Abstract
Objective
To quantify the Head Start (HS) teacher mediating and moderating influence on the effect of a wellness policy intervention.
Design
Intervention trial within a larger randomized community trial.
Setting
HS preschools in Hawaii.
Participants
Twenty-three HS classrooms located within 2 previously randomized communities.
Intervention
Seven-month multi-component intervention with policy changes to food served and service style, initiatives for employee wellness, classroom activities for preschoolers promoting physical activity (PA) and healthy eating, and training and technical assistance.
Main Outcome Measures
The Environment and Policy Assessment and Observation (EPAO) classroom scores and teacher questionnaires assessing on knowledge, beliefs, priorities, and misconceptions around child nutrition and changes in personal health behaviors and status were the main outcome measures.
Analysis
Paired t tests and linear regression analysis tested the intervention effects on the classroom and mediating and moderating effects of the teacher variables on the classroom environment.
Results
General linear model test showed greater intervention effect on the EPAO score where teachers reported higher than average improvements in their own health status and behaviors (estimate [SE] = −2.47 (0.78), P < .05).
Conclusions and Implications
Strategies to improve teacher health status and behaviors included in a multi-component policy intervention aimed at child obesity prevention may produce a greater effect on classroom environments.
Keywords: preschool wellness policy, childhood obesity, employee wellness, mediation analysis
INTRODUCTION
Children being overweight and obese is defined as having a body mass index for age above the 85th percentile. It is a serious public health concern in the US1,2 and increases risk for cardiovascular disease, diabetes, and cancer and for being overweight and obese as adults.3–6 Prevalence of childhood obesity is especially high in Native Hawaiian and Pacific Islander children.7–9 In Hawai’i, about 39% of children entering kindergarten are overweight or obese.9
An obesogenic environment refers to the social and built environments (eg, policies, food availability, access to physical activity [PA], norms) that encourage people to eat more calories than they expend, leading to obesity.10 The already high prevalence of unhealthy weight combined with the dynamic interactions between personal and built environmental factors contributes to the risk for developing obesity and has created a need for multilevel interventions that address various environmental factors and influences of obesity.10
The early childhood years present a sensitive time when a child’s lifelong eating habits and risk for future obesity are developed.11,12 Child care centers are good venues for obesity prevention. About half of US children under age 5 years spend a significant amount of time in these centers, where they consume two-thirds of daily nutritional needs through meals and snacks.13,14 Many US states have made progress toward implementing child care center licensing requirements that address preventing obesity, but such requirements are not currently in place in Hawai‘i.15
Head Start (HS) is a federally funded preschool program serving low-income children aged 3–5 years.16 Head Start teachers have an influential role in ensuring compliance with nutrition policies, and thus serve as a potential leverage point for obesity prevention efforts through policy change.17,18 Successful HS interventions have used collaborative approaches and have provided training and technical assistance for new policy implementation and facilitated employee wellness activities to support childhood obesity prevention efforts.19–24 For example, Lanigan’s23 wellness policy intervention was based on 3 principles that providers would be more likely to adopt childhood obesity prevention practices if: (1) they felt that failure to do so would be damaging to children, (2) they felt they could make a difference in children’s eating habits, and (3) they were provided with training and tools to make changes. The intervention collaborated with teachers to create center goals for obesity prevention and provided education, training, and resources to implement the goals. The study found positive correlations between center staff’s feeding knowledge, misconceptions, and self-efficacy and observed child care center meal time feeding practices, nutrition education, and family communication, which suggested that teachers are an influencing factor on classroom practices.23 Another employee wellness intervention, targeting improving the health status and behaviors of preschool teachers, demonstrated a positive effect on teachers’ self-efficacy for communicating nutrition information to parents and on the frequency of fruits and vegetables served at centers, which suggested that interventions promoting teacher wellness can have effects that affect child health, in this case increasing the availability of fruits and vegetables in classrooms.22 Other studies demonstrated that teachers’ feeding styles influence children’s food consumption25 and that teachers’ lack of concern about childhood obesity becomes a barrier to prevention efforts.18 These influences and findings regarding the effects of employee wellness on classroom availability of fruits and vegetables suggest that teacher-level characteristics could explain some level of intervention effectiveness or ineffectivness in these studies. It is plausible that teachers, who are making improvements to their own personal health habits, including physical activity and eating, may place a greater emphasis on PA and healthy eating in their classrooms.
