Abstract
In recent years, there has been a significant effort to identify high-risk plaques in vivo prior to acute events. While number of imaging modalities have been developed to identify morphologic characteristics of high-risk plaques, prospective natural-history observational studies suggest that vulnerability is not solely dependent on plaque morphology and likely involves additional contributing mechanisms. High wall shear stress (WSS) has recently been proposed as one possible causative factor, promoting the development of high-risk plaques. High WSS has been shown to induce specific changes in endothelial cell behavior, exacerbating inflammation and stimulating progression of the atherosclerotic lipid core. In line with experimental and autopsy studies, several human studies have shown associations between high WSS and known morphological features of high-risk plaques. However, despite increasing evidence, there is still no longitudinal data linking high WSS to clinical events. As the interplay between atherosclerotic plaque, artery, and WSS is highly dynamic, large natural history studies of atherosclerosis that include WSS measurements are now warranted. This review will summarize the available clinical evidence on high WSS as a possible etiological mechanism underlying high-risk plaque development.
Keywords: Acute coronary syndrome, Coronary artery disease, Computational fluid dynamics, High-risk plaque, Wall shear stress
Introduction
Since the introduction of the high-risk plaque concept, there have been significant efforts to identify high-risk plaques in vivo prior to rupture. In recent years, number of invasive and non-invasive imaging modalities have been developed that are able to identify morphologic characteristics of high-risk plaque [1]. Nevertheless, prospective natural-history observational studies using these imaging technologies have consistently shown that not all plaques go through the rapid progression phase and few high-risk plaques will give rise to a clinical event [2–4]. These data suggest that plaque vulnerability is not solely dependent on plaque morphology and likely involves additional contributing mechanisms such as mechanical stress and strain [5,6]. High wall shear stress (WSS) has recently been proposed as one of the contributing factors to development high-risk plaques. The role of WSS in the initiation and progression of atherosclerosis at the molecular level has been extensively discussed in the literature [6,7]. This review will summarize the available clinical evidence on high WSS as a possible etiological mechanism underlying high-risk plaque development.
High-Risk Plaque
The morphology of high-risk plaques responsible for acute coronary syndromes (ACS) varies from thrombosis with or without coronary occlusion to sudden narrowing of the lumen from intraplaque hemorrhage (IPH). Plaque rupture is the most common cause of myocardial infarction and along with plaque erosion are primary plaque morphologies responsible for the development of intraluminal thrombosis and subsequent myocardial ischemia [8]. Eruptive calcified nodules are the less common cause of thrombosis [5]. While recent analyses suggest different etiologies for plaque rupture and plaque erosion [5,9,10], mechanisms of plaque rupture have been extensively studied and morphological features of rupture-prone plaques are well established (Table 1) [8]. No single morphological features have been identified for erosion-prone plaques; nevertheless, we know that eroded plaques with thrombosis are rarely calcified or associated with expansive remodeling, and show minimal inflammation [8,11]. Ruptured plaques are typically fibroatheromas (FA)s, defined by their large lipid-rich necrotic core [12,13]. The necrotic core in ruptured plaques is comparatively larger than in non-ruptured FA [11]. Cholesterol crystal formation may also be evident, which is thought to augment the inflammatory response and promote plaque instability [14]. The overlying fibrous cap separates the thrombogenic necrotic core from the arterial lumen. The thickness of the fibrous cap adjacent to the site of rupture is <65μm [15], while the cap is often heavily infiltrated with inflammatory cells and exhibits fewer smooth muscle cells [11]. These cellular changes promote degradation of the collagen-rich cap matrix, resulting in cap thinning and eventually rupture [16]. Deeper within the plaque, cell death and necrotic core debris may act as a driver for the development of calcium phosphate spheres within the plaque, which appear to coalesce over time to form macroscopic calcified plates or nodules [17]. Small regions of microcalcification may also act to increase the tensile stress within the lesion or the cap itself, further increasing the likelihood of rupture [18,19]. Neovascularization is also frequently present, with these vessels arising from the adventitial vasa vasorum and their recruitment stimulated by the release of angiogenic factors from vascular smooth muscle cells [20]. The endothelium of these immature vessels has been shown to be leaky, providing an alternative mechanism for the entry of inflammatory cells, erythrocytes and plasma proteins into the plaque [21]. Additionally, neovessel rupture may result in IPH, resulting in rapid plaque expansion and promoting inflammation and necrotic core growth [22]. Finally, high-risk plaques frequently exhibit outward (or positive) vascular remodeling, defined as an expansion in the external elastic lamina when compared with the adjacent healthy arterial segment [23].
Table 1.
Features of rupture-prone plaques (modified from Falk et al. [8]).
|
While our understanding of atherosclerotic plaque development is evolving, recent analysis of large clinical data has confirmed that plaques responsible for ACS have larger plaque and necrotic core volumes with greater expansive remodeling, compared with asymptomatic plaques [24]. A systematic literature review now points to clinical evidence of accelerated and rapid plaque growth prior to ACS. This initiates with slow intraluminal plaque growth and expansive remodeling (outward plaque growth) during which the lumen size stays relatively preserved. When plaque growth reaches the limit of expansive remodeling, accelerated intraluminal growth and narrowing ensues (Figure 1). It is postulated that intraplaque neovascularization with incompetent vessels that leak red blood cells at the borders of the necrotic core, IPH, and subclinical cycles of rupture and healing are mechanisms for this accelerated plaque growth and possibly total occlusion [5]. Luminal thrombus, plaque fissure, and IPH are the main factors contributing to the sudden increase in plaque size and luminal narrowing ultimately resulting in the onset of ACS [25].
Figure 1.
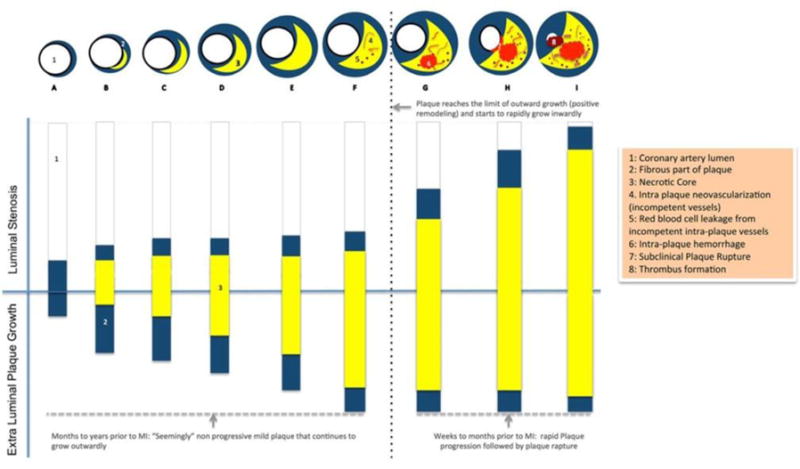
Possible mechanism for rapid plaque progression before myocardial infarction (from Ahmadi et al. [24] with permission)
High Wall Shear Stress
Under physiological conditions, atherosclerotic plaque is subject to mechanical loading due to pulsatile blood pressure and flow [26]. Studies have shown that mechanical stimuli can affect the bio-function of vascular endothelial [27] and smooth muscle cells [28], possibly contributing to the initialization and progression of atherosclerosis. Several animal and human studies in coronary and carotid arteries suggest a role for local hemodynamic factors, including WSS, in the evolution of atherosclerotic plaques [7,29–31]. Different flow patterns directly determine endothelial cell morphology, metabolism, and inflammatory phenotype through signal transduction and gene and protein expression [32]. Endothelial cells are capable of perceiving WSS as a mechanical signal, transmitting this into the cell interior, triggering serial cellular signaling responsible for gene expression and regulating the function of vascular smooth muscle cells [33].
