Abstract
The osteoid osteoma is a benign primary bone tumor that affects mainly males in the second and third decades of life. Radiographic findings show a radiolucent nidus surrounded by reactive sclerotic bone, particularly in the long bones of the lower extremity. Clinically, it presents persistent pain, which is worse at night and improves with salicylates. It can be a self-limiting injury, with an average duration of three years, but because of pain intensity and intolerance to prolonged use of nonsteroidal anti-inflammatories, surgical treatment is an option. The diagnosis is suspected according to the history and radiographic findings, and the confirmation is made by histological analysis. The traditional surgical treatment is the complete excision of the nidus, but some disadvantages have been described, such as difficulties in localizing the lesion and risk of fracture during the procedure, hospital stay for pain control, and unfavorable esthetic outcome. The authors report a series of cases treated with thermal radiofrequency ablation guided by computed tomography in this service. It is a safe and an effective percutaneous method that aims to cure, minimizing the trauma and morbidity when compared with the conventional block-resection method.
Keywords: Osteoid osteoma, Radiofrequency, Bone neoplasms, Ablation techniques, Computed tomography
Resumo
O osteoma osteoide é um tumor ósseo primário benigno que acomete mais o sexo masculino na segunda e terceira décadas da vida. Radiograficamente, caracteriza-se por um nicho radiolucente cercado por osso esclerótico reativo, principalmente em ossos longos da extremidade inferior. Clinicamente, apresenta uma dor persistente de longa duração, com pioria noturna e melhoria com salicilatos. Embora possa ser uma lesão autolimitada, com duração média de três anos, a ressecção da lesão é uma opção de tratamento devido à intensidade da dor e intolerância ao uso prolongado de anti-inflamatórios não hormonais. Sua suspeita diagnóstica baseia-se principalmente na história clínica e nos achados radiográficos, a confirmação é feita pelo estudo anatomopatológico. O tratamento cirúrgico clássico é a excisão cirúrgica completa do nicho, porém são descritas desvantagens como a dificuldade para a localização intraoperatória da lesão, risco de fratura durante o procedimento, tempo de internação hospitalar para controle álgico e resultado estético desfavorável. Relatamos uma série de casos tratados com termoablação por radiofrequência guiada por tomografia computadorizada em nosso serviço. Trata-se de um método percutâneo seguro e eficaz que tem como objetivo a cura, minimiza o trauma e a morbidade do procedimento, quando comparado com o método convencional de ressecção em bloco.
Palavras-chave: Osteoma osteoide, Radiofrequência, Neoplasias ósseas, Técnicas de ablação, Tomografia computadorizada
Introduction
Osteoid osteoma is a benign primary bone tumor initially reported by Heine1; Bergstrand2 described its histology. In 1935, Jaffe3 classified this neoplasm as a clinical and pathological entity, differentiating it from other tumors.
This is a benign primary neoplasm whose nidus is formed by hypervascularized immature osteoid tissue, surrounded by reactive sclerotic bone. It accounts for 10% of the benign bone tumors4, 5, 6; it mostly affects males, in a ratio ranging from 1.6:1 to 4:1.6, 7 The most prevalent age group is the second to third decades of life.8
Osteoid osteoma can be observed in almost any bone region, but it has a higher incidence in long bones, mainly in the diaphyseal region of the tibia and femur.1, 6
Clinically, it presents with a persistent, long-lasting and vague pain, with nocturnal worsening, that is sometimes relieved with the use of salicylates and non-steroidal anti-inflammatory drugs (NSAIDs).7, 9
Radiographically, it is characterized by the presence of a radiolucent nidus whose diameter rarely exceeds 2 cm,1, 4, 9 often surrounded by reactive sclerotic bone.
The main radiographic differential diagnoses of osteoid osteoma are bone infarction, chronic osteomyelitis, and chondroblastoma.10 Sometimes, complementary imaging tests such as computed tomography (CT) or magnetic resonance imaging can provide a better characterization of the niduse11, 12; bone scan may reveal an intense nidus activity and low activity of the surrounding reactive area.13 The final diagnosis is made through the anatomopathological exam.
