Abstract
Background
Caring for a child with complex communication needs associated with a developmental condition frequently adds stress to the caregiver. Furthermore, professional assistance is scarce in low-income rural settings. For such children speech is frequently unachievable. Augmentative and alternative communication provides options for supplementing or replacing speech with other techniques. The current study aimed to examine the experiences of caregivers in Kenya before and after a home-based intervention using augmentative and alternative communication techniques with children with complex communication needs.
Methods
Caregivers were interviewed pre- and post-intervention. The interviews were digitally recorded, transcribed and translated into English. Content analysis was applied through the stages of text familiarization and topic organization. Emergent themes and their sub-themes were identified and labelled. Connections between themes were established and interpretations made. The procedure was completed by a second researcher independently. Conflicting ideas were jointly discussed until consensus was achieved.
Results
Four themes emerged from the data: communication process; struggle; normality; and supernatural power. Before intervention, the caregivers acknowledged their expertise in communications with the child, while also revealing their sense of isolation, burden and pain. Normality was present as a source of comparison and also an aspirational goal. Post-intervention more positive language was used to describe the child. There was an ‘opening up’ of communication that recognized the child’s strengths and some social support systems were re-established. The power of the supernatural was recognized before and after intervention.
Conclusion
Caring of a child with complex communication needs presents many challenges. A home-based intervention using augmentative and alternative communication techniques appears to have been a catalyst for some positive transformations in the caregivers’ experiences, although it is not possible to attribute this change to any one aspect. The potentials of the home-based intervention would benefit from further investigation on a larger scale.
Keywords: augmentative and alternative communication, caregiver, communication, experiences, Kenya, rural
Introduction
Caregiving for children with developmental conditions frequently places stress on the primary caregiver. The extensive and continuous support required across the child’s lifespan may impact on family functioning and social relationships (Raina et al. 2004). Evidence suggests long-term caregiving is associated with fatigue, financial difficulties and parenting distress (Hassall et al. 2005; Murphy et al. 2006; Green 2007). Developmental conditions, such as cerebral palsy, cognitive impairment, deafness and autism may be associated with a range of communication impairments that affect individuals of all ages (Enderby 1997). Ambikile and Outwater (2012) reported psychological and physical challenges associated with caregiving of children with a similar range of conditions in Tanzania. The inadequacy of social support systems and the economic challenges of poverty, combined with the extra expenses associated with meeting the child’s needs were a further source of stress (Ambikile & Outwater 2012). Other characteristics of the caregiving experience have been identified such as worry about the future (Murphy et al. 2006), addressing competing demands of daily life (Raina et al. 2005; Ambikile & Outwater 2012), and physical and emotional strain (Hamzat & Mordi 2007). The latter includes coping with the social stigma of caring for such a child (Dunst et al. 2002), which may extend to the child’s condition being viewed as resulting from evil spirits (Hamzat & Mordi 2007; Gona et al. 2011). Most of the research referred to about parents’ experiences is not in the African context, so experiences may be different.
The involvement of caregivers in the main context, in which the child lives, interacts, learns and plays, is considered critical to the success of an intervention (Case 2000; Granlund et al. 2008). For some individuals the nature of their physical, and/or cognitive impairments makes speech an unrealistic target (Wilkinson & Henning 2007). Augmentative and alternative communication (AAC) is a practice whereby spoken communication may be supplemented or replaced by other techniques (Royal College of Speech & Language Therapists 2006). Options for supporting communication typically fall into aided or unaided communication (Beukelman & Mirenda 1992). Aided communication introduces a device outside the communicator’s body (Tonsing et al. 2005). Linguistic ‘utterances’ are represented by graphic symbols, picture board, book or set of objects. Computer-aided communication that provide voice output are used in many high income countries (Alant 2005b), but cost prohibits more global usage. Unaided communication uses the person’s body as a language or a system of sign support for spoken language. Users of aided and non-aided variously employ features of natural communication according to individual capacities, e.g. facial expression, body gesture, eye gaze, vocalization and speech.
The International Society for Augmentative and Alternative Communication (ISAAC) has debated over many years the relevance of AAC to people residing in countries where poverty and human survival are threatened (Alant 2005a,b, 2007). In Africa, the majority of AAC development work has been centred in South Africa looking at cross-cultural readability of graphic symbols (Haupt & Alant 2002; Basson & Alant 2005; Bornman et al. 2009); facilitation of language and literacy (Alant & Moolman 2002); effects of visual characteristics on symbol usage (Alant et al. 2010); and use of communication boards to report crimes (Bornman et al. 2009). Mukhopadhyay and Nwaogu (2009) reported a lack of AAC knowledge and skills among teachers in Botswana. A desire for AAC-based knowledge and specialist training was reported amongst speech therapists in Egypt (Wormnaes & Malek 2004).
The aim of this study was to explore the effects and development potential of a home-based intervention in AAC for children with complex communication needs characterized by little or no speech in a rural part of Kenya.
Research questions
-
1
What are the experiences of the caregivers of children with little or no functional speech?
-
2
What are the experiences of the caregivers when a home-based, AAC intervention is introduced?
Design and methodology
A single case series was conducted. A qualitative methodology was applied before and after a home-based AAC intervention.
