Abstract
Background and Aims
Bile duct surgery (BDS), percutaneous transhepatic cholangiography (PTC), and endoscopic retrograde cholangiopancreatography (ERCP) are alternative interventions used to treat biliary disease. We aim to describe trends in ERCP, BDS, and PTC on a nationwide level in the United States.
Methods
We used the National Inpatient Sample to estimate age-standardized utilization trends of inpatient diagnostic ERCP, therapeutic ERCP, BDS, and PTC between 1998 and 2013. We calculated average case fatality, length of stay, patient demographic profile (age, gender, payer), and hospital characteristics (hospital size and metropolitan status) for these procedures.
Results
Total biliary interventions decreased over the study period from 119.8 to 100.1 per 100,000. Diagnostic ERCP utilization decreased by 76%, and therapeutic ERCP utilization increased by 35%. BDS rates decreased by 78%, and PTC rates decreased by 24%. ERCP has almost completely supplanted surgery for the management of choledocholithiasis. Fatality from ERCP, BDS, and PTC have all decreased, whereas mean length of stay has remained stable. The proportion of, Medicare-insured, Medicaid-insured and uninsured patients undergoing biliary procedures has increased over time. The majority of the increase in therapeutic ERCP and decrease in BDS occurred in large, metropolitan hospitals.
Conclusions
Although therapeutic ERCP utilization has increased over time, the total volume of biliary interventions has decreased. BDS utilization has experienced the most dramatic decrease, possibly a consequence of the increased therapeutic capacity and safety of ERCP. ERCPs are now predominantly therapeutic in nature. Large urban hospitals are leading the shift from surgical to endoscopic therapy of the biliary system.
Introduction
Bile duct surgery (BDS), percutaneous transhepatic cholangiography (PTC), and endoscopic retrograde cholangiopancreatography (ERCP), are alternative interventions used in the management of biliary tract disease. Before the widespread availability of ERCP, BDS was the mainstay of treatment for biliary disease. The first endoscopic cannulation of the ampulla of Vater was described in 1968,1 and technological advances over subsequent decades led to widespread adoption of ERCP as a critical therapeutic modality in the management of biliary tract pathology.2–6 PTC also evolved in the 1970s, but has largely remained a “rescue procedure” used when therapeutic ERCP fails, is not feasible due to patient instability, or is unavailable.7
A single previous study has described trends in ERCP utilization on a population-level in the United States. The study indicated that diagnostic ERCPs peaked in 1996 and subsequently down-trended up to the last studied year, whereas inpatient therapeutic ERCPs continued to increase over the study period.8 These data are now greater than a decade old, and it is unknown if the previously described trends in ERCP utilization persist.8
It is widely assumed based on convenience, cost, and patient preference, that therapeutic ERCP has gradually supplanted surgical exploration and PTC as the preferred method for management of biliary pathology, and this has certainly been consistent with the experience at our center. However, there are no population-level data confirming these trends because BDS and PTC trends have not been previously described in the United States.
In this study, we describe overall utilization trends in diagnostic ERCP, therapeutic ERCP, BDS, and PTC in the United States using an annual, nationwide, stratified sample of all discharges between the years 1998 and 2013. We also describe changes in hospitalization length, mortality, demographic profiles, and hospital characteristics for these interventions over time.
Methods
Databases
The National Inpatient Sample (NIS) is a component of the Healthcare Cost and Utilization Project (HCUP), and is the largest publicly available all-payer inpatient healthcare database in the United States yielding national estimates of hospital inpatient stays. It provides reliable estimates from more than 35 million hospitalizations nationally, based on a stratified cluster random sampling of more than 7 million hospital stays each year (approximately 20% of admissions from all non-Federal, acute care U.S. hospitals). The NIS covers all patients, including individuals covered by Medicare, Medicaid, or private insurance, as well as those who are uninsured. It captures both clinical and non-clinical data including primary and secondary diagnoses, primary and secondary procedures, patient demographic characteristics, hospital characteristics, payment sources and charges, discharge status, and length of stay. Data from 1998 to the last available year at the time of this study (2013) were gathered.
To determine the relative proportions of inpatient and outpatient ERCPs, we also extracted data from the State Ambulatory Surgery Database (SASD), a component of HCUP, which contains data on ambulatory surgeries and procedures occurring in free-standing ambulatory surgical centers and hospital outpatient departments. Data were gathered for the end of our study period from the 3 largest states which participate in the SASD: New York (year 2013), Florida (year 2013), and California (year 2011 because this was the last available year of data).