Macroscopically, the nidus is well-delimited and wine-colored. Normally, it does not exceed 2 cm in diameter. Microscopically, it is composed of a richly vascularized osteoid matrix and a mature intertwined bone trabeculae; it may also feature areas of central ossification.
Classically, treatment consists of block resection of the nidus. However, intraoperatively, it may be difficult to identify the exact location of the tumor.9 Thus, minimally invasive approaches such as the percutaneous method, aided by imaging methods, override this difficulty.
CT-guided radiofrequency ablation is a percutaneous technique in which the use of electrodes connected to an energy source leads to protein denaturation and coagulative necrosis.14 However, a disadvantage of the method is the lack of material for anatomopathological examination and diagnostic confirmation.
This study aimed to demonstrate the efficacy of the adopted treatment, with satisfactory results in the control of patients with osteoid osteoma.
Material and methods
The authors describe the cases of five patients with diagnostic suspicion of osteoid osteoma who underwent CT-guided radiofrequency thermoablation between September 2010 and March 2013 at this service.
The need for an informed consent was waived, as data was collected through medical records.
Patients reported pain as main complaint; no patient reported a predilection for the night period and all presented failure to respond to drug treatment with salicylates.
Clinical and imaging examinations included conventional radiographs and CT scans to aid in the diagnosis.
Patients included in the study are listed in Table 1; Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5 present the images acquired during the procedure.
Table 1.
List of the patients included in the study.
| Age | Gender | Location | |
|---|---|---|---|
| Case 1 | 16 years | Female | Talus |
| Case 2 | 21 years | Female | Olecranon |
| Case 3 | 38 years | Male | Humerus |
| Case 4 | 38 years | Male | Tibia |
| Case 5 | 20 years | Male | Femur |
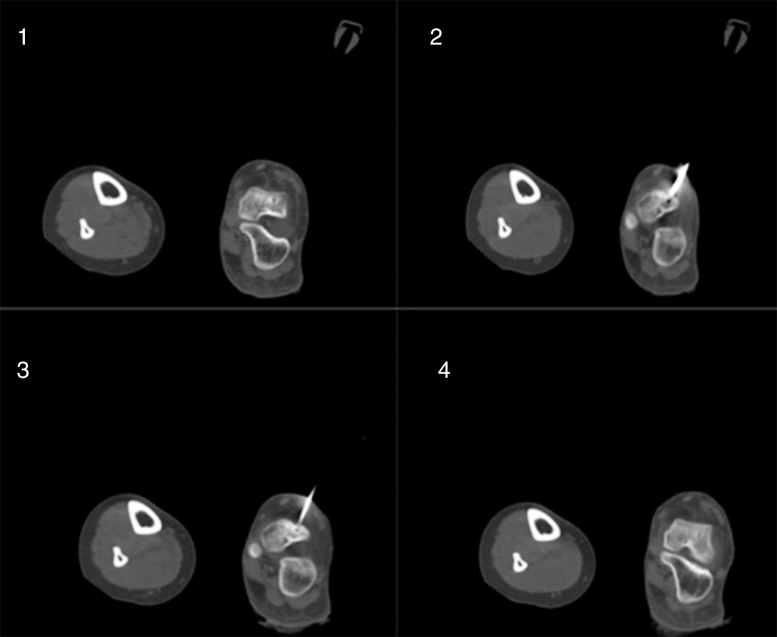
Fig. 1.
(1) Axial CT scan of the left foot, indicating osteolytic lesion with sclerotic halo, located in the domus of the talus, compatible with osteoid osteoma; (2) introduction of the Jamshidi needle through the nidus; (3) positioning of the ablation needle in the path created by the Jamshidi needle; (4) control CT after the procedure. Case 1: B.S.O.C., 16 years, female.
