Abstract
Objectives
Very little is known about socioeconomic differentials in mortality among persons surviving to old age in sub-Saharan Africa. We report on the impact of low socioeconomic position (SEP) on mortality over a five-year observation period among community dwelling older adults living in South-Western Nigeria.
Method
Data are from a household multi-stage probability sample of 2149 Yoruba Nigerians aged 65 years or older. We collected information on indices related to health and well-being at baseline (2003/2004). Socioeconomic positions were estimated using asset-based measures relevant to low income settings. Information on mortality was obtained by research supervisors in multiple waves (2007, 2008, and 2009). Associations between baseline covariates and mortality were explored using discrete time survival models and life tables.
Results
We recorded 357 deaths over five years, or an annual mortality rate of 4.7% (95% C.I= 4.2-5.2). Being 80 years or older (H.R= 1.6, 95% C.I= 1.1-2.5), and belonging to the lowest SEP (H.R= 1.5, 95% C.I= 1.1-2.1) were the main predictors of mortality. The significant effect of lowest SEP on mortality risk over the study period was independent of age, gender, education, rural or urban residence, weight, physical activity level or social engagement.
Conclusion
In this sample of older persons living in an economically disadvantaged context, we found persistent socioeconomic differentials in mortality estimated, conservatively, over five years.
Keywords: Wealth index, Risk factors, Life expectancy, social welfare
Introduction
Globally, approximately 64% of the population of persons who are 60 years and older currently reside in developing countries (Velkoff & Kowal, 2007). Estimates suggest that this proportion will increase to about 80% in the next four decades (World Health Organisation, 2008). However, surviving to old age remains a challenge in many such countries. Despite global increases in life expectancy and decreases in mortality (Adeyi, Smith, & Robles, 2007; Wang et al., 2012), poverty and deprivation may affect long term survival among people in low- and middle-income countries (LMICs). In Nigeria, as an example, about 70% of the population live on less than $1.25 per day (Central Bank of Nigeria, 2011). In addition, there are no social welfare packages, and access to health care is limited and dictated by personal financial resources(Uwakwe et al., 2009). Belonging to a lower socio-economic position (SEP) in these circumstances is therefore likely to affect the health and survival of the older person.
Although fairly little is known about aging processes in Nigeria, it is has been projected that despite an average life expectancy at birth of about 52 years(United Nations International Children's Emergency Fund, 2008), the population surviving to the age of 65 years in the country may have the prospect of an additional 15 years of life (Gureje, Ogunniyi, Kola, & Afolabi, 2006; World Health Organisation, 2008).
The observations that persons in lower socioeconomic groups are more likely to die at younger ages while a comparatively healthier and wealthier section of the population survives to old age have been made in some high income countries (Beckett, 2000; Turra & Goldman, 2007) as well as in some LMICs with social welfare schemes and equitable access to healthcare (Rosero-Bixby & Dow, 2009). This has led to a suggestion that perhaps ‘selective mortality’ is in operation (Beckett, 2000; Phelan, Link, Diez-Roux, Kawachi, & Levin, 2004). In this context, socioeconomic differences may be less clearly associated with health and mortality in the population surviving to old age (Phelan et al., 2004). Contrary to these observations, it is plausible to expect that, in Nigeria, where there are no social welfare schemes that provide access to quality health care for older adults, socio-economic differentials in health and mortality will persist in old age. However, the extent of this relationship has not been formally investigated.
The present study describes the impact of low SEP on all-cause mortality during a five-year observation period in a probability sample of persons who were 65 years or older living in communities spread across the Yoruba-speaking region of Nigeria, a geographical area equivalent to about 25 million population. The Yorubas are a distinct ethnic group in regard to language, culture, and social organization from the other ethnic groups in Nigeria. We have relied on asset based measures to provide a direct and relatively stable estimation of SEP, and hypothesized that belonging to the lowest SEP, relative to higher positions, will be associated with higher mortality among older adults in the population.
Methods
Sample selection, recruitment and follow-up
The Ibadan Study of Aging (ISA) has been previously described (Gureje, Kola, & Afolabi, 2007); we provide only a brief overview here. Individuals were selected using stratified multistage cluster sampling from eight neighboring states of the South-West and North-central regions of Nigeria, representing approximately 22% of the total Nigerian population at the time of study. From 15 strata, based on state and urban versus rural location, 43 Local Government Areas were selected as the primary sampling units (PSUs). Secondary sampling units (SSUs), defined by numeration units of 50 to 70 housing units, were selected from each PSU (172 SSUs in total). A simple random sample of 17 households with individuals aged 65 years or over was then selected from each SSU. One individual from each household was approached to participate in the study. For households with multiple eligible individuals (aged 65 years or over and fluent in Yoruba – the local language), the one individual was selected using a Kish grid (Kish L, 1949). Up to five calls were made to contact the selected individual and there was no replacement for those who could not be contacted or who refused to participate in the study. The overall response rate was 75.0%.
