Abstract
Imaging studies of the pancreas provide valuable information on the pathophysiology of diabetes and direction of the clinical management. Comparative studies on the imaging and microscopic pathology will be required to validate the importance of the images.

As diabetes is defined by glucose dysmetabolism, pathological investigations on the pancreas in patients with diabetes have mostly been concentrated on the changes of Langerhans islets (endocrine pancreas). In fact, nearly complete loss of β‐cells is usual in autoimmune‐mediated or fulminant type 1 diabetes. Also, in type 2 diabetes, β‐cell mass is reduced to approximately 50% in obese USA patients, 35% in lean USA patients, 40% in Korean patients, 40% in European patients and 30% in Japanese patients. Because pancreatic islets occupy just 2.0–4.0% fractional area of the pancreatic parenchyma, total pancreatic volume is a major determinant of the islet endocrine cell mass. In patients with type 2 diabetes, the remaining total β‐cell mass inversely correlates with glycated hemoglobin and hyperglycemic levels at the time of autopsy. In persons with hemipancreatectomy, insulin secretion is deteriorated with glucose intolerance reflected by insufficiency of β‐cells to compensate for raised glucose. In contrast to the changes of endocrine pancreas, however, not much attention has been paid to the changes in the exocrine pancreas in diabetes patients. In conjunction with the qualitative changes of exocrine pancreas, recent studies have shed light on the importance of pancreatic size in the understanding of the pathophysiology of diabetes1, 2. Pancreas atrophy is found to be a consistent feature in type 1 diabetes patients, and its clinical implication is currently sought. In contrast, although still controversial, investigations have shown that the pancreas size and contour were altered in type 2 diabetes patients. As such, it appears that information of the pancreas volume and structure could potentially be valuable indices for the clinical management and prediction of the prognosis in patients with diabetes.
Recent progress in the technology of pancreatic imaging by computed tomography or magnetic resonance imaging (MRI) has made it feasible to precisely measure the pancreas size (cm3) or volume (mL; Figure 1 ). With both procedures, the average volume of the pancreas was mostly comparable among healthy individuals. However, pancreatic weight obtained at autopsy ranging approximately 70–140 g was not consistent, but mostly larger compared with the values measured by imaging studies1. Pancreas weight is known to increase in parallel with increased body mass index in American healthy controls, and pancreatic weight is increased in obese individuals1. Whether hypertrophic exocrine pancreas or fatty infiltration contributes to the enlargement awaits further investigation. Furthermore, in studies on organ donors with type 1 diabetes, pancreas weight was significantly reduced to the extent of nearly half the size of healthy controls3. In recent imaging studies, type 2 diabetes was also found to accompany a slightly, but significantly, reduced (7–33%) size of the pancreas as well as an irregular outline of the pancreatic border1, 2. Interestingly, Al‐Mrabeh et al.2 investigated the effect of a low‐energy diet for 8 weeks followed by weight maintenance for 6 months on pancreatic imaging. At the end, they divided treated patients into two groups – the diabetes‐reversal group and non‐responders. They found that the pancreas volume was not normalized even after the reversal of diabetes, but the irregularity of the pancreas border was altered after reversal of diabetes. In addition, applied MRI studies, such as proton magnetic resonance spectroscopy or three‐point Dixon's technique, showed the increased pancreatic fat contents in patients with type 2 diabetes2. Furthermore, it was found that subjects with fatty pancreas developed type 2 diabetes during the 5‐year observation period4. Thus these findings underscore the prognostic importance of pancreas morphology in imaging studies in clinical practice, which might benefit patients for better management of diabetes.
Figure 1.
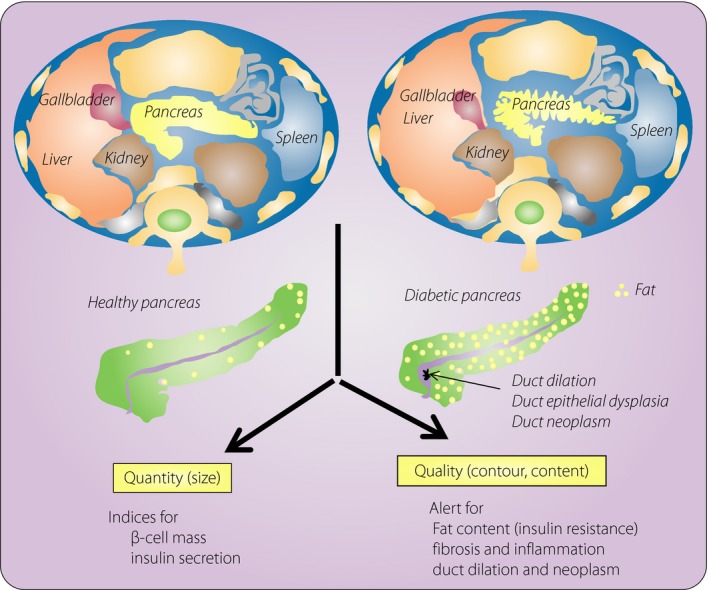
Recent advancements of imaging studies on the pancreas provide new information on the pathophysiology of diabetes and direction for the clinical management of diabetes. With computed tomography or magnetic resonance imaging, the size of the pancreas was found to be smaller in diabetes patients, and its border was irregular. Increased fat content, fibrosis and inflammatory changes were also found in the pancreas of type 2 diabetes patients. In addition, the imaging studies are useful for identifying possible risks for the pancreatic ductal neoplasm.
