tape is passed through the rotator cuff tendon approximately 3 to 5 mm medial to the bony fragment (Fig 7). This step is repeated for the posteromedial anchor (Fig 7). Subsequently, a lateral row of anchors is placed in a similar fashion to that of the medial anchors (Fig 8). Again, an arthroscopic punch is used to prepare the anterior-lateral bone socket approximately 5 mm lateral to the edge of the GT fracture while maintaining at least a 15-mm bone bridge from the anteromedial anchor. One limb of suture tape from each medial anchor is retrieved through the anterolateral portal and preloaded into the eyelet of the anterior-lateral anchor. Mild tension is applied through the suture tapes to reduce and compress the bony fragment against the GT (Fig 8A). Intraoperative fluoroscopy in multiple planes is again used to confirm anatomic fracture reduction (Fig 5C). While maintaining adequate tension, the anterolateral anchor is guided into place using a driver and rotated clockwise to achieve bony fixation (Fig 8B). The remaining suture limbs are cut and the procedure is repeated for placement of the posterolateral anchor (Fig 8 C and D). At this point, the shoulder is taken through passive range of motion to confirm a stable, reduced fixation construct under both direct visualization (Fig 9) and fluoroscopy. Pearls and pitfalls of the procedure are outlined in Table 2.
Fig 6.
View of a right shoulder through the anterolateral portal of the first anchor placement medial to the fracture at the level of the articular margin. (A) With the help of an arthroscopic punch (arrows), a bone socket for the first anchor is created 1 to 2 mm lateral to the articular margin. (B) A vented 4.75-mm knotless suture anchor (arrow) loaded with suture tape (arrowheads) is placed in this anteromedial socket. (C) Final view of the first anchor placement (arrow). The asterisk symbol (*) indicates the supraspinatus footprint. (SSP, supraspinatus tendon.)
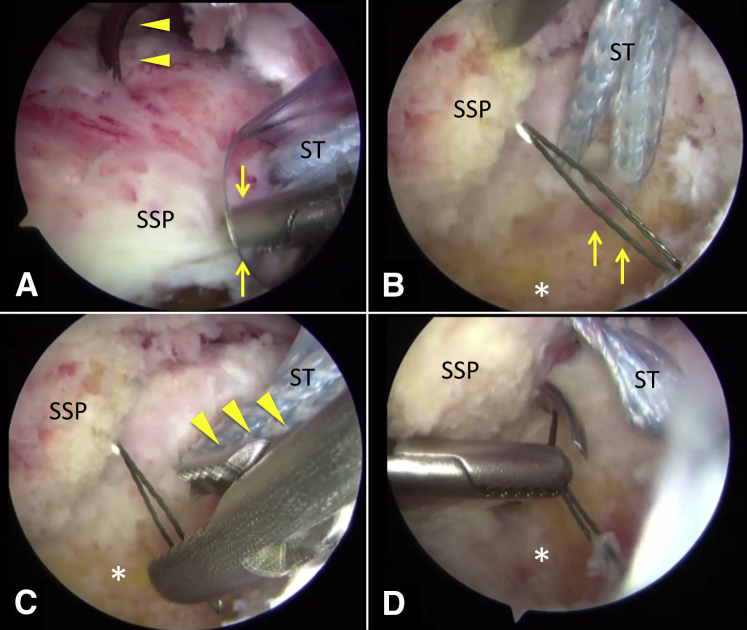
Fig 7.
View of a right shoulder through the posterior portal of passing the medial suture tapes through the rotator cuff tendon. (A) As the supraspinatus tendon (SSP) is held in the anatomic position with the arthroscopic grasper (arrows) via the anterolateral portal, a suture passing device (arrowheads) via the anterior portal is passed through the supraspinatus tendon. (B) Through the suture shuttling device, a nitinol wire is passed (arrows) and (C) retrieved with an arthroscopic grasper (arrowheads) out the anterolateral portal; suture tapes are subsequently passed through the supraspinatus tendon out the anterior portal using the wire (not seen). (D) The process is repeated for the second medial row suture anchor; note that the first suture anchor tapes (ST) have already been passed through the supraspinatus tendon. The asterisk symbol (*) indicates the supraspinatus footprint.
