Abstract
Context:
Diabetes mellitus (DM) has become an epidemic in the United States and is associated with increased risk of multiple comorbidities, including painful musculoskeletal conditions. A common treatment for many of these painful musculoskeletal conditions is local soft tissue and intra-articular corticosteroid injection (CSI). These local injections have the potential to cause elevated blood glucose levels (BGLs) and cause complications in patients with DM. Therefore, it was the objective of this investigation to review the currently available evidence that directly addresses the effects of local CSIs used for painful musculoskeletal conditions on BGL in patients with DM.
Evidence Acquisition:
PubMed, Google Scholar, EMBASE, CINAHL, and Cochrane Review databases were searched with a combination of the terms corticosteroid, glucocorticoid, steroid, injection, musculoskeletal, and diabetes. Search limits included the English language. Bibliographic references from these articles were also examined to identify pertinent literature.
Study Design:
Clinical review.
Level of Evidence:
Level 3.
Results:
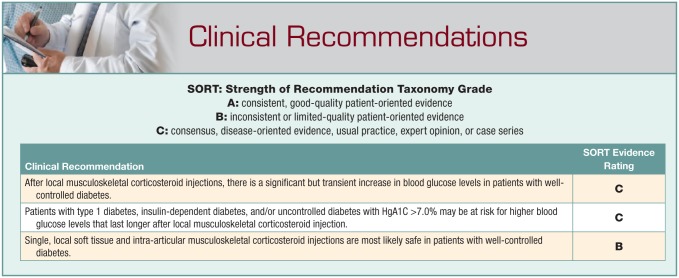
Ten studies that met the inclusion criteria were reviewed. All these studies showed significant but transient increases in postinjection BGL after a single local CSI in patients with DM. There were no adverse reactions or complications reported.
Conclusion:
Single, local soft tissue and intra-articular musculoskeletal CSIs are most likely safe in patients with well-controlled DM.
Keywords: steroid injection, diabetes, glucose, intra-articular, soft tissue
Diabetes mellitus (DM) has become an epidemic in the United States and affects almost 10% of the population, or approximately 30 million Americans. Its incidence is on the rise, with 1.4 million Americans newly diagnosed with diabetes every year.3 Current high-quality evidence has established that regular physical activity can either prevent or delay the development of type 2 diabetes (T2DM) along with many if its associated conditions, thus improving quality of life, morbidity, and mortality in these patients.8 Unfortunately, diabetes is positively associated with many painful musculoskeletal disorders of both the axial skeleton and limbs, including trigger finger, adhesive capsulitis of the shoulder, carpal tunnel syndrome, and osteoarthritis.5,14,17 These painful conditions can be disabling and may impede the ability of these patients to be able to participate in regular physical activity.
Local corticosteroid injections (CSIs) are often used as one of the first-line treatments in the conservative management of many painful musculoskeletal conditions of the soft tissues and joints such as bursitis, tendinopathy, and osteoarthritis because of their ease of delivery, low cost, and relatively low risk to the patient. These local injections are aimed at relieving pain, reducing inflammation, and improving mobility. While data are mixed on long-term outcomes for locally administered CSI, it is clear that some patients receive short-term benefit from these injections, and in some cases, these injections may prolong or even obviate the need for surgery.6,16,21
It has been well established that systemic corticosteroids effect blood glucose levels (BGLs), especially in those patients with altered glucose metabolism; however, there is little information on the systemic effects of local CSI on blood glucose control in patients with DM. To date, there have been several small-scale prospective studies but no large-scale randomized controlled trials examining the effects of locally administered CSI on BGL. In addition, the American Academy of Orthopedic Surgeons,1 American College of Sports Medicine,2 American Diabetes Association,3 and American Medical Society for Sports Medicine4 make no recommendations regarding steroid injections in patients with DM. Understanding the possible side effects of locally administered CSIs in patients with DM is important for both clinicians and patients to know to develop the most appropriate treatment plan as well as provide counseling on postinjection care. Therefore, it was the objective of this investigation to review the currently available evidence that directly addresses the effects of local soft tissue and intra-articular CSIs used for musculoskeletal conditions on BGL in patients with DM.
