Abstract
Osteochondritis dissecans (OCD) of the capitellum is a common disorder that causes pain and functional limitation in the adolescent elbow. Although conservative management is the first line of treatment, surgical intervention is usually recommended for patients with persistent mechanical symptoms, loose bodies, or unstable lesions. Elbow arthroscopy has become the gold standard to evaluate and treat symptomatic OCD lesions. Arthroscopic debridement and bone marrow stimulation have been shown to yield good short-term results. Unfortunately, long-term follow-up has shown less favorable outcomes, with degenerative changes frequently documented. Current marrow stimulation techniques promote the formation of fibrocartilage, which is known to be less durable than hyaline cartilage. We describe an arthroscopic technique of debridement and drilling supplemented with a micronized allogeneic cartilage scaffold to address OCD lesions of the capitellum in an effort to promote hyaline cartilage formation.
Overuse injuries make up many of the nontraumatic elbow injuries seen in young athletes.1, 2 Fortunately, most overuse elbow injuries are treated with rest and activity modification with a typical full return to sports and excellent long-term function.1, 2 Osteochondritis dissecans (OCD) of the capitellum is a frequently encountered overuse disorder of the adolescent elbow, which often leads to pain and functional limitation.1, 2 Frequently associated with sports such as baseball and gymnastics, repetitive loading of the radiocapitellar joint leads to a localized osteonecrosis of the subchondral bone.2, 3, 4 If this process is not recognized and treated in a timely manner, it may progress to separation of the subchondral bone with subsequent fragmentation and loose body formation.1, 2
Arthroscopic intervention is typically recommended for patients with persistent symptoms, and debridement with marrow stimulation is a commonly performed procedure.5 Despite good to excellent short-term results, multiple alternative surgical options have been developed in an effort to improve long-term function.5 The addition of BioCartilage (Arthrex, Naples, FL), a micronized allogeneic cartilage scaffold, to traditional marrow stimulation may assist in the formation of a more durable hyaline-like cartilage and minimize long-term degenerative changes.6
Surgical Technique
Our technique uses the traditional lateral decubitus position with a well-padded small joint limb holder (Arthrex) and a tourniquet for optimal visualization (Video 1, Tables 1 and 2). In our experience the lateral position allows for greater elbow flexion than the prone position to access the anterior aspect of the capitellum.
Table 1.
Key Steps in Arthroscopic Treatment of Capitellum OCD With BioCartilage
| 1. Evaluation of the anterior compartment of the elbow for loose bodies |
| 2. Use of an inferior posterior-lateral portal for optimal visualization of the OCD lesion |
| 3. Removal of necrotic bone from the base of the OCD lesion |
| 4. Creation of vertical stable margins on the periphery of the OCD lesion |
| 5. Percutaneous perpendicular entry of a 4.5-mm K-wire for marrow stimulation |
| 6. Adequate drying of the joint by use of controlled suction and cotton-tipped applicators |
| 7. Smoothing of the BioCartilage just below the chondral margins |
| 8. Superior percutaneous entry of the fibrin glue applicator |
OCD, osteochondritis dissecans.
Table 2.
Pearls and Pitfalls of Arthroscopic Treatment of Capitellum OCD With BioCartilage
| Pearls |
| Use of retractors and exterior stitches to maintain space during dry arthroscopy |
| Use of a spinal needle with suction and sterile cotton-tipped applicators to maintain dry arthroscopy |
| Shortening of the delivery needle to allow ease of passage of the BioCartilage mixture |
| Percutaneous superior entry for fibrin glue applicator to allow gravity application |
| Pitfalls |
| Failure to position the elbow to allow adequate flexion to visualize the anterior aspect of the OCD lesion |
| Failure to evaluate the anterior compartment for loose bodies |
| Failure to establish vertical margins and remove the necrotic bone at the base of the OCD lesion |
| Inability to maintain adequate space for dry arthroscopy |
OCD, osteochondritis dissecans.