Study Definitions
All patients who were discharged between 1998 and 2013 with an International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) primary procedure code for diagnostic ERCP, therapeutic ERCP, BDS, and PTC were included. The specific ICD-9-CM codes used are as follows: diagnostic ERCP (51.10, 51.11), therapeutic ERCP (51.14, 51.15, 51.64, 51.84, 51.85, 51.86, 51.87, 51.88), BDS (51.32, 51.36, 51.41, 51.42, 51.43, 51.49, 51.51, 51.59, 51.71, 51.72, 51.79), and PTC (51.96, 51.98) (see Supplementary Table 1 for description of codes). BDS was further classified by ICD-9-CM family as anastomosis of bile duct (51.32, 51.36), incision for relief of bile duct obstruction (51.41, 51.42, 51.43, 51.49), other incision of bile duct (51.51, 51.59), and repair of bile ducts (51.71, 51.72, 51.79).
Data Collection and Analysis
National incidence rates of inpatient diagnostic ERCP, therapeutic ERCP, BDS, and PTC were calculated per 100,000 U.S. residents per year. Mean inpatient length of stay and mean case fatality rates were calculated for each group of interventions. Demographic and hospital data were recorded for each group of interventions, including age group, gender, and payer information, hospital size, and hospital metropolitan status.9 An indirect standardization method using the census year 2010 as the reference year was used.10 U.S. population data were derived from the annual Bridged-Race Population Estimates, published by the National Center for Health Statistics of the Centers for Disease Control.11 All data extraction and analysis was performed on SAS Enterprise Guide Version 7.11 (SAS Institute Inc., Cary, NC).
Results
Utilization Trends
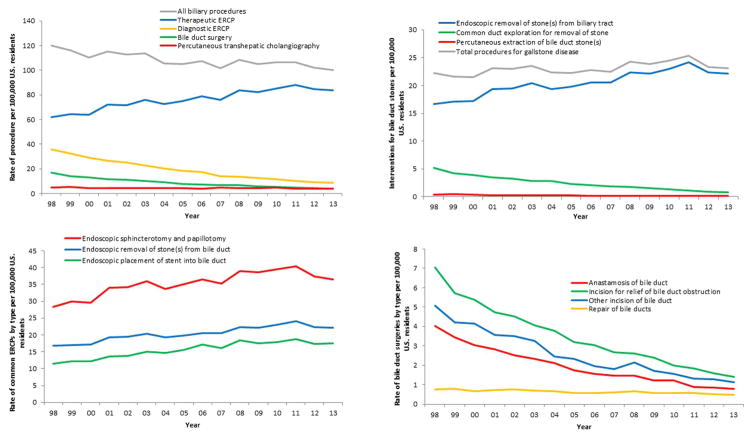
Age-standardized utilization trends for diagnostic ERCP, therapeutic ERCP, BDS, and PTC are shown in Figure 1A. Total biliary interventions (defined as the aggregate of diagnostic ERCP, therapeutic ERCP, BDS, and PTC) declined 15.6%, from 119.8 (95% CI, 114.6–125.0) to 100.1 (95% CI, 97.5–102.7) per 100,000 between 1998 and 2013. Total ERCP utilization decreased 5.6%, from 98.0 (95% CI, 93.9–102.1) to 92.5 (95% CI, 90.5–94.5) per 100,000 over this time period. There were substantial differences in trends between diagnostic and therapeutic ERCPs. Diagnostic ERCPs decreased 76.1%, from 36.0 (95% CI, 33.7–38.4) to 8.6 (95% CI, 8.2–9.0) per 100,000; therapeutic ERCPs increased 35.3%, from 62.0 (95% CI, 58.4–65.6) to 83.9 (95% CI, 82.1–85.8) per 100,000. On a per capita basis, the decrease in rate of diagnostic ERCPs was greater than the increase in rate of therapeutic ERCPs. BDS demonstrated a 77.5% decline over the study period, from 16.9 (95% CI, 14.2–19.6) to 3.8 (95% CI, 2.2–5.4) per 100,000. PTC demonstrated a 24.0% decline, from 5.0 (95% CI, 4.2–5.8) to 3.8 (95% CI, 3.6–4.0) per 100,000.
Figure 1.