Study site
The study was conducted in the Kilifi Health and Demographic Surveillance System (KHDSS) area of the Kenya Medical Research Institute (KEMRI). The KHDSS has as area of 900 km2. It has a population of about 250 000 inhabitants. It is estimated that 8–10% of this population are children with moderate to severe disabilities (KHDSS 2012). It is one of the poorest areas in Kenya. Rehabilitation services comprised occupational therapy, physiotherapy and orthopaedic technology located at the district hospital. There was no speech and language therapy. With regard to education, there were two special schools and five special needs units on mainstream school sites.
Ethics
The study was approved by the Kenya National Ethics and Review Committee (SSC # 1996) and the Ethics Committee for Development at the University of East Anglia.
Sample
Twelve children aged 4–12 years were recruited from the Educational Assessment and Resource Centre (EARC) register of 2000 children. Each child presented with:
Limited or no functional communication, including those with restricted speech and language, and those with severe intelligibility problems.
A recognized condition, including cerebral palsy, cognitive impairment, deafness and autistic spectrum disorder.
In addition, it was required that the children resided with their caregivers most of the time and the caregivers were willing to commit time to the intervention.
Sample recruitment focused on children with complex communication needs associated with a primary diagnosis of cerebral palsy, autistic spectrum disorder, cognitive impairment and deafness. The aim was to recruit at least two children from each diagnostic category to increase the range of likely AAC approaches that would be involved. The head of the EARC selected a total of 32 children out of the 2000 registered who met the inclusion criteria. Using a purposive-convenience sampling procedure, 12 children were recruited representing all four categories of primary condition and with age range from 4–12 years. Age 4 is the age when a typically developing child would usually be considered a competent communicator. There was a balanced ratio of males to females. Two caregivers declined to take part in the study due to family problems leaving a sample of 10 caregivers. A family of a third child (P4) relocated and was subsequently withdrawn from the study. Table 1 provides a summary of the presenting characteristics of the nine children who took part in the study.
Table 1.
Summary of participants’ characteristics
| Participant | Gender | Age* | Health condition | Activity & participation for communication |
|---|---|---|---|---|
| P1 | Male | 11;00 | Cerebral palsy (quadriplegic) and profound intellectual disability. | Unable to walk or sit unsupported. Limited voluntary control of head movement and directional eye gaze. No evidence of verbal comprehension but recognizes basic objects. Reliant on others for interpreting his needs and initiating interaction. Smiles and vocalizes to mother. Does not attend school. |
| P2 | Female | 3;07 | Global developmental delay of unknown aetiology. | Some crawling behaviour and sits on floor unsupported. Parental report of skills loss and regression in social behaviour after first 12 months of typical development. No evidence of verbal comprehension. Stares blankly for long periods of time; poor attention; repetitive behaviours, e.g. hand wringing; attempts to say ‘baba’, and laughs and claps hands to self. Does not attend school. |
| P3 | Male | 6;00 | Cerebral palsy (quadriplegic); epilepsy. | Unable to walk; bottom shuffles on floor; points with left hand-arm to people and objects in the immediate environment. Evidence of verbal comprehension at 2–3 word level. Attempts speech – largely unintelligible due to motor speech problems; relies on familiarity of partner to understand him; clear picture recognition; selects from array of 8 pictures upwards. Attends special needs unit attached to school. |
| P5 | Female | 6;00 | Intellectual disability; poor attention and hyperactivity. | Able to walk; uses hands to pick up things. Verbal comprehension is reliant on situational cues. Engages in activities in self-absorbed way, e.g. hums to self, picks up bits from ground to eat, places hands in sand and flicks leaves on empty meal sack. No speech but attempts communication through gesture; gets frustrated when not understood uses social eye gaze, smiles & laughs; recognizes familiar people. Does not attend school. |
| P6 | Female | 6;00 | Moderate hearing impairment (currently no hearing aids). | Motor skills are unimpaired. Verbal comprehension is approximately at the two-word level but reliant on environmental cues; watches other people’s faces closely; Shows interest in environment and; attempts to copy write letters; has wide range of communicative functions, e.g. expresses needs, comments on events, attempts communication with familiars but has restricted vocabulary. Understood usually by familiar people at homestead. Does not attend school. |
| P7 | Male | 5;06 | Cerebral palsy (quadriplegic); intellectual disability. | Shows desire to communicate; indicates when happy or sad through facial expression; greets people; understands basic instructions, e.g. ‘no’; shows recognition of everyday objects but no concept of pictures. Does not attend school. |
| P8 | Male | 12;00 | Autistic spectrum disorder. | Motor skills are unimpaired. Verbal comprehension appears to be at the 4+ word level. – Fairly self-sufficient in home with reduced need to communicate; likes to take apart objects but does not put them back together understands simple instructions; appears aloof and does not engage socially with others at home. Attends special needs unit attached to school. |
| P9 | Female | 6;00 | Severe intellectual disability – Down syndrome. | Able to walk independently; attempts to hold a pen for ‘pretend writing’. Verbal comprehension at the 1–2 word level with support of situational cues. Parents ignorant of condition initially. Attempts speech but cannot be understood by parents and family; uses gestures to express range of functions, e.g. protest, request, share communicative point, attract attention. Does not attend school. |
| P10 | Female | 6;00 | Cerebral palsy (quadriplegic); global developmental delay – nystagmus noted – vision queried. | Unable to walk; able to reach and grab with right arm-hand. Verbal comprehension at basic situational level. Makes small vocalizations; directional eye gaze but also reaches out to mother; facial expression to communicate likes/dislikes, happy/sad; able to attract attention. Does not attend school. |
The numbers before the semicolon mean ‘years’ and the numbers after the semicolon mean ‘months’.
