Abstract
Context:
The medial head of the gastrocnemius is the third most commonly strained muscle in elite athletes after the biceps femoris and rectus femoris. The differential diagnosis of posterior calf injury includes musculoskeletal and nonmusculoskeletal causes. Classically, delineation of these injuries from one another relied primarily on historical features and physical examination findings. The utilization of musculoskeletal ultrasound (sonography) has augmented the diagnosis of these injuries by providing dynamic, real-time confirmation.
Evidence Acquisition:
A review of PubMed, OVID, and MD Consult prior to January 2016 was performed using search terms, including soleus ultrasound, gastrocnemius ultrasound, and tennis leg. The references of the pertinent articles were further reviewed for other relevant sources.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
There have been few reviews to date of calf injuries and the use of sonography in their diagnosis. Prompt diagnosis utilizing ultrasound allows the clinician to focus management on gastrocnemius injury if present. Two-thirds of calf injuries occur at the junction of the fascia between the medial head of the gastrocnemius and the soleus. Injuries to the lateral head of the gastrocnemius occur in up to 14% of patients in some case series, but injury may occur anywhere from the proximal origin to the mid-belly to the fascial junction with the soleus. Numerous injuries to the posterior compartment can mimic gastrocnemius strain, and musculoskeletal ultrasound can aide in their diagnosis by incorporating real-time imaging into the grading of the injury and visual confirmation of physical examination findings.
Conclusion:
Acute injury to the posterior compartment of the lower extremity can represent a diagnostic challenge. Medial gastrocnemius strain represents the most common injury of the posterior compartment of the lower extremity. Ultrasound is a useful tool to assist the clinician in determining the specific cause of calf injury, estimate the severity of the injury, and monitor progress of healing. The vast majority of calf injuries can be diagnosed and managed without any additional imaging. Serial diagnostic ultrasound of an injured area allows for direct monitoring of tissue healing and may allow the clinician to more confidently assess response to treatment and help guide return-to-play decisions.
Keywords: ultrasound, sonography, gastrocnemius, calf, lower leg
Partial rupture of the medial head of the gastrocnemius at the aponeurosis of the soleus muscle was first described as “tennis leg” in 1883.2,17,22 While frequent among tennis athletes, the injury occurs in multiple sports and from a variety of activities, even namaz prayer.27 Originally, physicians thought most injuries were related to isolated plantaris rupture until intact plantaris muscle with isolated tearing of the medial head of the gastrocnemius was noted during operative exploration.16 Subsequent improvements in diagnostic imaging demonstrate that a variety of pathological entities mimic medial gastrocnemius injury.
Ultrasound offers particular value as an inexpensive means to evaluate muscular calf injuries, and improvements in the technical capability of diagnostic musculoskeletal ultrasound has allowed for better visualization of the soft tissue structures. The use of ultrasound to diagnose tennis leg was first described in a case report,5 and subsequently, a case series of 141 patients and 4 cadavers with suspected calf injury revealed injuries to the medial gastrocnemius (n = 94, 66.7%), fascial separation between the medial head of the gastrocnemius and soleus with swelling (n = 30, 21.3%), partial rupture of the soleus (n = 1, 0.7%), and complete rupture of the plantaris (n = 2, 1.4%).8
Methods
Three separate searches were conducted using PubMed, Ovid, and MD Consult using the terms soleus ultrasound, gastrocnemius ultrasound, and tennis leg on January 3, 2016. PubMed results were limited to human subjects, English language, results within the MEDLINE database, and only articles with an abstract available. Titles and abstracts were reviewed individually, and if an abstract discussed sonographic imaging of injuries of the lower extremity in human subjects, tennis leg, or injuries to the lower leg, then the complete article was downloaded and reviewed.
Cases and their respective sonographic images discussed in this article were obtained using a GE LOGIQe with a frequency set from 10 to 12 MHz for the duration of the scan (protocol in Appendix 1, images in Appendix 2, available at http://journals.sagepub.com/doi/suppl/10.1177/1941738117696019).
Results
The PubMed database revealed the following results: 4327 results for “soleus ultrasound,” 4380 results for “gastrocnemius ultrasound,” and 78 results for “tennis leg.” During the OVID review, 11,302 results were discovered for “soleus ultrasound,” 11,616 results for “gastrocnemius ultrasound,” and 7697 results for “tennis leg.” MD Consult revealed 231 results for “soleus ultrasound,” 535 results for “gastrocnemius ultrasound,” and 311 results for “tennis leg.”