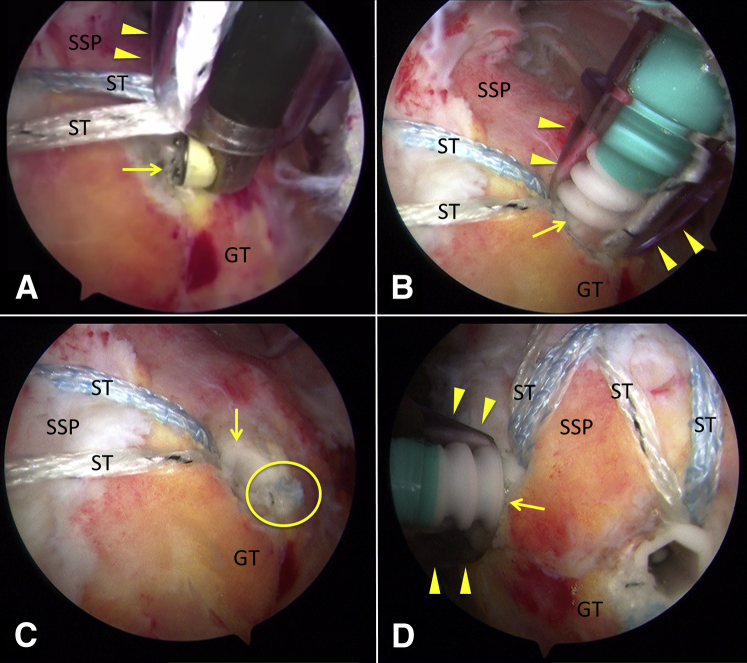
Fig 8.
Arthroscopic view of a right shoulder showing the placement of the lateral row of suture anchors. (A) View through the posterior portal showing the use of a radiofrequency ablator (arrow) to mark the appropriate position of the anterolateral anchor approximately 5 mm lateral to the edge of the greater tuberosity fracture; note that 1 suture tape (ST) from each medial row anchor has already been passed through the anterolateral portal (arrowheads). (B) View through the posterior portal showing the placement of the anterolateral anchor (arrow) via the anterolateral portal (arrowheads); 1 ST from each medial anchor has been preloaded into the eyelet of the anterolateral anchor. (C) View through the posterior portal of the completed anterolateral anchor (arrow) after the ends of the suture tapes (circle) have been cut. (D) View through the anterolateral portal of the posteromedial suture anchor (arrow) being placed via the posterior portal (arrowheads); note that 1 ST from each medial anchor has been preloaded into the eyelet of the posterolateral anchor. (GT, greater tuberosity; SSP, supraspinatus tendon.)
Fig 9.
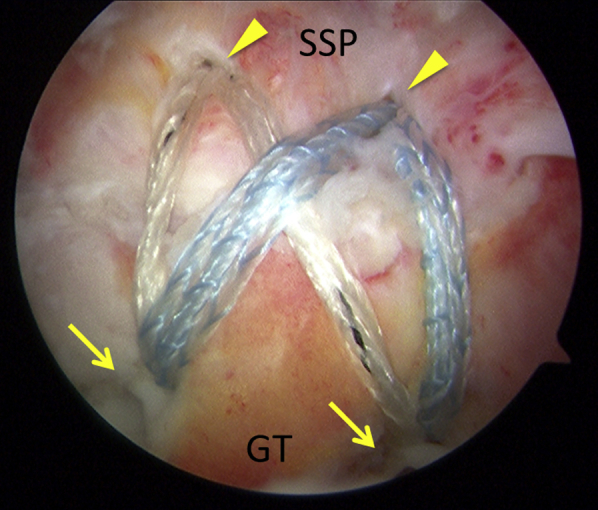
View of the right shoulder through the anterolateral anchor of the completed repair; the construct avoids over-reduction and under-reduction as the fragments are secured on both the medial and lateral sides. The arrows indicate the lateral row of suture anchors, and the arrowheads indicate the medial row of suture anchors. (GT, greater tuberosity; SSP, supraspinatus tendon.)
Table 2.