Methods
Interviews were conducted with the caregiver of each child at two different times: before the intervention; and at the end of a 6-month implementation period. The interviews were conducted at the homestead and focused on the caregiver’s experiences of having a child with complex communication needs, specifically:
Child’s communication with caregiver;
Child’s communication with other people;
Caregiver’s communication with child;
Available support;
Caregiver’s view of the future.
All the interviews were facilitated by the first author, a native user of the local languages (Kiswahili and Giriama). He was unknown to the participants and their families. The interviews were digitally recorded. During the pre-intervention interview, a trained speech & language therapist conducted informal assessments of the children. The local assets of the homestead were recorded using a standard format that was completed with the caregiver and supplemented by observations (Appendix I). This information informed aspects of the intervention, such as the interests of the child, the availability of key family members for communication, the facilities in the home and other people in the neighbourhood. In addition, an adapted version of the Communication Profile, which was developed as an outcome measuring tool in Uganda (Baker & Hartley 1999), was administered. Data arising from the Communication Profile are reported in a second paper currently in preparation.
The intervention
The design and content of each participant’s intervention was based on an ecological view of the developing child in the natural context (Granlund et al. 2008). The completed Communication Profile informed the content of the intervention. The caregiver was viewed as the agent for change, occupying a pivotal role in the implementation of the intervention.
Individual goals were configured around the International Classification of Functioning, Disability and Health for Children and Young People (WHO 2007), a derived version from the ICF that aims to capture the characteristics of the developing child in a changing environment (Granlund et al. 2008). Based on Nakajima’s three maxims, cited by Alant (2005a), the intervention needed to be technically valid, economically feasible, and socially and culturally acceptable. Technical validity was attained by providing in situ training for the main caregiver on how to use the recommended AAC technique with the child. Economic feasibility was upheld by using low-technology options that required neither power supply, nor technical expertise for use and maintenance. Use of local resources helped to keep financial costs low. Social and cultural acceptability was catered for by negotiating the content of the intervention with the main caregiver and using locally sourced materials.
Four main approaches were assigned to the individual participants (Appendix II). Four participants (P1, P5, P7 & P10) used ‘objects of reference’ defined as objects to which particular meanings have been assigned (Park 1995, 1997). Two participants used a ‘total communication’ approach (P6 & P9). Derived from an educational approach for children with hearing impairment (Mayer & Lowenbraun 1990), it emphasizes the flexible use of communication across the range of techniques (Bradshaw 2000). P3 used two ‘communication boards’, pointing at pictorial representations of important people, things and activities. The first board displayed photographs of important people in his life. The second communication board displayed ‘picture communication symbols’ representing core vocabulary items, devised using the software package Board maker (Mayer-Johnson 1981–2008). P8 was introduced to the ‘picture exchange communication system’ (Bondy & Frost 1994). Pictures were cut out of the packaging of food items purchased at the local supermarket and P8 was trained to trade these pictures for things he wanted – emulating requesting behaviour. P2 used sensory-based interaction based on principles of Intensive Interaction (Nind & Hewett 1994), whereby the caregiver follows the child’s behavioural lead, shaping their responses into playful interactions. Figure 1 shows the AAC materials assembled. Intervention plans for each participant are summarized in Table 2. The rationale underpinning each plan was constructed according to the individual’s presentation in terms of body structure and function, activities and participation (WHO 2007).
Figure 1.
Augmentative and alternative communication materials.
Table 2.