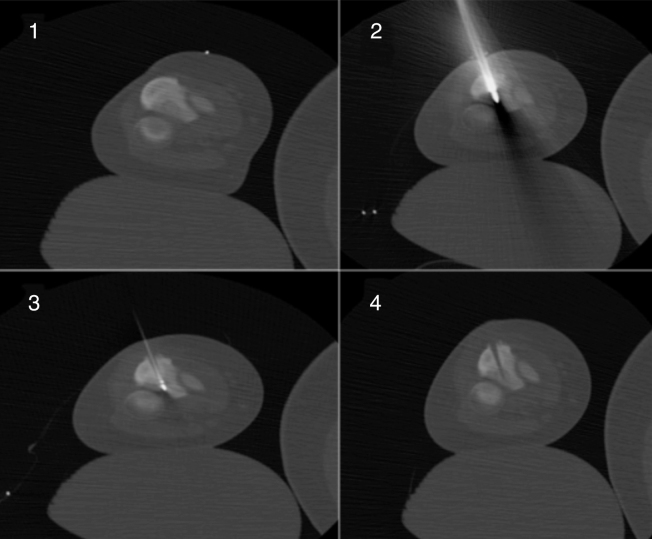
Fig. 2.
(1) Axial CT scan of the left elbow, indicating osteolytic lesion, located in the left olecranon, suggestive of osteoid osteoma; (2) introduction of the Jamshidi needle in the posterior region of the olecranon; (3) introduction of the ablation needle; (4) control CT after the procedure. Case 2: P.P.C., 21 years, female.
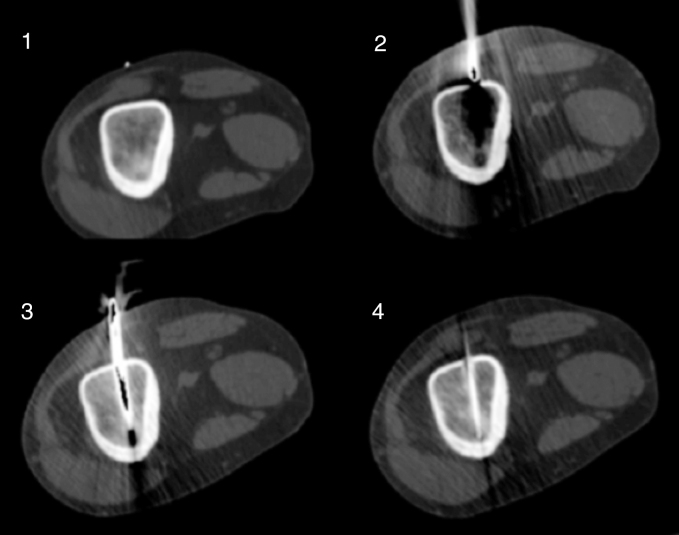
Fig. 3.
(1) Axial CT scan of the right arm showing an osteolytic lesion with sclerotic halo, located in the humerus, associated with cortical thickening, suggestive of osteoid osteoma; (2) beginning of insertion of the Jamshidi needle; (3) Jamshidi needle inserted inside the humerus; (4) CT of the right arm showing the correct positioning of the ablation needle inside the lesion. Case 3: R.M., 38 years, male.
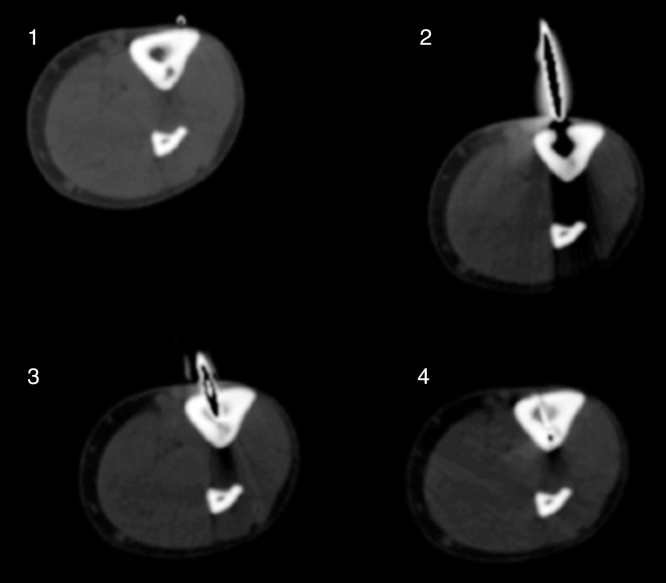
Fig. 4.
