Abstract
Context:
Anterior knee pain (AKP) represents the most common reason to consult with a clinician who specializes in the knee. Despite the high incidence of the disorder, however, its etiology is still controversial. Many unnecessary surgeries that may damage the patient are done for this clinical entity.
Evidence Acquisition:
A PubMed search from 1995 through June 2016.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
The etiology of AKP is multifactorial, and patients with AKP may therefore be divided into several subpopulations. The whole picture must be addressed for each patient to identify all potentially modifiable factors and to achieve better outcomes. Both pelvifemoral dysfunction and psychological factors that may affect the development and symptoms of AKP must be considered to identify therapeutic targets within the context of treatment. Patients presenting with AKP frequently respond well to load restriction that protects their knee and reduces pain during rehabilitation. Surgery should only be considered in very select cases. In a patient who has undergone previous patellar realignment surgery and experienced increased pain, iatrogenic medial patellar instability should be considered.
Conclusions:
The etiology of AKP is multifactorial, and several subpopulations of AKP patients exist and their treatment must be personalized. Normally, the focus is on the knee of a patient with AKP, and only that joint is examined. However, that focus can lead to overlooking other important etiological factors that may be present.
Keywords: anterior knee pain, patellofemoral pain, homeostasis, psychological factors, femoral torsion
Anterior knee pain (AKP) represents the most common reason to consult with a clinician who specializes in the knee.1 Despite the high incidence of the disorder, however, its etiology is still controversial.25 Moreover, a clear association is lacking between objective factors and subjective complaints of pain and discomfort.25 A clear understanding of the cause of pain is crucial to properly selecting treatment, whether it is nonsurgical or surgical. The etiology of AKP is multifactorial, and patients with AKP may therefore be divided into several subpopulations.1,25 The variety of factors might explain the very often unpredictable results of treatment. AKP can be very frustrating for both the patient and the treating physician, not only because of the unpredictable results but also because of the recurrence rate; restrictions to the patient’s daily physical activity; time off work; lack of understanding among family members, colleagues, and others; and the generally decreased quality of life. Between 70% and 90% of patients with AKP experience recurrent or chronic pain.1
It has long been accepted that a direct relation exists between tissue damage and/or structural changes and AKP. However, this classic “biomedical model,” which has conventionally been used to identify the best treatment, is not necessarily the appropriate approach for the patient with AKP. The goal of this article is to analyze how to deal with AKP in the active young patient in order to offer effective and safe treatment. The whole picture for each patient must be considered to identify all potentially modifiable factors and to achieve better outcomes.
Think of Soft Tissues First
When a patient is seen with AKP, first think about soft tissues (synovial tissue, Hoffa fat pad, and lateral retinaculum) as the primary source of the discomfort because all of these are well-innervated structures.10 Improvement in the patient’s pain after selective use of local anesthetics or through use of bandaging/taping to unload specific anatomical innervated structures that are inflamed and sensitive, support the conclusion of soft tissues of the knee being the origin of pain.7
Soft tissue impingement (peripatellar synovitis, suprapatellar fat pad impingement, and Hoffa fat pad impingement) or infrapatellar fat pad edema can generate pain by producing transitory ischemia, and therefore the loss of homeostasis, as well as by producing mechanical stimulation of nociceptors (Figure 1).25,35 In these patients, a peripatellar synovectomy may be a good option when there is a persistent AKP refractory to conservative measures of load restriction, cooling, and safe, nonpainful physical therapy. Soft tissue impingement can also be associated with osseous hypertension, which can produce transitory ischemia and mechanical stimulation of nociceptors.25 Patients with an increase of the intraosseous hypertension of the patella with a positive “pain provocation test” (pain reproduced by raising intrapatellar pressure) could be good candidates for extra-articular patellar decompression.21 This increase in the intraosseous pressure of the patella occurs in patients with AKP who experience pain when sitting with a bent knee (“movie sign”). In theory, it is secondary to a temporary obstruction of venous flow.1 Focal synovial hypertrophy around the inferior patellar pole may also be responsible for AKP.20 Patients unresponsive to nonoperative management could be good candidates to arthroscopic peripatellar synovectomy.20
Figure 1.