Summary of intervention characteristics tailored to individual participants
| Participant | AAC technique | Goals | Operational access (motor skills for communication) | Linguistic content (vocabulary to be targeted) | Materials |
|---|---|---|---|---|---|
| P1 | Objects of reference | To request the thing he wants by responding to a ‘yes’/‘no’ choice when offered either one or a pair of real life objects. | Mother holds up objects either singly or in pairs. P1 uses eye gaze (L–R) to identify preferred object. | ‘Drink’ or ‘no drink’; ‘food’ or ‘no food’; ‘comb hair’ or ‘no comb hair’; ‘wipe face’ or no wipe face’; ‘play’ or ‘no play’. | Box of everyday objects: face cloth; shaker; comb; cup. |
| P2 | Multi-sensory interaction based on principles of Intensive Interaction. | To engage in socially interactive play with mother, father and familiar others at home. | Mother engages in playful interactions with child using multi-sensory material, watches naturally occurring behaviours of child and imitates them. | ‘Mama’(mum) and ‘Baba’(dad) | Multi-sensory objects: cloth; mirror; body lotion; fan. |
| P3 | Pictorial communication board(s) | To communicate basic needs; to tell his family about things that have happened or people he has seen. | Left arm-hand gestural point to pictures displayed on communication board. | Mama, Baba, family members; drink, food, sleep, happy, sad, me, want, like, go, no, yes, school, bed, food, drink, fruit, shop, neighbours. | Two communication boards: 1. photographs of P3 and all the familiar people in his life; 2. line drawings for vocabulary using board maker. |
| P4 | Objects of reference | To communicate basic needs; to engage in socially interactive play with familiar people at home. | Use of eye gaze and giving objects. | Drink; toys; fruit; food. | Box of everyday objects: face cloth; shaker; comb; cup; bowl; mirror. |
| P5 | Objects of reference | To communicate basic needs; to engage in socially interactive play with familiar people. | Use of eye gaze and giving objects. | Food; writing; goat; cow; duck; chicken; water; bicycle; coconut; house; bed; drink. | Box of everyday objects: face cloth; shaker; comb; cup; bowl; mirror. |
| P6 | Total communication | To expand communicative vocabulary; to use a range of expressive functions. | Naming of objects, people and actions in the environment to provide a speech production model for P6 – supported by signs. | Vocabulary used in daily routines, e.g. duck; dog; chicken; goat; cow; water; bicycle; house; washing; food; drink; mobile phone. | Large mirror to provide visual feedback in speech practice. Signs drawn from Kenyan Sign Language. |
| P7 | Objects of reference | To communicate basic needs and simple choices. | Use of left arm-hand to remove objects from board and give to Mama. | Drink (cup); food (bowl); comb; face cloth (bathe); play (shaker toy). | Everyday object board: face cloth; shaker; comb; cup; bowl; mirror. |
| P8 | Graphic symbols (Picture Exchange Communication System) | To communicate basic needs. | Use of hand function for giving and receiving objects. | Drink: juice; milk; crisps; biscuits; banana; apple; mango; biscuit. | Picture tokens: fruit; crisps; juice; milk. |
| P9 | Total communication | To build functional vocabulary to support expressive language. | Use of signs as ramps for speech. | Food; writing; goat; cow; duck; chicken; water; bicycle; coconut; house; bed; drink. | Kenyan sign language; core vocabulary of everyday objects, actions and events. |
| P10 | Objects of reference | To communicate basic needs and to interact socially. | Use of right arm-hand to remove objects from board and give to Mama. | Drink (cup); food (bowl); comb; face cloth (bathe); play (shaker toy); mirror (play). | Everyday object board: face cloth; shaker; comb; cup; bowl; mirror |
AAC, augmentative and alternative communication.
The associated materials were supplied to each caregiver and a demonstration of how to use the materials with the child was given, supported by a verbal explanation. The intervention was carried out for a period of 6 months with one monitoring visit every month, which served as a check on progress and the reassertion of intervention principles.
Data analysis
The digital recording of the interviews were saved to computer and transcribed and translated into English before being imported to NVIVO 7 computer program for storage and management. In order to access the lived experiences of the caregivers, content analysis as described by Taylor-Powell and Renner (2003) was used. First the text was read and re-read for familiarization, with any impressions recorded in note form. Then the data were organized by the topics covered in the interview schedule. Any consistencies and differences were identified across the respondents. In order to bring meaning to the words as defined by the ideas, concepts or terminology expressed by the respondents, a label was assigned to each theme, from which sub-themes were extracted. Connections within and between themes were explicated, before finally interpreting the data. This latter stage involved inspecting the categorized data against the time line of the intervention. A second, independent analysis of the data was conducted to enhance the validity of the research findings. The two analyses were cross-checked and any conflicting ideas jointly discussed until consensus was achieved.
Interpretation of the data used Raina and colleagues’s (2004) theory-based, multidimensional, conceptual model of the caregiving process. The model comprises six interrelated constructs (background and context; child characteristics; caregiver strain/stress; intrapsychic factors; coping factors; and outcomes). Each construct consists of factors that are defined by the causal relationships between them.
Results
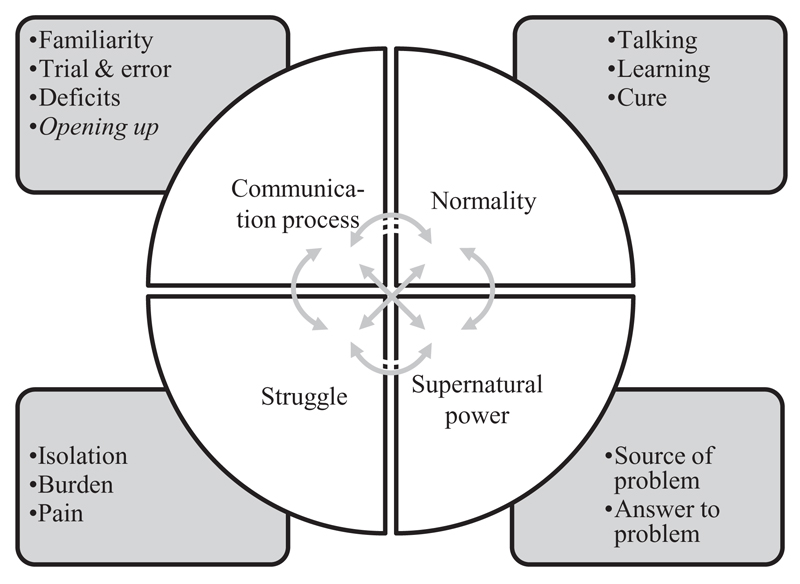
Four main themes emerged from the data: communication process; normality; struggle and supernatural power, as shown in Fig. 2. The bullet point items represent sub-themes. The arrows at the centre of the schematic diagram indicate interconnections between themes. While the themes were observed to cut across the caregiver’s experience before and after the intervention, certain transformations were also noted.