Discussion
The anatomy and interplay of the Achilles tendon and musculature of the posterior calf (Figure 1) can represent a diagnostic challenge when an injury occurs. For simplicity’s sake, many clinicians use the term “tennis leg” to refer to all muscle injuries in the superficial calf not involving the Achilles. The reservation of the term “tennis leg” for such an injury arises from the injury’s typical mechanism: sudden push-off when initiating a sprint or jump, thus causing the ankle to rapidly change from plantar flexion to dorsiflexion with the knee remaining in full extension or hyperextension.21 Muscle strains of the gastrocnemius most often occur in poorly conditioned male athletes in the fourth to sixth decades of life7,13,19,21 but also in conditioned athletes during sudden, ballistic movement of the lower extremity.
Figure 1.
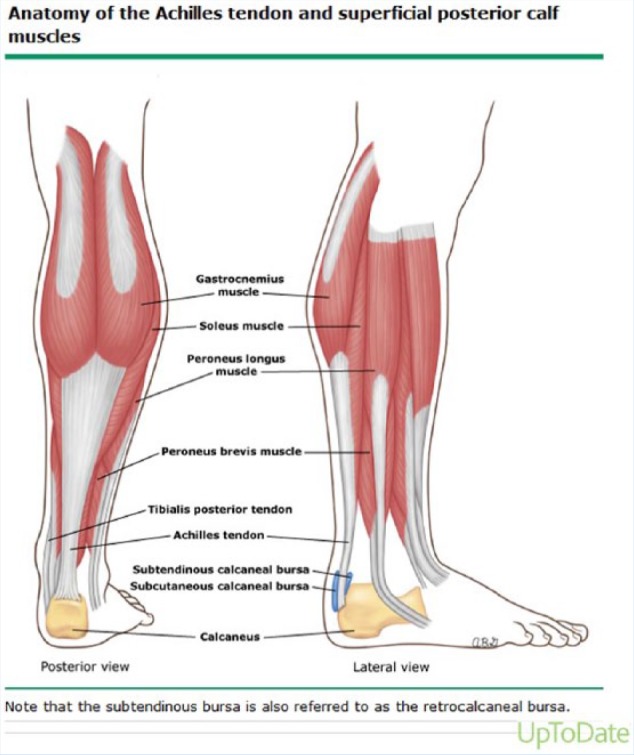
Anatomy of the Achilles tendon and superficial posterior calf muscles. Reproduced with permission from Fields KB. Evaluation and diagnosis of common causes of foot pain in adults. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. Accessed on 03 February 2016. Copyright © 2016 UpToDate, Inc.11
A case series reviewing calf injuries with ultrasound revealed that approximately two-thirds of these injuries occur at the junction of the fascia between the medial head of the gastrocnemius and the soleus.8 As an example, a well-conditioned female recently presented for evaluation after being injured during a jazzercise class. Focal hypoechoic change was noted at the insertion of the medial head of the gastrocnemius into the fascia (see Figure 1 in Appendix 2) in the distal fibers of the muscle. A focal hypoechoic change likely representing blood was located between the fascia and the muscular fibers of the medial head of the left gastrocnemius along the proximal and mid-portion of the muscle (see Figure 2 in Appendix 2). Increased Doppler flow was present throughout the hypoechoic regions as well. Comparison of the patient’s right (unaffected) and left (injured) medial gastrocnemius at similar positions demonstrated appreciable differences in their sonographic appearance (see Figure 3 in Appendix 2).
The case above demonstrates a classic injury occurring at the junction of the medial head of the gastrocnemius with the fascia. However, injury to the lateral head of the gastrocnemius occurs in up to 14% of some case series (see Figures 4 and 7 in Appendix 2).26 Case series also document that injury to the gastrocnemius can range from the proximal gastrocnemius origin (Figure 4 in Appendix 2) to the mid-belly to the aponeurosis of the 2 heads or the fascial junction with the soleus (see Figure 5 in Appendix 2). Injuries can be isolated to the gastrocnemius or to the soleus or involve both muscles.
Numerous injuries to the posterior compartment can mimic gastrocnemius strain and should be included in the differential diagnosis, including Achilles tendon rupture, popliteal artery entrapment, soleus syndrome, acute compartment syndrome, chronic exertional compartment syndrome, plantaris injury, and injuries to the structures of the deep compartment (tibialis posterior, flexor digitorum longus, and flexor hallicus longus). There have been documented cases of a symptomatic flexor hallicus longus,1 a symptomatic accessory flexor digitorum longus,1,3,14,23 and a symptomatic accessory soleus.1,10 Deep vein thrombosis (DVT) is both a differential diagnosis and a complication of this condition, and assessment of the calf veins at the time of the scan is standard.20 If there is strong suspicion for DVT based on the clinician’s sonographic findings or clinical history, a formal bilateral lower extremity ultrasound with Doppler should be considered to evaluate for DVT. Severe gastrocnemius strains may be mistaken for DVT or thrombophlebitis, leading to treatment with anticoagulants, which can increase bleeding in the torn gastrocnemius muscle as well as subject patients to complications from anticoagulation treatment.4
Delineating soleus from gastrocnemius injury can be clinically challenging. Their respective mechanisms are slightly different as the soleus strain results from passive dorsiflexion of the ankle while the knee is flexed7—a mechanism commonly encountered when running uphill. While gastrocnemius strain is often acute, soleus strain is usually an overuse injury that develops primarily in distance runners who may be training at a mileage level too great for their level of fitness.9,12 Pain is elicited by placing maximal stretch on the injured soleus muscle through simultaneous dorsiflexion of the ankle and flexion of the knee; in severe cases, this will be painful when performed passively as well.