(1) CT of the right leg showing a localized osteolytic lesion in the lateral cortex of the tibia; (2) medial positioning of the Jamshidi needle; (3) CT control of the positioning of the Jamshidi needle, immediately before reaching the nidus; (4) tomographic image of the correct positioning of the ablation needle inside the lesion. Case 4: L.A.C.B., 33 years, male.
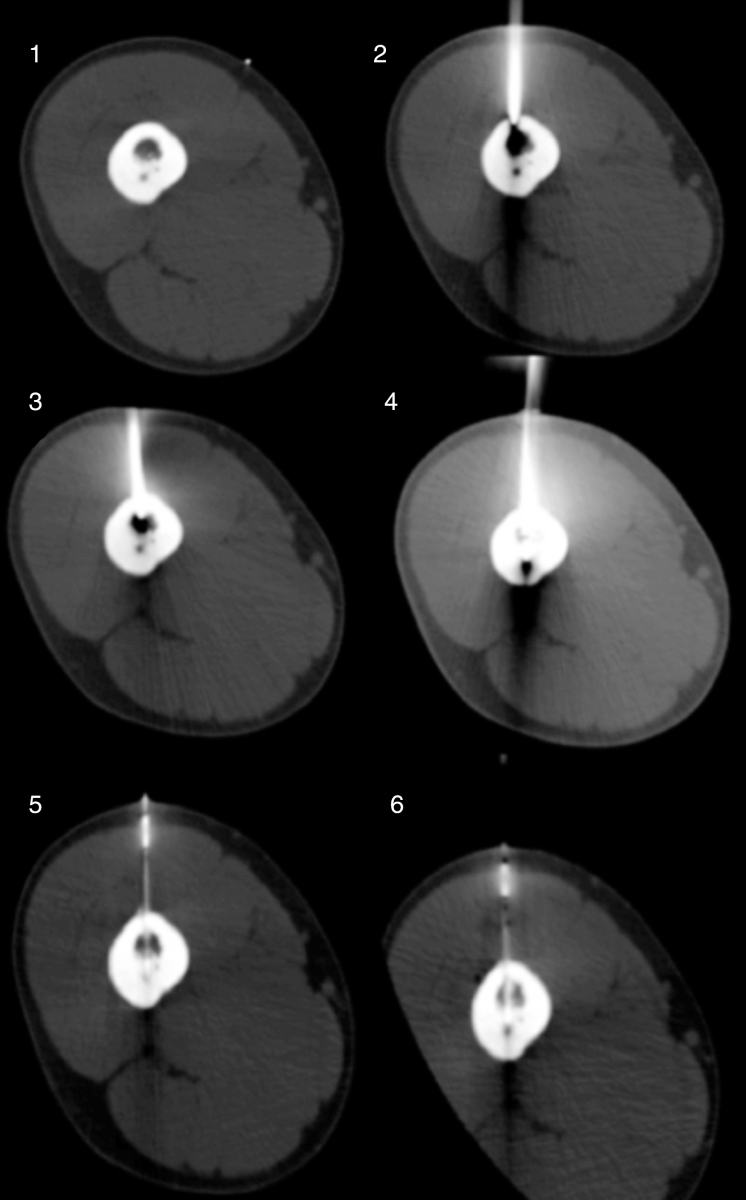
Fig. 5.
(1) Axial CT of the right thigh showing an osteolytic image in the femoral cortex; (2) image showing the Jamshidi needle inside the femoral cortex; (3 and 4) CT control of the path made by the Jamshidi needle; (5 and 6) CT control showing the ablation needle within the nidus. Case 5: D.C.N., 20 years, male.
Procedure technique
Patient is positioned on the CT frame under general anesthesia. Asepsis and antisepsis measures performed for the procedure. CT images are made, identifying the exact location of the nidus, its relationship with adjacent structures, and the best path to its center.
After CT planning, an 8-gauge bone needle (Jamshidi) is inserted into the nidus, thus making the orifice through which the cool-tip single radiofrequency needle, with a 1-cm bone-specific active probe, is passed. After the needle is introduced and its positioning is confirmed through imaging exam, ablation is initiated. The classical initial cycle lasts approximately 12 min, and the maximum temperature of the needle to the end of the procedure is 60 °C. Cooling is provided by 0.9% saline every minute, maintaining the temperature of the active probe below 10 °C. After this first cycle, cold saline circulation is turned off and the second cycle starts. The charring cycle is done without cooling; it lasts 4–6 min and the temperature reaches 80 °C to 90 °C.