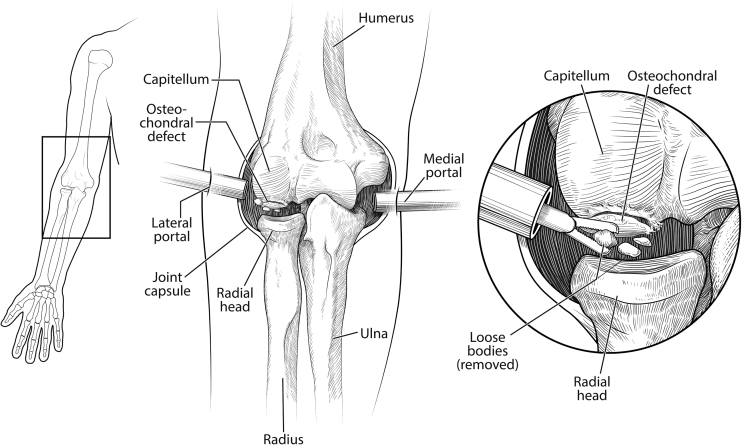
Objective Diagnosis
After the elbow is insufflated, a standard proximal anterior-medial portal is established and a diagnostic arthroscopy of the anterior aspect of the elbow joint is performed (Table 1). The radiocapitellar joint is visualized, and the radial head is rotated to visualize the periphery of the articular surface. A standard anterior-lateral portal is created by an outside-in technique with a spinal needle and scalpel. The loose bodies are often larger than standard elbow cannulas, and an arthroscopic grasper (Smith & Nephew, Andover, MA) inserted percutaneously is useful in retrieving and removing loose bodies (Figs 1 and 2). Concomitant pathology may be addressed within the anterior compartment in the same setting.
Fig 1.
Coronal view of the anterior compartment of the right elbow in the flexed position showing arthroscopic medial and lateral portals for arthroscopic treatment of loose bodies associated with an unstable osteochondritis dissecans lesion of the capitellum. The enlarged coronal inset shows retrieval of the loose bodies with an arthroscopic grasper.
(Reproduced with permission from the illustrator. ©2017 Robert Edwards, M.S., C.M.I.)
Fig 2.
Arthroscopic view from the medial portal of the anterior compartment of the right elbow in the lateral decubitus position with a 30° arthroscope visualizing retrieval of a loose body (arrow) with an arthroscopic grasper.
Debridement and Bone Marrow Stimulation
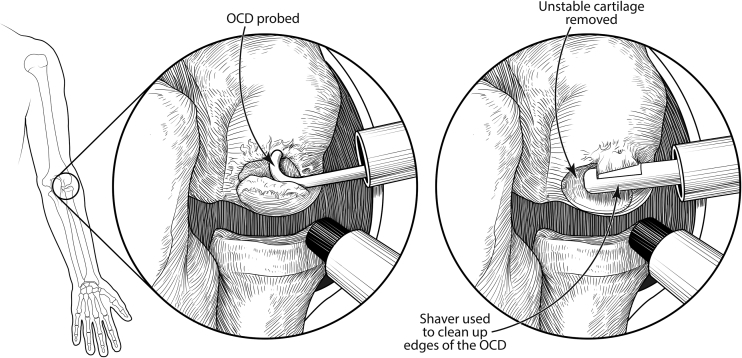
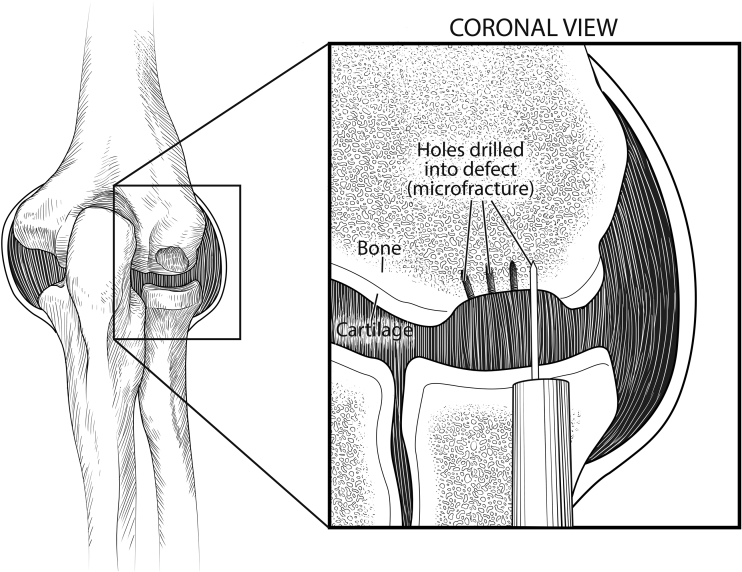