Methods
A literature search of PubMed, Google Scholar, EMBASE, CINAHL, and Cochrane Review databases was conducted with a combination of the search terms corticosteroid, glucocorticoid, steroid, injection, musculoskeletal, and diabetes. The search was limited to the English language. All prospective and retrospective studies examining the effect of local soft tissue or intra-articular steroid injections on BGL in patients with DM were eligible for inclusion. Bibliographic references from these articles were also examined to identify pertinent literature. Studies evaluating epidural steroid injections were excluded from this review. Single case reports and review articles were also excluded. A total of 11 prospective studies examining the effects of local musculoskeletal corticosteroid injections on glucose levels in patients with DM were found.
Results
Ten studies that met inclusion criteria were reviewed (see Supplemental Table 1 in the Appendix, available in the online version of this article). Study populations were small, ranging from 6 to 40 participants. Five studies included only patients with T2DM,9-12,15 3 studies included patients with T1 and T2DM,13,18,20 and 2 studies did not specify DM type.7,19 Patients without DM were included in only 2 studies.15,19
While most patients in these studies received intra-articular injections of the knee, shoulder, wrist, and ankle, 4 studies included extra-articular soft tissue injections of the finger and wrist.7,13,18,20 These 4 studies report similar BGL after local CSI as the studies that evaluated BGL after CSI of the larger knee and shoulder joints. The majority of patients included in all of the studies had well-controlled DM, with mean HgA1C ≤7.0% in all but 2 studies.9,18 None of the study protocols changed usual regimens for diabetes care (ie, diet, physical activity, or medication) during the study period.
All 10 studies reviewed showed significant but transient increases in postinjection BGL with peak individual blood sugars as high as 518 mg/dL. Mean blood sugar elevations reported ranged from 125 to 320 mg/dL. Most studies found time to peak postinjection BGL occurred within 1 to 5 days, and BGL returned to baseline in less than 24 hours up to 10 days. Study protocols varied in how patients were asked to monitor BGL, including timing and method of monitoring. None of the studies specifically reported postprandial BGL.
Patients with T1DM or insulin-dependent diabetes (IDDM) had higher postinjection BGL than those with T2DM not requiring insulin in 2 studies.18,20 In another study, patients with HgA1C >7.0% had BGLs that were higher and lasted longer than those with lower HgA1C levels.13 Two studies included a comparison between patients with and without DM and found that patients with DM had a greater absolute increase in BGLs.15,18 While 1 of these studies found that patients with DM had a longer time to return to baseline BGL,15 the other study found that all patients had returned to baseline BGL by 24 hours.18
While none of the studies specifically evaluated adverse reactions or complications from elevated BGL, no adverse events were reported in any of these studies. However, given that significant mean blood sugar elevations ranged from 125 to 320 mg/dL, there is the potential for complications to occur, especially in patients with uncontrolled diabetes (ie, BGL >250 mg/dL).
Conclusion
Based on current evidence, there is a significant but transient increase (mean, 125-320 mg/dL) in BGL after a single CSI in patients with well- or near well-controlled DM. The increases in BGL were short-lived, and there were no serious adverse events reported in any of these studies. Patients with IDDM, T1DM, and/or uncontrolled DM with HgA1C >7.0% may be at increased risk for higher BGLs that last longer.
Single, local soft tissue and intra-articular CSIs are most likely safe in patients with well-controlled DM. Patients with DM need to be advised of the risk of elevated BGLs after CSI and the need for close monitoring of BGLs postinjection prior to intervention. However, this risk needs to be balanced with possible benefits of the injection, including relief of pain, increased ability to perform physical activity with decreased risk of complications from DM, and improved quality of life, as well as possible avoidance of surgery.
Supplementary Material
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1.American Academy of Orthopedic Surgeons. Clinical practice guidelines. http://www.aaos.org/guidelines/. Accessed September 3, 2016.
- 2.American College of Sports Medicine. Position stands. http://acsm.org/public-information/position-stands. Accessed September 3, 2106.
- 3.American Diabetes Association. Standards of care. http://professional.diabetes.org/content/clinical-practice-recommendations/. Accessed September 3, 2016.
- 4.American Medical Society for Sports Medicine. AMSSM publications and position statements. http://www.amssm.org/Publications.html. Accessed September 3, 2106.