A, Age-standardized trends in the rate of diagnostic ERCP, therapeutic ERCP, BDS, and PTC per 100,000 United States residents. “All biliary interventions” is defined as the sum of diagnostic ERCP, therapeutic ERCP, BDS, and PTC. B, Age-standardized trends in the rate of ERCP (51.88), BDS (51.41), and PTC (51.96) for the management of bile duct stones. ‘All interventions for bile duct stones’ is defined as the sum of 51.88, 51.41, and 51.96. C, Age-standardized rates of endoscopic sphincterotomy and papillotomy (51.85), endoscopic insertion of stent into bile duct (51.87) and endoscopic removal of stone(s) from biliary tract (51.88). D, Age-standardized rates of BDS per 100,000 United States residents by primary type of surgery: anastomosis of bile duct (51.32, 51.36), incision for relief of bile duct obstruction (51.41, 51.42, 51.43, 51.49), other incision of bile duct (51.51, 51.59), and repair of bile ducts (51.71, 51.72, 51.79). See Supplemental Tables 2 and 3 for corresponding data tables.
Trends in Intervention for Choledocholithiasis
Endoscopic removal of stone(s) from biliary tract (ICD-9-CM 51.88), common duct exploration for removal of stone(s) (ICD-9-CM 51.41), and percutaneous extraction of bile duct stone(s) (ICD-9-CM 51.96) are alternative interventions used to manage choledocholithiasis. The individual trends of these 3 interventions, as well as the aggregate utilization of these 3 interventions, are shown in Figure 1B. Although the aggregate number of procedures for choledocholithiasis has increased only very mildly over time (from 22.2 per 100,000 in 1998 to 23.0 per 100,000 in 2013), there have been significant changes in the distribution of these procedures. Total ERCP use for choledocholithiasis has increased from 16.7 to 22.1 per 100,000; conversely, common duct exploration has decreased from 5.2 to 0.8 per 100,000. Percutaneous extraction has remained an uncommonly used intervention, decreasing in rate from 0.3 to 0.1 per 100,000. At the beginning of the study period, ERCP accounted for 75.2% of all procedures for choledocholithiasis. By the end of the study period, ERCP accounted for 96.1% of all procedures for choledocholithiasis.
Trends in Common Therapeutic ERCP Codes
The 3 most common therapeutic ERCPs were endoscopic sphincterotomy and papillotomy (ICD-9-CM 51.85), endoscopic insertion of stent into bile duct (ICD-9-CM 51.87), and endoscopic removal of stone(s) from biliary tract (ICD-9-CM 51.88), which collectively made up over 85% of therapeutic ERCPs in 2013. The age-standardized rates of these 3 procedures are shown in Figure 1C. Although all 3 procedures demonstrated increases over time, endoscopic insertion of stent into bile duct had the large percentage increase (53%) over the study period.
Trends in BDS by Surgery Type
Trends in BDS by ICD-9-CM procedure family are showing in Figure 1D. Although all 4 BDS groups experienced declines, incisions for relief of bile duct obstruction experienced the largest decrease, from 7.0 per 100,000 in 1998 to 1.4 per 100,000 in 2013 (80.0% decrease). Repair of bile ducts experienced the smallest decline, from 0.8 per 100,000 in 1998 to 0.5 per 100,000 in 2013 (37.5% decrease).
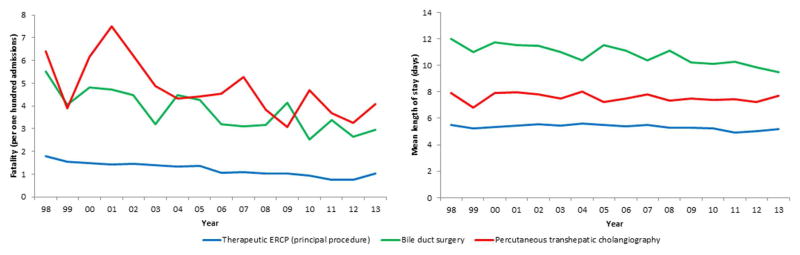
Trends in Case Fatality and Length of Stay
Trends in case fatality during admissions for which therapeutic ERCP, BDS, or PTC are the principal procedure between 1998 and 2013 are depicted in Figure 2A. Therapeutic ERCPs demonstrate a consistently lower case fatality rate compared with BDS and PTC. In 1998, 1.8 deaths per 100 hospitalizations were noted when therapeutic ERCP was the principal procedure; this rate decreased to 1.0 deaths per 100 hospitalizations by 2013. BDS case fatality declined from 5.5 to 3.0 per 100 hospitalizations between 1998 and 2013. PTC also demonstrated a reduction in case fatality from 6.4 to 4.1 deaths per 100 hospitalizations between 1998 and 2013.
Figure 2.
A, Trends in case fatality (defined as in-hospital deaths per 100 discharges) for hospitalizations in which ERCP, BDS, or PTC is listed as the principal procedure. B, Trends in average length of stay for hospitalizations in which ERCP, BDS, or PTC is listed as principle procedure. See Supplementary Tables 4 and 5 for corresponding data tables.
