Abstract
BACKGROUND:
Timely identification of high blood lactate levels in septic patients may allow faster detection of those patients requiring immediate resuscitation. Point-of-care (POC) testing is being increasingly utilized in the emergency department (ED). We examined the accuracy and time-saving effect of a handheld POC lactate device for the measurement of fingertip and whole blood lactate as compared with reference laboratory blood testing in septic ED patients.
METHODS:
A convenience sample of adult ED patients receiving serum lactate testing were enrolled prospectively in the ED of a multidisciplinary tertiary care hospital serving the population of one of the major cities of Pakistan. Participants underwent fingertip POC lactate measurement with a portable device simultaneous whole blood sampling for analysis by both the POC lactate device and standard laboratory method. Lactate measurements were compared by intraclass correlation (ICC) and Bland and Altman plots.
RESULTS:
Forty-three septic patients were included in the study. The fingertip POC & whole blood POC lactate measurements each correlated tightly with the reference method (ICC=0.93 & ICC=0.92, respectively). Similarly at 6 hours, the fingertip POC & whole blood POC lactate measurements demonstrated satisfactory correlation with the reference method (ICC=0.95 & ICC=0.97, respectively).
CONCLUSION:
Fingertip POC lactate measurement is an accurate method to determine lactate levels in septic ED patients.
KEY WORDS: Sepsis, Point of care, Lactate, Emergency department, Pakistan
INTRODUCTION
Sepsis and septic shock are common medical conditions associated with significant morbidity, mortality, and healthcare expense.[1] Despite the use of abundant healthcare resources worldwide, severe sepsis and septic shock have a mortality rate of 10%–30%, and 30%–50%, respectively.[2,3] Estimates include 60%–80% of deaths in low- to middle-income countries (LMICs).[4] Sepsis is a time-sensitive condition amenable to early intervention. Serum lactate level obtained in the emergency department (ED) is predictive of mortality among patients with suspected infection and can be used to guide early resuscitation via serial measurement.[5–8] International consensus-based guidelines on sepsis recommend that serum lactate measurement be available with a rapid turnaround time (“within minutes”) to help identify patients with tissue hypo-perfusion who are at an increased risk of morbidity and mortality.[9] Early recognition of elevated lactate levels in sepsis may hasten identification of patients eligible for aggressive resuscitation.[10]
There are numerous hindrances to the early detection of lactate levels in the ED due to prolonged ED waiting time, increased patient volume and delays due to limitations of traditional laboratory analysis[11] Test results may therefore take hours to return and must be actively sought out by the clinician. The gold standard for the determination of lactate is the laboratory gold-standard enzymatic colorimetric assay method. Point-of-care (POC) devices have recently been implemented in a wide variety of settings, from veterinary studies to humans, from ED triage to the intensive care unit (ICU), to hasten detection of time-sensitive disease states and expedite care.[12–14] Such POC devices do exist for the rapid evaluation of lactate. In an animal study which compared four POC meters in animals, all POC lactate meters demonstrated a sensitivity of 100% and a specificity of 95.7%–98.6% with a cut-off plasma lactate concentration of 4 mmol/L.[12] In LMICs such as Pakistan where the mortality rate of sepsis has been shown to be 23% (95%CI 19%–26%), no study at present, has been performed to evaluate if a POC lactate device is an accurate means to assess lactate levels in the septic patient.[15]
Our research objective was to assess the accuracy of handheld POC device for the measurement of fingertip lactate (as well as blood lactate) when compared with reference laboratory testing in septic patients arriving to the ED.
METHODS
Our study was a prospective cohort conducted at the ED, Aga Khan University Hospital, Karachi, from August 2014 to February 2015. The Aga Khan University Hospital is a 500-bed urban tertiary care hospital with a 45-bed Emergency Department which provides care to 45 000 patients annually. Ethical approval was obtained from the Ethics Review Committee (ERC) at the Aga Khan University Hospital.
We calculated a total sample size of 14 subjects using software NCSS PASS (Power analysis and sample size) version 13.0.6.[16] The sample size was increased to a total of 43 patients for improved validation. We employed purposive sampling strategy. Our inclusion criteria enlisted adult patients more than 18 years of age, presenting to the ED with severe sepsis/septic shock as per the discretion of the treating Emergency Physician such as to require a serum lactate measurement. Severe sepsis and septic shock were defined as per the Surviving Sepsis Campaign.[17] Out of these, patients who refused consent, those who were clinically assessed to have systemic inflammatory response syndrome (SIRS)/sepsis, or those who had a contaminated fingertip or blood from venipuncture were excluded.