Figure 2.
Schematic diagram of themes and sub-themes.
Communication process
Communication process was characterized by approaches used by the caregivers for communicating with and understanding their children. The first sub-theme was familiarity. The caregivers drew on personal knowledge and experience to interpret the child’s behaviours, which were usually focused on the supply of basic needs.
When she is hungry, she will follow you, lie down, and then you will know that she is hungry. [P9]
Even before the intervention was introduced, the caregivers recognized their pivotal role in respect of the child’s communication. Some of the caregivers articulated real understanding of the unique ways the child communicated.
… when she sees some people on a motorbike falling down she can’t say ‘I saw people on a motorbike falling down’. She will say ‘prrrr’ then signs the action of falling down – then you understand that a person on a motorbike fell down. [P6]
This contrasted with the perceived difficulties of others.
Other people cannot communicate with him. It is I who can communicate with him. [P7]
Communicating specific choices or ideas frequently led the caregivers to a trial and error approach, where different things were tried out with the child and the resultant responses gauged.
But the problem is to know the type of food he will prefer that day. I give this he refuses. I give him this he vomits. So I keep on trying till that food which he will be contented with…. [P7]
The lack of clear communication was noted in the form of perceived impairments observed in the child. This was linked closely to the struggles many expressed.
She can’t talk. I can’t know when she is hungry. [P10]
The fourth sub-theme was termed opening up, which emerged in the post-intervention interviews, capturing new ways of understanding and communicating with the child.
She has now made a big difference. She can now stare at a thing, and when something passes by and it has some sound she looks wanting to know where it comes from. [P2]
The widening of the child’s social horizons was reported by caregivers denoting not only active communication of the child but positive responding by others.
My child is feeling at peace. Even if a visitor arrives you will see him celebrating until they come and greet each other. [P7]
Normality
The theme of normality resonated throughout the caregiver narratives, both pre- and post-intervention. There was a strong desire for the child to develop similarly to age-matched peers in the area of talking.
I want her to be like others. I want her to talk [P2]
Learning was identified as a key to the child’s developmental progression and to later occupation.
I would like him to be able to walk, talk, and learn how to make things using his hands, like sewing shoes, woodwork. [P3]
The hope of a cure was also present in the narratives. Sometimes the sentiment was qualified by particular achievements that were desired for the child, and this usually involved ‘talking’:
… you wake up one morning and you start talking with him and he is able to reply you … [P1]
I want her to get cured. [P5]
A child’s school attendance was considered an essential need by most of the caregivers, which was related to amelioration of the child’s difficulties.
What is remaining is to get full healing and by next year he should be going to school and continue to see good development until he walks. [P7]
Post-intervention view of normality was qualified with a more measured sense of reality.
I have expectations that he will open up because where he comes from is far. [P8]
There was even a sort of rationalization of ‘miracle’ in real terms.
For this exercise it is as if the brain is opening up. The brain opening up is a miracle I had not realised before. [P7]
However, the aspiration of normality also persisted, with speech being the ultimate and desirable outcome.
I expect her to talk and the madness change and be able to understand, … when she is somewhere she can settle and her mind be opened. [P5]
Struggle
The majority of caregivers spoke of their own struggles to bring up their children, which was characterized by feelings of isolation.
…. he was drooling something from the mouth like charcoal, something thick and smelling like somebody who had died three days ago. In fact I could not sit with somebody near me. I used to sit alone. [P7]
After the intervention, there appeared to be a reconnection with other family members.
My husband now gives me support. You changed him. [P5]
Everyone feels happy in giving different forms of support to me and the child. I can’t believe this. [P7]
The sub-theme of burden resonated throughout the narratives. The burden of caring for the children was variously defined as financial:
The money we have used on him is a lot. [P8]
And physical
Carrying the child daily even at school I sometimes tell the teacher I’m tired today. I will bring him tomorrow. [P3]
While the burden of caring had not simply disappeared, post-intervention interviews revealed the construction of some new perspectives of the child.
Sometimes you can see him with other children from here playing and he can be there playing and if it is something funny, he also laughs. [P8]
Many of the caregivers spoke of the pain experienced in relation to their child. Sometimes the realization that the child was different was the catalyst and sometimes the lack of opportunities available.
I feel hurt. This is because she can’t talk, she can’t walk. That’s why I feel my heart burning [P10]
The caregivers expressed the impact of their child’s difficulties as a disturbance to their own well-being.
The condition he is in makes me have no peace. This is because a sickness is not something that can make a person happy [P7]
Post-intervention there was a positive shift in the language used by nearly all the caregivers to describe their own state of well-being.
I feel happy because she is now becoming enlightened. [P6]
The sense of well-being even prompted one caregiver to talk of the support that might be afforded to others in a similar situation.
Even if I see another parent with a child like mine I can tell the parent that there is an organisation that can help a child like this. [P9]
The one exception was the caregiver of P10 who spoke more than any other caregiver of a supernatural power that had determined the fate of herself and her daughter.