At present, there is no consensus within human studies on the range of WSS and cut-off values that constitute low, intermediate (physiologic), and high WSS. In general, low WSS is typically represented by <10 dynes/cm2 [34–37]. However, intermediate and high WSS values are less clearly defined. For years, WSS was categorized to only low and non-low (also called “high WSS” at the time). Based on this classification, there has been a consensus that low and/or oscillatory WSS results in atherosclerosis initiation and progression [32], and some investigators even proposed a role for low WSS in the development of high-risk plaque [30,38]. On the other hand, the so called “non-low or high WSS” was thought to be atheroprotective. In recent years, investigators categorized non-low WSS (previously called “high WSS”) to physiologic WSS and high WSS (higher than physiologic values); and have shown an emerging but somewhat controversial role for high WSS in development of high-risk plaque features. The interest in high WSS as a potential pathological mechanism was driven by observational data showing a localized elevation of WSS on each plaque surface (top portion of the maximal stenosis) and that the location of focally elevated WSS was frequently matched with the plaque rupture site [39]. High WSS has been shown in experimental studies to induce specific changes in endothelial cell behavior, including modifying gene expression and expression of matrix metalloproteinases [40,41]. Such changes have potential to exacerbate inflammation and promote progression of the atherosclerotic lipid core [6,7,42]. In the carotid circulation, ulceration of carotid plaques, visible on angiography or on pathological examination, was seen most often in regions where WSS was highest [43] and the inflammatory burden was severe [44]. In line with the experimental and autopsy studies, longitudinal and cross-sectional human coronary and carotid studies have shown an increase in plaque necrotic core, calcium [35], and strain [45], development of expansive remodeling [35,46], presence of IPH [47], large necrotic core [34,46,48], a necrotic core in contact with the lumen [48], and napkin-ring sign [46] in areas exposed to high WSS. Meanwhile, some data show that WSS might not have the same role in development of plaque erosion as it has in the development of plaque rupture [9,10].
Our group was the first to compare plaque development characteristics in coronary segments with low, physiologic (intermediate) and high WSS (defined as <10 dynes/cm2, 10–25 dynes/cm2, and >25 dynes/cm2, respectively) [35]. In this study, 20 patients with non-obstructive coronary artery disease on optimal medical therapy were investigated. At 6-month follow-up, areas with low WSS had plaque progression, compared to intermediate and high WSS, which exhibited overall plaque regression. Areas of high WSS were also noted to have greater progression of necrotic core (a trait also shared by areas of low WSS) and calcium (Figure 2A). High WSS further demonstrated regression of fibrous and fibrofatty tissue, which was possibly indicative of a transition to a more vulnerable plaque phenotype. Interestingly, in this study both low and high WSS arterial regions had similar increases in necrotic core, while only high WSS demonstrated increases in dense calcium and decrease in fibrous and fibrofatty tissue. We further showed that areas with combination of large plaque (>60% plaque burden), pathologic intimal thickening phenotype, and high WSS at baseline were more likely to develop an increase in necrotic core, a decrease in fibrofatty and fibrous tissue, and expansive remodeling at 6-month follow-up compared to areas with either of these characteristics alone, suggesting an incremental value of high WSS in predicting increased plaque vulnerability [49]. Gijsen et al. were the first to show an in vivo relationship between high WSS and plaque strain [45]. They measured plaque strain at baseline and follow up, as a marker of the change in plaque composition, in 8 human coronary arteries from 7 patients referred for coronary interventions. Plaques were divided to upstream, throat, shoulder and downstream regions and IVUS-derived computational fluid dynamics (CFD) and palpography were used for WSS calculation and plaque strain analysis. The authors found a significant increase in plaque strain in those plaque regions exposed to highest tertile of WSS (average 39.3±15.3 dynes/cm2) at baseline indicating that those plaque regions became softer (and presumably more vulnerable) overtime. From 17 studied plaques, 12 showed a positive relationship between WSS and change in plaque strain (Figure 2B). Using reconstructions of 10 coronary arteries divided into 865 cross-sections (average of median value of WSS per cross-sectional area 40 46 dynes/cm2), Wentzel et al. showed that plaques residing in areas with above the median WSS value were associated with increased necrotic core and higher frequency of necrotic core contact with the lumen when compared with plaques residing in areas with less than the median WSS [48]. This conclusion is in line with the findings published by Gijsen et al [50] demonstrating that upstream, shoulder, and throat regions of a plaque had higher WSS values (25.5 8.9, 20.7 9.8, and 23.2 11.1 dynes/cm2, respectively) compared to the downstream segments (6.7 3.5 dynes/cm2). In that study, WSS was categorized as low, intermediate, or high based on the tertiles. They found that an increase in WSS correlated with an increase in radial strain (a marker for plaque structural integrity), suggesting that plaque segments exposed to high WSS were structurally weaker, and therefore more prone to rupture. In a recent cross-sectional study of 80 patients with suspected or known coronary artery disease, using coronary computed tomography angiography (CCTA)-derived CFD and WSS calculation (HeartFlow™ Analysis, HeartFlow Inc, Redwood City, California, USA), Park et al. investigated local hemodynamic characteristics within stenotic lesions (stenosis >30% by visual estimation) divided into minimal lumen area (MLA) (3 mm length) and relative upstream and downstream segments [46]. In this study, compared to segments with lowest (<55.8 dyne/cm2) and middle (55.8–111.9 dyne/cm2) tertiles of WSS, segments with highest tertile of WSS (>111.9 dyne/cm2) had a significantly greater proportion of plaques with high-risk features including low-density plaque, napkin-ring sign and expansive remodeling while spotty calcification was not observed in the lowest tertile of WSS at all. An interesting finding of this study was that while overall higher WSS was associated with higher odds ratio of high-risk plaques, the odds ratio of high-risk plaques increased at both extremes of WSS with the lowest odds ratio at around WSS of ≈40 dyne/cm2. The markedly higher absolute values of WSS in this study (range ≈0 to 500 dynes/cm2) compared to other human coronary studies however should be interpreted with caution since the WSS calculation was based on multiple assumptions used in the HeartFlow™ Analysis and not based on the patient-specific invasively measured velocity.
Figure 2.