In contrast to the advancement in the measurement of pancreas size by imaging studies, weighing of the pancreas organ at autopsy has been incomplete. In fact, weighing of the pancreas is not routinely recommended in autopsy rooms, and the data of pancreas weight are missing in many autopsy files. This could be due to the autopsy procedures long historically being carried out using the Rokitansky method, which adopts en mass removal of all viscera; whereas every internal organ is taken in each by Virchow's method, which is nowadays uncommon in Western countries. The problem for the measurement of the pancreas might also be ascribed to the difficulty in separation of the pancreas from the duodenal wall and adjacent soft tissues. Furthermore, the pancreas is surrounded by retroperitoneal fatty tissues, where the pancreatic border of the pancreas is often obscure. For the obtainment of reproducible data on the true weight of the pancreas, it might therefore be essential for pathologists to make efforts to isolate the pancreas organ, and to standardize the method for the dissection of the pancreas from the duodenal wall and retroperitoneal fat pad in the autopsy rooms. Consequently, it will be possible to confirm the validity of the values obtained from imaging studies and autopsy data.
What is then the major factor for altered size and structure in the pancreas in diabetes patients? Currently, in both type 1 and type 2 diabetes patients, the reduction of pancreas size might be accounted for by: (i) lack of insulin action on the exocrine pancreas resulting in tissue atrophy, as insulin is a potent growth factor for the exocrine pancreas (disruption of endocrine and exocrine relationship); (ii) alternately, it might be possible that patients with a small sized pancreas are likely to develop diabetes; (iii) there also emerges a possibility that immune or inflammation‐mediated damage might involve both endocrine and exocrine tissues in diabetes patients, resulting in significant parenchymal atrophy; and (iv) excessive fat infiltration might also result in replacement of acinar tissues in type 2 diabetes patients, with resultant loss of pancreas volume. Unfortunately, as most of the data for pancreas size are cross‐sectional, mechanisms for atrophy still remain speculative. In patients with type 1 diabetes, there is no significant correlation between pancreatic size and the duration of diabetes, implicating the factors other than endocrine pancreas in the pancreatic atrophy3. In this regard, it is of note that duct‐centric lobular atrophy related to obstructive pancreatitis is commonly encountered in slowly‐progressive insulin‐dependent diabetes with markedly reduced pancreas weight5. In a similar manner, pancreatic atrophy is often accompanied by inflammatory changes in type 2 diabetes patients. Such ductal lesions are now found to frequently be associated with dysplastic epithelial lesions; that is, precursor lesions of ductal neoplasms. We might also determine the related genes that influence the pancreatic structure by recently developed single nucleotide polymorphism or genome‐wide associated spectrum.
Detection of fat content in the pancreas on the imaging studies might deserve some comments. In type 2 diabetes patients, fat infiltration in the pancreas, as well as in the liver, is implicated in the insulin resistance and lipotoxicity to the pancreatic islets. Visceral adiposity with inflammatory changes could compose typical pathophysiology encountered in type 2 diabetes patients. Modern MRI is exploited to detect increased fat deposition showing an irregular border of the pancreas rim, a typical sign of diabetes in type 2 diabetes patients2, whereas no difference was detected in type 1 diabetes patients. Thus, it is indicated that the imaging analysis extends from merely the size measurement, but to qualitative evaluation of pancreatic parenchyma. In addition, advances in the imaging studies have shown the frequent presence of pancreatic tumors, such as intraductal neoplasms in patients with diabetes. Scrutinized analysis of MRI or computed tomography images with comparison of pathological findings is urgently required for the future protection of associated tumors in the pancreas or possible overdiagnosis of the images. Apparently, we have gained a new approach for the evaluation of diabetes by imaging studies with high resolution, which we expect will provide a great deal of new information on patients and better clinical management of diabetes.
Disclosure
The author declares no conflict of interest.
References
- 1. Saisho Y, Butler AE, Meier JJ, et al Pancreas volumes in humans from birth to age one hundred taking into account sex, obesity, and presence of type 2 diabetes. Clin Anat 2007; 20: 933–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Al‐Mrabeh A, Hollingsworth KG, Steven S, et al Morphology of the pancreas in type 2 diabetes: effect of weight loss with or without normalization of insulin secretory capacity. Diabetologia 2016; 59: 1753–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Campbell‐Thompson MI, Kaddis JS, Wasserfall C, et al The influence of type 1 diabetes on pancreatic weight. Diabetologia 2016; 59: 217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yamazaki H, Tuboya T, Katanuma A, et al Lack of independent association between fatty pancreas and incidence of type 2 diabetes: 5‐year Japanese cohort study. Diabetes Care 2016; 39: 1677–1683. [DOI] [PubMed] [Google Scholar]
- 5. Kobayashi T, Aida K, Fukui T, et al Pancreatic ductal hyperplasia/dysplasia with obstructive chronic pancreatitis: an association with reduced pancreatic weight in type 1 diabetes. Diabetologia 2016; 59: 865–867. [DOI] [PMC free article] [PubMed] [Google Scholar]