Plantaris rupture may mimic gastrocnemius strain. The plantaris tendon, if present, can be seen deep to the gastrocnemius muscle (Figure 2). The plantaris crosses midline posterior to the knee joint from its origin at the lateral supracondylar ridge and then continues to move medially between the muscle bellies of the medial head of the gastrocnemius and soleus muscles before inserting onto the medial aspect of the Achilles tendon, 5 to 10 cm above the calcaneus. The plantaris tendon, which classically ruptures at the proximal muscle belly, has also been known to rupture in an acute isolated manner at the mid-plantaris tendon.15 Symptoms are often less severe, and the location of focal tenderness is in the mid-Achilles region rather than the proximal calf.15,25 Whereas pain is typically a major limitation in movement after gastrocnemius strain, patients with isolated plantaris injury will have full active range of motion without major strength loss or symptom provocation. Ultrasound can confirm the diagnosis, although the plantaris can be difficult to identify in some patients given its small size.24 Magnetic resonance imaging can be used to make a definitive diagnosis. Figure 6 in Appendix 2 displays a hyperechoic area of probable calcification surrounded by hypoechoic change within the medial aspect of the Achilles, 7 cm superior to the calcaneus, representing a ruptured and retracted plantaris tendon.
Figure 2.

Deep muscles of the posterior compartment, highlighting the plantaris muscle’s origin, course, and insertion. Gastrocnemius, soleus, and Achilles tendon are removed in this view.
The value of sonography extends beyond narrowing the initial differential and confirming the diagnosis.6,18 Sonography can be an excellent tool for assessing response to therapy by correlating clinical findings with recovery. Various stages of healing can be imaged after injury. Figure 7 in Appendix 2 demonstrates sonographic findings of an acute-on-chronic injury. Figure 8 in Appendix 2 demonstrates a notable injury to the medial head of the gastrocnemius; on 2-week follow-up examination, the patient’s repeat ultrasound was consistent with early scar formation (see Figure 9 in Appendix 2) and decreased edema as well as resolving hypoechoic defects in longitudinal views from 2 weeks earlier. Sonography can confirm complete discontinuity of the muscle with extensive edema and hemorrhage, such as the injury demonstrated in Figure 10 in Appendix 2. This type of injury mandates a more conservative approach and usually a period of nonweightbearing. Conversely, injuries that resolve quickly, such as those demonstrated in Figures 8 and 9 in Appendix 2, may progress more rapidly with rehabilitation and return to play.
Conclusion
Acute injury to the posterior compartment of the lower extremity can represent a diagnostic challenge. Medial gastrocnemius strain represents the most common injury of the posterior compartment of the lower extremity. Prompt diagnosis utilizing ultrasound allows the clinician to focus management on gastrocnemius injury. A clear diagnostic finding on scanning often helps in the decision not to do additional testing for DVT. Experienced clinicians with ultrasound can assess whether the deep venous system has flow and compressibility and thus appears patent. Musculoskeletal ultrasound allows the incorporation of real-time imaging into the grading of injury and visual confirmation of physical examination findings and patient symptoms.6,18 Ultrasound proves a useful tool to assist the clinician in assessing the specific cause of calf injury, estimating the severity of the injury, monitoring progress of healing, and managing the vast majority of these injuries without additional imaging. Monitoring tissue healing with serial ultrasound imaging may allow the physician to more confidently assess the response of injury to treatment and to decide the timing of return to play of these athletes.
Supplementary Material
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article. The views expressed in this paper are those of the authors and do not necessarily reflect those of the United States Army or any other section of the Department of Defense.