Pearls and Pitfalls of the Surgical Technique
| Pearls | Pitfalls |
|---|---|
| Position the fluoroscopy machine ahead of time. Placing the bow superiorly with the x-ray beam anterior to the patient's shoulder facilitates easy use throughout the case without limiting exposure | Failing to obtain preoperative advanced imaging can lead to overlooking concomitant injuries, such as rotator cuff tears or secondary fracture patterns |
| Carefully and thoroughly debride the fracture site of any interposed soft tissue and/or callus | Inadequate fracture debridement can prohibit anatomic reduction |
| Hold the fracture fragment in place with a grasper while positioning the lateral row suture anchors | Relying on arthroscopic visualization without the addition of fluoroscopy may lead to malreduction |
Postoperative Rehabilitation
The patient is placed in a sling with abduction pillow. We initiate passive shoulder range of motion immediately if the repair is secure or at 14 days after surgery in more comminuted or less stable situations. Active range of motion of the elbow, wrist, and fingers is initiated immediately. Active shoulder range of motion is begun 4 to 6 weeks postoperatively as clinical examination and radiographic follow-up dictate. Resisted elbow flexion exercises may begin 6 weeks after surgery. Shoulder strengthening exercises are initiated 8 weeks postoperatively.
Discussion
There is a paucity of data in the literature concerning agreed-upon indications for surgical treatment of isolated GT fractures and the corresponding outcomes of such treatment.12, 13
Studies on arthroscopic-assisted GT fracture fixation are limited to individual case reports and case series. Kim and Ha3 retrospectively reviewed 23 patients who underwent arthroscopic-assisted fixation of minimally displaced or nondisplaced GT fractures associated with at least 6 months of chronic shoulder pain. Patients were reassessed at an average of 29 months postoperatively; at that time, University of California, Los Angeles (UCLA) scores were good to excellent in 20 patients and fair in 3 patients. Moreover, 19 patients had returned to previous level of activities. Notably, patients participating in overhead sports had a significantly lower level of return to activity.3 Ji et al.14 retrospectively reviewed 16 patients who underwent arthroscopic double-row suture anchor fixation for comminuted or displaced GT fractures with at least 5 mm of displacement in any plane. Patients were reassessed at an average of 24 months postoperatively. The visual analog scale improved from 9.4 to 1.2, the UCLA score improved to 31 points (3 excellent, 11 good, and 2 poor), and the American Shoulder and Elbow Surgeons score improved to 88.1 points. Mean forward flexion, abduction, external rotation, and internal rotation were 148.7°, 145°, 24°, and to L1, respectively.14 Tsikouris et al.15 investigated the outcomes of arthroscopic-assisted GT fracture fixation on 12 athletes (6 professional, 6 recreational) observed over a 5-year period. No major complications occurred, and all patients achieved UCLA scores over 30 at 6 months. Most notably, all athletes returned to their preoperative activity level with no residual pain.15 Most recently, Liao et al.16 published the largest series in the literature directly comparing arthroscopic to open fixation for GT fractures in 26 versus 53 patients, respectively; the authors found no clinically significant difference in time to union, complications, or outcomes scores between the groups.16
Lin et al.17 compared double-row suture anchor fixation (DR), suture-bridge technique using knotless suture anchor fixation (SB), and two-screw fixation (TS) techniques. Mean force of cyclic loading to create 3 mm of displacement was significantly different among all 3 groups (SB > DR > TS). Mean force of cyclic loading to create 5 mm of displacement and ultimate failure load were not significantly different between the suture anchor groups (SB vs DR); however, both groups were significantly superior to the TS group. The authors conclude that suture anchor constructs provide stronger fixation than screws for GT fractures.17
Overall, outcomes and biomechanical studies show that arthroscopic-assisted GT fixation is a safe, effective, and reliable alternative to open fixation for fractures of the GT of the humerus. Long-term studies should be performed to assess outcomes, and comparative studies should be performed to elucidate the advantages and disadvantages of open versus arthroscopic-assisted procedures.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C.K. receives support from the Steadman Philippon Research Institute and Arthrex. J.P. receives support from the Steadman Philippon Research Institute and Arthrex. E.M.F. receives support from the Steadman Philippon Research Institute. P.J.M. receives support from Arthrex, Medbridge, Springer Publishing, Steadman Clinic, Smith & Nephew, Siemens, Össur, GameReady, and VuMedi.