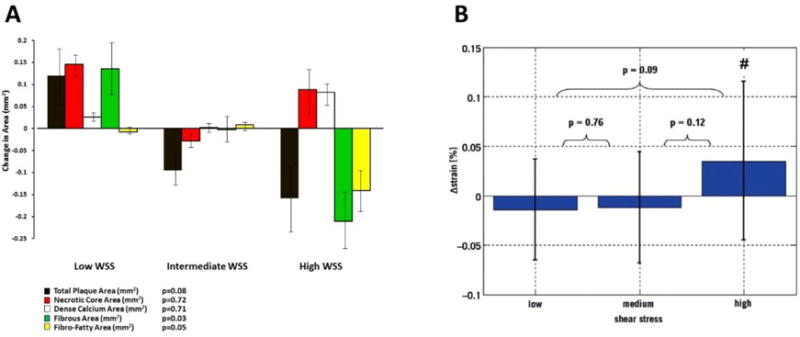
A) Change in plaque composition in low, intermediate, and high WSS segments over 6 months. WSS: wall shear stress (from Samady et al. [35]). B) Change in plaque strain in tertiles of WSS over 6 months. (# denotes that change is significantly different from zero at a p <0.05 level) (Reprinted from EuroIntervention 7/1, Gijsen et al., High shear stress induces a strain increase in human coronary plaques over a 6-month period, 121–127 [45], Copyright (2011), with permission from Europa Digital & Publishing).
While the above discussed studies provide evidence linking high WSS to high-risk plaque, not all studies have shown consistent results. The PREDICTION study is the largest cohort to describe the effects of WSS and vascular characteristics on plaque progression [36]. IVUS and angio-derived CFD and WSS calculation was done in 3 vessels of 374 high-risk patients presented with ACS (~60% STEMI). Each artery was divided into relatively large 3-mm segments. Stone et al. studied selected 15mm segments which had a discrete narrowing (throat) in the middle of the segment at baseline and luminal narrowing (>0.1mm2) in both upstream and downstream segments at 6- to 10-month follow-up. Tertiles of WSS in those selected 3mm segments (10 dynes/cm2 and 17 dynes/cm2) were used to define low, moderate and high WSS. The main finding of this study was that the lower baseline WSS was an independent predictor of higher plaque burden and smaller lumen at follow-up. In line with our previous findings, they also found that segments with baseline high WSS showed a reduction in both plaque area and plaque burden as well as an increase in lumen area at follow-up. While the values of WSS and plaque burden at the throat or the highest value of WSS in the 3mm segment were not reported, 73% of throat segments had high WSS at baseline (much higher than upstream and downstream segments) (Figure 4). Interestingly, the authors only assessed the relationship between downstream WSS and luminal narrowing at the throat, reporting that lower baseline WSS downstream to the throat was associated with worsening of luminal narrowing at the throat at follow-up. Therefore, the relationship between WSS at the throat and progression of luminal narrowing (and plaque burden) at the same location in this study is unknown. While this study is the only human study with clinical outcomes, the number of events were too few during the 1-year follow-up, leaving the trial underpowered to detect an association between WSS and clinical events and potentially high-risk plaques. In line with previous large studies, this study showed that the large plaque size at baseline was the most powerful predictor of increased plaque burden and worsening of clinically relevant luminal obstructions needing revascularization at follow-up. In a recently published cross-sectional study, optical coherence tomography (OCT)-derived CFD and plaque analysis was done in 30 patients with stable angina or ACS [51]. WSS was classified into low (≤25th percentile), moderate (between 25th and 75th percentiles), and high (≥75 percentile) based on the distribution of WSS values in each artery. While there is no information on the plaque size and number of FA in each WSS category, the authors showed that FA in low WSS segments had thinner fibrous cap compared with high WSS. Additionally, FA in low WSS segments were predominantly thin-cap FA (TCFA), while those FA in high WSS segments were predominantly thick-cap FA (ThCFA). The fact that low and high WSS in this study were relative to the distribution of WSS in each artery makes it difficult to compare the findings of this study with other studies using commonly used or at least known cutoff values for WSS. In another cross-sectional study, OCT-derived CFD and plaque analysis was done in 21 patients presenting with ACS [37]. Each coronary artery was divided into sequential 3mm segments and only nonculprit segments without significant stenosis were analyzed (total of 146 segments). In this study, segments with low WSS (<10 dynes/cm2) had higher prevalence of lipid-rich plaques and TCFA than segments with non-low (“higher”) WSS (≥10 dynes/cm2). Also, considering the limitations of OCT in quantification of macrophage density [52], they showed that lipid plaques in segments with low WSS had thinner fibrous cap and higher macrophage density. While the authors state that “normal WSS” is assumed to be between 10 and 25 dynes/cm2 and high WSS more frequently occurs at the throat of a stenosis, they divided WSS to low and non-low only and therefore reported the results for the combined normal and high WSS segments. More importantly, segments with “significant stenosis” (>40% area stenosis) were excluded from the analysis resulting in the relatively low median WSS value of 7.4 (IQR, 4.4–12.3) dynes/cm2, a very high prevalence of segments with low WSS (66%) and presumably very low prevalence of segments with high WSS (if any at all) in the study. Nevertheless, the clinical relevance of small plaques with thin fibrous cap is not well established [4].
Figure 4.
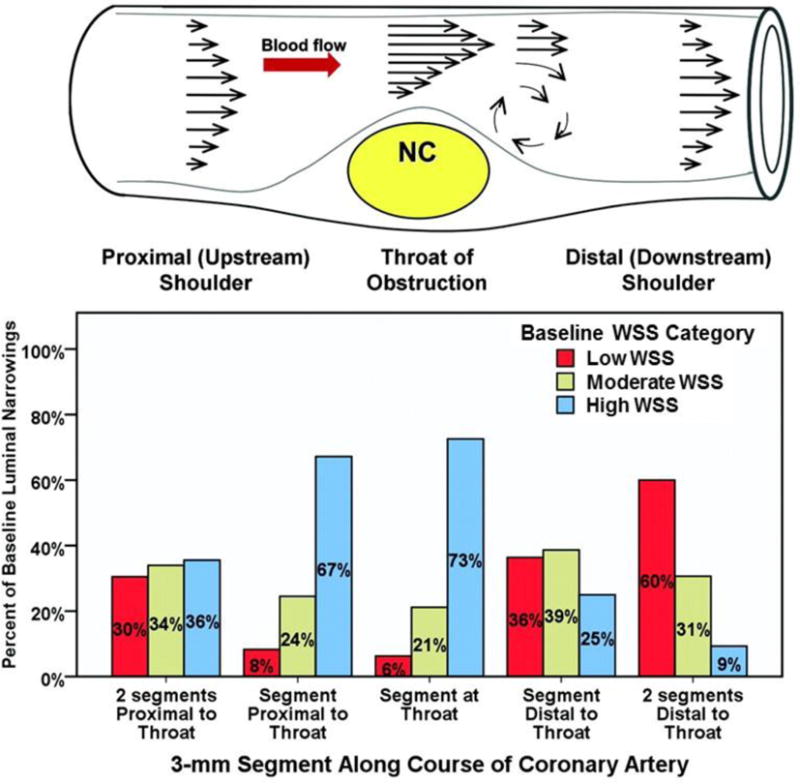
Baseline WSS patterns along the course of a coronary artery obstruction. The 3 WSS categories (low <10 dynes/cm2; moderate, 10–17 dynes/cm2; high >17 dynes/cm2) in the bar graph were derived from the terciles of the WSS frequency distribution in 3-mm segments. NC: necrotic core; WSS: wall shear stress (modified from Stone et al. [36] with permission).