Results
Follow-up consisted of clinical and radiographic examinations after the first week of the procedure, as well as after the first, sixth and 12th months of the procedure; after this period, patients were considered to be in remission and told to return yearly. The most important period to evaluate tumor recurrence is within the first 12 months.9 In the ablation treatment, no material for anatomopathological examination was retrieved. No intercurrences were observed during the ablative procedure; patients evolved without radiographic recurrence of the lesion until the present, and with complete resolution of the pain.
Discussion
Osteoid osteoma is a benign bone tumor that usually affects young individuals. It has a typical clinical presentation; in most cases, the pain is intermittent, with nocturnal worsening, and a satisfactory response to salicylates. Its diagnostic suspicion is based mainly on clinical history, physical examination, and radiographic findings.9
The classic treatment requires complete surgical excision of the nidus. The disadvantages of this procedure include the difficulty in locating the intraoperative lesion, even with the use of image-guided Kirschner wires; the need for a new approach when resection is incomplete; the risk of damaging adjacent structures; and the risk of postoperative complications such as unsatisfactory esthetic results and vulnerability to fractures due to the bone defect caused by resection. For this reason, in some cases it is necessary to use synthetic material and bone grafts, which increases the morbidity of the procedure.15, 16
TC-guided radiofrequency thermoablation is a minimally invasive percutaneous technique with low morbidity and high accuracy in locating the lesion. Its possible complications include cellulitis, bleeding, and infection at the site of entry of the needle into the skin. Care must be taken regarding the surrounding structures, such as the nerves; respecting the 1-cm distance limit from these structures to the active probe avoids thermal lesions.14 Theoretically, the main disadvantage of this method is the absence of anatomopathological confirmation of the diagnosis. However, some authors defend that the diagnosis is predominantly clinical and radiographic; histopathological confirmation is not necessary, and its absence does not interfere in the clinical outcome.14, 15, 17, 18
The limitations of this study were the small number of patients and the short follow-up time elapsed from the treatment to the drafting of the present article.
The results obtained in the study are similar to those reported by other authors.14, 15, 16, 19, 20
Conclusion
CT-guided radioablation is an appropriate option for the treatment of osteoid osteoma, presenting good results.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgement
To Cassia da Silva for the help provided in conducting this study.
Footnotes
Study conducted at the Hospital AC Camargo Cancer Center, São Paulo, SP, Brazil.
Referências
- 1.Heine J. Einheilender Knochensequester und der Grundphalanx des Ringfingers. Arch Klin Chir. 1927;146:737–753. [Google Scholar]
- 2.Bergstrand H. Über eine eigenartige, wahrscheinlich bisher nicht beschriebene osteoblastische Krankheit in den langen Knochen der Hand und des Fusses. Acta Radiol. 1930;11(6):596–613. [Google Scholar]
- 3.Jaffe H.L. Osteoid osteoma. A benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg. 1935;31(5):709–728. [Google Scholar]
- 4.Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma. Skeletal Radiol. 1993;22(7):485–500. doi: 10.1007/BF00209095. [DOI] [PubMed] [Google Scholar]