Most of the case is completed in the posterior compartment, and we initially use a standard posterior-central portal for diagnostic purposes. A posterior-lateral working portal is used to initially to debride any soft tissue in the lateral gutter and remove additional loose bodies. An inferior posterior-lateral portal is then created, and the arthroscope is positioned here for optimal visualization of the capitellar OCD. A probe is used to evaluate the stability of the OCD (Figs 3 and 4). Once the OCD is deemed unstable, a grasper is used to remove the unstable cartilage. An arthroscopic open curette (Smith & Nephew) is useful to remove any necrotic bone from the base of the lesion and create stable vertical edges on the periphery (Fig 5). A 4.5-mm shaver (Smith & Nephew) is then used to remove debris and smooth the edges (Fig 4). We emphasize the importance of debriding the base of the lesion until bleeding bone is encountered and establishing a stable border with perpendicular margins in preparation for cartilage restoration. A 4.5-mm K-wire is then percutaneously inserted perpendicular to the lesion to perform marrow stimulation (Figs 6 and 7).
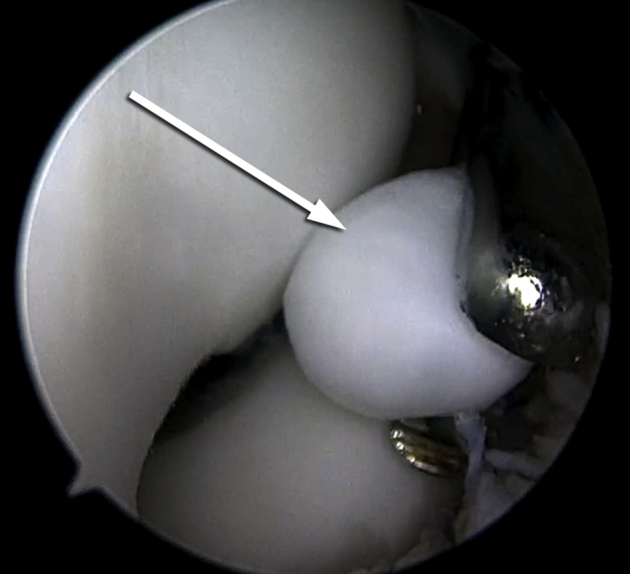
Fig 3.
Arthroscopic view from the distal posterior-lateral portal of the posterior compartment of the right elbow in the lateral decubitus position with a 30° arthroscope visualizing arthroscopic probing of an unstable osteochondritis dissecans lesion (arrow) of the capitellum.
Fig 4.
Coronal view of the posterior compartment of the right elbow in the flexed position showing arthroscopic proximal and distal posterior-lateral portals for arthroscopic probing (left) and shaving (right) of an unstable osteochondritis dissecans (OCD) lesion of the capitellum.
(Reproduced with permission from the illustrator. ©2017 Robert Edwards, M.S., C.M.I.)
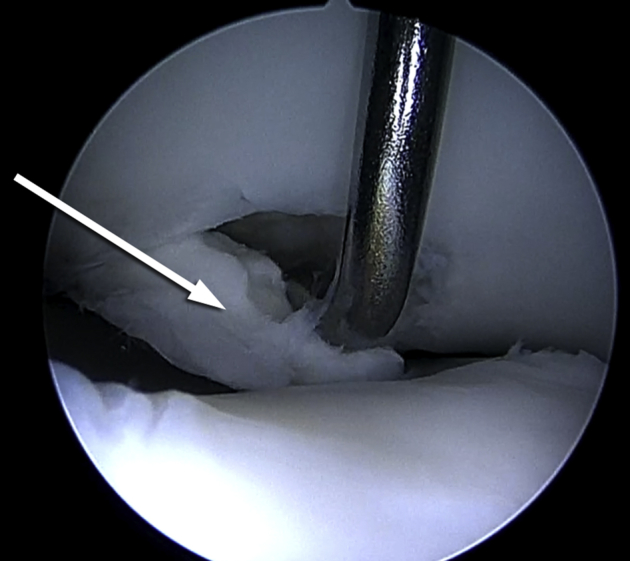
Fig 5.