Mediation and moderation analysis offers a means to improve understanding of intervention and program outcomes.26 A mediating variable is 1 that accounts for the significant relationship observed between an independent and dependent variable, providing a potential explanation for the results seen.27 For example, an intervention successful at improving child behaviors, such as the level of PA, as the result of a policy intervention may be explained by an intervention effect on social or psychosocial variables, such as improved attitudes of intervention implementers regarding PA. On the other hand, a moderating variable affects the direction and/or strength of the relationship between an independent and dependent variable. This third variable represents an interaction effect between those variables and provides information about conditions in which an intervention can achieve the desired results.27 A moderation analysis may determine that a PA intervention was successful at improving the PA levels of females but not males, thus identifying gender as a moderating variable. Childhood obesity prevention interventions have yielded varying levels of effect on child and environmental outcomes but often lack mediation and moderation analysis, resulting in imprecise implications for future practice.18–25 Baranowski and Russell26 provided a model for intervention evaluation that was specifically designed to enhance understanding of how interventions yield desired outcomes. Implementation of this analysis can provide more information about the mechanisms of intervention effects, thus improving the precision of recommendations for practice.
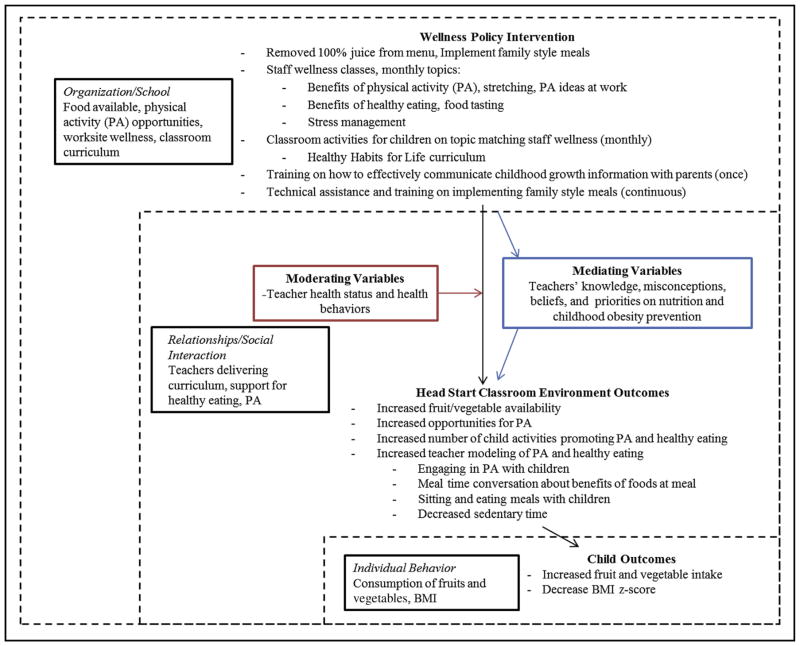
This study’s primary objective was to build evidence about the influence of HS teachers on the effect of child care center wellness policies on the nutrition and PA environment of HS classrooms in Hawai‘i. Specifically, the focus was on HS teachers’ health status, eating and PA behaviors, and efficacy, misconceptions, and knowledge related to child nutrition and priority placed on childhood obesity prevention. Figure 1 depicts the framework for this study based on the social ecologic model,10 specifically the relationship among the wellness policy intervention, the teacher level mediating and moderating variables, the classroom environment, and child level outcomes related to obesity. The researchers hypothesized that the intervention effect on the HS PA and nutrition environment would be explained (mediated) in part by teachers’ prioritization of child nutrition and beliefs that were consistent with evidenced-based practices for childhood obesity prevention, as measured by the Child Care Provider Healthy Eating and Activity survey (CCPHEA).23 Improvements in teachers’ scores, such as teacher priority, could explain why the intervention was effective in improving the classroom PA environment. Greater priority placed on childhood obesity, prevention, and healthy eating by teachers as a result of the intervention could explain why the policy intervention that included activities that promoted classroom PA were more effective in improving the classroom environment. The researchers also hypothesized that teachers’ own personal health behaviors, PA and healthy eating, and health status would influence (moderate) the intervention effect on the classroom environment.