I feel she won’t be able (to communicate) because what I was being told by the people who are superstitious [P10]
Supernatural power
Supernatural Power was frequently attributed with not only the source of the child’s condition, but also with providing the potential answer to the problem. It encompassed both cultural beliefs and practices, such as witchcraft, as well as religious observances and convictions. Community beliefs in witchcraft and evil spirits appeared to be associated with sadness and pain, either because of feeling that someone else had been responsible for the child’s disability, or that the caregiver herself was viewed as the cause.
They say she was taken by someone and made a seat for the jinnis (evil spirits) [P10]
I had to move to another church because I was thought to be having ‘jinnis’ (evil spirits). I felt a lot of pain. [P8]
Religious beliefs also appeared to bring some sustenance to the caregivers during difficult times
But If I remember God I have to be grateful. [P3]
Post-intervention, the caregiver perspective appeared to move from a superstitious, causal explanation of the child’s condition, to a newly perceived reality.
I now feel happy and have hope. Do you know that I can now communicate with him? Sometimes our traditions confuse us. [P7]
This did not mean that traditional beliefs had simply disappeared, but that new experiences of the child’s communication occupied an equally important place. However, intervention from high powers was expected by most of the caregivers and was apparent in both the pre- and post-intervention narratives. The hope of a miracle to bring change to the existing situation was expressed both before the intervention.
Though I have gone through difficult times I have faith that one day God will touch him and will be opened and will be able to sit by himself. [P1]
And afterwards:
I am praying God to help…. [P9]
Discussion
Before intervention
Caregiving is a normal part of a parental role, which is traditionally carried out by the mother as reported by Hamzat and Mordi (2007). Having a child with high support needs has the potential to alter ‘the balance between external, environmental demands and the perceived internal ability to respond’ (Raina et al. 2004). Stress occurs when demands start to impact on everyday activities. Individual characteristics of both the caregiver, such as age, marital status and coping ability, and the child, such as the severity of impairment and level of support needs, are potential factors of influence. With the exception of one mother whose husband was deceased, the other caregivers all had husbands. However, the level of support from the husbands in managing the child’s needs appeared to be fairly erratic, with the caregiving demands being managed mainly by the mother. This resonates findings by Green (2007), Murphy and colleagues (2006), and Hassall and colleagues (2005). Tensions between delivering care to the child while also carrying out other occupational roles in the home have been referred to as ‘caregiver strain’ by Raina and colleagues (2004).
While the children had a range of conditions that variously affected motor, cognitive and social development, they had complex communication needs in common. Although pre-intervention, the caregivers’ narratives revealed their natural expertise in understanding the behaviours of their children, the additional responsibility of deciphering meanings and the noted lack of understanding by others may have represented a further difficulty. Although not reported in detail, this is inferred in Ambikile and Outwater’s (2012) report of communication problems contributing to the emotional strain experienced by parents. Not surprisingly, the self-perception of the caregiver, together with stress management have been identified as direct predictors of the caregiver’s psychological health (Raina et al. 2004).
Social and economic factors may also have affected the caregiving experience (Raina et al. 2004). Certainly all the families in the sample lived in rural locations, with limited access to formal support. Some mentioned the option of occupational therapy at the hospital, but lack of transport and time constraints on domestic occupation prevented attendance. Additionally, only two of the nine children attended school regularly. Thus the support systems, both external to the family and internal to the marital unit, appeared to be inadequate. This undoubtedly contributed to the caregiver’s sense of isolation and perception of burden, which is consistent with findings by Ambikile and Outwater (2012).
Traditional, cultural beliefs added to the struggles experienced by some caregivers, which echoes findings by Gona and colleagues (2011) in the same region. The attribution of the child’s condition to evil spirits (‘jinnis’) has also been reported in Nigeria (Hamzat & Mordi 2007). Such beliefs were linked to the stigmatization of the child and the poor responses of others (Ambikile & Outwater 2012). Where the answer to the child’s condition was placed in religious beliefs, there was a sense of the caregiver waiting for change or a miracle to happen. It has been argued that attributing responsibility for the child’s disability to a higher authority, e.g. God, represents a coping strategy whereby stress may be alleviated (Treloar 2002; Burker et al. 2005; Balasundaram 2007; Gona et al. 2011).
After intervention
The home-based intervention comprised many features, which may have contributed to the new-found experiences reported by the caregivers. The extra attention afforded by the home intervention, which entailed regular home visits, new interest in the child where none was shown before and listening to what the caregiver has to say, may have affected a more positive view of the child and his/her condition. It is possible that the interactive nature of the intervention and the novel materials in use attracted the attention of others to the child, which is consistent with Anderson and colleagues (2011), who showed how typical children viewed friendship positively with children using AAC. The intervention activities were tailored to the individual’s behavioural characteristics that most of the caregivers were already responding to, albeit in a limited way. Thus the intervention provided validation of the caregiver as the expert, which is consistent with Raina and colleagues’s (2005) recommendation. The pivotal role occupied by the caregivers as active agents in the delivery of the intervention further imbued them with power, thereby affirming their roles (Granlund et al. 2008). The techniques were designed to complement the available skills of the children so that the families were exposed to what the child could do, instead of what they could not do. Bringing to light the potentials of the children provided a healthy counterpoint to the unrealistic hope of normality and cure held by the majority. Although the post-intervention narratives revealed persistence in this regard, ‘learning’ opportunities were now in place, which were connected with the idea of ‘cure’. The powerful influence of cultural beliefs in causal attribution of the child’s condition remained for one caregiver; however, the remainder related more to the idea of divine intervention providing the ultimate answer. Finally, the social impact of the study may have influenced the expression of positive views of the caregivers after the intervention.