The inconsistency between the findings of studies investigating the role of WSS in development of atherosclerosis has been shown in a systematic review and is mainly derived from differences in patient population, study duration, definitions, methodologies (CFD methods, side branch inclusions, velocity measurements, etc.), and endpoints [27,53]. Overall, it seems that the few studies [36,37,51] that failed to show an association between high WSS and high-risk plaques or showed an association between low WSS and features of high-risk plaques suffered from two common limitations: 1) dividing segments to only low and non-low WSS (no separation of high from normal/intermediate WSS) and/or 2) lack or limited number of segments with significant disease and therefore limited number of segments with high WSS. While the interplay between atherosclerotic plaque, artery, and WSS seems to be very dynamic and the exact mechanism of rapid plaque progression and triggers of expansive remodeling as well as the role of WSS in these processes is unclear, it is possible that both extremes of WSS (lower and higher than normal/physiologic WSS) are associated with high-risk plaque features at different phases of atherosclerotic plaque development. Nevertheless, the studies discussed above all have a consistent finding; the presence of higher WSS at the throat of the stenosis compared with both the upstream and downstream arterial segments. The dominance of high WSS and almost nonexistence of low WSS in the throat of relatively large plaques simply demonstrates the coexistence of high WSS with advanced atherosclerosis. While it is established that peak WSS increases with advanced plaque progression as a result of a narrower lumen [54], it is very well possible that high WSS has distinct effects on plaque progression and arterial remodeling during different phases of plaque development (early vs. advanced plaques). On one hand, it is believed that expansive remodeling is an adaptive response to elevated WSS, restoring WSS to a more physiological range and thus preserving luminal dimensions [55]. On the other hand, when inward progression of the plaque starts, subsequent plaque enlargement and lumen narrowing result in abnormally high values of WSS. It is possible that while some arteries manage to restore WSS to physiological values through expansive remodeling, the others fail and therefore continue having high WSS and expansive remodeling, possibly resulting in rapid plaque progression. Finally, it is difficult to know if the calculated high WSS at these locations is the result of the change in geometry and velocity affecting the calculation of WSS or high WSS is part of the numerous pathological changes resulting in development of these large plaques with features of high-risk or rupture-prone plaques.
High WSS and Individual Characteristics of High-Risk Plaque
a) High WSS and Intraplaque Hemorrhage
Intra-plaque hemorrhage is frequently observed in culprit plaques responsible for an ischemic clinical event, particularly in the carotid arteries [56]. As previously stated, IPH is thought to develop from rupture of a neovessel within the plaque, although plaque fissuring and associated incorporation of a non-occlusive thrombus has been hypothesized as an alternative mechanisms to IPH development [57]. The relationship between WSS and IPH was first shown in a serial imaging study of a carotid plaque, with a higher volume of IPH associated with high WSS [58]. High WSS at baseline was associated with subsequent ulceration at follow-up imaging. The relationship between WSS and IPH was further explored in a relatively large cross-sectional study in 93 carotid arteries of 74 asymptomatic participants from the Rotterdam Study who underwent magnetic resonance imaging for CFD simulations and plaque composition assessment [47]. The investigators found a relationship between higher maximum WSS and the presence of IPH and calcification, independent of plaque thickness, age, and sex. However, it is still unclear whether these observations represent a causative mechanism. WSS is known to become increased with progressive degrees of luminal stenosis and studies in carotid arteries have shown a clear link between stenosis severity and IPH [59]. Further longitudinal observational studies assessing the predictors of IPH are therefore required.
b) High WSS and Necrotic Core
Although human studies are few, the available evidence suggests a link between high WSS and plaque lipid accumulation. As discussed above, in addition to the study by Wetzel et al. [48] which showed a cross-sectional association between higher WSS and larger necrotic lipid core as well as increased necrotic core in contact with the lumen, two longitudinal studies investigated this relationship. Gijsen et al. [45] found a significant increase in plaque strain at 6-month follow-up in regions with high WSS at baseline, indicating that these regions got ‘softer’ overtime and therefore likely to have increased lipid deposition. Our group was the first to demonstrate a relationship between baseline high WSS and increase in necrotic core at 6-month follow-up using virtual-histology intravascular ultrasound (VH-IVUS) [35]. We also found a cross-sectional relationship between high WSS and larger plaques as well as larger necrotic cores in another study of 27 patients [34]. Of note, while several studies have shown high predictive accuracies for VH-IVUS compared to ex vivo human coronary histology [60,61] and in vivo directional coronary atherectomy specimens [62], one potential limitation of studies using VH-IVUS is that the presence of dense calcium may induce an artificial coding representing necrotic core in the adjacent tissue. Although these studies require further confirmation in larger patient cohorts, they suggest that high (or supraphysiological) WSS may be a determinant of increased lipid (necrotic core) accumulation, a known ‘high-risk’ plaque characteristic.
c) High WSS and Large Plaque
Multiple studies have shown that the predominant WSS found in segments with large plaque is the high WSS. In an analysis of patients with non-obstructive coronary artery disease, two-thirds of the segments within large plaques (plaque burden ≥40%) had high WSS, while only 4% of these segments had low WSS. In addition, there was a significant positive linear relationship between WSS and plaque burden in larger plaques (plaque burden ≥ 46%) [34] (Figure 3). In the previously mentioned longitudinal study of human coronary arteries, segments with high WSS had sufficient plaque burden (45.5±15.9%) at baseline to cause blood flow acceleration and elevated WSS without being flow limiting (as determined by fractional flow reserve) [35]. In line with these studies, another group found that WSS was significantly higher in stenotic segments (stenosis >30% by visual estimation) than non-stenotic segments (39.5% of stenotic segments were exposed to WSS >40 dyne/cm2) and WSS had the highest value in MLA location compared to upstream and downstream locations [46]. These findings are however not indicative of causal relationship between high WSS and larger plaques.
Figure 3.
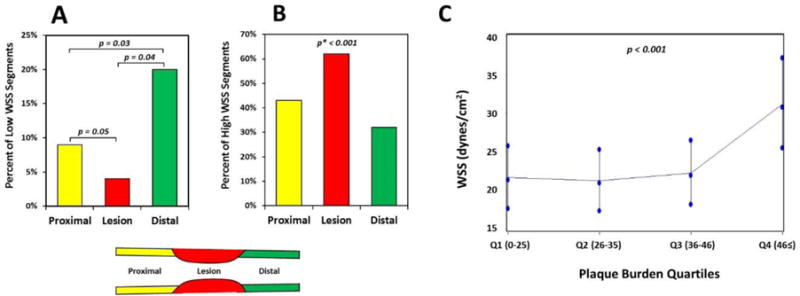
A) Percent of segments with low WSS (<10 dynes/cm2) within the lesions and proximal to and distal to lesions. B) Percent of segments with high WSS (≥25 dynes/cm2) within the lesions and proximal to and distal to lesions (*P value: the GLIMMIX procedure in SAS did not converge when fitting the statistical model for Figure 3B. Convergence was achieved when lesion and distal were consolidated into one category). C) Association between WSS and quartiles of plaque burden. The range of plaque burden in each quartile is shown in brackets (Error bars are 1 standard error). WSS: wall shear stress (from Eshtehardi et al. [34]).