Figure 1.
Conceptual framework of suggested mediating and moderating effects of teacher-level outcomes that may influence the relationship between the wellness policy intervention and changes in classroom and child outcomes, within the socioecological model of obesity prevention. BMI indicates body mass index.
METHODS
Setting
This research was embedded within the randomized community trial, the Children’s Healthy Living Program for Remote Underserved Minority Populations in the Pacific Region.28 A total of 23 HS classrooms located in 2 communities on O‘ahu joined the study, including 11 HS classrooms in the intervention group and 12 in the delayed-intervention group. After teachers completed informed consent, children from the 23 HS classrooms were recruited to participate at HS orientation meetings and in their classrooms by the researcher and/or HS teacher. Parents of children at HS provided consent for child participation. The Institutional Review Board from University of Hawai’i at Mānoa approved this research.
Intervention
The multi-component intervention was 7 months long; it aimed to support teachers in implementing wellness policies to promote nutrition and PA in their classrooms to affect multiple contributing factors to the availability of obesity-food, classroom activities and practices, and social norms. Described more fully elsewhere,29 this included changes to meal service style and types of food served; for example, 100% fruit juice was removed from meal and snack menus and only whole fresh or canned fruit was offered as the fruit component. Teachers were supported with classroom resources from the Healthy Habits for Life curriculum and training and technical assistance, and through monthly employee wellness activities that reinforced their role as models for healthy eating and PA in the classroom. Figure 1 lists intervention activities that were included. Monthly wellness topics were parallel to classroom resources; for example, for 1 month the wellness activity for teachers was on the benefits of PA with walk-a-mile maps around their centers and the classroom activity included a read and dance poem about the heart and being active. Policy implementation and teacher wellness activities started in October, 2013, the second month of the HS program year, after baseline data collection; it ended in May, 2014.
Assessment Tools
Table 1 lists the 3 assessment tools that were used. The Environment and Policy Assessment and Observation (EPAO) tool assessed changes in the nutrition and PA environment of the classroom as a result of policy.30 The protocol consisted of a full-day visit to review documents and observe activities. The EPAOs were completed by graduate student interns who were trained by the researcher and were blinded to the study arm of the classrooms being observed. One or 2 interns simultaneously observed each classroom at baseline in April to May, 2013, and a year later in April to May, 2014.
Table 1.
Assessment Tools and Scoring Methodology Used to Measuring Intervention Effect on Classroom Environment and Teachers’ Influence on that Relationship
| Assessment Tool Description | Assessment Items | Scoring Methodology | |
|---|---|---|---|
| EPAO28: Tests effect of policy implementation and intervention on nutrition and PA classroom environment | EPAO nutrition sub-areas
|
EPAO PA sub-areas
|
Items (n = 81) coded 0, 1, or 2 (0 = least desirable; 2 = most desirable) Mean of each sub-area item multiplied by 10 (range, 0–20) for sub-area score Mean of 8 nutrition sub-areas = total nutrition score Mean of 8 PA sub-areas = total PA score Mean of total nutrition and PA scores = total EPAO score for each classroom at baseline and follow-up |
| Child Care Provider Healthy Eating and Activity Survey23: Assess teachers’ efficacy, knowledge, and misconceptions about child nutrition and priority placed on childhood obesity prevention |
|
Responses coded 1–4 (strongly disagree to strongly agree), with lower score for more desirable response. 4 category scores calculated (efficacy, misconceptions, knowledge, and priority) by summing category items (range, 3–20): efficacy, questions 1–3; misconception, questions 4–6; feeding knowledge, questions 10–14; and priority, questions 7–9. |
|
| Monthly teacher health status, diet habits, and PA behavior survey29: Changes in teacher health status, diet habits, and PA behaviors | Have you seen an improvement in your knowledge and skills of physical activities? Have you seen an improvement in your knowledge and skills of nutrition and healthy eating? Have you seen an increase in physical activity? Have you been choosing water over soda and sugary drinks? Have you been eating more vegetables and fruits? Have you been reducing your portion size? Have you seen an improvement in your overall physical health? Have you seen any loss of body weight? Have you seen any improvement in your cholesterol? Have you seen any improvement in your blood pressure? Have you seen any improvement in your mental health? |
Yes = 1; no = 0 Sum of responses calculated each month (range, 0–14) Mean of each month’s total taken to create 1 Health Behavior and Indicators score/classroom |
|
EPAO indicates Environment and Policy Assessment and Observation; PA, physical activity.