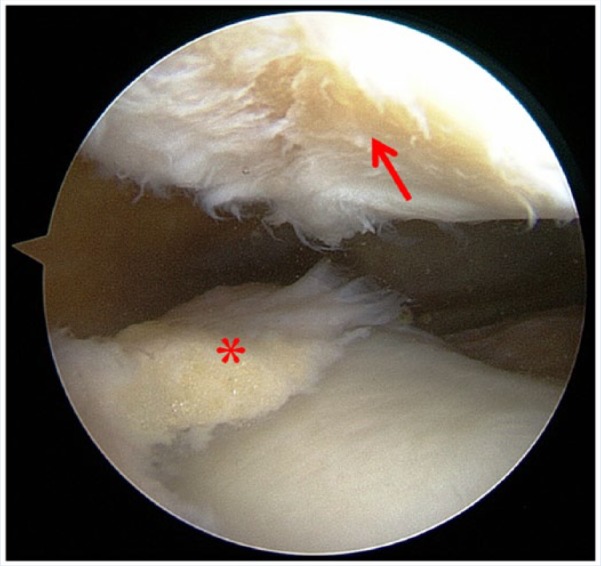
Anterior knee pain intensity is not related to the severity or the extension of the chondropathy of the patellae (arrow) found during surgery. In this particular patient, pain disappeared after an isolated arthroscopic partial synovectomy (asterisk) without specific treatment of the chondropathy.
Another potential source of AKP is the saphenous nerve injury/irritation after medial blunt trauma or prior knee surgery; it can even occur spontaneously. The patient presents with sharp burning pain, hyperesthesia, and/or allodynia (neuropathic pain). Medications such as gabapentin can have an ameliorative effect in such cases.16
The origin of pain is the lateral retinaculum in only a few cases.26,30 Histologic evidence of nerve injury (neuromas, microneuromas, and neural myxoid degeneration) in the lateral retinaculum has been shown to be related to chronic patella imbalance.30 In these cases, the pain is secondary to the loss of chemical/biologic homeostasis,25,35 and it is neuropathic (ie, caused by neurologic damage).35 In patients with clear signs and symptoms of lateral patellar hypercompression syndrome, lateral retinaculum release is indicated after failure of an adequate conservative treatment.26 A lateral retinacular lengthening could be considered in these patients. It has the same effect regarding elimination of hypercompression and hypertension on the lateral side as the lateral retinacular release. However, it avoids the secondary complications of lateral retinacular release, such as medial patellar instability. If the lateral retinaculum is not tight, however, it should not be released. Moreover, an isolated lateral retinaculum release should never be performed in the presence of trochlear dysplasia, patella alta, or hyperelasticity.26
Beware of Structural Anomalies
Structural anomalies do not provide a complete explanation of the pain experienced by patients with AKP.25 In fact, structural anomalies (patellar chondropathy, patellofemoral malalignment, patellar tilt and/or lateral patellar subluxation) and AKP are poorly correlated; that is, structural anomalies are often not responsible for the pain (Figure 1).17,25 Therefore, detecting a structural anomaly is not a “green light” to correct it surgically. The worst AKP may occur secondary to a surgical procedure intended to correct structural anomalies that in retrospect were probably unrelated to the patient’s pain and disability.
There does not appear to be link between the outcome (positive or negative) and the presence or absence of patellofemoral malalignment after realignment surgery.25 This may mean that patellofemoral malalignment after a realignment surgery is not always associated with pain. In addition, patellofemoral chondropathy is extremely common, and only a small number of patients with a patellar chondral lesion have AKP related to it. Patellofemoral chondropathies that are found incidentally while addressing other pathology should probably be left alone.12 AKP in young patients has typically been termed “chondromalacia patellae.” However, that disorder is not synonymous with patellofemoral pain, and it is incorrect to use it to describe a clinical condition. Therefore, it is imperative, even in patients with evident structural anomalies, to search for alternative causes of AKP. Finally, it should be noted that, structural anomalies are either minor or completely absent in a very high percentage of patients with AKP.9
In selected cases, structural anomalies can cause AKP. For example, a softening of the distal pole of the patella can trigger disabling pain that is completely recalcitrant to conservative treatment.15 In these patients, the pain is theoretically secondary to excessive stress on the underlying innervated bone due to the altered ability of the cartilage to distribute pressures to the subchondral bone. In these patients, a short, steep anteromedial tibial tubercle transfer could relieve pain due to the unloading effect of this type of osteotomy.15 However, this surgical technique must be targeted to patients with very clear clinical findings and intractable pain.