Arthroscopic view from the distal posterior-lateral portal of the posterior compartment of the right elbow in the lateral decubitus position with a 30° arthroscope visualizing removal of unstable cartilage (arrow) from an unstable osteochondritis dissecans lesion of the capitellum with an arthroscopic open curette.
Fig 6.
Coronal view of the posterior compartment of the right elbow in the flexed position showing an osteochondritis dissecans lesion of the capitellum after the unstable cartilage has been removed. The enlarged inset shows arthroscopic microfracture of the osteochondritis dissecans lesion of the capitellum with a K-wire through a distal posterior-lateral portal.
(Reproduced with permission from the illustrator. ©2017 Robert Edwards, M.S., C.M.I.)
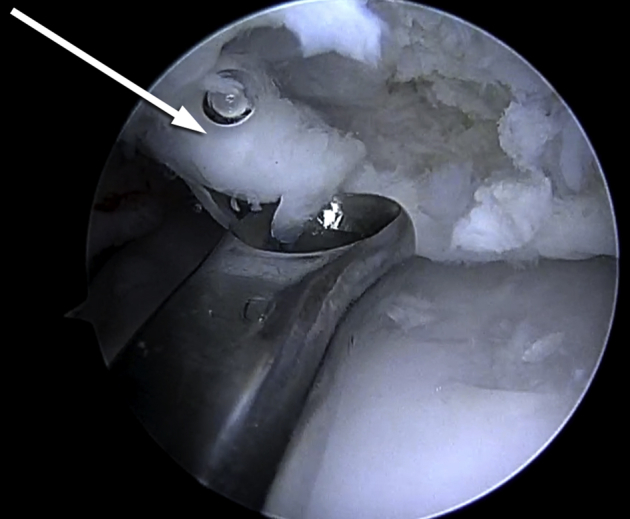
Fig 7.
Arthroscopic view from the distal posterior-lateral portal of the posterior compartment of the right elbow in the lateral decubitus position with a 30° arthroscope visualizing microfracture of an osteochondritis dissecans lesion of the capitellum with a K-wire (arrow).
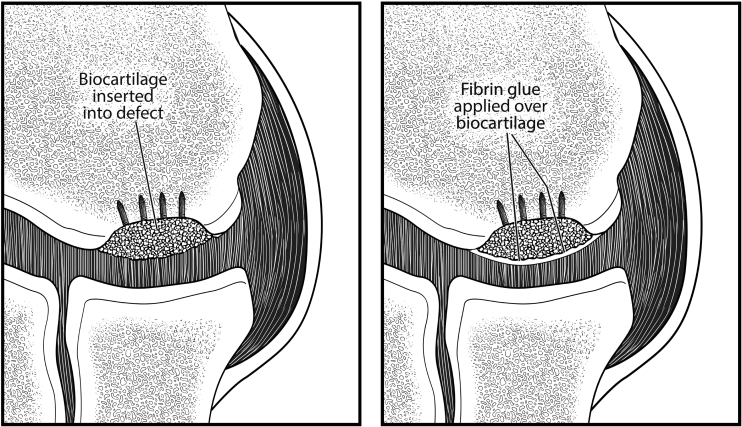
BioCartilage Application
The arthroscopic fluid is turned off, and the joint is dried by use of suction and sterile cotton-tipped applicators (Medline Industries, Mundelein, IL). We often use percutaneous switching sticks as retractors or external nylon stitches to pull the surrounding soft tissue away from the field to maintain visualization after the arthroscopic fluid has been removed. Once the defect is dried thoroughly, the straight delivery needle (Arthrex) is inserted and the previously prepared BioCartilage is delivered into the lesion. An arthroscopic paddle (Arthrex) is used to spread and smooth the BioCartilage evenly over the lesion in an effort to slightly recess the BioCartilage to the surrounding articular cartilage (Fig 8). A dual-lumen applicator tip (Baxter, Deerfield, IL) is percutaneously inserted superior to the lesion to apply the fibrin glue to seal the BioCartilage (Fig 9). The superior location of the dual-lumen applicator tip allows for gravity to assist with application of the glue on the lesion from superior to inferior. The glue is allowed to dry for 5 minutes, and the patient is placed in a posterior splint and sling postoperatively. The patient is placed in a hinged elbow brace 1 week postoperatively, and a gradual progressive rehabilitation program is initiated with a physical therapist.
