Abstract
BACKGROUND:
Atrial fibrillation (AF) is the most common arrhythmia treated in the emergency department (ED), with primary electrical cardioversion (PEC) the preferred method of rhythm control. Anecdotally, patients undergoing ED procedural sedation (EDPS) for PEC differ from those requiring EDPS for other procedures: they are at higher risk of adverse events, and require fewer drugs and lower doses. We attempt to verify this using an EDPS registry at a Canadian, tertiary care teaching hospital.
METHODS:
This is a retrospective review of patients that underwent EDPS for the period of June 2006 to September 2014. We compared demographics, medication use and intra-procedural adverse events between those receiving EDPS for PEC for AF compared to that for other indications. We report the asssociation between AEs and predictors using logistic regression.
RESULTS:
A total of 4 867 patients were included, 714 for PEC for AF and 4 153 for other indications. PEC patients were more likely male (58.5% vs. 47.1%), older (59.5 years vs. 48.1 years), and less likely to be ASA I (46.6% vs. 69.0%). PEC patients received smaller doses of propofol and less likely to receive adjuvant analgesic therapy (11.5% vs. 78.2%). PEC patients were more likely to experience hypotension (27.6% vs. 16.5%) but respiratory AEs (apnea, hypoxia and airway intervention) were not different.
CONCLUSION:
EDPS for PEC differs from that conducted for other purposes: patients tend to be less healthy, receive smaller doses of medication and more likely to suffer hypotension without an increase in respiratory AEs. These factors should be considered when performing EDPS.
KEY WORDS: Procedural sedation, Atrial fibrillation, Electrical cardioversion
INTRODUCTION
Atrial Fibrillation (AF) is the most common arrhythmia treated in the emergency department (ED).[1] Recent years have seen a move toward primary electrical cardioversion (PEC) of the condition in the ED, fuelled by both recognition of the limitations of chemical cardioversion and increased comfort and expertise in emergency department procedural sedation (EDPS).[1] PEC has been found to be both safe and effective,[1–4] and the approach has been supported by the 2010 Canadian Cardiovascular Society AF clinical practice guidelines.[5] In June 2006, the ED in the Halifax Infirmary developed an EDPS registry in which all patients undergoing EDPS are prospectively registered for the purposes of quality improvement.
At the Charles V. Keating Emergency and Trauma Centre, approximately 1 000 EDPS are performed annually. The proportion of all procedural sedations for PEC has increased from 6% in 2006 to 19.3% in 2014. In a study from the University of Alberta, 30.5% of 177 EDPSs were for PEC.[6] While PEC is the preferred method of treatment for acute AF by emergency physicians in our academic department, this trend is not universal across Canada. One group of investigators found a high degree of variation in management approaches for recent-onset AF in academic hospital EDs. Specifically, they found that the incidence of primary cardioversion in eligible patients varied from 7% to 69% in the hospitals studied,[7] and it does appear that nationally much debate remains regarding the optimal treatment of the condition.[8,9] The primary issues of debate include whether rate or rhythm control is a better strategy, and if so, whether this varies in different subsets of patients, and whether primary cardioversion should be the principle treatment modality in patients with a low risk of stroke. One glaring omission in the debate regarding primary cardioversion is any reference to the optimal way in which sedation to facilitate the PEC should be performed.
EDPS requires specific expertise and carries the risk of significant adverse events if not performed with attention to the proper patient selection, medication administration, appropriate monitoring and the skill set to rescue patients from unintended over-sedation. Propofol, a short acting anaesthetic agent, is the most commonly used medication for EDPS. Although it can cause hypotension and respiratory depression, propofol has been extensively studied in the ED setting and has been shown to be both safe and efficacious.[9] However, special care must be used when propofol is administered to patients with underlying cardio-respiratory disease who concurrently have an acute arrhythmia. PEC is an unpleasant, although very brief procedure in the vast majority of cases. It would be expected that EDPS for PEC should require a shorter procedure time and lower doses of sedative or analgesic compared to EDPS for other emergency conditions, which are generally longer in duration and involve more painful stimulation of the patients. In a previous study to evaluate the safety of propofol for EDPS, a majority of patients received solely propofol, with 16.8% of patients receiving fentanyl, with no patient in the study suffering an adverse outcome.[9] Anecdotally, our experienced sedationists have observed that cardioversion for EDPS can be conducted with fewer drugs and lower doses than those for other patients requiring EDPS. This observation, however, needs to be verified objectively.