A Tissue Homeostasis Perspective
According to the tissue homeostasis theory, joints are not simply mechanical structures, they are systems that are alive and metabolically active.8,9 Pain arises from a pathophysiological mosaic of causes, including increased osseous remodeling, increased intraosseous pressure, or peripatellar synovitis leading to a reduced “envelope of function” (or “envelope of load acceptance”).9 This envelope of function is defined by the range of loading and energy absorption that coexists with normal tissue healing and maintenance (ie, tissue homeostasis). The envelope of function is obviously greater for a young athlete than for a sedentary elderly individual. Loads that surpass the envelope of function but do not cause macrostructural failure trigger a supraphysiologic overload. However, if the patellofemoral system experiences high enough forces, macrostructural failure can happen (Figure 2).
Figure 2.
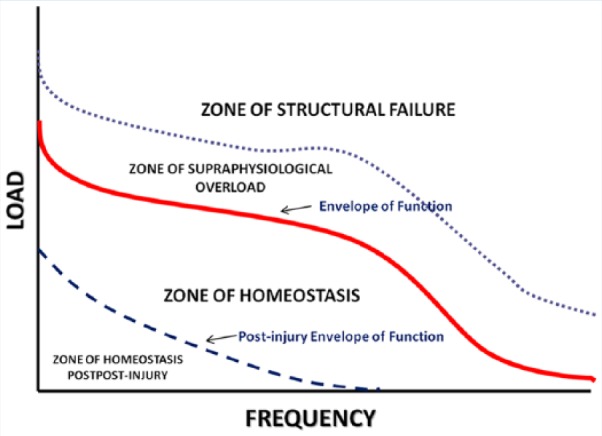
Four sets of factors define the envelope of function, which may also be called the “zone of homeostasis.”8 The first set encompasses anatomic factors such as a tissue’s morphology, structural integrity, and biomechanical characteristics. The second set includes kinematic factors, which involve the dynamic control of a joint and include proprioceptive sensory output, sequencing of motor units within the brain, reflex mechanisms in the spine, and muscle strength and motor control. Physiological factors compose the third set and include the underlying genetic contributions to molecular and cellular homeostatic mechanisms that control the quality and rate of healing. Finally, treatment factors comprise the type of rehabilitation and surgery.
Technetium-99m-methyl diphosphonate (technetium-99m-MDP) scintigraphy can reveal the metabolic and geographic characteristics of bone homeostasis, which is the normal osseous metabolic status of a living joint. A relationship between an abnormally increased technetium bone scan of the patellofemoral joint and AKP has been demonstrated.9 Moreover, an association between restoration to a normal bone scan and AKP resolution after conservative treatment has been documented.9 However, the loss of tissue homeostasis is not limited to osseous components.
Patients who initially present with AKP often respond well to load restriction because it tailors their envelope of function to the current state of their knee and permits pain-free rehabilitation.9 Documenting which activities trigger pain is critical. Those activities lie outside the envelope of function and need to be avoided or minimized for healing to occur. This restriction does not mean that the patient must be sedentary. In fact, it is best that the patient remains as active as possible. Activity cannot exceed the upper limit of the joint’s envelope of function, but within that parameter all kinds of activities are acceptable.8 The objective of this activity is to maintain muscle condition and the joint’s range of motion without overloading it. Any activity that provokes pain within the patellofemoral joint indicates supraphysiologic loading that will subvert the normal healing process.