d) High WSS and Arterial Remodeling
The relationship between high WSS and arterial expansive remodeling is more controversial than other high-risk plaque characteristics, with human studies reporting inconsistent results. In 12 patients with 6-month follow-up, Stone et al. observed a plaque progression and expansive (positive) static remodeling in regions with baseline low WSS, consistent with the results observed in animal models [63]. Interestingly, in a study of 13 patients with 8-month follow-up, the same group later showed that baseline low WSS regions were associated with plaque progression but constrictive static remodeling [64]. Following this, our group investigated the relationship between baseline low and high WSS and serial remodeling over 6 months [35]. Consistent with the results of the more recent study by Stone et al., constrictive serial remodeling was observed more frequently in low WSS regions. We also found for the first time that regions with baseline high WSS develop more excessive expansive (positive) serial remodeling compared to low and intermediate WSS regions. In line with our findings, a recently published cross-sectional study by Park et al., found greater proportion of plaques with expansive (positive) static remodeling in segments with the highest tertile of WSS compared to segments with lowest and middle tertiles of WSS [46].
e) High WSS and Plaque Structural Stress
Plaque structural stress (PSS) has been proposed as a potential mechanism for plaque rupture, occurs when intra-plaque stress exceeds the material strength of the overlying fibrous cap. High PSS has been observed in areas of plaque rupture in histological studies [65–67] and in vivo carotid studies have found PSS to be higher in patients presenting with symptoms of cerebral ischemia [68]. In addition, VH-IVUS-based PSS is shown to be higher in TCFAs as compared to ThCFAs and also in patients presenting with ACS as compared to stable angina [69]. In a relatively large longitudinal study, non-culprit lesions at baseline responsible for clinical events at follow-up at high-risk regions (i.e. plaque burden ≥70% and TCFA) showed significantly higher PSS compared to controls [19]. Furthermore, PSS improved the ability of VH-IVUS to predict clinical events in high-risk plaques, further implicating the role of PSS in the pathophysiology of plaque rupture. High WSS may also be involved in this process, acting in combination with PSS to promote plaque failure, as arterial regions that demonstrate high WSS are also associated with higher PSS. It is therefore possible that plaque rupture in high-risk coronary regions occurs when PSS and WSS exceed a critical threshold.
Summary
There is increasing evidence from both cross-sectional and longitudinal human studies to suggest that high WSS is frequently associated with high-risk plaque features. However, the role of WSS as a trigger for rapid plaque progression and expansive remodeling remains unclear and there remains ongoing debate as to whether changes in WSS magnitude are the driving force or consequential effect of atherosclerotic disease progression. Most importantly there is still insufficient data linking high WSS to the development of hard clinical events, including myocardial infarction. Large natural history studies of atherosclerosis in humans that include WSS measurements are now warranted.
Acknowledgments
Funding Source
P Eshtehardi and OY Hung received salary support from the Ruth L Kirschstein National Research Service Awards training grant (5T32HL007745). H Samady receives research funding from the Georgia Research Alliance, the Wallace H. Coulter Foundation, Volcano Corporation, St. Jude Medical, Gilead Sciences Inc., Medtronic Inc. and Abbott Vascular. DP Giddens receives research funding from the Georgia Research Alliance and the Wallace H. Coulter Foundation. AJ Brown is funded by the British Heart Foundation and the Academy of Medical Sciences. C Costopoulos is supported by the British Heart Foundation.
Abbreviations
- ACS
acute coronary syndrome
- CAD
coronary artery disease
- CCTA
coronary computed tomography angiography
- CFD
computational fluid dynamics
- FA
fibroatheroma
- IPH
intraplaque hemorrhage
- OCT
optical coherence tomography
- PSS
plaque structural stress
- TCFA
thin-cap fibroatheroma
- ThCFA
thick-cap fibroatheroma
- VH-IVUS
virtual histology intravascular ultrasound
- WSS
wall shear stress
Footnotes
Disclosures
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
- 1.Tarkin JM, Dweck MR, Evans NR, Takx RA, Brown AJ, Tawakol A, Fayad ZA, Rudd JH. Imaging Atherosclerosis. Circ Res. 2016;118:750–769. doi: 10.1161/CIRCRESAHA.115.306247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calvert PA, Obaid DR, O’Sullivan M, Shapiro LM, McNab D, Densem CG, Schofield PM, Braganza D, Clarke SC, Ray KK, West NE, Bennett MR. Association between IVUS findings and adverse outcomes in patients with coronary artery disease: the VIVA (VH-IVUS in Vulnerable Atherosclerosis) Study. JACC Cardiovascular Imaging. 2011;4:894–901. doi: 10.1016/j.jcmg.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Cheng JM, Garcia-Garcia HM, de Boer SPM, Kardys I, Heo JH, Akkerhuis KM, Oemrawsingh RM, van Domburg RT, Ligthart J, Witberg KT, Regar E, Serruys PW, van Geuns R-J, Boersma E. In vivo detection of high-risk coronary plaques by radiofrequency intravascular ultrasound and cardiovascular outcome: results of the ATHEROREMO-IVUS study. European Heart Journal. 2014;35:639–647. doi: 10.1093/eurheartj/eht484. [DOI] [PubMed] [Google Scholar]
- 4.Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J, Farhat N, Marso SP, Parise H, Templin B, White R, Zhang Z, Serruys PW. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–235. doi: 10.1056/NEJMoa1002358. [DOI] [PubMed] [Google Scholar]
- 5.Yahagi K, Kolodgie FD, Otsuka F, Finn AV, Davis HR, Joner M, Virmani R. Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis. Nature reviews Cardiology. 2016;13:79–98. doi: 10.1038/nrcardio.2015.164. [DOI] [PubMed] [Google Scholar]
- 6.Brown AJ, Teng Z, Evans PC, Gillard JH, Samady H, Bennett MR. Role of biomechanical forces in the natural history of coronary atherosclerosis. Nature reviews Cardiology. 2016;13:210–220. doi: 10.1038/nrcardio.2015.203. [DOI] [PubMed] [Google Scholar]
