Abstract
A 39-yerar-old man was admitted to our hospital with behavioral disturbances and generalized headaches. He was diagnosed with CNS toxoplasmosis after performing a brain biopsy. He found to be HIV positive with a CD4 of 14/uL He was started on ant toxoplasmosis along with antiretroviral therapy. He presented 6 weeks after discharge with worsening headache thought to be related to relapse of toxoplasmosis. However, he found to have severe anemia related to CMV-induced gastrointestinal bleeding. He was started on anti-cytomegalovirus drugs and has finally achieved significant improvement.
Introduction
This report details a case of cerebral toxoplasmosis as a first manifestation of HIV infection causing midline shift requiring urgent cerebral biopsy to rule out CNS lymphoma before starting steroid therapy. The patient initially presented with headache and confusion. He underwent MRI which was remarkable for ring-enhancing lesion in the right basal ganglia with 7 mm midline shift to the left. Subsequently, the patient underwent stereotactic right basal ganglion lesion biopsy with a Toxoplasma gondii detected by nucleic acid amplification. Patient was treated with trimethoprim/sulfamethoxazolefor a total of 6 weeks along with antiretroviral therapy, and patient eventually achieved significant improvement. Interestingly, 6 weeks after discharge, the patient returned presenting with worsening headaches and escalating fatigue suggesting a relapse of the cerebral toxoplasmosis. Repeated MRI showed significant improvement in his brain lesion, however, he found to have severe anemia. Upper GI endoscopy revealed gastric ulceration which was positive for cytomegalovirus. Patient was treated with valganciclovir 900 for a total of 4 weeks and he eventually achieved significant improvement.
Case report
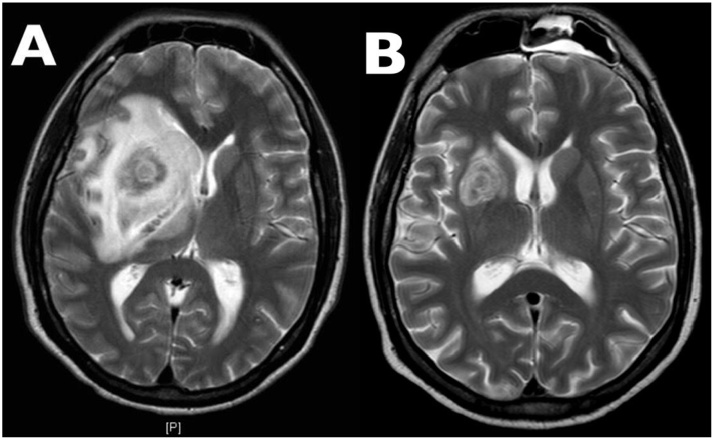
A 39-yerar-old man presented to the emergency room with a 2-week-long clinical picture of behavioral disturbances and generalized headaches. His past medical history was unremarkable. The patient indicated he was also experiencing nausea without vomiting, and chills but no fever. He also found himself to be more confused recently and his roommate found him lying down on the shower floor holding his head. He denied seizure-like activity. Patient was a homosexual, having had 3 partners over the previous 6 months, but never tested for HIV/STD in the past. He moved to the US last October from Venezuela where he had lived previously. He reported travel to Italy and the Dominican Republic as well. In the ER, his blood tests were unremarkable except for a white cell count at 4.1 × 10 cells/mm3. A neurological examination only highlighted drowsiness. A gadolinium-enhanced MRI scan of the brain (Fig. 1A) showed a 2.9 cm ring-enhancing lesion in the right basal ganglia with central area of necrosis and extensive surrounding vasogenic edema causing a 7 mm midline shift to the left, right frontotemporal sulci effacement, and near complete effacement of the right lateral ventricle.
Fig. 1.
(A) A magnetic resonance image with gadolinium enhancement at initial presentation. The image shows a 2.9 cm ring-enhancing lesion in the right basal ganglia with central area of necrosis and extensive surrounding vasogenic edema causing a 7 mm midline shift to the left, effacement of right frontotemporal sulci, and nearly complete effacement of the right lateral ventricle. Mass effect also causes right-sided uncal herniation effacing the ambient cistern. There are two additional enhancing satellite lesions in the left posterior frontal lobe. (B) A magnetic resonance image with gadolinium enhancement 6 weeks after treatment. This is an image of the brain after treatment showing significant decrease in size and interval resolution of peripheral enhancement of a hemorrhagic lesion in the head of the right caudate nucleus. Surrounding vasogenic edema has nearly completely resolved as well. Previously described additional small enhancing lesions in the left cerebral hemisphere are no longer present.