Interestingly a review calling for “guidelines-to-bench approach to research” to “allow for the development of important, clinically relevant new knowledge with impacts on patient management and future AF guidelines”[10] fails to address the issue of how best to manage the sedation required to facilitate the PEC, a point arguably of as much, if not more, importance to emergency physicians who are considering whether to add PEC to their practice.
At the Charles V. Keating Emergency and Trauma Centre, EDPS is performed by specially trained Advanced Care Paramedics.[11] The EDPS program follows a very stringent protocol[12] and the clinical details of every EDPS are recorded on a specific patient care record (Figure 1). The physician responsible for the patient determines whether they can tolerate the procedure. The choice of sedative and analgesia is generally left at the discretion of the paramedic, although the attending physician can modify this decision. Anecdotally, such modification is rare at our institution. A registry for the purpose of continuous quality improvement is maintained and regularly reviewed to ensure patient safety and appropriate care. This registry provides an ideal opportunity to compare EDPS conducted for PEC to those performed for other reasons. Recognizing that the majority of EDPS is conducted on younger, healthy patients with many for orthopedic manipulations, we hypothesize that that practitioners skilled in EDPS for more traditional reasons may be less well prepared to safely conduct EDPS in patients requiring PEC. Retrospectively examining EDPS records in both groups may allow us to identify features to bear in mind for practitioners expanding their practice into this area.
Figure 1.
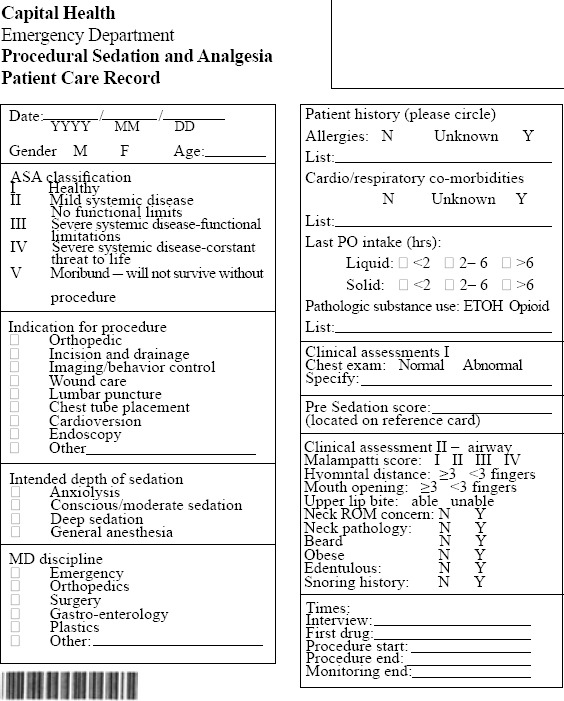
Data collection tool.
The objective of our study was to determine if there are important differences in patient characteristics and clinical outcomes in patients receiving EDPS using propofol for PEC compared to those receiving EDPS using propofol for other indications.
METHODS
This retrospective study examined the EDPS records of 4 867 patients treated at the Charles V. Keating Emergency and Trauma Centre, a tertiary-care, academic teaching center in Halifax, Nova Scotia with an annual ED census of 70 000 visits. The Halifax EDPS registry has been previously described but in short all EDPS are prospectively captured and for this study the period of review was June 2006 to September 2014.[11–13] The data are inputted by an administrative assistant, and one of the co-authors regularly runs database queries to detect input errors and missing data for the purpose of reconciliation. All data were abstracted from the registry, a Microsoft Access database created specifically for the purpose of managing the quality of EDPS. We analysed only patients who received exclusively propofol with or without fentanyl. We did this because these drugs are used in the majority of the PSAs at our institution[13] and to reduce pharmacological bias where other medications were used. There is no specific protocol for drug dosing for PEC or any other indication for EDPS at our institution, so these data represent our current practice in ED.