Conclusion
The parental experience of caring for a child with complex communication needs associated with a developmental condition presents many challenges. A home-based intervention using AAC techniques appears to have been a catalyst for some positive transformations in the caregivers’ experiences, although it is not possible to attribute this change to any one aspect. Building on assets of the homestead, the child’s available skills and the caregiver’s natural expertise, using locally sourced AAC materials and focusing on home-based implementation were all key components. The potentials of the home-based intervention would benefit from further investigation on a larger scale.
Supplementary Material
Key messages.
The multi-faceted, home-based, AAC intervention provided some new opportunities for the caregiver to:
Connect in a meaningful way with the child’s own communication skills;
Affirm and build on existing communication with the child;
Re-establish social support systems.
Acknowledgement
We would like to thank the Director of Kenya Medical Research Institute for permission to publish the data. We would also like to thank the Educational Assessment and Resource team in Kilifi. Most importantly we would like to express our appreciation for the involvement of the mothers, their children and other family members who participated in this study. This work was supported by KEMRI/Wellcome Trust research programme and the C.P. Trust (UK). Charles Newton is supported by Wellcome Trust, UK.
References
- Alant E. Cultural and socio-economic influences on communication. In: Alant E, Lloyd LL, editors. Augmentative & Alternative Communication & Severe Disabilities: Beyond Poverty. Whurr; London, UK: 2005a. pp. 95–107. [Google Scholar]
- Alant E. AAC technology for development. In: Alant E, Lloyd L, editors. Augmentative and Alternative Communication and Severe Disabilities: Beyond Poverty. Whurr Publishers; London, UK: 2005b. pp. 192–220. [Google Scholar]
- Alant E. Training and intervention in South Africa. [last accessed on 5 June 2012];ASHA Leader. 2007 Available at: http://develop.asha.org/Publications/leader/2007/070814/f070814a1.htm. [Google Scholar]
- Alant E, Moolman E. Blissymbol learning as a tool for facilitating language and literacy development. South African Journal of Education. 2002;21:339–334. [Google Scholar]
- Alant E, Kolatsis A, Lilienfeld M. The effect of sequential exposure of color conditions on time and accuracy of graphic symbol location. Augmentative and Alternative Communication. 2010;26:41–47. doi: 10.3109/07434610903585422. [DOI] [PubMed] [Google Scholar]
- Ambikile JS, Outwater A. Challenges of caring for children with mental disorders: experiences and views of caregivers attending the outpatient clinic at Muhimbili National Hospital, Dar es Salam, Tanzania. Child Adolescent Psychiatry Mental Health. 2012;6:16. doi: 10.1186/1753-2000-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson K, Balandin S, Clendon S. ‘He cares about me and I care about him.’ Children’s experiences of friendship with peers who use AAC. Augmentative & Alternative Communication. 2011;27:77–90. doi: 10.3109/07434618.2011.577449. [DOI] [PubMed] [Google Scholar]
- Baker H, Hartley S. Piloting a Communication Ability Outcome Measuring Tool in Uganda. DIFID Report School Aged Child Health Programme. Centre for International Child Health, Institute of Child Health; London, UK: 1999. [Google Scholar]
- Balasundaram P. Love is not a feeling: faith and disability in the context of poverty. Journal of Religion, Disability and Health. 2007;11:15–22. [Google Scholar]
- Basson M, Alant E. The iconicity and ease of learning of picture communication symbols: a study with Afrikaans-speaking children. The South African Journal of Communication Disorders. 2005;52:5–12. [PubMed] [Google Scholar]
- Beukelman D, Mirenda P. Augmentative & Alternative Communication: Management of Severe Communication Disorders in Children and Adults. Paul Brookes; London, UK: 1992. [Google Scholar]
- Bondy AS, Frost LA. The picture exchange system. Focus on Autistic Behaviour. 1994;9:1–19. [Google Scholar]
- Bornman J, Alant E, Du Preez A. Translucency and learnability of Blissymbols in Setswana-speaking children: an exploration. Augmentative & Alternative Communication. 2009;25:287–298. doi: 10.3109/07434610903392456. [DOI] [PubMed] [Google Scholar]
- Bradshaw J. A total communication approach: towards meeting the communication needs of people with learning disabilities. Tizard Learning Disability Review. 2000;5:27–30. [Google Scholar]
- Burker EJ, Evon DM, Sedway JA, Egan T. Religious and non-religious coping in lung transplant candidates: does adding God to the picture tell us more? Journal of Behavioural Medicine. 2005;28:513–555. doi: 10.1007/s10865-005-9025-4. [DOI] [PubMed] [Google Scholar]
- Case S. Refocusing on the parent: what are the social issues of concern for parents of disabled children? Disability & Society. 2000;15:271–292. [Google Scholar]
- Dunst CJ, Boyd K, Trivette CM, Hamby DW. Family-oriented programme models and professional help giving practices. Family Relations. 2002;51:221–229. [Google Scholar]