Trends in length of stay of hospitalizations with principal procedure of therapeutic ERCP, BDS, or PTC demonstrated modest changes over time (Figure 2B). In 1998, BDS, PTC, and therapeutic ERCP had mean length of stay of 12.0, 7.9, and 5.5 days, respectively. In 2013, BDS, PTC, and ERCP mean length of stay had decreased to 9.5, 7.7, and 5.2 days, respectively.
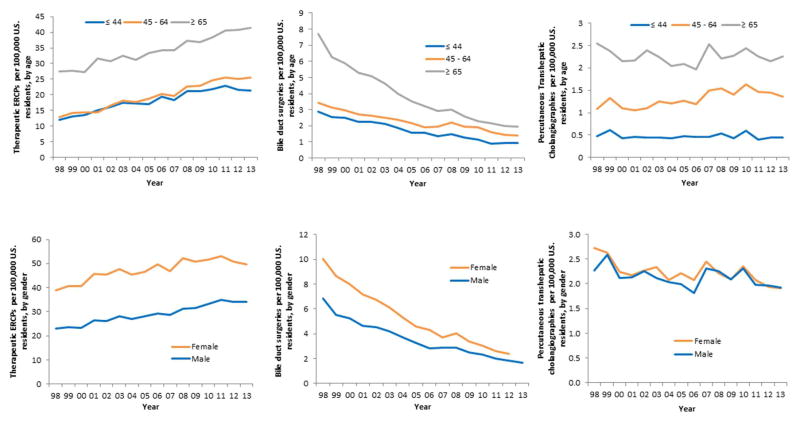
Demographic Profile of Patients
Trends in rates of ERCP, BDS, and PTC all remained consistent across age and gender brackets over the 16-year study period (Figure 3). Patients who underwent therapeutic ERCPs tended to be predominantly female and older. Therapeutic ERCPs increased from 39.0 to 49.8 per 100,000 for females, and from 23.0 to 34.0 per 100,000 for males over the study period. Approximately half of ERCPs were performed on patients 65 and older. The age and gender profile of patients undergoing BDS was similar to the profile of patients undergoing ERCP. Unlike ERCP and BDS, patients undergoing PTC were equally likely to be female as male, with an approximately equal ratio over the study period
Figure 3.
Trends in the rate of therapeutic ERCP. (A), BDS (B), and PTC (C) by age. Age-standardized trends in the rate of therapeutic ERCP (D), BDS (E), and PTC (F) by gender. See Supplementary Tables 6 and 7 for corresponding data tables.
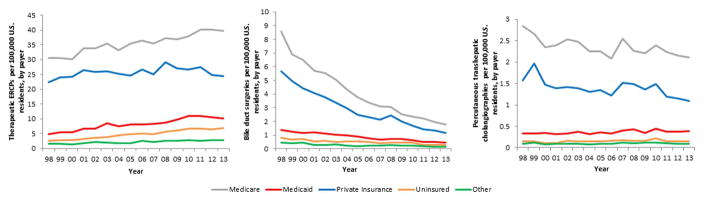
Payer Profile of Patients
The payer profile of patients undergoing inpatient biliary procedures is depicted in Figure 4. There were higher rates of Medicaid-insured and uninsured patients undergoing biliary procedures of all types in 2013 compared with 1998. The increase in rates of Medicaid-insured and uninsured patients was greatest for therapeutic ERCP. In 1998, 4.9 Medicaid and 2.6 uninsured per 100,000 therapeutic ERCPs occurred; this rate increased to 10.1 Medicaid and 6.8 uninsured per 100,000 by 2013. The payer profile for BDS and PTC also reflected proportionally more Medicaid-insured and uninsured patients in 2013 relative to 1998. All 3 procedures demonstrated a lower proportion of privately insured patients in 2013 relative to 1998.
Figure 4.
Age-standardized trends in payer profile for therapeutic ERCP (A), BDS (B), and PTC (C). See Supplementary Table 8 for corresponding data table.