The CCPHEA is a validated tool developed by Lanigan23 that assesses child care providers’ efficacy, knowledge, misconceptions, and priorities regarding their role in child feeding, nutrition, and obesity prevention (Table 1). It was selected to demonstrate the mediating role of teachers regarding the effect of policy implementation on environmental changes (EPAO scores). Head Start staff in intervention and delayed intervention classrooms completed the survey before participating in the wellness policy training in August, 2013, and at again in April to May, 2014.
A monthly survey assessing teacher health status, diet habits, and PA behaviors was adapted from a previous study, prompting teachers to assess changes in their own health status, diet, and PA behaviors (11 items in total) as a result of the monthly employee wellness activities.31 Survey items were used to calculate a Health Behavior Indicator (HBI) score (Table 1). The HBI scores were used in the moderation analysis of HS teachers’ health status on the intervention effect.
Statistical Analysis
The researchers used paired t tests to assess HS center–level changes. Multiple regression models were used to compare HS center–level outcomes in nutrition and PA practices between the intervention and delayed intervention classrooms, controlling for baseline scores.
To test the mediating effect of teacher CCPHEA scores (efficacy, priority, knowledge, and misconceptions) on the intervention effect of class level, the criteria of Baron and Kenny27 were followed for the establishment of mediation. A series of linear regression models were estimated to test whether detected effects of the intervention on class-level outcomes were mediated by teacher CCPHEA. For mediation to be inferred, the association originally found between the intervention and the outcome variables had to be decreased or eliminated after mediators were added to the model.27
To test the moderating effect of teacher HBI scores (teachers’ health status, diet, and PA behaviors) on the intervention effect of class-level outcomes, teacher HBI scores were dichotomized to 1 = scores at or above the mean and 0 = scores below the mean. An interaction term was then created between the intervention variable (coded as 1 = treatment group and 0 = delayed intervention group) and HBI variables and added to the regression models.
Statistical significance for all tests was set at P < .05 for 2-tailed tests and conducted using SAS, version 9.4 (Chapel Hill, NC, 2012).
RESULTS
The teacher sample included 46 teachers from 23 HS classrooms, 2 teachers per HS classroom. The EPAOs were completed at baseline and at 7-month follow-up for all 23 classrooms. The CCPHEA surveys were completed by 1 or both HS teachers in each classroom at baseline and follow-up. In cases where both teachers completed CCPHEA surveys, the mean score of the 2 teachers was used for analysis.
No baseline significant difference was observed between intervention HS classes and delayed intervention HS classes in EPAO-total score nutrition and PA environment, or in teacher CCPHEA scores on misconception, knowledge, or priority related to child nutrition (Table 2). Only the baseline mean teacher CCPHEA efficacy score was significantly higher in the intervention classrooms (mean, 7.00; SD, 1.00) than in the delayed intervention classrooms (mean, 6.10; SD, 0.80).
Table 2.