Look Beyond the Patellofemoral Joint for the Primary Cause of AKP
The main problem with AKP has been long assumed to involve the patella. However, a growing body of literature links abnormal femur rotation with AKP.3,13,18,23,31,34,36 When the femur rotates under the patella in the transverse plane, abnormal patellar tracking occurs along with patellofemoral imbalance and subsequent pain (Figure 3).25 In these patients, the primary problem lies in the femur, not in the patella. In a small number of patients, femur malrotation is secondary to structural anomalies (eg, femoral anteversion or torsional anomaly secondary to femoral fracture),18,34,36 but in most patients the malrotation is functional (eg, secondary to a weak hip musculature).3,23,31 This last link is supported by strengthening of hip abductors and external rotator muscles, effectively improving pain in this AKP patient subgroup, which is mostly female.19
Figure 3.
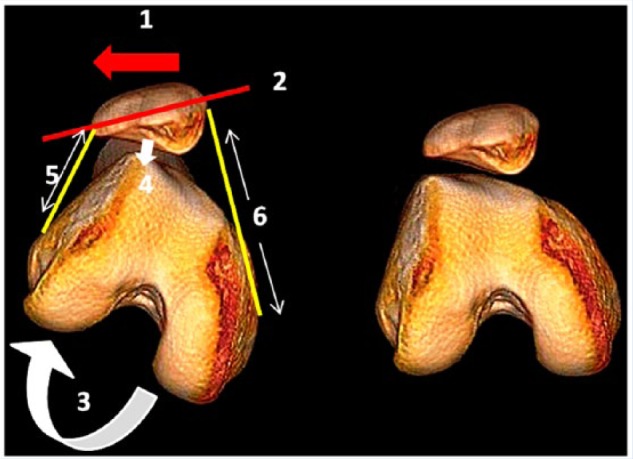
Three-dimensional computed tomography demonstrating abnormal patellar tracking secondary to femoral internal rotation. On the right is a normal knee. The left shows how the rotating movement of the femur underneath the patella in the transverse plane leads to abnormal patellar tracking (1, lateral patellar subluxation and 2, patellar tilt). The patella maintains a horizontal position while the femur internally rotates; therefore, the patellar subluxation is not the result of patella moving on the femur but of the result of the femur rotating underneath the patella. 3, inward twisting of the knee. 4 (arrow), compression in the lateral patellofemoral joint increases. 5, retracted lateral retinaculum. 6, tension increases in the medial retinaculum. The final result is patellofemoral imbalance.
Most studies analyze the importance of internal femoral rotation in the genesis of AKP, but only a few have focused on external femoral rotation. An external rotational deformity of the femur greater than 10° provokes an abnormal loading of the patellofemoral joint, potentially leading to AKP.36 However, although lower extremity rotational deformities increase the risk of AKP and represent a predisposing factor, they are not sufficient to cause AKP on their own.13
A growing body of literature links the hip with AKP.11,22,32 An interesting and novel link has been found between cam femoroacetabular impingement (FAI) and AKP.31 Cam FAI patients develop an avoidance behavior consisting of functional external femoral rotation to prevent the impingement and associated hip pain.31 This femoral rotation could provoke a patellofemoral imbalance that could theoretically lead to patellofemoral pain. These patients tend to go to a clinician because of AKP that is recalcitrant to conservative treatment. However, the patient often discontinues physical therapy because he or she does not get the expected results. After some time, the patient experiences disabling hip pain. In such a patient, knee pain and disability resolve once FAI is addressed and treated.31 Therefore, assessment of cam FAI should be a part of the physical examination of patients with AKP, especially in patients with pain that persists after conservative treatment. Once a causal relationship is established between cam FAI and AKP, cam surgery is recommended.
Psychological Factors Approach: They are only Pain Modulators, Not the Cause of Pain
As previously noted, most AKP patients have chronic pain. Chronic pain is a multidimensional experience. Therefore, consideration is needed not only for sensory features but also affective and cognitive features.