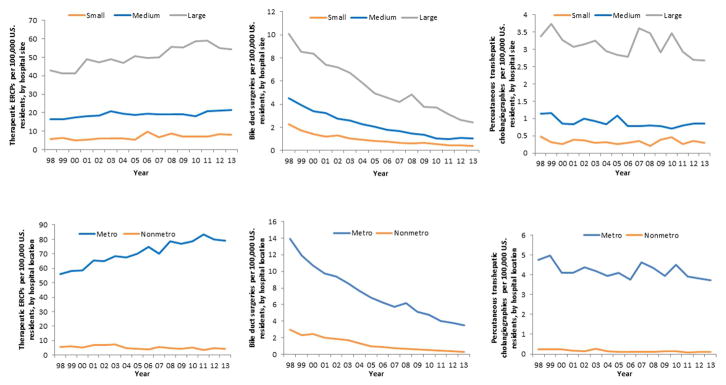
Hospital Characteristics
The characteristics of hospitals performing biliary procedures are depicted in Figure 5. The rate of therapeutic ERCPs consistently increased over time for hospitals of all sizes. Large hospitals performed twice as many therapeutic ERCPs as medium-sized hospitals, and roughly seven-fold as many as small hospitals throughout the study period. Therapeutic ERCPs were performed far more frequently in hospitals located in metropolitan areas, and this rate increased between 1998 (56.2 per 100,000) and 2013 (79.3 per 100,000). Non-metropolitan hospitals performed therapeutic ERCPs at rates lower than metropolitan hospitals throughout the study period; in addition, non-metropolitan hospitals showed a decrease in the rate of therapeutic ERCPs between 1998 (5.6 per 100,000) and 2013 (4.5 per 100,000).
Figure 5.
Age-standardized trends in the rate of therapeutic ERCP (A), BDS (B), and PTC (C) by hospital size. Age-standardized trends in the rate of therapeutic ERCP (D), BDS (E), and PTC (F) by hospital metropolitan status. See text for description of classifications of hospital characteristics. See Supplementary Tables 9 and 10 for corresponding data tables. Metro; metropolitan-located hospital; non-metro; non-metropolitan located hospital.
BDS was performed more frequently in large hospitals compared with medium-sized hospitals, and more frequently in medium-sized hospitals compared with small hospitals. Hospitals located in metropolitan areas performed BDS at a higher rate (13.9 per 100,000 in 1998 and 3.5 per 100,000 in 2013) compared with hospitals in non-metropolitan areas (3.0 per 100,000 in 1998 and 0.3 per 100,000 in 2013), and both rates decreased over time. Similar to BDS and therapeutic ERCP, PTC was more likely to be performed in large hospitals and in hospitals located in metropolitan areas.
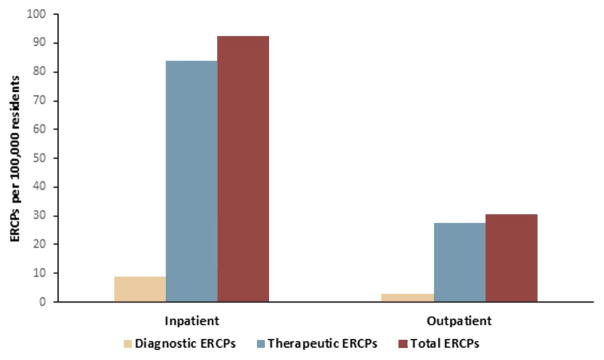
Proportion of Outpatient to Inpatient ERCPs
Data from the California, Florida, and New York SASD databases indicate 30.3 outpatient ERCPs performed per 100,000 residents. In contrast, 92.5 inpatient ERCPs were performed per 100,000 residents in 2013, based on NIS data. Thus the majority of ERCPs by the end of our study period were still being performed on an inpatient basis, with more than 3 inpatient ERCPs performed for every outpatient ERCP. Similar to inpatient ERCPs, outpatient ERCPs were predominantly therapeutic in nature, with 27.4 outpatient therapeutic and 2.9 outpatient diagnostic ERCPs performed per 100,000 residents, respectively (Figure 6).
Figure 6.
Rate of therapeutic and diagnostic ERCPs in outpatient settings based on the State Ambulatory Surgery Databases (California year 2011, Florida year 2013, and New York year 2013) compared with inpatient rates based on the National Inpatient Sample (year 2013).
Discussion
Our data suggest that there have been dramatic changes in the clinical approach to biliary disease, with consequent changes in utilization of biliary interventions in the United States over the 16-year study period. Aggregate biliary interventions have fallen from 119.8 to 100.1 per 100,000 U.S. residents. The major drivers of this trend are both a 76% decline in the rate of diagnostic ERCPs, and a 78% decline in the rate of BDS. The greatest rates of decline were noted for BDS involving incision of the bile duct for relief of obstruction/other reasons and creation of bile duct anastomoses. Notably, repair of bile ducts demonstrated the least decrease over the study period. This may be related to the continued need for bile duct repair to manage laparoscopic cholecystectomy-associated bile duct injury. The rate of therapeutic inpatient ERCPs has continued to increase at a brisk pace coincident with a decrease in rates of BDS. Our data suggest that part of this increase in therapeutic ERCP utilization is due to the increased reliance on ERCP for the management of choledocholithiasis.
