After three days of deliberation an advisory panel to the US Food and Drug Administration decided that the widely used cyclo-oxygenase-2 (COX 2) inhibitors rofecoxib (Vioxx), celecoxib (Celebrex), and valdecoxib (Bextra) all carry serious risks of heart attack and stroke and recommended that the FDA demand that the drugs carry “black box” warnings. But the panel did not recommend that the drugs be withdrawn from the market.
The panel was convened after Merck voluntarily withdrew rofecoxib (Vioxx) from the market on 30 September (BMJ 2004;329: 816, 9 Oct) when it was found that the drug doubles the risk of heart attacks and strokes in patients who take it for 18 months or longer.
US media coverage of the panel's findings has been criticised by Dr Alastair Wood, the panel's chairman and associate dean at Vanderbilt University School of Medicine, Nashville. He said that the coverage was distorted because it focused on the fact that the panel had not recommended the drugs' withdrawal rather than on its finding of an increased risk of heart attack and stroke.
He said, “The general outcome [of the hearings] was greatly overrated in the US press. Two drugs were recommended for removal from the market by almost 50% of the committee. The press took this [the fact that a majority did not vote for withdrawal] as an endorsement [of their safety] by the committee. But it clearly was not. This is like assembling a group of pilots at the end of a jet way and half of the pilots tell you the plane is unsafe to fly. Would you get on it?”
The US findings came after similar findings by Australian and European authorities. On 10 February Australia's Therapeutic Goods Administration instituted a requirement that all COX 2 drugs carry a black box warning highlighting the risk of serious cardiovascular events and strongly urged doctors and patients to adhere to lower dose ranges (www.tga.gov.au/media/2005/050210_cox2.pdf).
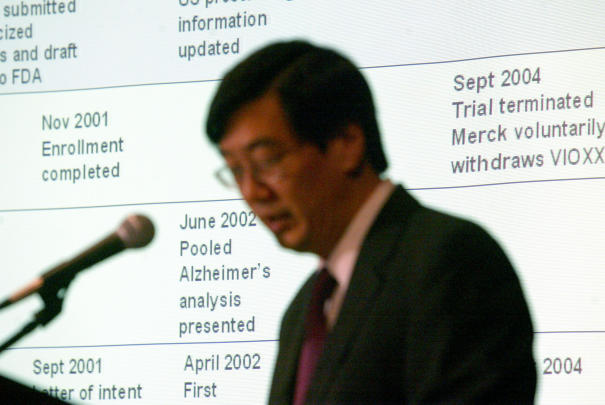
Figure 1.
Dr Peter Kim, president of Merck Research Laboratories, said that the company was considering returning rofecoxib (Vioxx) to the market
Credit: DIANE BONDAREFF/AP
After four days of deliberations the European Medicines Agency issued a statement on 17 February contraindicating COX 2 drugs for patients with ischaemic heart disease or stroke and urging caution for patients with risk factors such as high blood pressure, hyperlipidaemia, diabetes, heart disease, smoking, or peripheral vascular disease (www.emea.eu.int/pdfs/human/press/pr/6275705en.pdf).
The FDA advisory panel, a joint meeting of the agency's Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee, also recommended that the FDA require strongly worded black box warnings for each of the three COX 2 inhibitors currently approved in the United States—celecoxib, valdecoxib, and rofecoxib. The decision about rofecoxib was needed, according to FDA officials, because the drug was not ordered off the market but was withdrawn voluntarily.
The panel's finding of a class effect led to an unexpected announcement—which one committee member called a “cliff hanger”—by Dr Peter Kim, president of Merck Research Laboratories, who told the committee, “When we withdrew rofecoxib we thought there were safe alternatives.” But he said that in light of “new scientific information” Merck would consider returning rofecoxib to the market.
During the three days of hearings the 32 member panel heard emotional testimony from a number of patients who said that only a certain COX 2 drug helped their pain and who begged the panel not to withdraw their treatment.
The challenge of making decisions in the face of imperfect science was a topic of much discussion. Panel members repeatedly cited examples of findings from observational studies that were later discredited by randomised controlled trials. One panellist said, “The road to hell is paved with biological plausibility.”
Dr David Graham, the FDA's associate director for science in the Office of Drug Safety, presented unpublished data confirming the risks of rofecoxib and the risks of heart attack and stroke associated with non-selective non-steroidal anti-inflammatory drugs, such as the top selling drug meloxicam (Mobic).
A few panellists raised questions about Dr Graham's data, but others defended both his findings and the nature of the study.
Questions were also raised during the hearings about whether cardiovascular risks were dealt with in a timely and appropriate manner after the Vioxx gastrointestinal outcomes research (VIGOR) study in 2000 that first showed excess cardiovascular deaths in patients taking the drug (N Engl J Med 2000;343: 1520-811087881).
Dr Richard Platt, a member of the Drug Safety and Risk Management Advisory Committee and chairman of the Department of Ambulatory Care and Prevention at Harvard Medical School and Harvard Pilgrim Health Care, said, “My concern is that the VIGOR study did not result in a prompt change in practice.” Part of the problem in realising there was a genuine signal, said Dr Platt, was that common disorders are harder than rare problems to confirm as side effects of a drug.
Some panel members urged caution about placing warnings on COX 2 drugs, saying they didn't want to “scare” patients by issuing warnings without definitive proof of harm. But other members said that the standards of scientific proof for efficacy should not be the same as the standards used to warn of harm.
“One of the particular problems with COX 2 inhibitors,” said Dr Platt, “is that they were very widely used almost as soon as they were released, and they were used by many more people than just those at high risk for gastrointestinal problems.” That problem, he said, was greatly aggravated by advertising directly to consumers.
Dr Curt Furberg, another member of the Drug Safety and Risk Management Advisory Committee, said that he was pleased with the black box warning, as it would make it very hard for manufacturers to advertise.
Dr Garret FitzGerald, a cardiologist at the University of Pennsylvania and a guest speaker at the hearing, said, “For those who wanted to pretend this is just a Vioxx problem... I'm glad to say those ghosts were exorcised.”
“We need to figure out how we can do a better job in the future,” said Dr Platt. “I think it would be very worthwhile for the FDA to enhance its capacity to identify important adverse events more quickly.”