One of the myths about AKP patients is that they have “peculiar” psychological traits underlying the genesis of pain.5,6,25 Very often, AKP patients have severe pain and disability with insignificant clinical and radiological findings; many have allodynia or hyperalgesia. Furthermore, they have a high incidence of anxiety, depression, kinesiophobia (a fear that movement will cause further injury or reinjury and additional pain) and catastrophizing ideas (expectation that the pain will worsen and no recourse exists for controlling it).5,6 The clinician may therefore conclude that a patient’s main problem is psychological, but that is not necessarily true. The severe pain that these patients experience causes the psychological factors, not vice versa.5,6 Psychological factors can, however, modulate pain. For example, catastrophizing leads to chronification of pain due to neurophysiological processes.27 Furthermore, even in patients with clear structural findings, psychological factors influence and modify pain sensation as well as subsequent impairment and can therefore hinder recovery.27
Clinical improvement in pain after treatment has been associated with reduced catastrophizing and kinesiophobia.5 This finding is clinically relevant because it contradicts the belief that patients with AKP have preexisting psychological problems that are responsible for pain. However, psychological factors might fuel unexplained pain and reduced function that persist after appropriate treatment.
AKP patients also have some degree of disability that is not directly related to the degree of pain, but can worsen if fear-avoidance patterns to reduce pain appear. The correlation between pain and disability is only moderate in AKP patients.6 Psychological factors have been observed to influence the degree of disability that AKP patients have.6
Among the psychological factors, the most relevant from a clinical standpoint is catastrophization, which is related to the pain as well as the disability of AKP patients.27 Therefore, the first time a patient with AKP is seen in the clinic, an assessment based on the “pain catastrophizing scale” can be routinely performed.33 Given the importance that catastrophization has as a barrier to recovery from pain and disability in AKP patients, it should be included in the therapeutic targets to enable complementary treatment that may bolster conventional treatments (physical therapy, surgery, or both). The rationale behind this approach is illustrated by the efficacy of cognitive behavioral interventions for reducing pain catastrophizing in patients being treated for arthritis.4 Moreover, similar results have been observed between lumbar fusion and cognitive behavioral interventions in patients with lumbar pain.2
Along with the patients’ beliefs and cognitions about pain, clinicians must not forget that the physicians treating those patients also have beliefs and cognitions.25 Therefore, a physician could potentially influence the course of the illness, in either a positive or a negative way, by reinforcing or modifying the patient’s beliefs and cognitions about pain.
AKP in a Patient with a Previous Surgery of the Extensor Mechanism of the Knee: Iatrogenic Medial Patellar Instability and the Failed Medial Patellofemoral Ligament Surgery
Iatrogenic medial patellar instability (IMPI) is an often severe, postsurgical objective condition with its own characteristics. In most of these cases, it appears after realignment surgery and frequently causes incapacitating chronic and disabling AKP along with serious psychological problems.28 In a comparison of IMPI patients with a previous series of more typical AKP patients, the former have higher rates of kinesiophobia (100% vs 80%), catastrophizing (41% vs 37%), anxiety (59% vs 37%), and depression (24% vs 11%).26
“Extensive” or overrelease of the lateral retinaculum is clearly a major cause of IMPI.26 Overrelease can be a result of excessive severance of the lateral retinaculum with transection of the vastus lateralis tendon. It may also arise from release of a lateral retinaculum in the context of trochlear dysplasia, patella alta, or hyperelasticity, or the lateral retinaculum may have already been lax, which suggests poor patient selection. This iatrogenic condition should no longer exist and could almost be eliminated by avoiding overrelease of the lateral retinaculum, only releasing a tight lateral retinaculum, and focusing on normalizing the abnormal anatomy.26
All too often, the pain and disability from IMPI is much worse than the preoperative symptoms that the surgery was intended to resolve. The diagnosis can be established by physical examination (a positive Fulkerson relocation test),14 simple therapeutic tests (significant relief from their pain with a “reverse” McConnell taping),26 and confirmed by imaging techniques (stress radiography and stress axial computed tomography scans).26 Reconstruction of the deep transverse layer of the lateral retinaculum using a central strip of the iliotibial band can successfully treat these severely disabled patients.28
AKP is also common after medial patellofemoral ligament reconstruction. Any deviation from anatomic placement of the femoral attachment point caries the risk of producing abnormal/harmful patellofemoral contact pressures, leading to painful patellofemoral osteoarthritis.24,29 In these patients, the resection of the previous graft and a new reconstruction of the medial patellofemoral ligament using an anatomic femoral attachment is required.