Neurosurgery was consulted and a stereotactic biopsy from the right basal ganglion lesion performed. Immunohistopathology revealed necrotic material with a mixed inflammatory infiltrate, vascular fibrinoid necrosis, and small hematoxylin stain particles that arose suspicion of Toxoplasmosis. Toxoplasma gondii DNA was detected by nucleic acid amplification. The patient was began on dexamethasone at 4 mg IM every 6 h. His CD4 cell count was 14/uL and HIV viral load 34,913 copies/mL.
Further laboratory analyses disclosed positivity for anti-toxoplasma immunoglobulin G. Pyrimethamine and sulfadiazine were unavailable so the patient was started on trimethoprim-sulfamethoxazole of the trimethoprim equivalent 10 mg/kg/day PO q12h for a total of 6 weeks along with antiretroviral therapy including Elvitegravir/cobicistat/emtricitabine/tenofovir.
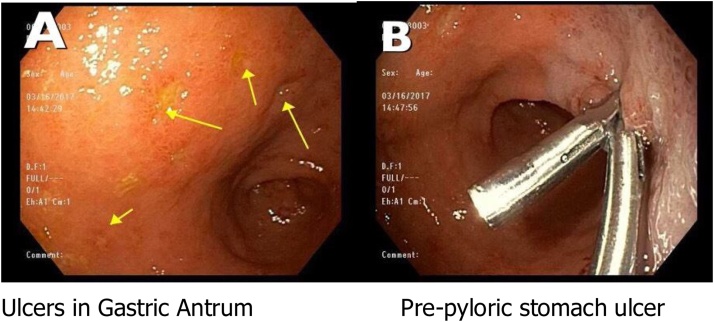
The patient was discharged in a good condition. Impotently 6 weeks after discharge, he returned presenting with worsening headaches and escalating fatigue. He denied reflux, heartburn, melena, hematochezia, abdominal pain, diarrhea, constipation or emesis. He further declared that his steroid dose was decreased from QID to TID dosing 2 days before the beginning of his symptoms. MRI was repeated which exhibited significant improvement in brain mass and surrounding edema (Fig. 1B). His labs were remarkable for hemoglobin of 6.4 g/dL which was a downtrend compared to the previous admission when he had hemoglobin of a 13.2 g/dL. Upper endoscopy performed which revealed oozing gastric ulcers with an adherent clot (Fig. 2A + B). Biopsy from gastric ulcers showed focal ulceration with Cytomegalovirus inclusions, and benign hyperplastic gastric glandular epithelial changes. Patient was treated with valganciclovir 900 for a total of 4 weeks and he eventually achieved significant improvement.
Fig. 2.
Upper GI endoscopy with scattered moderate inflammation characterized by shallow ulcerations was found in the gastric antrum (A) and in the gastric body. The largest lesion was 5 mm in largest dimension (B) which was injected with epinephrine for hemostasis. Biopsies were taken with a cold forceps for histology.
Discussion
Toxoplasmosis in patients who are immunocompromised can be life threatening. In this population, toxoplasmosis occurs generally owing to reactivation of a chronic disease and most typically affects the central nervous system. Toxoplasmic encephalitis has a varied clinical presentation, ranging from an acute state of confusion with or without focal neurological deficits often slowly progressing over days to a subacute gradual process evolving over weeks. Other presentations of toxoplasmosis in patients who are immunocompromised include chorioretinitis [1], pneumonitis [2], or multi-organ failure [3].
Multiple ring-enhancing lesions in the brain raise questions about the true diagnosis. The etiologies are many neoplastic, infectious, vascular, inflammatory and demyelinating conditions and depend on a patient’s geographical location. The most common causes of multiple ring enhancing lesions in an immunocompromised lesion with low CD4 count include brain abscess, toxoplasmosis and lymphoma. The enhancing lesions are often of variable in size and surrounded by a varying amount of perifocal vasogenic edema. Typically, the ring enhancing lesions are located at the junction of the gray and white matter, but one might also find them in the sub-cortical area, deep in the brain parenchyma; they can even be superficial [4].