References
- 1. Al-Himdani S, Talbot C, Kurdy N, Pillai A. Accessory muscles around the foot and ankle presenting as chronic undiagnosed pain. An illustrative case report and review of the literature. Foot (Ednib). 2013;23:154-161. [DOI] [PubMed] [Google Scholar]
- 2. Arner O, Lindholm A. What is tennis leg. Acta Chir Scand. 1958;116:73-75. [PubMed] [Google Scholar]
- 3. Athavale SA, Geetha GN, Swathi Morphology of flexor digitorum accessorius muscle. Surg Radiol Anat. 2012;34:367-372. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM. Traumatic disorders. In: Canale ST, Beaty JH, eds. Campbell’s Operative Orthopaedics. Philadelphia, PA: Mosby; 2008:233-234. [Google Scholar]
- 5. Bianchi S, Martolini C, Abdelwahab IF, Derchi LE, Damiani S. Sonographic evaluation of tears of the gastrocnemius medial head (“tennis leg”). J Ultrasound Med. 1998;17:157-162. [DOI] [PubMed] [Google Scholar]
- 6. Botter LA, Oliveira RO, Suenaga E, et al. Differential diagnosis of calf pain by ultrasonography. Einstein. 2008;6:229-233. [Google Scholar]
- 7. Campbell JT. Posterior calf injury. Foot Ankle Clin. 2009;14:761-771. [DOI] [PubMed] [Google Scholar]
- 8. Delgado GJ, Chung CB, Lektrakul N, et al. Tennis leg: clinical US study of 141 patients and anatomic investigation of four cadavers with MR imaging and US. Radiology. 2002;224:112-119. [DOI] [PubMed] [Google Scholar]
- 9. Dixon JB. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Curr Rev Musculoskelet Med. 2009;2:74-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Doda N, Peh WC, Chawla A. Symptomatic accessory soleus muscle: diagnosis and follow-up on magnetic resonance imaging. Br J Radiol. 2006;79:e129-e132. [DOI] [PubMed] [Google Scholar]
- 11. Fields KB. Evaluation and diagnosis of common causes of foot pain in adults. http://www.uptodate.com/home. Accessed February 3, 2016.
- 12. Fields KB. Running injuries—changing trends and demographics. Curr Sports Med Rep. 2011;10:299-303. [DOI] [PubMed] [Google Scholar]
- 13. Gallo RA, Plakke M, Silvis ML. Common leg injuries of long-distance runners: anatomical and biomechanical approach. Sports Health. 2012;4:485-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gupta R, Brijendra S. Flexor digitorum longus muscle—an unusual presentation; anatomy and clinical significance, a case report. J Dent Med Sci. 2013;5:1-3. [Google Scholar]
- 15. Harmon KJ, Reeder MT, Udermann BE, Murray SR. Isolated rupture of the plantaris tendon in a high school track athlete. Clin J Sport Med. 2006;16:361-363. [DOI] [PubMed] [Google Scholar]
- 16. Harvey FJ, George C, Harvey PM. Surgical availability of the plantaris tendon. J Hand Surg Am. 1983;8:243-247. [DOI] [PubMed] [Google Scholar]
- 17. Hood WP. On lawn tennis leg. Lancet. 1883;2:728-729. [Google Scholar]
- 18. Kane D, Balint PV, Gibney R, Bresnihan B, Sturrock RD. Differential diagnosis of calf pain with musculoskeletal ultrasound imaging. Ann Rheum Dis. 2004;63:11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kwak HS, Lee KB, Han YM. Ruptures of the medial head of the gastrocnemius (“tennis leg”): clinical outcome and compression effect. Clin Imaging. 2006;30:48-53. [DOI] [PubMed] [Google Scholar]
- 20. Lee JC, Mitchell AW, Healy JC. Imaging of muscle injury in the elite athlete. Br J Radiol. 2012;85:1173-1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Millar AP. Strains of the posterior calf musculature (“tennis leg”). Am J Sport Med. 1979;7:172-174. [DOI] [PubMed] [Google Scholar]
- 22. Powel RM. Lawn tennis leg. Lancet. 1883;2:44. [Google Scholar]
- 23. Saar WE, Bell J. Accessory flexor digitorum longus presenting as tarsal tunnel syndrome: a case report. Foot Ankle Spec. 2011;4:379-382. [DOI] [PubMed] [Google Scholar]
- 24. Simpson SL, Michael SH, Roberto HB. The plantaris tendon graft: an ultrasound study. J Hand Surg Am. 1991;16:708-711. [DOI] [PubMed] [Google Scholar]
- 25. Walden M, Hagglund M, Ekstrand J. UEFA Champions League study: a prospective study of injuries in professional football during the 2001-2002 season. Br J Sports Med. 2005;39:542-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Weishaupt D, Schweitzer ME, Morrison WBJ. Injuries to the distal gastrocnemius muscle: MR findings. Comput Assist Tomogr. 2001;25:677-682. [DOI] [PubMed] [Google Scholar]
- 27. Yilmaz C, Orgenc Y, Ergenc R, Erkan N. Rupture of the medial gastrocnemius muscle during namaz praying: an unusual cause of tennis leg. Comput Med Imaging Graph. 2008;32:728-731. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