Although the overall burden of choledocholithiasis has remained stable, ERCP has almost completely supplanted surgical exploration for biliary stone disease. Although therapeutic ERCP is no longer practiced for some indications such as sphincter of Oddi dysfunction, the continued evolution of new technology and techniques related to ERCP together with an increase in trained therapeutic endoscopists in the United States has expanded the breadth of ERCP into realms previously reserved for BDS. For instance, single-operator choledochoscopy, electro-hydraulic lithotripsy,12 and papillary large balloon dilation13 have all facilitated endoscopic management of large bile duct stones that previously required surgical bile duct exploration. Our data also show a rapid growth in the utilization of endoscopic biliary stent placement, whereas surgical incision for relief of obstruction has fallen. Self-expandable metallic stents may have replaced surgical bypass of the bile duct for neoplastic obstructions.14–16 Improved resolution imaging with computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP) allows differentiation of unresectable pancreaticobiliary neoplasms more readily, and may be driving a shift from surgery to ERCP for palliation. These trends are likely to continue in the future. Finally, there has been a large increase in the number of interventional endoscopy training programs in the United States, from 10 positions in 2000 to >65 in 2014.17 The availability of a larger number of highly trained interventional endoscopists able to tackle complex biliary endoscopy may be contributing to a decreased reliance on BDS. Although this is the first description of rates of BDS in the United States, a study of the single Canadian province of Manitoba also indicated a marked decrease in rates of open bile duct exploration coincident with the growth of therapeutic ERCP between 1984 and 2009.18
The rate of therapeutic ERCPs increased in metropolitan area hospitals over the study period, whereas non-metropolitan hospitals demonstrated a decline in therapeutic ERCP over the study period. Prior studies have demonstrated that high volume endoscopists, typically located in large hospitals in metropolitan areas, perform ERCPs with fewer adverse events and less radiation exposure to patients and providers.19, 20 Superior outcomes may be expected if patients needing ERCP were primarily referred to these high-volume centers. Although the rate of total ERCPs has changed little, the relative contribution of therapeutic and diagnostic ERCPs has changed greatly. Diagnostic ERCPs constitute less than one tenth of all inpatient ERCPs in 2013, compared with approximately one-third of ERCPs in 1998. A major driver in this trend may be increased reliance on non-invasive imaging (including ultrasound, MRCP, and CT) and lower-risk endoscopic procedures such as endoscopic ultrasound (EUS)21 for the diagnosis of biliary disease.22 It is also likely that the true rate of ERCPs performed purely for diagnostic reasons is lower than the rate of 8.6 per 100,000 U.S. residents in 2013, as some ERCPs eventually coded as “diagnostic” are often planned with therapeutic intent (for instance, a patient with choledocholithiasis where the stone has passed by the time the ERCP is performed).20 Moreover, unsuccessful ERCPs planned with therapeutic intent may also be coded as diagnostic ERCPs.
We found that PTC utilization demonstrated relative stability over the last 16 years, and did not appear to have a correlative relationship with either the increase in inpatient therapeutic ERCPs or decrease in BDS. As PTCs are typically “rescue procedures” performed only where ERCP fails or the patient is deemed too high-risk or ill for BDS, there may be little substitution effect.
Case fatality for inpatient therapeutic ERCP has steadily decreased over the last 15 years. Improvements in ERCP endoscope and device technology, risk stratification with EUS and MRCP, patient selection, anesthesia support, and peri-procedural care perhaps all contribute to this trend. BDS was associated with a consistently longer length of stay than PTC, which in turn was associated with a longer length of stay than ERCP. Given the inherent morbidity of abdominal surgery as compared with an endoscopic or interventional radiology procedure, this finding is not unexpected.23, 24 Because PTC is often used after failure of ERCP, a longer length of stay than for ERCP would also be expected. Average length of stay decreased only very slightly for all 3 categories of procedures over the 16-year time period. As a point of reference, the average length of stay for all hospital admissions in the United States stood at 4.8 days in 1998, and decreased only slightly to 4.6 days by 2009.25
There did not appear to be any major differences with regard to age and gender distributions between therapeutic ERCP and BDS. The age and gender distributions for these 2 modalities also did not change greatly between 1998 and 2013. The payer profile for ERCP, BDS, and PTC all reflected a higher level of Medicaid-insured and uninsured patients, and a lower rate of private insurance in 2013 compared with 1998. These correspond to national trends toward decreased rates of private health insurance coverage and increased rates of Medicaid-insured and uninsured hospitalizations before the implementation of the Medicaid expansion provisions of the Patient Protection and Affordable Care Act in 2014. The majority of the increase in utilization of ERCP and the majority of decrease in utilization of BDS occurred in large, metropolitan hospitals. Large, metropolitan hospitals typically have high ERCP volumes, skilled therapeutic endoscopists, and access to cutting edge technology; this is perhaps why the transition from operative to endoscopic interventions has been greatest in these hospitals.