Corticosteroids significantly impact the ability for contrast dye to cross the blood-brain barrier in neuroimaging studies. As a result, during interpretation one needs to take the dose and duration of glucocorticoids carefully into account [5], [6]. If the primary CNS lymphoma is a possible diagnostic consideration, dexamethasone should be withheld unless cerebral edema and mass effect are clinically significant. The reason for this is the prompt antineoplastic effect of dexamethasone. In some cases, the response can be so dramatic that it impacts the clinic’s ability to properly biopsy the tumor. In only a few days, a tumor can manifes decrease in enhancement to such a degree that it may not appear on the localizing scan carried out prior to biopsy [7].
Many HIV infected individuals have cytomegalovirus (CMV) infection, and the greatest risk occurs to HIV patients when the CD4 count falls below 50. While CMV disease can affect the entire GI tract, it more frequently involves the esophagus and the colon [8]. CMV typically presents with distal esophageal ulcerations; accordingly, biopsies from the ulcer base are more likely to demonstrate characteristic CMV inclusions, which are usually seen in stromal and endothelial cells, as compared to HSV infection, which manifests in squamous cells [9]. One would most often treat this orally or with an intravenous ganciclovir12 (5 mg/kg twice daily) or foscarnet (90 mg/kg two twice daily), both of which are viral DNA polymerase inhibitors. Cidofovir is less common for treatment. Immunocompetent patients often do not need treatment with antivirals. The recurrence of headache in this patient suggested the relapse of toxoplasmosis but the headache was found to be caused by a prominent anemia related to CMV-induced gastrointestinal bleeding. Headache can be a prominent symptom of anemia.
Learning objectives
We report a case of cerebral Toxoplasmosis causing a midline shift as a first manifestation of HIV infection that required urgent cerebral biopsy. His course was complicated by severe anemia and cytomegalovirus gastritis
Conflicts of interest
The author has no financial conflicts of interest
Authors’ contributions
All authors were involved in the management of the patient. All authors read and approved the final manuscript.
References
- 1.Pereira N.M., Shah I., Lala M. Toxoplasmosis with chorioretinitis in an HIV-infected child with no visual complaints-importance of fundus examination. Oxf Med Case Reports. 2017 doi: 10.1093/omcr/omw094. U.S. national library of medicine, 03 2017. Web. 09 Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Undseth Ø., Primary toxoplasmosis with critical illness and multi-organ failure in an immunocompetent young man. https://www.ncbi.nlm.nih.gov/pubmed/23902584. N.p., Jan. 2014. [DOI] [PubMed]
- 3.Velásquez J.N., Ledesma B.A., Nigro M.G., Vittar N., Rueda N., De Carolis L. Pulmonary toxoplasmosis in human immunodeficiency virus-infected patients in the era of antiretroviral therapy. Lung India. 2017 doi: 10.4103/0970-2113.173063. U.S. national library of medicine, n.d. Web. 09 Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smirniotopoulos J.G., Murphy F.M., Rushing E.J., Rees J.H., Schroeder J.W. Patterns of contrast enhancement in the brain and meninges. Radiographics. 2007;27:525–551. doi: 10.1148/rg.272065155. [DOI] [PubMed] [Google Scholar]
- 5.Macdonald D.R., Cascino T.L., Schold S.C., Jr., Cairncross J.G. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol. 1990;8(7):1277–1280. doi: 10.1200/JCO.1990.8.7.1277. [DOI] [PubMed] [Google Scholar]
- 6.van den Bent M.J., Vogelbaum M.A., Wen P.Y., MacDonald D.R., Chang S.M. end point assessment in gliomas: novel treatments limit usefulness of classical MacDonald’s criteria. J Clin Oncol. 2009;27(18):2905–2908. doi: 10.1200/JCO.2009.22.4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Porter A.B., Giannini C., Kaufmann T., Lucchinetti C.F., Wu W., Decker P.A. Primary central nervous system lymphoma can be histologically diagnosed after previous corticosteroid use: a pilot study to determine whether corticosteroids prevent the diagnosis of primary central nervous system lymphoma. Ann Neurol. 2008;63:662–667. doi: 10.1002/ana.21366. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Pellecchia P., Brandt L.J. Intestinal abnormalities in AIDS. In: Classen M., Tytgat G.N.J., Lightdale C.J., editors. Gastroenterological endoscopy. 2nd edition. Thieme; Stuttgart, Germany: 2010. pp. 753–765. [Google Scholar]
- 9.Matsumoto C. Gastrointestinal infections in solid organ transplant recipients. Curr Opin Organ Transplant. 2004;9(4):406–410. [Google Scholar]