Data was collected in phases of 12-hour ED shifts. A pre-formed data collection tool was filled out which included demographic details obtained from the patient or his/her next of kin, as well as clinical data as per the patients’ medical charts. Variables included triage time, working diagnosis formed in the ED, time of blood sampling for lactate analysis, sepsis-related organ failure assessment (SOFA) score calculation,[18] time to antibiotic administration, time to steroid administration, use of vasopressors and mortality outcome at 24 hours of first presentation to the ED. Fingertip (capillary) and venous blood samples were then serially collected for each patient; at the time of enrollment (T0), and then again after six hours of resuscitative measures (T6) in order to calculate the rate of lactate clearance. These values were entered into the data collection tool.
Venous blood samples were obtained as per the discretion of the treating physician following routine ED care protocol. Samples were collected in Gray top tubes (sodium fluoride/potassium oxalate) which were placed in an ice container and immediately sent to the central ED/hospital laboratory. These were then analyzed on Dimension RXL & Advia 1800 (laboratory gold-standard enzymatic colorimetric assay), installed in ED stat lab &/or main lab which is calibrated and maintained according to the manufacture standards. This serum lactate measurement is obtained in approximately 30 minutes and served as the “reference method”.
Point-of-care lactate measurement was performed with a “StatStrip” lactate with a detection range of 0.7–20.0 mmol/L, and a result turnover time of 13 seconds.[19] This POC device requires 0.6 microlitre of whole blood. The device uses single-use test strips containing an enzyme-coated electrode. The machine was calibrated by primary investigator by using a factory-supplied calibration strip, and tested by using a check strip with a known value, every 12 hours while in use. The principal investigators received in-depth training on the use of the POC device from a representative of the manufacturer.
Informed consent was obtained for fingertip POC and blood POC lactate level analysis. Finger-prick was performed with disposable lancet after cleaning with an alcohol swab in order to remove traces of sweat so as to avoid contamination. This capillary blood was then utilized for POC analysis. The venous blood drawn for laboratory reference measurement was also used for POC analysis in order to avoid unnecessary venipuncture.
Data was entered and analyzed by using statistical package version 20 (SPSS v.20). Frequencies and percentages were derived for categorical variables. Means and standard deviations were calculated for normally distributed continuous variables. Skewed continuous variables were reported as median and inter quartile range. Agreement of the POC device with the laboratory reference method was assessed by calculating the intra-class correlation coefficient (ICC), and ICC values greater than 0.9 were considered having excellent agreement. To determine the variability of the POC device, as compared to the reference method, Bland and Altman plots were developed with mean difference and limits of agreement. Fingertip POC and whole blood POC values were each compared with the reference method. The post hoc analysis demonstrated that a sample size of 14 subjects with 6 observations per subject achieves 90% power to detect an intra-class correlation of 0.9 under the alternative hypothesis when the intra-class correlation under the null hypothesis is 0.7 using an F-test with a significance level of 0.05.
RESULTS
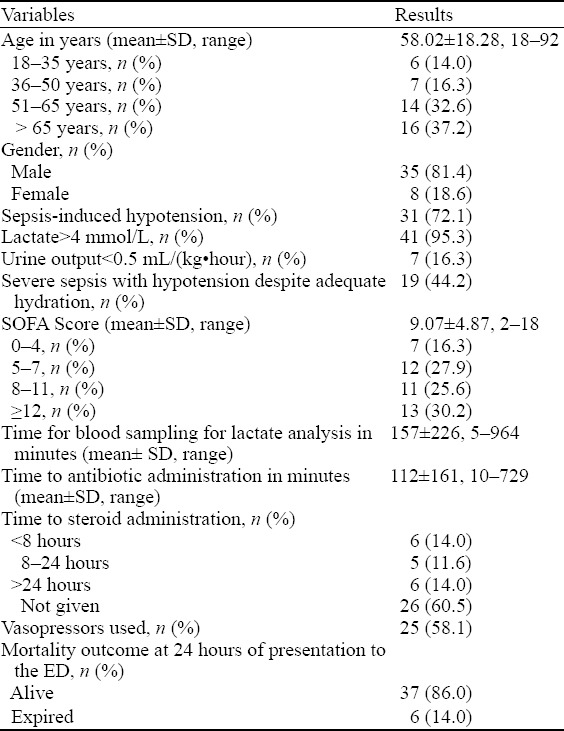
A total of 43 patients consented to be a part of the study. The mean age of population was 58.02 (SD=18.28) years. More than three-quarters were males (n=35, 81.4%). Almost 72% (n=31) of patients presented with septic shock and 58.1% (n=25) patients required vasopressor use. The average time for blood sampling for lactate analysis and antibiotic administration was 157±226 minutes and 112±161 minutes, respectively. Thirty-seven (86%) patients survived at 24 hours of presentation to the ED (Table 1).