- 7.Hung OY, Brown AJ, Ahn SG, Veneziani A, Giddens DP, Samady H. Association of Wall Shear Stress with Coronary Plaque Progression and Transformation. Interventional Cardiology Clinics. 2015;4:491–502. doi: 10.1016/j.iccl.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Falk E, Nakano M, Bentzon JF, Finn AV, Virmani R. Update on acute coronary syndromes: the pathologists’ view. European heart journal. 2013;34:719–728. doi: 10.1093/eurheartj/ehs411. [DOI] [PubMed] [Google Scholar]
- 9.Campbell IC, Suever JD, Timmins LH, Veneziani A, Vito RP, Virmani R, Oshinski JN, Taylor WR. Biomechanics and inflammation in atherosclerotic plaque erosion and plaque rupture: implications for cardiovascular events in women. PloS one. 2014;9:e111785. doi: 10.1371/journal.pone.0111785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campbell IC, Timmins LH, Giddens DP, Virmani R, Veneziani A, Rab ST, Samady H, McDaniel MC, Finn AV, Taylor WR, Oshinski JN. Computational Fluid Dynamics Simulations of Hemodynamics in Plaque Erosion. Cardiovascular engineering and technology. 2013;4 doi: 10.1007/s13239-013-0165-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000;20:1262–1275. doi: 10.1161/01.atv.20.5.1262. [DOI] [PubMed] [Google Scholar]
- 12.Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW. A Definition of Advanced Types of Atherosclerotic Lesions and a Histological Classification of Atherosclerosis: A Report From the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation. 1995;92:1355–1374. doi: 10.1161/01.cir.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 13.Schaar JA, Muller JE, Falk E, Virmani R, Fuster V, Serruys PW, Colombo A, Stefanadis C, Ward CS, Moreno PR. Terminology for high-risk and vulnerable coronary artery plaques. Report of a meeting on the vulnerable plaque, June 17 and 18, 2003, Santorini, Greece. Eur Heart J. 2004;25:1077. doi: 10.1016/j.ehj.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, Abela GS, Franchi L, Nunez G, Schnurr M, Espevik T, Lien E, Fitzgerald KA, Rock KL, Moore KJ, Wright SD, Hornung V, Latz E. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464:1357–1361. doi: 10.1038/nature08938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burke AP, Farb A, Malcom GT, Liang YH, Smialek J, Virmani R. Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. New England Journal of Medicine. 1997;336:1276–1282. doi: 10.1056/NEJM199705013361802. [DOI] [PubMed] [Google Scholar]
- 16.Shah PK, Falk E, Badimon JJ, Fernandez-Ortiz A, Mailhac A, Villareal-Levy G, Fallon JT, Regnstrom J, Fuster V. Human monocyte-derived macrophages induce collagen breakdown in fibrous caps of atherosclerotic plaques. Potential role of matrix-degrading metalloproteinases and implications for plaque rupture. Circulation. 1995;92:1565–1569. [PubMed] [Google Scholar]
- 17.Bertazzo S, Gentleman E, Cloyd KL, Chester AH, Yacoub MH, Stevens MM. Nano-analytical electron microscopy reveals fundamental insights into human cardiovascular tissue calcification. Nat Mater. 2013;12:576–583. doi: 10.1038/nmat3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelly-Arnold A, Maldonado N, Laudier D, Aikawa E, Cardoso L, Weinbaum S. Revised microcalcification hypothesis for fibrous cap rupture in human coronary arteries. Proceedings of the National Academy of Sciences. 2013;110:10741–10746. doi: 10.1073/pnas.1308814110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown AJ, Teng Z, Calvert PA, Rajani NK, Hennessy O, Nerlekar N, Obaid DR, Costopoulos C, Huang Y, Hoole SP, Goddard M, West NE, Gillard JH, Bennett MR. Plaque Structural Stress Estimations Improve Prediction of Future Major Adverse Cardiovascular Events After Intracoronary Imaging. Circulation Cardiovascular imaging. 2016;9:e004172. doi: 10.1161/CIRCIMAGING.115.004172. [DOI] [PubMed] [Google Scholar]
- 20.Bentzon JF, Otsuka F, Virmani R, Falk E. Mechanisms of plaque formation and rupture. Circ Res. 2014;114:1852–1866. doi: 10.1161/CIRCRESAHA.114.302721. [DOI] [PubMed] [Google Scholar]
- 21.Sluimer JC, Kolodgie FD, Bijnens AP, Maxfield K, Pacheco E, Kutys B, Duimel H, Frederik PM, van Hinsbergh VW, Virmani R, Daemen MJ. Thin-walled microvessels in human coronary atherosclerotic plaques show incomplete endothelial junctions relevance of compromised structural integrity for intraplaque microvascular leakage. J Am Coll Cardiol. 2009;53:1517–1527. doi: 10.1016/j.jacc.2008.12.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michel JB, Virmani R, Arbustini E, Pasterkamp G. Intraplaque haemorrhages as the trigger of plaque vulnerability. Eur Heart J. 2011;32:1977–1985. 1985a, 1985b, 1985c. doi: 10.1093/eurheartj/ehr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Varnava AM, Mills PG, Davies MJ. Relationship between coronary artery remodeling and plaque vulnerability. Circulation. 2002;105:939–943. doi: 10.1161/hc0802.104327. [DOI] [PubMed] [Google Scholar]
- 24.Ahmadi A, Leipsic J, Blankstein R, Taylor C, Hecht H, Stone GW, Narula J. Do plaques rapidly progress prior to myocardial infarction? The interplay between plaque vulnerability and progression. Circulation research. 2015;117:99–104. doi: 10.1161/CIRCRESAHA.117.305637. [DOI] [PubMed] [Google Scholar]
- 25.Burke AP, Kolodgie FD, Farb A, Weber DK, Malcom GT, Smialek J, Virmani R. Healed plaque ruptures and sudden coronary death: evidence that subclinical rupture has a role in plaque progression. Circulation. 2001;103:934–940. doi: 10.1161/01.cir.103.7.934. [DOI] [PubMed] [Google Scholar]
- 26.Eshtehardi P, Teng Z. Protective or destructive: High wall shear stress and atherosclerosis. Atherosclerosis. 2016;251:501–503. doi: 10.1016/j.atherosclerosis.2016.05.046. [DOI] [PubMed] [Google Scholar]
- 27.Peiffer V, Sherwin SJ, Weinberg PD. Does low and oscillatory wall shear stress correlate spatially with early atherosclerosis? A systematic review. Cardiovasc Res. 2013;99:242–250. doi: 10.1093/cvr/cvt044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheng WP, Wang BW, Chen SC, Chang H, Shyu KG. Mechanical stretch induces the apoptosis regulator PUMA in vascular smooth muscle cells. Cardiovasc Res. 2012;93:181–189. doi: 10.1093/cvr/cvr280. [DOI] [PubMed] [Google Scholar]
- 29.Slager CJ, Wentzel JJ, Gijsen FJ, Schuurbiers JC, van der Wal AC, van der Steen AF, Serruys PW. The role of shear stress in the generation of rupture-prone vulnerable plaques. Nat Clin Pract Cardiovasc Med. 2005;2:401–407. doi: 10.1038/ncpcardio0274. [DOI] [PubMed] [Google Scholar]
- 30.Wentzel JJ, Chatzizisis YS, Gijsen FJ, Giannoglou GD, Feldman CL, Stone PH. Endothelial shear stress in the evolution of coronary atherosclerotic plaque and vascular remodelling: current understanding and remaining questions. Cardiovasc Res. 2012;96:234–243. doi: 10.1093/cvr/cvs217. [DOI] [PubMed] [Google Scholar]