Covariate Adjusted Means of Class-Level EPAO Nutrition, PA, and Total Scores and CCPHEA Misconception, Priority, Knowledge, and Efficacy Related to Child Nutrition at Postintervention, Comparing Intervention and Control Classroomsa
| Variables | Intervention Group Mean (SE) | Control Group Mean (SE) | Pb |
|---|---|---|---|
| EPAO-Nutrition | 14.9 (0.40) | 14.9 (0.39) | .98 |
| EPAO-PA | 16.5 (0.45) | 14.3 (0.43) | .002 |
| EPAO-Total | 15.7 (0.33) | 14.6 (0.32) | .04 |
| CCPHEA-Misconceptions | 6.5 (0.20) | 6.4 (0.21) | .85 |
| CCPHEA-Priority | 9.8 (0.37) | 9.5 (0.40) | .64 |
| CCPHEAS-Knowledge | 9.7 (0.41) | 10.0 (0.43) | .53 |
| CCPHEA-Efficacy | 6.1 (0.35) | 5.6 (0.38) | .32 |
CCPHEA indicates Child Care Provider Healthy Eating and Activity Survey; EPAO, Environment and Policy Assessment and Observation; PA, physical activity.
General linear regression model adjusted for baseline values;
Global F test in which at postintervention, the difference in means between the 2 groups is 0.
Teacher HBI scores ranged from 3 to 10.8 (possible range, 0–11). There was no significant difference in the mean average monthly teacher HBI scores between intervention and delayed intervention classrooms (7.67 ± 2.00 and 7.27 ± 2.11; P = .88).
Table 3 lists general linear regression model results on the differences between intervention and delayed intervention group follow-up EPAO-PA and EPAO-total scores, adjusting for baseline scores and testing for CCPHEA-priority mediation. There were no significant differences in EPAO-nutrition or any other CCPHEA scores between the intervention and delayed intervention groups. Mediation analysis found evidence of a mediating effect for CCPHEA–priority only on the intervention effect on EPAO-total but not on EPAO-PA (Table 3). The difference on EPAO-total between the 2 groups was reduced by 0.2 points from 1.1 to 0.9, and the difference between groups was no longer significant at P = .05.
Table 3.
Model Testing Teacher Priority Mediation as Determined by CCPHEA on Intervention Effects for Class-Level Total and PA Environment and Policy Changes Based on EPAO
| Variables | Intervention Group Mean (SE) Follow-Up | Delayed Intervention Group Mean (SE) Follow-Up | Difference | Pe |
|---|---|---|---|---|
| EPAO-PA | ||||
| Original modela | 16.5 (0.45) | 14.3 (0.43) | 2.2 | .002 |
| CCPHEA-priority modelb | 16.3 (0.42) | 14.4 (0.42) | 1.9 | .005 |
|
| ||||
| EPAO-Total | ||||
| Original modelc | 15.7 (0.33) | 14.6 (0.32) | 1.1 | .04 |
| CCPHEA-priority modeld | 15.6 (0.32) | 14.7 (0.32) | 0.9 | .08 |
CCPHEA indicates Child Care Provider Healthy Eating and Activity Survey; EPAO, Environment and Policy Assessment and Observation; PA, physical activity.
Adjusted for baseline EPAO-PA score;
Adjusted for baseline EPAO-PA and CCPHEA-priority;
Adjusted for baseline EPAO-Total score;
Adjusted for baseline EPAO-Total and CCPHEA-priority;
Global F test in which at follow-up, the difference in means between the 2 groups is 0.
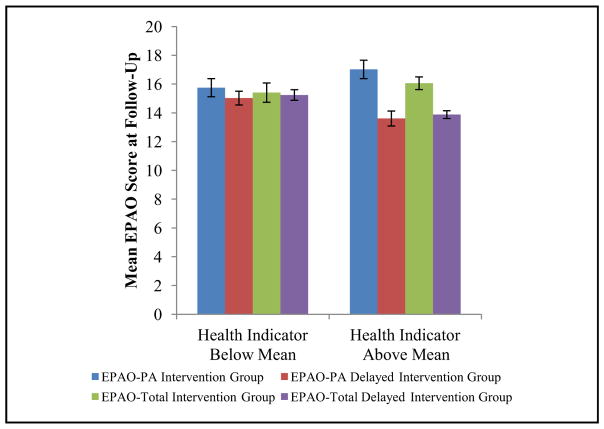
Moderation analysis demonstrated that in classrooms where teachers reported above-average HBI scores, the intervention had a greater effect on EPAO-PA and EPAO-total scores than it did in classrooms where teachers reported below-average HBI scores (Table 4). Classrooms in which teachers reported improvements above the mean in their own health behaviors also showed a greater intervention effect on EPAO-PA and EPAO-total scores (Figure 2).