- Enderby P. Therapy Outcome Measures: Speech-Language Pathology. Singular Publishing Group Inc; San Diego and London, UK: 1997. [Google Scholar]
- Gona JK, Mung’ala-Odera V, Newton CR, Hartley S. Caring for children with disabilities in Kilifi, Kenya: what is the carer’s experience? Child: Care, Health and Development. 2011;37:175–183. doi: 10.1111/j.1365-2214.2010.01124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granlund M, Björck-Åkesson E, Wilder J, Ylvén R. AAC interventions for children in a family environment: implementing evidence in practice. Augmentative & Alternative Communication. 2008;24:207–219. doi: 10.1080/08990220802387935. [DOI] [PubMed] [Google Scholar]
- Green SE. ‘We’re tired, not sad.’: benefits and burdens of mothering a child with a disability. Social Science Medicine. 2007;64:150–163. doi: 10.1016/j.socscimed.2006.08.025. [DOI] [PubMed] [Google Scholar]
- Hamzat TK, Mordi EL. Impact of caring for children with cerebral palsy on the general health of their caregivers in the African community. International Journal of Rehabilitation Research. 2007;30:191–194. doi: 10.1097/MRR.0b013e3281e5af46. [DOI] [PubMed] [Google Scholar]
- Hassall R, Rose J, McDonald J. Parenting stress in mothers of children with intellectual disability: effects of parental cognition relation to child characteristics and family support. Journal of Intellectual Disability and Research. 2005;49:405–418. doi: 10.1111/j.1365-2788.2005.00673.x. [DOI] [PubMed] [Google Scholar]
- Haupt L, Alant E. The iconicity of selected picture communication symbols for rural Zulu-speaking children. South African Journal of Communication Disorders. 2002;49:40–49. [PubMed] [Google Scholar]
- Kilifi Health Demographic and Surveillance System (KHDSS) Epidemiology and Demography. [last accessed 20 February 2012];2012 Available at: http://www.kemri-wellcome.org/khdss/
- Mayer P, Lowenbraun S. Total communication use among elementary teachers of hearing impaired children. American Annals of the Deaf. 1990;135:257–263. doi: 10.1353/aad.2012.0498. [DOI] [PubMed] [Google Scholar]
- Mayer-Johnson Picture communication symbols. [last accessed 11 June 2010];1981–2008 Boardmaker Plus v.6. Available at: http://www.mayer-johnson.co.uk.
- Mukhopadhyay S, Nwaogu P. Barriers to teaching non-speaking learners with intellectual disabilities and their impact on the provision of augmentative and alternative communication. International Journal of Disability, Development and Education. 2009;56:349–362. [Google Scholar]
- Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: caregiver perspective. Child: Care, Health and Development. 2006;33:180–187. doi: 10.1111/j.1365-2214.2006.00644.x. [DOI] [PubMed] [Google Scholar]
- Nind M, Hewett D. Access to Communication. David Fulton; London, UK: 1994. [Google Scholar]
- Park K. Using objects of reference: a review of the literature. European Journal of Special Needs Education. 1995;10:40–46. [Google Scholar]
- Park K. How do objects become objects of reference. British Journal of Special Education. 1997;24:108–114. [Google Scholar]
- Raina P, O-Donnell M, Schwqellnus H, Rosenbaum P, King G, Brehaut J, Russell DR, Swinton M, King S, Wong M, Walter SD, et al. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatrics. 2004;4:1–13. doi: 10.1186/1471-2431-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raina P, O-Donnell M, Rosenbaum P, Brehaut J, King G, Walter SD, Russell DR, Swinton M, Zhu B, Wood E. The health and well-being of caregivers of children with cerebral palsy. Paediatrics. 2005;115:626–e636. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- Royal College of Speech & Language Therapists. Communicating Quality 3. RCSLT; London, UK: 2006. [Google Scholar]
- Taylor-Powell E, Renner M. Analysing Qualitative Data. Programme Development and Evaluation, University of Wisconsin-Extension, Cooperative Extension; Madison, WI, USA: 2003. [Google Scholar]
- Tonsing KM, Alant E, Lloyd LI. Intervention issues. In: Alant E, Lloyd L, editors. Augmentative and Alternative Communication and Severe Disabilities: Beyond Poverty. Whurr Publishers; London, UK: 2005. pp. 30–67. Chapter 3. [Google Scholar]
- Treloar LL. Disability, spiritual beliefs and the church: the experiences of adults with disabilities and family members. Journal of Advanced Nursing. 2002;40:594–603. doi: 10.1046/j.1365-2648.2002.02417.x. [DOI] [PubMed] [Google Scholar]
- WHO. International Classification of Function. Disability and Health; Geneva, Switzerland: 2007. [Google Scholar]
- Wilkinson K, Henning S. The state of research in augmentative and alternative communication for children with developmental disabilities. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:58–69. doi: 10.1002/mrdd.20133. [DOI] [PubMed] [Google Scholar]
- Wormnaes S, Malek YA. Egyptian speech therapists want more knowledge about augmentative and alternative communication. Augmentative and Alternative Communication. 2004;20:30–41. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.