The study has several limitations and strengths. Our data were limited to inpatient procedures, and did not capture all outpatient ERCPs. However, our analysis of state ambulatory surgery data demonstrate that the majority of ERCPs in the United States continue to be performed on an inpatient basis as of the end of our study period, and that the trend toward predominantly therapeutic procedures is mirrored. The NIS captures data from non-Federal hospitals, so healthcare systems such as the U.S. Veterans Health Administration are not included. As with other database studies, misclassification of exposure is possible as the data are derived from procedure and outcome codes rather than direct medical chart review. On the other hand, our study is based on a nationally representative sample of all-payer inpatient discharges, and is the first description of national trends in BDS and PTC utilization, as well as the first description of trends in ERCP utilization in more than a decade. It also reports biliary procedural length of stay and fatality statistics, demographic variables, and hospital characteristics for the first time on a national-level.
In conclusion, over a 16-year study period from 1998 to 2013, the sum of all biliary interventions decreased. Although there have been significant declines in the rates of diagnostic ERCP and BDS, therapeutic ERCP utilization has continued to increase. Therapeutic ERCP has appropriately supplanted BDS for the management of choledocholithiasis; one may hypothesize that this is largely true for most biliary surgical indications other than for some forms of bile duct injury and curative resections for biliary tract cancer. The widespread availability of endoscopic expertise, the shorter length of stay, and lower fatality associated with ERCP may be driving these utilization trends, making ERCP the predominant intervention for the management of biliary tract disease in the United States.
Supplementary Material
Acknowledgments
Grant Support: RJH and MTB are supported by NIH Training Grant T32DK007056-40. This research was supported by the Stanford Division of Gastroenterology and Hepatology Divisional Seed Grant.
Glossary
- BDS
Bile duct surgery
- PTC
percutaneous transhepatic cholangiography
- ERCP
endoscopic retrograde cholangiopancreatography
- U.S
United States
- NIS
National Inpatient Sample
- ICD-9-CM
International Classification of Diseases, ninth revision, Clinical Modification
- CT
computed tomography
- MRCP
magnetic resonance cholangiopancreatography
- EUS
endoscopic ultrasound
Footnotes
Disclosures: the authors have no financial, professional, or personal conflicts of interest to disclose.
Author Contribution: NCT, GS, SB were involved in study concept and design; RJH, AM were involved in acquisition of data; RJH, MTB, AC, GS, SS and SB were involved in analysis and interpretation of data; RJH, NCT, MTB, AC, AM, GS, SS and SB were involved in drafting and critical revision of the manuscript for important intellectual content; RJH, NCT, and GS were involved in statistical analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167:752–6. doi: 10.1097/00000658-196805000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogoshi K, Tobita Y, Hara Y. Endoscopic observation of the duodenum and pancreatocholedochography using duodenofiberscope under direct vision. Gastrointestinal Endoscopy. 1970;12:83–96. [Google Scholar]
- 3.Takagi K, Ikeda S, Nakagawa Y, et al. Retrograde pancreatography and cholangiography by fiber duodenoscope. Gastroenterology. 1970;59:445–52. [PubMed] [Google Scholar]
- 4.Kawai K, Akasaka Y, Murakami K, et al. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148–51. doi: 10.1016/s0016-5107(74)73914-1. [DOI] [PubMed] [Google Scholar]
- 5.Cotton PB, Chapman M, Whiteside CG, et al. Duodenoscopic papillotomy and gallstone removal. Br J Surg. 1976;63:709–14. doi: 10.1002/bjs.1800630910. [DOI] [PubMed] [Google Scholar]
- 6.Soehendra N, Reynders-Frederix V. Palliative bile duct drainage - a new endoscopic method of introducing a transpapillary drain. Endoscopy. 1980;12:8–11. doi: 10.1055/s-2007-1021702. [DOI] [PubMed] [Google Scholar]
- 7.Okuda K. Thin needle percutaneous transhepatic cholangiography - historical review. Endoscopy. 1980;12:2–7. doi: 10.1055/s-2007-1021701. [DOI] [PubMed] [Google Scholar]