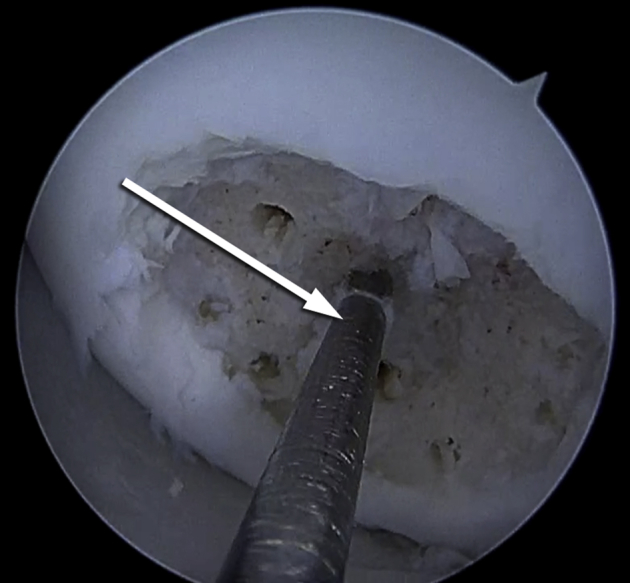
Fig 8.
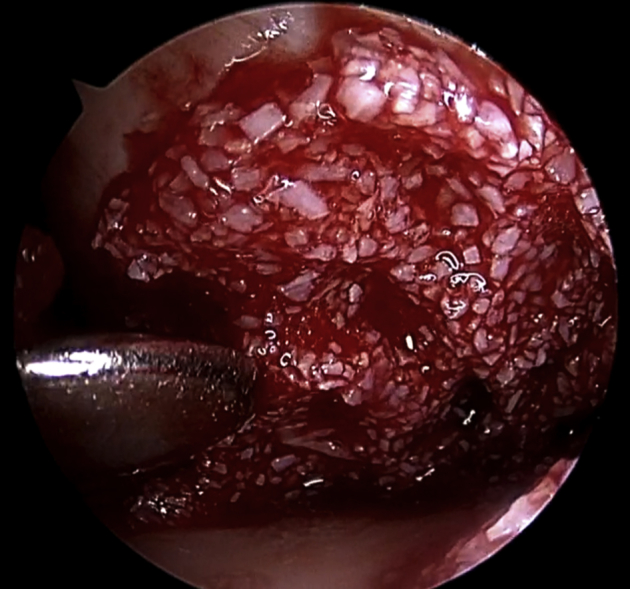
Arthroscopic view from the distal posterior-lateral portal of the posterior compartment of the right elbow in the lateral decubitus position with a 30° arthroscope visualizing smoothing of the BioCartilage over the osteochondritis dissecans lesion of the capitellum with a paddle.
Fig 9.
Coronal view of the posterior compartment of the right elbow in the flexed position showing an osteochondritis dissecans lesion of the capitellum after microfracture and application of the BioCartilage (left) and fibrin glue (right).
(Reproduced with permission from the illustrator. ©2017 Robert Edwards, M.S., C.M.I.)