Supplementary Data
A technique for arthroscopic reduction and internal fixation of a displaced greater tuberosity (GT) fracture. The case shows a knotless, linked, double-row construct that uses anchors and suture tapes. The injury occurred in a 47-year-old right hand-dominant man who fell on the ice and sustained a right GT fracture with minimal displacement. He was initially treated nonoperatively; however, he continued to have pain and weakness, particularly with overhead activity. At 4 months after injury, repeat radiographs showed nonunion of the GT with 6 mm of displacement. The patient elected to undergo arthroscopic reduction and fixation. From a standard posterior viewing portal, the Hill-Sachs lesion is visualized and debrided. Subacromial decompression, acromioplasty, and lysis of adhesions are performed using an arthroscopic shaver and a radiofrequency device. An anterolateral working portal is established. Attention is turned to the GT fracture. The callus is removed using a curette and an arthroscopic shaver. Before fracture fixation, the torn supraspinatus tendon and attached fracture fragment are mobilized to ensure that they can be reduced anatomically. After an anatomic reduction is obtained, fracture reduction is confirmed with fluoroscopy. Given the size of the bone fragment and concerns about comminution, the fracture was repaired using a knotless, linked, double-row construct with suture anchors and suture tapes. A punch is used to create a socket for the placement of a 4.75-mm suture anchor medial to the fracture at the level of the articular margin. With the assistance of an arthroscopic grasper, a suture shuttling device is used to pass the suture tapes from the medial row anchor through the rotator cuff tendon. The process is then repeated for a second medial row suture anchor. Intraoperative fluoroscopy in multiple planes is again used to confirm anatomic fracture reduction. The footprint is prepared for lateral row suture anchor insertion. At this point, 1 suture tape from each medial row anchor is loaded through the first lateral row anchor. The suture tapes can be tensioned before insertion of the anchor; the anchor is then advanced into the lateral aspect of the GT for fixation. The process is repeated for the second lateral row suture anchor. This construct compresses the rotator cuff tear laterally into anatomic position while simultaneously reducing the displaced GT fracture. The construct prevents over-reduction, under-reduction, and tilting of the fragment. At this point, the shoulder is taken through passive range of motion to confirm a stable, reduced fixation construct under both direct visualization and fluoroscopy. Immediately after surgery, the patient is placed in a sling with an abduction pillow. On postoperative day 10, the patient begins passive shoulder range of motion. Active shoulder range of motion is initiated 4 weeks postoperatively. Resisted elbow flexion begins at 6 weeks, and at 8 weeks shoulder strengthening begins.
References
- 1.Kim E., Shin H.K., Kim C.H. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci. 2005;10:441–444. doi: 10.1007/s00776-005-0924-6. [DOI] [PubMed] [Google Scholar]
- 2.Ogawa K., Yoshida A., Ikegami H. Isolated fractures of the greater tuberosity of the humerus: Solutions to recognizing a frequently overlooked fracture. J Trauma. 2003;54:713–717. doi: 10.1097/01.TA.0000057230.30979.49. [DOI] [PubMed] [Google Scholar]
- 3.Kim S.H., Ha K.I. Arthroscopic treatment of symptomatic shoulders with minimally displaced greater tuberosity fracture. Arthroscopy. 2000;16:695–700. doi: 10.1053/jars.2000.9237. [DOI] [PubMed] [Google Scholar]
- 4.Green A., Izzi J., Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003;12:641–649. doi: 10.1016/s1058-2746(02)86811-2. [DOI] [PubMed] [Google Scholar]
- 5.Greiner S., Scheibel M. [Bony avulsions of the rotator cuff: Arthroscopic concepts] Orthopade. 2011;40:21–24. doi: 10.1007/s00132-010-1676-3. 26-30 [in German] [DOI] [PubMed] [Google Scholar]
- 6.Katthagen J.C., Jensen G., Voigt C., Lill H. Arthroscopy for proximal humeral fracture. Arthroskopie. 2014;27:265–274. [Google Scholar]
- 7.Bell J.E., Leung B.C., Spratt K.F. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schai P.A., Hintermann B., Koris M.J. Preoperative arthroscopic assessment of fractures about the shoulder. Arthroscopy. 1999;15:827–835. doi: 10.1053/ar.1999.v15.015082. [DOI] [PubMed] [Google Scholar]
- 9.Mazzocca A.D., Millett P.J., Guanche C.A., Santangelo S.A., Arciero R.A. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33:1861–1868. doi: 10.1177/0363546505279575. [DOI] [PubMed] [Google Scholar]