- 5. Arkkila PE, Gautier JF. Musculoskeletal disorders in diabetes mellitus: an update. Best Pract Res Clin Rheumatol. 2003;17:945-970. [DOI] [PubMed] [Google Scholar]
- 6. Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;(2):CD005328. [DOI] [PubMed] [Google Scholar]
- 7. Catalano LW, 3rd, Glickel SZ, Barron OA, Harrison R, Marshall A, Purcelli-Lafer M. Effect of local corticosteroid injection of the hand and wrist on blood glucose in patients with diabetes mellitus. Orthopedics. 2012;35:e1754-e1758. [DOI] [PubMed] [Google Scholar]
- 8. Colberg SR, Albright AL, Blissmer BJ, et al. Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: joint position statement. Med Sci Sports Exerc. 2010;42:2282-2303. [DOI] [PubMed] [Google Scholar]
- 9. Habib GS, Abu-Ahmad R. Lack of effect of corticosteroid injection at the shoulder joint on blood glucose levels in diabetic patients. Clin Rheumatol. 2007;26:566-568. [DOI] [PubMed] [Google Scholar]
- 10. Habib GS, Bashir M, Jabbour A. Increased blood glucose levels following intra-articular injection of methylprednisolone acetate in patients with controlled diabetes and symptomatic osteoarthritis of the knee. Ann Rheum Dis. 2008;67:1790-1791. [DOI] [PubMed] [Google Scholar]
- 11. Habib GS, Miari W. The effect of intra-articular triamcinolone preparations on blood glucose levels in diabetic patients: a controlled study. J Clin Rheumatol. 2011;17:302-305. [DOI] [PubMed] [Google Scholar]
- 12. Habib GS, Safia A. The effect of intra-articular injection of betamethasone acetate/betamethasone sodium phosphate on blood glucose levels in controlled diabetic patients with symptomatic osteoarthritis of the knee. Clin Rheumatol. 2009;28:85-87. [DOI] [PubMed] [Google Scholar]
- 13. Kim N, Schroeder J, Hoffler CE, Matzon JL, Lutsky KF, Beredjiklian PK. Elevated hemoglobin A1C levels correlate with blood glucose elevation in diabetic patients following local corticosteroid injection in the hand: a prospective study. Plast Reconstr Surg. 2015;136:474e-479e. [DOI] [PubMed] [Google Scholar]
- 14. Koh S, Nakamura S, Hattori T, Hirata H. Trigger digits in diabetes: their incidence and characteristics. J Hand Surg Eur Vol. 2010;35:302-305. [DOI] [PubMed] [Google Scholar]
- 15. Moon HJ, Choi KH, Lee SI, Lee OJ, Shin JW, Kim TW. Changes in blood glucose and cortisol levels after epidural or shoulder intra-articular glucocorticoid injections in diabetic or nondiabetic patients. Am J Phys Med Rehabil. 2014;93:372-378. [DOI] [PubMed] [Google Scholar]
- 16. Nimigan AS, Ross DC, Gan BS. Steroid injections in the management of trigger fingers. Am J Phys Med Rehabil. 2006;85:36-43. [DOI] [PubMed] [Google Scholar]
- 17. Pai LW, Hung CT, Li SF, Chen LL, Chung Y, Liu HL. Musculoskeletal pain in people with and without type 2 diabetes in Taiwan: a population-based, retrospective cohort study. BMC Musculoskelet Disord. 2015;16:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stepan JG, London DA, Boyer MI, Calfee RP. Blood glucose levels in diabetic patients following corticosteroid injections into the hand and wrist. J Hand Surg Am. 2014;39:706-712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Uboldi F, Carlo-Stella N, Belloli L, Massarotti M, Marasini B. Glucose blood levels after intra-articular steroid injection in diabetic and non-diabetic patients. Clin Rheumatol. 2009;28:491-492. [DOI] [PubMed] [Google Scholar]
- 20. Wang AA, Hutchinson DT. The effect of corticosteroid injection for trigger finger on blood glucose level in diabetic patients. J Hand Surg Am. 2006;31:979-981. [DOI] [PubMed] [Google Scholar]
- 21. Xiao RC, Walley KC, DeAngelis JP, Ramappa AJ. Corticosteroid injections for adhesive capsulitis: a review [published online July 18, 2016]. Clin J Sport Med. doi: 10.1097/JSM.0000000000000358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.