Discussion
Treatment options for OCD of the capitellum include observation, bracing, arthroscopic debridement, fragment excision, removal of loose bodies, bone marrow stimulation, osteochondral grafting, and various methods of fragment fixation.1, 2, 5 As arthroscopy of the elbow has evolved, it has become the mainstay of treatment for this multifaceted condition.7 Arthroscopic debridement and bone marrow stimulation have yielded good short-term results in reduction of pain, improved range of motion, patient satisfaction, and return to sports.7, 8
Rahusen et al.9 found that 12 of 15 patients with unstable lesions returned to sports after arthroscopic debridement and abrasion chondroplasty. Ruch et al.10 found that all patients had pain relief and no limitations at 3.2 years' follow-up and that lesion size did not correlate with postoperative symptoms. Brownlow et al.11 reported good outcomes as well with an 81% rate of return to sports. Despite these good short-term results, long-term studies have shown rates of osteoarthritis of the radiocapitellar joint as high as 61%, and 42% of patients were symptomatic at 23 years.12, 13
Techniques that incorporate drilling, microfracture, or abrasion chondroplasty result in the formation of fibrocartilage within the OCD lesion.6 Because of poor long-term outcomes with less durable fibrocartilage, multiple authors have promoted autologous osteochondral transfer.14 Unfortunately, osteochondral autograft typically requires an open approach to the elbow and knee, with considerable donor-site morbidity.15 An optimal technique would comprise the simplicity of an arthroscopic approach and the capacity to generate a more hyaline-like cartilage without donor-site morbidity.6
In an effort to promote a more hyaline-like cartilage fill within the OCD lesion, we propose the use of BioCartilage to supplement marrow stimulation6 (Table 3). The addition of a micronized allogeneic cartilage scaffold has been shown to yield higher rates of hyaline cartilage formation in animal studies when compared with microfracture alone.6, 16 Our expectation is that a minimally invasive technique that promotes the formation of a more hyaline-like cartilage may result in a more durable surface and subsequent superior long-term results.6 To date, no results are available on arthroscopic debridement, drilling, and supplementation of BioCartilage,6 and further clinical studies will be needed to determine the long-term efficacy of this technique.
Table 3.
Advantages and Disadvantages of Arthroscopic Treatment of Capitellum OCD With BioCartilage
| Advantages |
| Minimally invasive outpatient arthroscopic approach |
| No need for a 2-stage procedure |
| No osteochondral harvest graft-site morbidity |
| Potential for a more hyaline-like cartilage fill within the OCD lesion |
| Disadvantages |
| Increased operative time and expense to the patient |
| Technically demanding procedure requiring advanced elbow arthroscopic skills |
| No proven long-term benefit of BioCartilage augmentation of microfracture |
OCD, osteochondritis dissecans.
Footnotes
The authors report the following potential conflict of interest or source of funding: P.E.C. receives support from Arthrex, Bon Secours, DJO, DePuy Mitek, Smith & Nephew. Fellowship support. B.A. receives support from Arthrex, Bon Secours, DJO, DePuy Mitek, Smith & Nephew. Fellowship support. S.E.P. receives support from Arthrex, Bon Secours, DJO, DePuy Mitek, Smith & Nephew. Fellowship support.
Supplementary Data
Arthroscopy of the right elbow of a young right hand–dominant overhead athlete. The anterior aspect of the radiocapitellar joint is evaluated from the anterior-medial portal, and multiple loose bodies are removed by a percutaneous technique with an arthroscopic grasper from an anterior-lateral portal. The unstable osteochondritis dissecans (OCD) lesion of the capitellum is evaluated from the inferior posterior-lateral portal. Removal of all unstable chondral fragments is accomplished with an open-ended curette and shaver. Microfracture is carried out with a K-wire percutaneously. The joint is adequately dried, arthroscopic application of BioCartilage is performed, and the BioCartilage is sealed with fibrin glue.