- 5.Busser W.M., Hoogeveen Y.L., Veth R.P., Schreuder H.W., Balguid A., Renema W.K. Percutaneous radiofrequency ablation of osteoid osteomas with use of real-time needle guidance for accurate needle placement: a pilot study. Cardiovasc Intervent Radiol. 2011;34(1):180–183. doi: 10.1007/s00270-010-9950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kransdorf M.J., Stull M.A., Gilkey F.W., Moser R.P., Jr. Osteoid osteoma. Radiographics. 1991;11(4):671–696. doi: 10.1148/radiographics.11.4.1887121. [DOI] [PubMed] [Google Scholar]
- 7.Boscainos P.J., Cousins G.R., Kulshreshtha R., Oliver T.B., Papagelopoulos P.J. Osteoid osteoma. Orthopedics. 2013;36(10):792–800. doi: 10.3928/01477447-20130920-10. [DOI] [PubMed] [Google Scholar]
- 8.Akhlaghpoor S., Aziz Ahari A., Arjmand Shabestari A., Alinaghizadeh M.R. Radiofrequency ablation of osteoid osteoma in atypical locations: a case serie. Clin Orthop Relat Res. 2010;468(7):1963–1970. doi: 10.1007/s11999-010-1265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campanacci M., Ruggieri P., Gasbarrini A., Ferraro A., Campanacci L. Osteoid osteoma direct visual identification and intralesional excision of the nidus with minimal removal of bone. J Bone Joint Surg Br. 1999;81(5):814–820. doi: 10.1302/0301-620x.81b5.9313. [DOI] [PubMed] [Google Scholar]
- 10.Becce F., Theumann N., Rochette A., Larousserie F., Campagna R., Cherix S. Osteoid osteoma and osteoid osteoma-mimicking lesions: biopsy findings, distinctive MDCT features and treatment by radiofrequency ablation. Eur Radiol. 2010;20(10):2439–2446. doi: 10.1007/s00330-010-1811-x. [DOI] [PubMed] [Google Scholar]
- 11.Liu P.T., Kujak J.L., Roberts C.C., de Chadarevian J.P. The vascular groove sign: a new CT finding associated with osteoid osteomas. Am J Roentgenol. 2011;196(1):168–173. doi: 10.2214/AJR.10.4534. [DOI] [PubMed] [Google Scholar]
- 12.Yip P.S., Lam Y.L., Chan M.K., Shu J.S., Lai K.C., So Y.C. Computed tomography-guided percutaneous radiofrequency ablation of osteoid osteoma: local experience. Hong Kong Med J. 2006;12(4):305–309. [PubMed] [Google Scholar]
- 13.Motamedi D., Learch T.J., Ishimitsu D.N., Motamedi K., Katz M.D., Brien E.W. Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiographics. 2009;29(7):2127–2141. doi: 10.1148/rg.297095081. [DOI] [PubMed] [Google Scholar]
- 14.Rosenthal D.I., Hornicek F.J., Torriani M., Gebhardt M.C., Mankin H.J. Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology. 2003;229(1):171–175. doi: 10.1148/radiol.2291021053. [DOI] [PubMed] [Google Scholar]
- 15.Barei D.P., Moreau G., Scarborough M.T., Neel M.D. Percutaneous radiofrequency ablation of osteoid osteoma. Clin Orthop Relat Res. 2000;373:115–124. doi: 10.1097/00003086-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Cantwell C.P., Obyrne J., Eustace S. Current trends in treatment of osteoid osteoma with an emphasis on radiofrequency ablation. Eur Radiol. 2004;14(4):607–617. doi: 10.1007/s00330-003-2171-6. [DOI] [PubMed] [Google Scholar]
- 17.Woertler K., Vestring T., Boettner F., Winkelmann W., Heindel W., Lindner N. Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol. 2001;12(6):717–722. doi: 10.1016/s1051-0443(07)61443-2. [DOI] [PubMed] [Google Scholar]
- 18.Rehnitz C., Sprengel S.D., Lehner B., Ludwig K., Omlor G., Merle C. CT-guided radiofrequency ablation of osteoid osteoma and osteoblastoma: clinical success and long-term follow up in 77 patients. Eur J Radiol. 2012;81(11):3426–3434. doi: 10.1016/j.ejrad.2012.04.037. [DOI] [PubMed] [Google Scholar]
- 19.Lindner N.J., Ozaki T., Roedl R., Gosheger G., Winkelmann W., Wörtler K. Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg Br. 2001;83(3):391–396. doi: 10.1302/0301-620x.83b3.11679. [DOI] [PubMed] [Google Scholar]
- 20.Cribb G.L., Goude W.H., Cool P., Tins B., Cassar-Pullicino V.N., Mangham D.C. Percutaneous radiofrequency thermocoagulation of osteoid osteomas: factors affecting therapeutic outcome. Skeletal Radiol. 2005;34(11):702–706. doi: 10.1007/s00256-005-0947-2. [DOI] [PubMed] [Google Scholar]