Patients were divided into two groups, those that received EDPS for PEC and those that received EDPS for other indications (orthopedic manipulation, incision and drainage [I&D], imaging/behaviour control, wound care, lumbar puncture, chest tube placement). Patient characteristics examined included age, gender and American Society of Anesthesiologists (ASA) physical status. Doses of medication (propofol and fentanyl) were also compared.
Adverse outcomes examined included hypotension, hypoxia, apnea and need for airway intervention. Hypotension was defined as any systolic blood pressure (SBP) <100 mmHg, or a 15% decrease from baseline if initial SBP was less than 100 mmHg. Hypoxia was defined as an oxygen saturation as measured by pulse oximetry <90%. Apnea was defined as the cessation of respiration for a period lasting >30 seconds. Airway intervention included the need for an oropharyngeal airway, non-invasive positive pressure ventilation, tracheal intubation or an airway maneuver (e.g., jaw thrust) in the peri-, intra- and post-procedure period. To assess for the association of procedure type (PEC versus all other procedures) with the above outcomes, we utilized a logistic model. We report the crude estimates of the odds ratio (OR), and the estimate of the OR adjusted for patient gender, age, ASA physical status, and propofol and fentanyl dose. We also evaluated patient opinion of the procedure to assess for tolerability of the interventions.
To validate the above models, we reported the P value of the Le Cessie-van Houwelingen test,[14,15] and assessed for the effect of collinearity using the variance inflation factors (VIFs). A VIF of greater than five was considered a priori an unacceptable level of dependency between the candidate predictors. All analyses are performed using R (v3.1.3, “Smooth Sidewalk”) in the RStudio GUI (v.0.98.1103). The study was approved by the Capital Health Ethics Review Board.
RESULTS
A total of 4 867 patients were included in our study dataset. We excluded 340 patients due to them receiving a sedative that was not propofol. Patient demographics are outlined in Table 1. Patients in the PEC group were more likely to be older, male and less likely to be assessed as an ASA I than the comparator group. The PEC group also tended to have received lower doses of both propofol and fentanyl, or received no analgesia.
Table 1.
Patient demographics
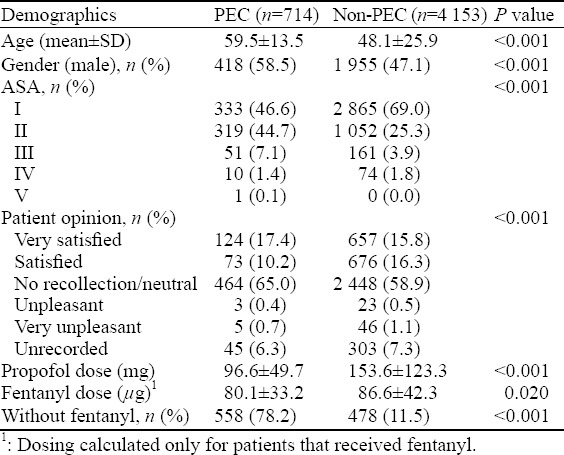
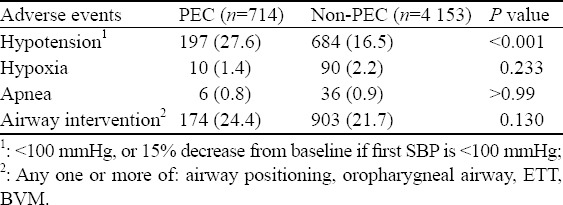
Table 2 outlines the rate of adverse events during EDPS. More patients in the PEC group experienced hypotension (27.6% vs. 16.5%, P<0.001); however, there were no statistically significant differences in hypoxia, apnea and need for airway interventions between the two groups.
Table 2.