Table 1.
Patient demographics (n=43)
At the time of arrival to the ED, fingertip POC lactate measurement correlated strongly with the laboratory reference method at time of arrival (correlation co-efficient =0.93). The Bland and Altman plot demonstrated mean differences of the two measurements, the serum lactate and the fingertip POC within the limits of agreement. Scattered values of the differences were plotted in Figure 1 against the average of the two measurements. The mean difference between serum lactate and fingertip POC lactate was calculated to be –0.32 with 95% confidence interval of mean difference of –2.56 and 1.92 with only 3 outliers falling outside the limits of agreement. It was therefore concluded that agreement is good between both methods (Figure 1).
Figure 1.
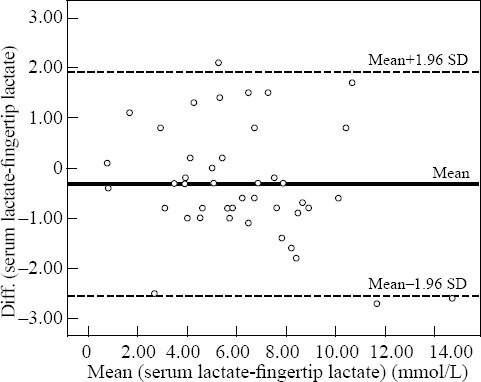
Reference versus fingertip point-of-care (mmol/L). Dotted line represents the mean difference between reference value and POC value. Dashed lines represent limits of agreement (95% confidence interval).
Whole blood POC lactate measurement correlated highly with the reference method, with correlation coefficient (r) of 0.92. The Bland and Altman plot demonstrated a mean difference of 0.2, with limits of agreement between –1.63 and 2.02. In this case, whole blood POC measurements more often measured lower than those measured by the reference laboratory method. Only two values fell outside of the limits of agreement from the upper side. The values scattered equally between the limits of agreement shows no systematic differences between both measurement and an excellent agreement proved for blood POC device and laboratory reference serum lactate (Figure 2).
Figure 2.

Reference versus whole blood point-of-care (mmol/L). Dotted line represents the mean difference between reference value and POC value. Dashed lines represent limits of agreement (95% confidence interval).
At 6 hours after arrival, fingertip POC lactate measurement continued to demonstrate adequate correlation with the laboratory reference method (r=0.97). The Bland and Altman plot demonstrated that fingertip POC measurements were slightly lower (mean difference =–0.34 with limits of agreement between –2.71 and 2.02 with 3 values lying outside the limits of agreement) (Figure 3).
Figure 3.
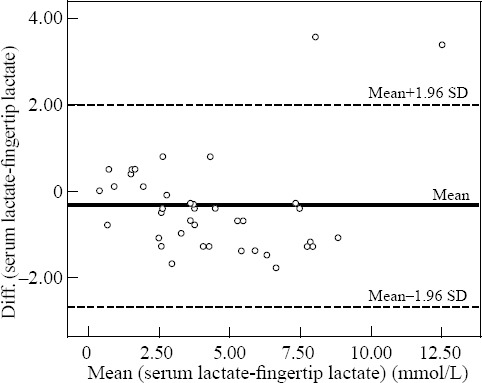
Reference versus fingertip point-of-care (POC) 6 hours after arrival (mmol/L). Dotted line represents the mean difference between reference value and POC value. Dashed lines represent limits of agreement (95% confidence interval).