Conclusion
The etiology of AKP is multifactorial, and therefore several subpopulations of AKP patients exist and their treatment must be personalized. Normally, the focus is on the knee of a patient with AKP, and only that joint is examined. However, that focus can lead to overlooking other important etiological factors that may be present. Both pelvifemoral dysfunction and psychological factors can modulate the disorder and must be considered as therapeutic targets within the context of AKP treatment. Patients who initially present with AKP often respond well to load restriction to a point within their envelope of function and a pain-free rehabilitation program. Only rarely should consideration be given to arthroscopic patellar denervation or surgical techniques to unload areas that could be the source of pain, such as the distal pole of the patella.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42:A1-A54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD. Surgery for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline. Spine. 2009;34:1094-1109. [DOI] [PubMed] [Google Scholar]
- 3. Cibulka MT, Threlkeld-Watkins J. Patellofemoral pain and asymmetrical hip rotation. Phys Ther. 2005;85:1201-1207. [PubMed] [Google Scholar]
- 4. Dixon KE, Keefe FJ, Scipio CD, Perri LM, Abernethy AP. Psychological interventions for arthritis pain management in adults: a meta-analysis. Health Psychol. 2007;26:241-250. [DOI] [PubMed] [Google Scholar]
- 5. Domenech J, Sanchis-Alfonso V, Espejo B. Changes in catastrophizing and kinesiophobia are predictive of changes in disability and pain after treatment in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2014;22:2295-2300. [DOI] [PubMed] [Google Scholar]
- 6. Domenech J, Sanchis-Alfonso V, Lopez L, Espejo B. Influence of kinesiophobia and catastrophizing on pain and disability in anterior knee pain patients. Knee Surg Sports Traumatol Arthrosc. 2013;21:1562-1568. [DOI] [PubMed] [Google Scholar]
- 7. Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports Med. 2012;42:51-67. [DOI] [PubMed] [Google Scholar]
- 8. Dye SF. The knee as a biologic transmission with an envelope of function: a theory. Clin Orthop Relat Res. 1996;325:10-18. [DOI] [PubMed] [Google Scholar]
- 9. Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;436:100-110. [DOI] [PubMed] [Google Scholar]
- 10. Dye SF, Vaupel GL, Dye CC. Conscious neurosensory mapping of the internal structures of the human knee without intraarticular anesthesia. Am J Sports Med. 1998;26:773-777. [DOI] [PubMed] [Google Scholar]
- 11. Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39:154-163. [DOI] [PubMed] [Google Scholar]
- 12. Elson DW, Jones S, Caplan N, St Clair Gibson A, Stewart S, Kader DF. Clinically insignificant association between anterior knee pain and patellofemoral lesions which are found incidentally. Knee. 2013;20:471-475. [DOI] [PubMed] [Google Scholar]
- 13. Erkocak OF, Altan E, Altintas M, Turkmen F, Aydin BK, Bayar A. Lower extremity rotational deformities and patellofemoral alignment parameters in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2016;24:3011-3020. [DOI] [PubMed] [Google Scholar]
- 14. Fulkerson JP. A clinical test for medial patella tracking. Tech Orthop. 1997;12:165-169. [Google Scholar]
- 15. Fulkerson JP. Why does distal patella articular softening happen? Orthop Today Eur. 2015;18:53-56. [Google Scholar]
- 16. Gidal BE. New and emerging treatment options for neuropathic pain. Am J Manag Care. 2006;12(9 suppl):S269-S278. [PubMed] [Google Scholar]
- 17. Johnson LL, van Dyk GE, Green JR, 3rd, et al. Clinical assessment of asymptomatic knees: comparison of men and women. Arthroscopy. 1998;14:347-359. [DOI] [PubMed] [Google Scholar]