Adverse events during emergency department procedural sedation, n (%)
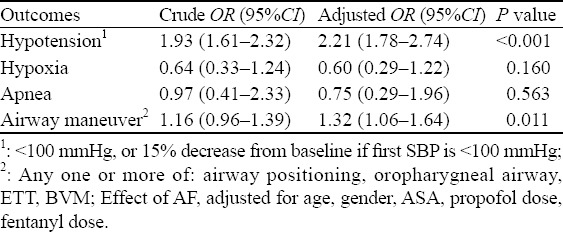
Logistic regression models assessing the association of the outcomes with PEC showed that patients in the PEC group were more than twice as likely to experience hypotension as the non-PEC group (OR=2.21; 95%CI 1.78–2.74), and were 32% more likely to require an airway intervention as the non-PEC group (OR=1.32; 95%CI 1.06–1.64). Although point estimates indicate that hypoxia and apnea were less likely to occur in the PEC group, these differences did not reach statistical significance (Table 3).
Table 3.
Logistic regression results
There were no deaths in the ED associated with EDPS, and no patients received tracheal intubation, or were admitted as a complication of the procedure. No vasopressor agents were used in any patients. All Hosmer-Le Cessie tests were non-significant, indicating an adequate fit of the linear models, and all VIFs were less than 1.5 for all predictors, indicating no overwhelming problems with variance inflation from collinearity.
DISCUSSION
The use of PEC for AF in patients at low risk for embolic complications (those with <48 hours of AF, or on therapeutic anticoagulation regimens) is rapidly becoming standard of care in the ED.[1] While EDPS has been standard of care for many years, it is a process of care that requires specific skill and knowledge. Experience gained performing EDPS on young patients with orthopedic or infectious indications may not be transferrable to patients with a new cardiac arrhythmia. Our data suggests that, although outcomes in both groups were favorable, patients in the PEC group had a lower baseline level of health (as measure by ASA categories) and were more likely to suffer hypotension and to receive airway manipulation, even though they received lower doses of medication and fewer received opioids in combination with the sedative.
Adverse effects of propofol are recognized as being more common with larger doses of the drug, when adjuvant opioids are used, and in patients with a lower baseline level of health.[9] Our findings of lower propofol and fentanyl doses and of more cases done without opioids suggest that the sedationists recognized the increased potential for adverse events in the PEC group and adjusted accordingly, mitigating, although not completely, a large increase in hypotension.
Another explanation for the lower doses or non-use of analgesics is that PEC is a rapid and (compared to fracture reduction) less painful procedure, and that the need for opioids is considered less. The increase in airway interventions without an increased incidence of hypoxia or apnea suggests a greater level of vigilance with respect to respiratory monitoring. We were not able to ascertain whether this was because patients in the PEC group were recognized as being potentially at greater risk for EDPS or because they had higher baseline ASA physical status.
Limitations
This study is a retrospective examination of registry data, and thus carries many of the limitations of retrospective research, especially the fact that the two groups are not randomized and several unmeasured variables may have contributed to differences in practice aside from the indication for EDPS. Although we were not able to find any adverse events that led to sedation related morbidity, the registry does not capture whether the procedure which required EDPS was successfully completed. One limitation of our study is that many patients undergoing EDPS may be under-treated for chronic hypertension, especially in the PEC group. A higher SBP than our chosen threshold may represent clinically relevant hypoperfusion to the vital organs in these patients. As such, our estimates are likely a minimum estimate of the true proportion of hypotension in both groups.
Additionally, our study represents a single centre, that utilizes specially trained paramedics to administer EDPS. This may affect the external validity of the study. Future research should focus on the balance between sedating to successfully complete the procedure and the risk of adverse events during said procedure.