Similarly, at six hours, whole blood POC lactate measurement also showed a high correlation with the reference method (r=0.95). The Bland and Altman plot showed a mean difference of –0.02, with limits of agreement between –1.55 and 1.50. Only 2 values fell outside of the limits of agreement. The scattered plot suggests variation of at least one method depends strongly on the magnitude of measurements (Figure 4).
Figure 4.

Reference versus whole blood point-of-care (POC) 6 hours after arrival (mmol/L). Dotted line represents the mean difference between reference value and POC value. Dashed lines represent limits of agreement (95% confidence interval).
DISCUSSION
Elevated blood lactate levels are typically present in patients with severe sepsis or septic shock.[1–2] The Surviving Sepsis Guidelines have instituted a protocol for resuscitation of a septic patient which incorporates lactate as a biomarker for the detection and for gauging the effectiveness of therapy.[4,7]
Our study was conducted with the aspect to come up with an alternative method to reduce the time taken to analyze the blood samples for lactate levels for determination of the severity of patient’s medical presentation and take action accordingly. While POC analysis for lactate was available within 12 seconds at the maximum, laboratory reference method via STAT lab still took 30–60 minutes for the results to get back. This study is in concordance with previously available data/studies that handheld POC lactate devices may serve as an effective alternative method of evaluation of blood lactate levels.[10,20–24] A study conducted by Singer et al[24] showed that not only was there a reduction in time to administration of intravenous fluids and antibiotics with a handheld/bedside POC device for lactate measurement, but there was also a reduction in the overall admissions to intensive care units and mortality.
Our study also showed a comparison between the two methods at the time of presentation to the ED and six hours after arrival to assess for effectiveness of resuscitative measures, fingertip/capillary and venous blood POC lactate measurement demonstrated adequate correlation with the laboratory reference method. However, venous blood POC lactate measurement signified a slightly stronger correlation than fingertip/capillary blood. Similar findings were shown by a study conducted by Contenti et al,[25] where the aim was to compare lactate level measurements from arterial, venous and capillary blood samples using a handheld point of care device. They were able to demonstrate that venous blood samples were superior in specificity and sensitivity to capillary and arterial blood samples for lactate levels.
We understand that through our research, this device can serve a swift alternative for detecting the lactate levels in sick patients presenting to the hospital. Low- to middle-income nations have various under resourced hospitals working under limited conditions for providing medical care to patients. If this device were to be used in such setups, it would certainly provide benefit in providing standard and timely care until more definitive treatment can be initiated by transport to more established medical facilities.[26]
Our study has certain limitations. First, the study comprised of a sample size which should be explicitly addressed before the POC lactate device is considered to be used beyond experimental purposes. Secondly, the analysis of results revealed outlier values that need further investigation through a study incorporating a larger sample size than the one we have used. Finally, proper cost effectiveness studies should be conducted in order to assess the economic aspect of POC lactate measurement in sepsis.
CONCLUSION
Our study demonstrates that the fingertip POC method is comparable to the serum method in determining the lactate levels in septic ED patients.
ACKNOWLEDGMENT
We are thankful to NOVA BIOMEDICAL and A.M. Sales and services for providing us with the Point of care “StatStrip” lactate meter for purpose of this study.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Ethical review committee of the Aga Khan University Hospital.
Conflicts of interest: None to declare.