- 31.Kwak BR, Back M, Bochaton-Piallat ML, Caligiuri G, Daemen MJ, Davies PF, Hoefer IE, Holvoet P, Jo H, Krams R, Lehoux S, Monaco C, Steffens S, Virmani R, Weber C, Wentzel JJ, Evans PC. Biomechanical factors in atherosclerosis: mechanisms and clinical implications. European heart journal. 2014;35:3013–3020. 3020a–3020d. doi: 10.1093/eurheartj/ehu353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pan S. Molecular mechanisms responsible for the atheroprotective effects of laminar shear stress. Antioxid Redox Signal. 2009;11:1669–1682. doi: 10.1089/ars.2009.2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fulton D, Gratton JP, McCabe TJ, Fontana J, Fujio Y, Walsh K, Franke TF, Papapetropoulos A, Sessa WC. Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601. doi: 10.1038/21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eshtehardi P, McDaniel MC, Suo J, Dhawan SS, Timmins LH, Binongo JN, Golub LJ, Corban MT, Finn AV, Oshinski JN, Quyyumi AA, Giddens DP, Samady H. Association of coronary wall shear stress with atherosclerotic plaque burden, composition, and distribution in patients with coronary artery disease. Journal of the American Heart Association. 2012;1:e002543. doi: 10.1161/JAHA.112.002543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Samady H, Eshtehardi P, McDaniel MC, Suo J, Dhawan SS, Maynard C, Timmins LH, Quyyumi AA, Giddens DP. Coronary artery wall shear stress is associated with progression and transformation of atherosclerotic plaque and arterial remodeling in patients with coronary artery disease. Circulation. 2011;124:779–788. doi: 10.1161/CIRCULATIONAHA.111.021824. [DOI] [PubMed] [Google Scholar]
- 36.Stone PH, Saito S, Takahashi S, Makita Y, Nakamura S, Kawasaki T, Takahashi A, Katsuki T, Nakamura S, Namiki A, Hirohata A, Matsumura T, Yamazaki S, Yokoi H, Tanaka S, Otsuji S, Yoshimachi F, Honye J, Harwood D, Reitman M, Coskun AU, Papafaklis MI, Feldman CL. Prediction of progression of coronary artery disease and clinical outcomes using vascular profiling of endothelial shear stress and arterial plaque characteristics: the PREDICTION Study. Circulation. 2012;126:172–181. doi: 10.1161/CIRCULATIONAHA.112.096438. [DOI] [PubMed] [Google Scholar]
- 37.Vergallo R, Papafaklis MI, Yonetsu T, Bourantas CV, Andreou I, Wang Z, Fujimoto JG, McNulty I, Lee H, Biasucci LM, Crea F, Feldman CL, Michalis LK, Stone PH, Jang IK. Endothelial shear stress and coronary plaque characteristics in humans: combined frequency-domain optical coherence tomography and computational fluid dynamics study. Circulation Cardiovascular imaging. 2014;7:905–911. doi: 10.1161/CIRCIMAGING.114.001932. [DOI] [PubMed] [Google Scholar]
- 38.Zaromytidou M, Siasos G, Coskun AU, Lucier M, Antoniadis AP, Papafaklis MI, Koskinas KC, Andreou Y, Feldman CL, Stone PH. Intravascular hemodynamics and coronary artery disease: new insights and clinical implications. Hellenic journal of cardiology: HJC = Hellenike kardiologike epitheorese. 2016 doi: 10.1016/j.hjc.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 39.Fukumoto Y, Hiro T, Fujii T, Hashimoto G, Fujimura T, Yamada J, Okamura T, Matsuzaki M. Localized Elevation of Shear Stress Is Related to Coronary Plaque Rupture: A 3-Dimensional Intravascular Ultrasound Study With In-Vivo Color Mapping of Shear Stress Distribution. Journal of the American College of Cardiology. 2008;51:645–650. doi: 10.1016/j.jacc.2007.10.030. [DOI] [PubMed] [Google Scholar]
- 40.White SJ, Hayes EM, Lehoux S, Jeremy JY, Horrevoets AJG, Newby AC. Characterization of the Differential Response of Endothelial Cells Exposed to Normal and Elevated Laminar Shear Stress. Journal of cellular physiology. 2011;226:2841–2848. doi: 10.1002/jcp.22629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Castier Y, Brandes RP, Leseche G, Tedgui A, Lehoux S. P47phox-dependent NADPH oxidase regulates flow-induced vascular remodeling. Circ Res. 2005;97:533–540. doi: 10.1161/01.RES.0000181759.63239.21. [DOI] [PubMed] [Google Scholar]
- 42.Dhawan SS, Avati Nanjundappa RP, Branch JR, Taylor WR, Quyyumi AA, Jo H, McDaniel MC, Suo J, Giddens D, Samady H. Shear stress and plaque development. Expert Rev Cardiovasc Ther. 2010;8:545–556. doi: 10.1586/erc.10.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lovett JK, Rothwell PM. Site of carotid plaque ulceration in relation to direction of blood flow: an angiographic and pathological study. Cerebrovasc Dis. 2003;16:369–375. doi: 10.1159/000072559. [DOI] [PubMed] [Google Scholar]
- 44.Dirksen MT, van der Wal AC, van den Berg FM, van der Loos CM, Becker AE. Distribution of inflammatory cells in atherosclerotic plaques relates to the direction of flow. Circulation. 1998;98:2000–2003. doi: 10.1161/01.cir.98.19.2000. [DOI] [PubMed] [Google Scholar]
- 45.Gijsen FJ, Mastik F, Schaar JA, Schuurbiers JC, van der Giessen WJ, de Feyter PJ, Serruys PW, van der Steen AF, Wentzel JJ. High shear stress induces a strain increase in human coronary plaques over a 6-month period. EuroIntervention: journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2011;7:121–127. doi: 10.4244/EIJV7I1A20. [DOI] [PubMed] [Google Scholar]
- 46.Park JB, Choi G, Chun EJ, Kim HJ, Park J, Jung JH, Lee MH, Otake H, Doh JH, Nam CW, Shin ES, De Bruyne B, Taylor CA, Koo BK. Computational fluid dynamic measures of wall shear stress are related to coronary lesion characteristics. Heart (British Cardiac Society) 2016;102:1655–1661. doi: 10.1136/heartjnl-2016-309299. [DOI] [PubMed] [Google Scholar]
- 47.Tuenter A, Selwaness M, Arias Lorza A, Schuurbiers JC, Speelman L, Cibis M, van der Lugt A, de Bruijne M, van der Steen AF, Franco OH, Vernooij MW, Wentzel JJ. High shear stress relates to intraplaque haemorrhage in asymptomatic carotid plaques. Atherosclerosis. 2016;251:348–354. doi: 10.1016/j.atherosclerosis.2016.05.018. [DOI] [PubMed] [Google Scholar]
- 48.Wentzel JJ, Schuurbiers JC, Gonzalo Lopez N, Gijsen FJ, van der Giessen AG, Groen HC, Dijkstra J, Garcia-Garcia HM, Serruys PW. In vivo assessment of the relationship between shear stress and necrotic core in early and advanced coronary artery disease. EuroIntervention: journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2013;9:989–995. doi: 10.4244/EIJV9I8A165. discussion 995. [DOI] [PubMed] [Google Scholar]