Table 4.
Moderating Effect of Teacher HBI Status (Above or Below Mean) on Total and PA Classroom Scores Based on EPAO, General Linear Model (Global F Test)
| Parameter | Estimate (SE) | t | Pr > |t| |
|---|---|---|---|
| EPAO-Total Model | |||
| Intercept | 7.05 (3.12) | 2.26 | .04 |
| Group (reference: delayed intervention) | 2.17 (0.53) | 4.10 | .001 |
| EPAO-Total | 0.63 (0.22) | 2.91 | .01 |
| HBI < mean (reference: > mean) | −1.07 (0.57) | −1.87 | .08 |
| Group × HBI intervention | −2.47 (0.78) | −3.15 | .006 |
|
| |||
| EPAO-PA Model | |||
| Intercept | 14.65 (3.16) | 4.63 | .001 |
| Group (reference: delayed intervention) | 3.46 (0.79) | 4.36 | .001 |
| EPAO-PA | 0.16 (0.22) | 0.76 | .46 |
| HBI < mean (reference: > mean) | −1.22 (0.83) | −1.46 | .16 |
| Group × HBI intervention | −2.65 (1.15) | −2.30 | .03 |
EPAO indicates Environment and Policy Assessment and Observation; HBI, Health Behavior and Indicators; PA, physical activity.
Figure 2.
Environment and Policy Assessment and Observation (EPAO) total and physical activity (PA) mean scores for intervention and delayed-intervention group at follow-up by teachers’ reported improvements in health behaviors and indicators below or above the mean.
DISCUSSION
The findings of this study suggest positive effects of a policy intervention on the HS PA environment. More important, they demonstrate the significant impact that HS teachers’ personal health behaviors have, as well as the priority they place on child nutrition, on the success of a classroom-based intervention. However, the policy intervention, which included changes to meal service style and types of foods and beverages served, did not have a significant impact on the HS nutrition environment.29 Other components of the intervention that aimed to improve teachers’ level of PA—for example, worksite wellness lessons on the benefits of PA and maps outlining a 1-mile walking path near the center—in addition to classroom activities that supported PA were effective in improving the PA environment in these classrooms.
Other interventions similarly showed greater changes observed in the PA components of the classroom environment than in the nutrition components. In the Georgia Department of Early Care and Learning study, significant effects of policy intervention on both the nutrition and PA components of the EPAO scores showed a smaller proportion of improvement in the nutrition sub-areas (2 of 8) compared with the PA sub-areas (5 of 8).20
However, in this study there was a mediating relationship between CCPHEA-priority scores and the intervention effect. In classrooms where higher priority was given to child nutrition, there was an observed increase in intervention effect. Lanigan’s23 Encouraging Healthy Activity and Eating in Childcare Environments intervention program found positive correlations between other CCPHEA variables, but not priority, and intervention effect on the classroom environmental factors. In a qualitative study, beliefs held by HS teachers, such as a low priority placed on childhood obesity, were identified as barriers to obesity prevention efforts.18 The current study’s finding that teacher priority regarding child nutrition influences the intervention effect quantitatively supports past qualitative evidence that the lack of priority placed on childhood obesity by HS teachers can be a barrier to prevention efforts.18
A moderating effect of teachers’ own health behaviors and status was found on the intervention effect on the classroom environment. Teachers who reported improvements in their own PA levels, weight control, dietary habits, skills, and knowledge about nutrition, above the mean, saw a greater intervention effect on the PA classroom environment than did teachers who showed no improvements. Other child care provider employee wellness interventions demonstrated similar effects of intervention activities on classroom outcomes, primarily related to foods offered in the classroom.22,23 Both of these findings support the influential role teachers have in facilitating a nutrition- and PA-promoting environment in preschool settings. It is likely that teachers who are moving toward improvements in their own health behaviors and status will create classrooms in which obesity prevention efforts are better supported. For example, a teacher who is increasing his or her own PA level may be more likely to engage in PA with children or may have experienced the benefits of PA personally, feeling more motivated to promote PA in the classroom. Figure 1 demonstrates how the intervention and outcomes address multiple factors that influence obesity, the organizational or school environment, the social interactions and relationships that occur in these places, and finally, the behaviors that can develop in these settings. The findings from this study suggest that an intervention that includes multiple components within the organizational or school environment—in this case employee wellness coupled with classroom-based activities—can produce a greater intervention effect on aspects of the classroom environment. The results of this study support the need for multi-component interventions that influence classroom practices as well as teachers who are responsible for implementing nutrition and health policy.