- 10.Vaishnav S., Millett P.J. Arthroscopic rotator cuff repair: Scientific rationale, surgical technique, and early clinical and functional results of a knotless self-reinforcing double-row rotator cuff repair system. J Shoulder Elbow Surg. 2010;19:83–90. doi: 10.1016/j.jse.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Greenspoon J.A., Petri M., Millett P.J. Arthroscopic knotless, double-row, extended linked repair for massive rotator cuff tears. Arthrosc Tech. 2016;5:e127–e132. doi: 10.1016/j.eats.2015.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pauly S., Scheibel M. [Rotator cuff avulsion fractures. Current concepts in the surgical treatment] Orthopade. 2016;45:159–166. doi: 10.1007/s00132-015-3214-9. [in German] [DOI] [PubMed] [Google Scholar]
- 13.Ji J.H., Jeong J.J., Kim Y.Y., Lee S.W., Kim D.Y., Park S.E. Clinical and radiologic outcomes of arthroscopic suture bridge repair for the greater tuberosity fractures of the proximal humerus. Arch Orthop Trauma Surg. 2017;137:9–17. doi: 10.1007/s00402-016-2586-6. [DOI] [PubMed] [Google Scholar]
- 14.Ji J.-H., Shafi M., Song I.-S., Kim Y.-Y., McFarland E.G., Moon C.-Y. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy. 2010;26:600–609. doi: 10.1016/j.arthro.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Tsikouris G., Intzirtis P., Zampiakis E. Arthroscopic reduction and fixation of fractures of the greater humeral tuberosity in athletes: A case series. Br J Sports Med. 2013;47 e3. [Google Scholar]
- 16.Liao W., Zhang H., Li Z., Li J. Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures? Clin Orthop Relat Res. 2016;474:1269–1279. doi: 10.1007/s11999-015-4663-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin C.-L., Hong C.-K., Jou I.M., Lin C.-J., Su F.-C., Su W.-R. Suture anchor versus screw fixation for greater tuberosity fractures of the humerus—a biomechanical study. J Orthop Res. 2012;30:423–428. doi: 10.1002/jor.21530. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A technique for arthroscopic reduction and internal fixation of a displaced greater tuberosity (GT) fracture. The case shows a knotless, linked, double-row construct that uses anchors and suture tapes. The injury occurred in a 47-year-old right hand-dominant man who fell on the ice and sustained a right GT fracture with minimal displacement. He was initially treated nonoperatively; however, he continued to have pain and weakness, particularly with overhead activity. At 4 months after injury, repeat radiographs showed nonunion of the GT with 6 mm of displacement. The patient elected to undergo arthroscopic reduction and fixation. From a standard posterior viewing portal, the Hill-Sachs lesion is visualized and debrided. Subacromial decompression, acromioplasty, and lysis of adhesions are performed using an arthroscopic shaver and a radiofrequency device. An anterolateral working portal is established. Attention is turned to the GT fracture. The callus is removed using a curette and an arthroscopic shaver. Before fracture fixation, the torn supraspinatus tendon and attached fracture fragment are mobilized to ensure that they can be reduced anatomically. After an anatomic reduction is obtained, fracture reduction is confirmed with fluoroscopy. Given the size of the bone fragment and concerns about comminution, the fracture was repaired using a knotless, linked, double-row construct with suture anchors and suture tapes. A punch is used to create a socket for the placement of a 4.75-mm suture anchor medial to the fracture at the level of the articular margin. With the assistance of an arthroscopic grasper, a suture shuttling device is used to pass the suture tapes from the medial row anchor through the rotator cuff tendon. The process is then repeated for a second medial row suture anchor. Intraoperative fluoroscopy in multiple planes is again used to confirm anatomic fracture reduction. The footprint is prepared for lateral row suture anchor insertion. At this point, 1 suture tape from each medial row anchor is loaded through the first lateral row anchor. The suture tapes can be tensioned before insertion of the anchor; the anchor is then advanced into the lateral aspect of the GT for fixation. The process is repeated for the second lateral row suture anchor. This construct compresses the rotator cuff tear laterally into anatomic position while simultaneously reducing the displaced GT fracture. The construct prevents over-reduction, under-reduction, and tilting of the fragment. At this point, the shoulder is taken through passive range of motion to confirm a stable, reduced fixation construct under both direct visualization and fluoroscopy. Immediately after surgery, the patient is placed in a sling with an abduction pillow. On postoperative day 10, the patient begins passive shoulder range of motion. Active shoulder range of motion is initiated 4 weeks postoperatively. Resisted elbow flexion begins at 6 weeks, and at 8 weeks shoulder strengthening begins.