- 49.Corban MT, Eshtehardi P, Suo J, McDaniel MC, Timmins LH, Rassoul-Arzrumly E, Maynard C, Mekonnen G, King S, 3rd, Quyyumi AA, Giddens DP, Samady H. Combination of plaque burden, wall shear stress, and plaque phenotype has incremental value for prediction of coronary atherosclerotic plaque progression and vulnerability. Atherosclerosis. 2014;232:271–276. doi: 10.1016/j.atherosclerosis.2013.11.049. [DOI] [PubMed] [Google Scholar]
- 50.Gijsen FJ, Wentzel JJ, Thury A, Mastik F, Schaar JA, Schuurbiers JC, Slager CJ, van der Giessen WJ, de Feyter PJ, van der Steen AF, Serruys PW. Strain distribution over plaques in human coronary arteries relates to shear stress. American journal of physiology Heart and circulatory physiology. 2008;295:H1608–1614. doi: 10.1152/ajpheart.01081.2007. [DOI] [PubMed] [Google Scholar]
- 51.Chatzizisis YS, Toutouzas K, Giannopoulos AA, Riga M, Antoniadis AP, Fujinom Y, Mitsouras D, Koutkias VG, Cheimariotis G, Doulaverakis C, Tsampoulatidis I, Chouvarda I, Kompatsiaris I, Nakamura S, Rybicki FJ, Maglaveras N, Tousoulis D, Giannoglou GD. Association of global and local low endothelial shear stress with high-risk plaque using intracoronary 3D optical coherence tomography: Introduction of ‘shear stress score’. European heart journal cardiovascular Imaging. 2016 doi: 10.1093/ehjci/jew134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Phipps JE, Vela D, Hoyt T, Halaney DL, Mancuso JJ, Buja LM, Asmis R, Milner TE, Feldman MD. Macrophages and intravascular OCT bright spots: a quantitative study. JACC Cardiovascular imaging. 2015;8:63–72. doi: 10.1016/j.jcmg.2014.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li Y, Gutierrez-Chico JL, Holm NR, Yang W, Hebsgaard L, Christiansen EH, Maeng M, Lassen JF, Yan F, Reiber JH, Tu S. Impact of Side Branch Modeling on Computation of Endothelial Shear Stress in Coronary Artery Disease: Coronary Tree Reconstruction by Fusion of 3D Angiography and OCT. J Am Coll Cardiol. 2015;66:125–135. doi: 10.1016/j.jacc.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 54.Yang C, Canton G, Yuan C, Ferguson M, Hatsukami TS, Tang D. Advanced human carotid plaque progression correlates positively with flow shear stress using follow-up scan data: an in vivo MRI multi-patient 3D FSI study. J Biomech. 2010;43:2530–2538. doi: 10.1016/j.jbiomech.2010.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zarins CK, Zatina MA, Giddens DP, Ku DN, Glagov S. Shear stress regulation of artery lumen diameter in experimental atherogenesis. J Vasc Surg. 1987;5:413–420. [PubMed] [Google Scholar]
- 56.Teng Z, Sadat U, Brown AJ, Gillard JH. Plaque hemorrhage in carotid artery disease: pathogenesis, clinical and biomechanical considerations. J Biomech. 2014;47:847–858. doi: 10.1016/j.jbiomech.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davies MJ, Thomas AC. Plaque fissuring–the cause of acute myocardial infarction, sudden ischaemic death, and crescendo angina. Br Heart J. 1985;53:363–373. doi: 10.1136/hrt.53.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Groen HC, Gijsen FJ, van der Lugt A, Ferguson MS, Hatsukami TS, van der Steen AF, Yuan C, Wentzel JJ. Plaque rupture in the carotid artery is localized at the high shear stress region: a case report. Stroke. 2007;38:2379–2381. doi: 10.1161/STROKEAHA.107.484766. [DOI] [PubMed] [Google Scholar]
- 59.McLaughlin MS, Hinckley PJ, Treiman SM, Kim SE, Stoddard GJ, Parker DL, Treiman GS, McNally JS. Optimal Prediction of Carotid Intraplaque Hemorrhage Using Clinical and Lumen Imaging Markers. AJNR Am J Neuroradiol. 2015;36:2360–2366. doi: 10.3174/ajnr.A4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002;106:2200–2206. doi: 10.1161/01.cir.0000035654.18341.5e. [DOI] [PubMed] [Google Scholar]
- 61.Nair A, Margolis MP, Kuban BD, Vince DG. Automated coronary plaque characterisation with intravascular ultrasound backscatter: ex vivo validation. EuroIntervention: journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2007;3:113–120. [PubMed] [Google Scholar]
- 62.Nasu K, Tsuchikane E, Katoh O, Vince DG, Virmani R, Surmely JF, Murata A, Takeda Y, Ito T, Ehara M, Matsubara T, Terashima M, Suzuki T. Accuracy of in vivo coronary plaque morphology assessment: a validation study of in vivo virtual histology compared with in vitro histopathology. J Am Coll Cardiol. 2006;47:2405–2412. doi: 10.1016/j.jacc.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 63.Stone PH, Coskun AU, Kinlay S, Clark ME, Sonka M, Wahle A, Ilegbusi OJ, Yeghiazarians Y, Popma JJ, Orav J, Kuntz RE, Feldman CL. Effect of endothelial shear stress on the progression of coronary artery disease, vascular remodeling, and in-stent restenosis in humans: in vivo 6-month follow-up study. Circulation. 2003;108:438–444. doi: 10.1161/01.CIR.0000080882.35274.AD. [DOI] [PubMed] [Google Scholar]
- 64.Stone PH, Coskun AU, Kinlay S, Popma JJ, Sonka M, Wahle A, Yeghiazarians Y, Maynard C, Kuntz RE, Feldman CL. Regions of low endothelial shear stress are the sites where coronary plaque progresses and vascular remodelling occurs in humans: an in vivo serial study. European heart journal. 2007;28:705–710. doi: 10.1093/eurheartj/ehl575. [DOI] [PubMed] [Google Scholar]
- 65.Richardson PD, Davies MJ, Born GV. Influence of plaque configuration and stress distribution on fissuring of coronary atherosclerotic plaques. Lancet. 1989;2:941–944. doi: 10.1016/s0140-6736(89)90953-7. [DOI] [PubMed] [Google Scholar]
- 66.Loree HM, Kamm RD, Stringfellow RG, Lee RT. Effects of fibrous cap thickness on peak circumferential stress in model atherosclerotic vessels. Circ Res. 1992;71:850–858. doi: 10.1161/01.res.71.4.850. [DOI] [PubMed] [Google Scholar]
- 67.Huang H, Virmani R, Younis H, Burke AP, Kamm RD, Lee RT. The impact of calcification on the biomechanical stability of atherosclerotic plaques. Circulation. 2001;103:1051–1056. doi: 10.1161/01.cir.103.8.1051. [DOI] [PubMed] [Google Scholar]
- 68.Tang D, Teng Z, Canton G, Yang C, Ferguson M, Huang X, Zheng J, Woodard PK, Yuan C. Sites of rupture in human atherosclerotic carotid plaques are associated with high structural stresses: an in vivo MRI-based 3D fluid-structure interaction study. Stroke. 2009;40:3258–3263. doi: 10.1161/STROKEAHA.109.558676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Teng Z, Brown AJ, Calvert PA, Parker RA, Obaid DR, Huang Y, Hoole SP, West NE, Gillard JH, Bennett MR. Coronary plaque structural stress is associated with plaque composition and subtype and higher in acute coronary syndrome: the BEACON I (Biomechanical Evaluation of Atheromatous Coronary Arteries) study. Circulation Cardiovascular imaging. 2014;7:461–470. doi: 10.1161/CIRCIMAGING.113.001526. [DOI] [PubMed] [Google Scholar]