This study has some limitations. The reliance on single assessments of classroom observations and on self-reported changes in teachers’ health status, diet, and PA behaviors is limiting. Repeat and alternative assessments should be included in future investigations. Finally, although the communities included in the research study were previously randomized and matched based on US Census data on race/ethnicity, income, and size,28 the sample was limited to this geographic region of Hawai‘i and may not be generalizable.
IMPLICATIONS FOR RESEARCH AND PRACTICE
The findings from this study demonstrate the effects of a policy intervention for childhood obesity prevention on classroom-level outcomes, including the influence that teacher-level variables have on the intervention effect, the first of its kind in Hawai‘i. This study supports the hypothesis that HS teachers serve as a leverage point for creating environments that promote PA and possibly a gatekeeper for childhood obesity prevention in preschool settings. Future research and intervention efforts could be targeted at improving teachers’ health practices, such as healthy eating and PA, delivered through employee-sponsored worksite wellness initiatives, or incorporated into extension education curriculum. Wellness activities and campaigns may be able to capitalize on teachers as role models of health for children in their classroom by providing suggestions on how to be active with the children during active play or healthy lunch ideas. Effort to increase the effects of wellness policies in preschools should be multilevel and consider including components focused on helping teachers make positive changes in their personal health behaviors. Future research efforts should include more focused assessments of changes that occur from employee wellness initiatives that affect specific aspects of the PA environment in classrooms. This could include identifying whether the improvement in HBI scores comes primarily from improvements in PA level. Additional studies on how to improve the nutrition environment significantly are needed, as well as interventions that include other factors related to obesity, such as parent and home environments, that are likely to influence childhood obesity and dietary intake.
Acknowledgments
This project is supported by the Agriculture and Food Research Initiative, Grant No. 2011-68001-30335 from the US Department of Agriculture National Institute of Food and Agricultural Science Enhancement Coordinated Agricultural Program, the staff of the Children’s Healthy Living Program, Honolulu Community Action Program Head Start Program.
References
- 1.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2003;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 2010;25:1–5. [PubMed] [Google Scholar]
- 4.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150:12–17. e12. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 5.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 6.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115:22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 7.Novotny R, Fialkowski MK, Li F, et al. Systematic review of prevalance of young child overweight and obesity in the United States–Affiliated Pacific region compared with the 48 contiguous states: the Children’s Healthy Living Study. Am J Public Health. 2015;105:e22–e35. doi: 10.2105/AJPH.2014.302283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baruffi G, Hardy CJ, Waslien CI, Uyehara SJ, Krupitsky D. Ethnic differences in the prevalence of overweight among young children in Hawai‘i. J Am Diet Assoc. 2004;104:1701–1707. doi: 10.1016/j.jada.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 9.Pobutsky A, Bradbury E, Reyes-Salvail F, Kishaba G. Overweight and obesity among Hawai‘i children aged 4 to 5 years enrolled in public schools in 2007–2008 and comparison with a similar 2002–2003 cohort. Hawai‘i J Med Public Health. 2013;72:225–236. [PMC free article] [PubMed] [Google Scholar]
- 10.Huang TT, Drewnosksi A, Kumanyika S, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6:A82. [PMC free article] [PubMed] [Google Scholar]
- 11.Nicklaus S. Development of food variety in children. Appetite. 2009;52:253–255. doi: 10.1016/j.appet.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 12.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 13.Federal Interagency Form on Child and Family Statistics. America’s Children: Key National Indicators of Well-being. Washington, DC: US Government Printing Office; 2013. [Google Scholar]
- 14.US Department of Education, NCfES, National Education Surveys Program. [Accessed March 14, 2016];Child care: percentage of children ages 3–6, not yet in kindergarten, in center-based care arrangments by child and family characteristics, and region, selected years 1995–2007. http://www.childstats.gov/americaschildren/tables/fam3b.asp?popup=true.