References
- 1.Tisano B.K., Estes A.R. Overuse injuries of the pediatric and adolescent throwing athlete. Med Sci Sports Exerc. 2016;48:1898–1905. doi: 10.1249/MSS.0000000000000998. [DOI] [PubMed] [Google Scholar]
- 2.Baker C.L., III, Romeo A.R., Baker C.L., Jr. Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38:1917–1928. doi: 10.1177/0363546509354969. [DOI] [PubMed] [Google Scholar]
- 3.Kobayashi K., Burton K.J., Rodner C., Smith B., Caputo A.E. Lateral compression injuries in the pediatric elbow: Panner's disease and osteochondritis dissecans of the capitellum. J Am Acad Orthop Surg. 2004;12:246–254. doi: 10.5435/00124635-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Takahara M., Mura N., Sasaki J., Harada M., Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89:1205–1214. doi: 10.2106/JBJS.F.00622. [DOI] [PubMed] [Google Scholar]
- 5.Churchill R.W., Munoz J., Ahmad C.S. Osteochondritis dissecans of the elbow. Curr Rev Musculoskelet Med. 2016;9:232–239. doi: 10.1007/s12178-016-9342-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abrams G.D., Mall N.A., Fortier L.A., Roller B.L., Cole B.J. BioCartilage: Background and operative technique. Oper Tech Sports Med. 2013;21:116–124. [Google Scholar]
- 7.Micheli L.J., Luke A.C., Mintzer C.M., Waters P.M. Elbow arthroscopy in the pediatric and adolescent population. Arthroscopy. 2001;17:694–699. doi: 10.1053/jars.2001.25338. [DOI] [PubMed] [Google Scholar]
- 8.Jones K.J., Wiesel B.B., Sankar W.N., Ganley T.J. Arthroscopic management of osteochondritis dissecans of the capitellum: Mid-term results in adolescent athletes. J Pediatr Orthop. 2010;30:8–13. doi: 10.1097/BPO.0b013e3181c3be83. [DOI] [PubMed] [Google Scholar]
- 9.Rahusen F.T., Brinkman J.M., Eygendaal D. Results of arthroscopic debridement for osteochondritis dissecans of the elbow. Br J Sports Med. 2006;40:966–969. doi: 10.1136/bjsm.2006.030056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruch D.S., Cory J.W., Poehling G.G. The arthroscopic management of osteochondritis dissecans of the adolescent elbow. Arthroscopy. 1998;14:797–803. doi: 10.1016/s0749-8063(98)70013-1. [DOI] [PubMed] [Google Scholar]
- 11.Brownlow H.C., O'Connor-Read L.M., Perko M. Arthroscopic treatment of osteochondritis dissecans of the capitellum. Knee Surg Sports Traumatol Arthrosc. 2006;14:198–202. doi: 10.1007/s00167-005-0623-z. [DOI] [PubMed] [Google Scholar]
- 12.Bauer M., Jonsson K., Josefsson P.O., Lindén B. Osteochondritis dissecans of the elbow: A long-term follow-up study. Clin Orthop Relat Res. 1992;(284):156–160. [PubMed] [Google Scholar]
- 13.Takahara M., Ogino T., Sasaki I., Kato H., Minami A., Kaneda K. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res. 1999;(363):108–115. [PubMed] [Google Scholar]
- 14.Tsuda E., Ishibashi Y., Sato H., Yamamoto Y., Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the capitellum in nonthrowing athletes. Arthroscopy. 2005;21:1270. doi: 10.1016/j.arthro.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Iwasaki N., Kato H., Kamishima T., Suenaga N., Minami A. Donor site evaluation after autologous osteochondral mosaicplasty for cartilaginous lesions of the elbow joint. Am J Sports Med. 2007;35:2096–2100. doi: 10.1177/0363546507306465. [DOI] [PubMed] [Google Scholar]
- 16.Fortier L.A., Chapman H.S., Pownder S.L. BioCartilage improves cartilage repair compared with microfracture alone in an equine model of full-thickness cartilage loss. Am J Sports Med. 2016;44:2366–2374. doi: 10.1177/0363546516648644. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopy of the right elbow of a young right hand–dominant overhead athlete. The anterior aspect of the radiocapitellar joint is evaluated from the anterior-medial portal, and multiple loose bodies are removed by a percutaneous technique with an arthroscopic grasper from an anterior-lateral portal. The unstable osteochondritis dissecans (OCD) lesion of the capitellum is evaluated from the inferior posterior-lateral portal. Removal of all unstable chondral fragments is accomplished with an open-ended curette and shaver. Microfracture is carried out with a K-wire percutaneously. The joint is adequately dried, arthroscopic application of BioCartilage is performed, and the BioCartilage is sealed with fibrin glue.