- 8.Mazen Jamal M, Yoon EJ, Saadi A, et al. Trends in the utilization of endoscopic retrograde cholangiopancreatography (ERCP) in the United States. Am J Gastroenterol. 2007;102:966–75. doi: 10.1111/j.1572-0241.2007.01127.x. [DOI] [PubMed] [Google Scholar]
- 9.Sethi S, Friedland S, Banerjee S. U.S. Survey Assessing Current ERCP-Related Radiation Protection Practices. Gastrointest Endosc. 2015;81:AB352. [Google Scholar]
- 10.Boyle P, Parkin DM. Statistical methods for registries. IARC Sci Publ; 1991. Cancer registration: principles and methods; pp. 126–58. [PubMed] [Google Scholar]
- 11.Bridged-Race Population Estimates, United States. Population by state, county, age, sex, bridged-race, and Hispanic origin. National Center for Health Statistics.: U.S. Census Bureau; 1990–1999, 2000–2009, 2010–2013. [Google Scholar]
- 12.Swahn F, Edlund G, Enochsson L, et al. Ten years of Swedish experience with intraductal electrohydraulic lithotripsy and laser lithotripsy for the treatment of difficult bile duct stones: an effective and safe option for octogenarians. Surg Endosc. 2010;24:1011–6. doi: 10.1007/s00464-009-0716-8. [DOI] [PubMed] [Google Scholar]
- 13.Draganov PV, Evans W, Fazel A, et al. Large size balloon dilation of the ampulla after biliary sphincterotomy can facilitate endoscopic extraction of difficult bile duct stones. J Clin Gastroenterol. 2009;43:782–6. doi: 10.1097/MCG.0b013e31818f50a2. [DOI] [PubMed] [Google Scholar]
- 14.Decker C, Christein JD, Phadnis MA, et al. Biliary metal stents are superior to plastic stents for preoperative biliary decompression in pancreatic cancer. Surg Endosc. 2011;25:2364–7. doi: 10.1007/s00464-010-1552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siddiqui AA, Mehendiratta V, Loren D, et al. Fully covered self-expandable metal stents are effective and safe to treat distal malignant biliary strictures, irrespective of surgical resectability status. J Clin Gastroenterol. 2011;45:824–7. doi: 10.1097/MCG.0b013e318211f96f. [DOI] [PubMed] [Google Scholar]
- 16.Aadam AA, Evans DB, Khan A, et al. Efficacy and safety of self-expandable metal stents for biliary decompression in patients receiving neoadjuvant therapy for pancreatic cancer: a prospective study. Gastrointest Endosc. 2012;76:67–75. doi: 10.1016/j.gie.2012.02.041. [DOI] [PubMed] [Google Scholar]
- 17.Elta GH, Jorgensen J, Coyle WJ. Training in interventional endoscopy: current and future state. Gastroenterology. 2015;148:488–90. doi: 10.1053/j.gastro.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 18.Moffatt DC, Yu BN, Yie W, et al. Trends in utilization of diagnostic and therapeutic ERCP and cholecystectomy over the past 25 years: a population-based study. Gastrointest Endosc. 2014;79:615–22. doi: 10.1016/j.gie.2013.08.028. [DOI] [PubMed] [Google Scholar]
- 19.Varadarajulu S, Kilgore ML, Wilcox CM, et al. Relationship among hospital ERCP volume, length of stay, and technical outcomes. Gastrointest Endosc. 2006;64:338–47. doi: 10.1016/j.gie.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 20.Liao C, Thosani N, Kothari S, et al. Radiation exposure to patients during ERCP is significantly higher with low-volume endoscopists. Gastrointest Endosc. 2015;81:391–8. e1. doi: 10.1016/j.gie.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Scheiman JM, Carlos RC, Barnett JL, et al. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? A prospective trial and cost analysis. Am J Gastroenterol. 2001;96:2900–4. doi: 10.1111/j.1572-0241.2001.04245.x. [DOI] [PubMed] [Google Scholar]
- 22.ASGE Standards of Practice Committee. Maple JT, Ben-Menachem T, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71:1–9. doi: 10.1016/j.gie.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 23.Garcarek J, Kurcz J, Guzinski M, et al. Ten years single center experience in percutaneous transhepatic decompression of biliary tree in patients with malignant obstructive jaundice. Adv Clin Exp Med. 2012;21:621–32. [PubMed] [Google Scholar]
- 24.Sheridan WG, Williams HO, Lewis MH. Morbidity and mortality of common bile duct exploration. Br J Surg. 1987;74:1095–9. doi: 10.1002/bjs.1800741208. [DOI] [PubMed] [Google Scholar]
- 25.Healthcare Cost and Utilization Project. 2011. Rockville, MD: Agency for Healthcare Research and Quality; 2011. HCUP FACTS AND FIGURES: STATISTICS ON HOSPITAL BASED CARE IN THE UNITED STATES, 2009. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.