CONCLUSION
EDPS for PEC is generally safe and well tolerated. It does, however differ from that done for other indications in that patients have a lower baseline level of health, and are more likely to suffer hypotension during the procedure. It appears that PEC patients are given lower doses of medications, are less likely to receive combinations of sedatives and analgesics and are more likely to receive airway interventions, although they do not have a higher rate of hypoxia or apnea. Practitioners should be aware of these differences when considering adding EDPS for PEC to their practice.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Capital Health Ethics Review Board.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Butler M proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
REFERENCES
- 1.Stiell IG, Clement CM, Perry JJ, Vaillancourt C, Symington C, Dickinson G, et al. Association of the Ottawa Aggressive Protocol with rapid discharge of emergency department patients with recent-onset atrial fibrillation or flutter. CJEM. 2010;12(3):181–91. doi: 10.1017/s1481803500012227. [DOI] [PubMed] [Google Scholar]
- 2.Burton JH, Vinson DR, Drummond K, Strout TD, Thode HC, McInturff JJ. Electrical cardioversion of emergency department patients with atrial fibrillation. Ann Emerg Med. 2004;44(1):20–30. doi: 10.1016/j.annemergmed.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 3.Michael JA, Stiell IG, Agarwal S, Mandavia DP. Cardioversion of paroxysmal atrial fibrillation in the emergency department. Ann Emerg Med. 1999;33(4):379–87. doi: 10.1016/s0196-0644(99)70300-8. [DOI] [PubMed] [Google Scholar]
- 4.Xavier Scheuermeyer F, Grafstein E, Stenstrom R, Innes G, Poureslami I, Sighary M. Thirty-day outcomes of emergency department patients undergoing electrical cardioversion for atrial fibrillation or flutter. Acad Emerg Med. 2010;17(4):408–15. doi: 10.1111/j.1553-2712.2010.00697.x. [DOI] [PubMed] [Google Scholar]
- 5.Stiell IG, Macle L. Canadian Cardiovascular Society atrial fibrillation guidelines 2010:management of recent-onset atrial fibrillation and flutter in the emergency department. Can J Cardiol. 2011;27(1):38–46. doi: 10.1016/j.cjca.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Bawden J, Villa-Roel C, Singh M, Fabris G, Bond K, Boyko D, et al. Procedural sedation and analgesia in a Canadian ED:a time-in-motion study. Acad Emerg Med. 2010;29(9):1083–8. doi: 10.1016/j.ajem.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 7.Stiell IG, Clement CM, Brison RJ, Rowe BH, Borgundvaag B, Langhan T, et al. Variation in management of recent-onset atrial fibrillation and flutter among academic hospital emergency departments. Ann Emerg Med. 2011;57(1):13–21. doi: 10.1016/j.annemergmed.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Murray S, Lazure P, Pullen C, Maltais P, Dorian P. Atrial fibrillation care:challenges in clinical practice and educational needs assessment. Can J Cardiol. 2011;27(1):98–104. doi: 10.1016/j.cjca.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Campbell SG, Magee KD, Zed PJ, Froese P, Etsell G, LaPierre A, et al. End-tidal capnometry during emergency department procedural sedation and analgesia:a randomized, controlled study. World J Emerg Med. 2016;7(1):13–8. doi: 10.5847/wjem.j.1920-8642.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stanley N. From guidelines to bench:implications of unresolved clinical issues for basic investigations of atrial fibrillation mechanisms. Can J Cardiol. 2011;27(1):19–26. doi: 10.1016/j.cjca.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Campbell SG, Petrie DA, MacKinley P, Froese P, Etsell G, Warren DA, et al. Procedural sedation and analgesia facilitator -expanded scope role for paramedics in the Emergency Department. [accessed Mar 2015];Journal of Emergency Primary Health Care. 6(3) http://pandora.nla.gov.au/pan/37708/20091028-0000/www.jephc.com/full_articlecd6f.html?content_id=486 . [Google Scholar]
- 12.Campbell SG, Magee KD, Kovacs GJ, Petrie DA, Tallon JM, McKinley R, et al. Procedural sedation and analgesia in a Canadian adult tertiary care emergency department:a case series. CJEM. 2006;8(2):85–93. doi: 10.1017/s148180350001352x. [DOI] [PubMed] [Google Scholar]
- 13.Campbell SG, Froese P, Butler M, Etsell GR, Lapierre A, MacKinley R, et al. Propofol is officially the ’sedative of choice’in Halifax!An update from the Halifax ED Procedural Sedation registry. CJEM. 2013;(S15) [Google Scholar]
- 14.Le Cessie S, van Houwelingen J. A goodness-of-fit test for binary regression models, based on smoothing methods. Biometrics. 1991:1267–82. [Google Scholar]
- 15.Rahman NHNA, Hashim A. The use of propofol for procedural sedation and analgesia in the emergency department:a comparison with midazolam. Emerg Med J. 2001;28:861–5. doi: 10.1136/emj.2009.085019. [DOI] [PubMed] [Google Scholar]