- 15.Benjamin SE, Cradock A, Walker EM, Slining M, Gillman MW. Obesity prevention in child care: a review of U.S. state regulations. BMC Public Health. 2008;8:188. doi: 10.1186/1471-2458-8-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Administration for Children and Families. [Accessed March 14, 2016];About Head Start. http://www.acf.hhs.gov/programs/ohs/about/head-start.
- 17.Lumeng JC, Kaciroti N, Sturza J, et al. Changes in body mass index associated with Head Start participation. Pediatrics. 2015;135:e449–e456. doi: 10.1542/peds.2014-1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes CC, Gooze RA, Finkelstein DM, Whitaker RC. Barriers to obesity prevention in Head Start. Health Aff. 2010;29:454–462. doi: 10.1377/hlthaff.2009.0499. [DOI] [PubMed] [Google Scholar]
- 19.Ward DS, Benjamin SE, Ammerman AS, Ball SC, Neelon BH, Bangdiwala SI. Nutrition and PA in child care: results from an environmental intervention. Am J Prev Med. 2008;35:352–356. doi: 10.1016/j.amepre.2008.06.030. [DOI] [PubMed] [Google Scholar]
- 20.Lyn R, Maalouf J, Evers S, Davis J, Griffin M. Nutrition and PA in child care centers: the impact of a wellness policy initiative on environment and policy assessment and observation outcomes, 2011. Prev Chronic Dis. 2013;10:E83. doi: 10.5888/pcd10.120232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alkon A, Crowley AA, Neelon SE, et al. Nutrition and PA randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health. 2014;14:215. doi: 10.1186/1471-2458-14-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gosliner WA, James P, Yancey AK, Ritchie L, Studer N, Crawford PB. Impact of a worksite wellness program on the nutrition and PA environment of child care centers. Am J Health Promot. 2010;24:186–189. doi: 10.4278/ajhp.08022719. [DOI] [PubMed] [Google Scholar]
- 23.Lanigan JD. The relationship between practices and child care providers’ beliefs related to child feeding and obesity prevention. J Nutr Educ Behav. 2012;44:521–529. doi: 10.1016/j.jneb.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 24.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91:831–840. doi: 10.3945/ajcn.2009.28826. [DOI] [PubMed] [Google Scholar]
- 25.Hughes SO, Patrick H, Power TG, Fisher JO, Anderson CB, Nicklas TA. The impact of child care providers’ feeding on children’s food consumption. J Dev Behav Pediatr. 2007;28:100–107. doi: 10.1097/01.DBP.0000267561.34199.a9. [DOI] [PubMed] [Google Scholar]
- 26.Baranowski T, Russell J. Understanding the mechanisms of change in children’s physical activity programs. Exer Sport Sci Rev. 2005;33:163–168. doi: 10.1097/00003677-200510000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 28.Wilken LR, Novotny R, Fialkowski MK, et al. Children’s Healthy Living (CHL) Program for remote underserved minority populations in the Pacific region: rationale and design of a community randomized trial to prevent early childhood obesity. BMC Public Health. 2013;13:944. doi: 10.1186/1471-2458-13-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Esquivel MK, Nigg C, Fialkowski MK, Braun K, Li F, Novotny R. Head Start Wellness Policy Intervention in Hawaii: a project of the Children’s Healthy Living Program (CHL) Child Obes. 2015;12:26–32. doi: 10.1089/chi.2015.0071. [DOI] [PubMed] [Google Scholar]
- 30.Ward D, Hales D, Haverly K, et al. An instrument to assess the obesogenic environment of child care centers. Am J Health Behav. 2008;32:380–386. doi: 10.5555/ajhb.2008.32.4.380. [DOI] [PubMed] [Google Scholar]
- 31.Yin Z, Parra-Medina D, Cordova A, et al. Miranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Child Obes. 2012;8:429–439. doi: 10.1089/chi.2012.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]