- 18. Karaman O, Ayhan E, Kesmezacar H, Seker A, Unlu MC, Aydingoz O. Rotational malalignment after closed intramedullary nailing of femoral shaft fractures and its influence on daily life. Eur J Orthop Surg Traumatol. 2014;24:1243-1247. [DOI] [PubMed] [Google Scholar]
- 19. Khayambashi K, Mohammadkhani Z, Ghaznavi K, Lyle MA, Powers CM. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2012;42:22-29. [DOI] [PubMed] [Google Scholar]
- 20. Maier D, Bornebusch L, Salzmann GM, Südkamp NP, Ogon P. Mid- and long-term efficacy of the arthroscopic patellar release for treatment of patellar tendinopathy unresponsive to nonoperative management. Arthroscopy. 2013;29:1338-1345. [DOI] [PubMed] [Google Scholar]
- 21. Miltner O, Siebert CH, Schneider U, Niethard FU, Graf J. Patellar hypertension syndrome in adolescence: a three-year follow up. Arch Orthop Trauma Surg. 2003;123:455-459. [DOI] [PubMed] [Google Scholar]
- 22. Nakagawa TH, Serrão FV, Maciel CD, Powers CM. Hip and knee kinematics are associated with pain and self-reported functional status in males and females with patellofemoral pain. Int J Sports Med. 2013;34:997-1002. [DOI] [PubMed] [Google Scholar]
- 23. Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639-646. [DOI] [PubMed] [Google Scholar]
- 24. Sanchis-Alfonso V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg. 2014;22:175-182. [DOI] [PubMed] [Google Scholar]
- 25. Sanchis-Alfonso V. Holistic approach to understanding anterior knee pain. Clinical implications. Knee Surg Sports Traumatol Arthrosc. 2014;22:2275-2285. [DOI] [PubMed] [Google Scholar]
- 26. Sanchis-Alfonso V, Merchant AC. Iatrogenic medial patellar instability—an avoidable injury. Arthroscopy. 2015;31:1628-1632. [DOI] [PubMed] [Google Scholar]
- 27. Sanchis-Alfonso V, Montesinos-Berry E, Domenech J. Catastrophic thinking is a new puzzle piece in understanding anterior knee pain. Orthop Today Eur. 2014;17:44-50. [Google Scholar]
- 28. Sanchis-Alfonso V, Montesinos-Berry E, Monllau JC, Merchant AC. Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy. 2015;31:422-427. [DOI] [PubMed] [Google Scholar]
- 29. Sanchis-Alfonso V, Ramirez-Fuentes C, Montesinos-Berry E, Domenech J, Martí-Bonmatí L. Femoral insertion site of the graft used to replace the medial patellofemoral ligament influences the ligament dynamic changes during knee flexion and the clinical outcome [published online December 12, 2015]. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-015-3905-0. [DOI] [PubMed] [Google Scholar]
- 30. Sanchis-Alfonso V, Roselló-Sastre E, Monteagudo-Castro C, Esquerdo J. Quantitative analysis of nerve changes in the lateral retinaculum in patients with isolated symptomatic patellofemoral malalignment. A preliminary study. Am J Sports Med. 1998;26:703-709. [DOI] [PubMed] [Google Scholar]
- 31. Sanchis-Alfonso V, Tey M, Monllau JC. A novel association between femoroacetabular impingement and anterior knee pain. Pain Res Treat. 2015;2015:937431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39:12-19. [DOI] [PubMed] [Google Scholar]
- 33. Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524-532. [Google Scholar]
- 34. Teitge RA. Patellofemoral syndrome a paradigm for current surgical strategies. Orthop Clin North Am. 2008;39:287-311. [DOI] [PubMed] [Google Scholar]
- 35. Wolf CJ. Pain: moving from symptom control toward mechanism-specific pharmacologic management. Ann Intern Med. 2004;140:441-451. [DOI] [PubMed] [Google Scholar]
- 36. Yildirim AO, Aksahin E, Sakman B. The effect of rotational deformation patellofemoral parameters following the treatment of femoral shaft fracture. Arch Orthop Trauma Surg. 2013;133:641-648. [DOI] [PubMed] [Google Scholar]