Contributors: Baig MA proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
REFERENCES
- 1.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 2.Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877–87. doi: 10.1056/NEJMoa067373. [DOI] [PubMed] [Google Scholar]
- 3.Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358(2):111–24. doi: 10.1056/NEJMoa071366. [DOI] [PubMed] [Google Scholar]
- 4.Majid H, Sabeen A. Sepsis and septic shock:updates. Pak J Chest Med. 2013;19(2) URL: http://www.pjcm.net/index.php/pjcm/article/view/57 . [Google Scholar]
- 5.Shapiro NI, Howell MD, Talmor D, Nathanson LA, Lisbon A, Wolfe RE, et al. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med. 2005;45(5):524–8. doi: 10.1016/j.annemergmed.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, Shah CV, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37(5):1670–7. doi: 10.1097/CCM.0b013e31819fcf68. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, et al. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32(8):1637–42. doi: 10.1097/01.ccm.0000132904.35713.a7. [DOI] [PubMed] [Google Scholar]
- 8.Marx J, Walls R, Hockberger R. Rosen’s Emergency Medicine-Concepts and Clinical Practice. 8th edition. New york, NY: Saunders; 2013. pp. 1864–74. [Google Scholar]
- 9.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign:international guidelines for management of severe sepsis and septic shock 2008. Crit Care Med. 2008;36(1):296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 10.Gaieski DF, Drumheller BC, Goyal M, Fuchs BD, Shofer FS, Zogby K. Accuracy of handheld point-of-care fingertip lactate measurement in the emergency department. West J Emerg Med. 2013;14(1):58–62. doi: 10.5811/westjem.2011.5.6706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Veelen MJ, van den Brand CL, Reijnen R, van der Linden MC. Effects of a general practitioner cooperative co-located with an emergency department on patient throughput. World J Emerg Med. 2016;7(4):270–3. doi: 10.5847/wjem.j.1920-8642.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karapinar T, Kaynar O, Hayirli A, Kom M. Evaluation of 4 point-of-care units for the determination of blood l-lactate concentration in cattle. J Vet Intern Med. 2013;27(6):1596–603. doi: 10.1111/jvim.12204. [DOI] [PubMed] [Google Scholar]
- 13.Degroote NE, Pieper B. Blood glucose monitoring at triage. J Emerg Nurs. 1993;19(2):131–3. [PubMed] [Google Scholar]
- 14.Slomovitz BM, Lavery RF, Tortella BJ, Siegel JH, Bachl BL, Ciccone A. Validation of a hand-held lactate device in determination of blood lactate in critically injured patients. Crit Care Med. 1998;26(9):1523–8. doi: 10.1097/00003246-199809000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Khan NU, Razzak JA, Alam SM, Ahmad H. Emergency department deaths despite active management:experience from a tertiary care centre in a low-income country. Emerg Med Australas. 2007;19(3):213–7. doi: 10.1111/j.1742-6723.2007.00920.x. [DOI] [PubMed] [Google Scholar]
- 16.NCSS PASS. [Accessed 12th December 2016]. 13 Website: http://www.ncss.com/download/pass. Published 2015.
- 17.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign:international guidelines for management of severe sepsis and septic shock 2012. Crit Care Med. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 18.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 19.StatStrip®Connectivity and StatStrip Xpress Point-of-Care Lactate Analyzers. [Accessed 10th November 2016]. Website: http://www.novabiomedical.com/products/statstrip-lactate/
- 20.Weil MH, Afifi AA. Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock) Circulation. 1970;41(6):989–1001. doi: 10.1161/01.cir.41.6.989. [DOI] [PubMed] [Google Scholar]
- 21.Vincent JL, Dufaye P, Berré J, Leeman M, Degaute JP, Kahn RJ. Serial lactate determinations during circulatory shock. Crit Care Med. 1983;11(6):449–51. doi: 10.1097/00003246-198306000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Shapiro NI, Fisher C, Donnino M, Cataldo L, Tang A, Trzeciak S, et al. The feasibility and accuracy of point-of-care lactate measurement in emergency department patients with suspected infection. J Emerg Med. 2010;39(1):89–94. doi: 10.1016/j.jemermed.2009.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tanner RK, Fuller KL, Ross ML. Evaluation of three portable blood lactate analysers:Lactate Pro, Lactate Scout and Lactate Plus. Eur J Appl Physiol. 2010;109(3):551–9. doi: 10.1007/s00421-010-1379-9. [DOI] [PubMed] [Google Scholar]
- 24.Singer AJ, Taylor M, LeBlanc D, Williams J, Thode HC., Jr ED bedside point-of-care lactate in patients with suspected sepsis is associated with reduced time to iv fluids and mortality. Am J Emerg Med. 2014;32(9):1120–4. doi: 10.1016/j.ajem.2014.06.027. [DOI] [PubMed] [Google Scholar]
- 25.Contenti J, Corraze H, Lemoël F, Levraut J. Effectiveness of arterial, venous, and capillary blood lactate as a sepsis triage tool in ED patients. Am J Emerg Med. 2015;33(2):167–72. doi: 10.1016/j.ajem.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 26.Batra P, Dwivedi AK, Thakur N. Bedside ABG, electrolytes, lactate and procalcitonin in emergency pediatrics. Int J Crit Illn Inj Sci. 2014;4(3):247–52. doi: 10.4103/2229-5151.141467. [DOI] [PMC free article] [PubMed] [Google Scholar]