Baseline assessments were conducted between November 3, 2003, and August 27, 2004. Three follow-up waves were implemented in 2007, 2008 and 2009. Of the baseline sample, 63.0% were fully re-interviewed at the final follow-up. We recorded 268, 67, and 22 deaths in 2007, 2008, and 2009, respectively. They represented 16.6% of the baseline sample. A total of 835 participants or 38.9% of the baseline sample were lost to follow-up cumulatively over the 5-year period of the study. Respondents who were lost to follow-up were more likely to belong to lower SEPs.
Measures and Procedure
Mortality
Information on mortality was collected at each of the assessment periods by trained research interviewers. Information about death was obtained in each instance from a member of the household and recorded in a case record format. A verbal autopsy survey was conducted during the 2007 wave, for deaths occurring between 2003/2004 and 2007, but the results of that survey are not the focus of the present report.
Living condition and socioeconomic status
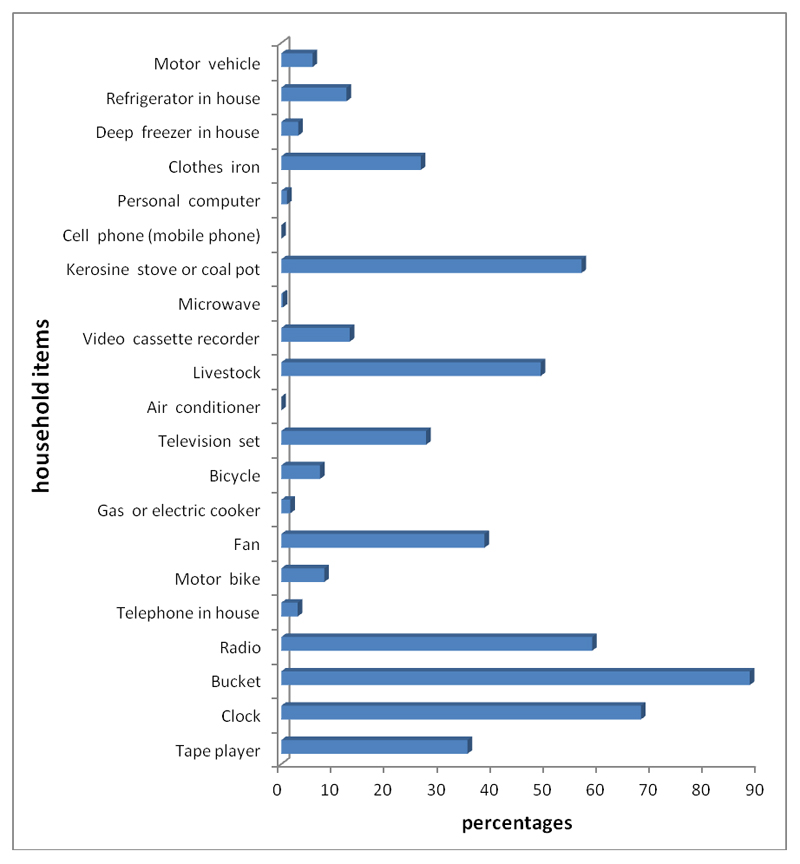
The living condition of the households in the baseline survey of the ISA was ascertained using measures such as the number and type of household items, the type of material used for the floor and walls of the house, as well as sources of water supply and energy for cooking and lighting. These variables have previously been reported as important indices of the economic status of older adults in developing countries (Ferguson, Tandon, & Gakidou, 2003; Rutstein, 2008). While the list of household items may provide a direct measure of economic status(Ferguson et al., 2003), the type of flooring and walls of the house, as well as the sources of water and energy supply may be used as valid proxies(Rutstein, 2008). We used an inventory of 21 household and personal items such as chairs, radio, television sets, cookers, and iron to classify the socioeconomic status of the participants (wealth index). Each participant’s status was determined by relating the number of their household possessions to the median number of possessions of the overall sample. Thus, a respondent’s economic status was classified as low if the number of possessions was ≤0.5 of the median, low-average if it was >0.5-1.0; high-average if >1.0-2.0 and high if >2.
Other baseline risk factors
Several demographic, health and lifestyle factors and chronic medical conditions were assessed in 2003/2004. For participants who, because of illiteracy, were unable to provide their age, important local historical events were used to estimate the approximate year of their birth. Residence was classified as rural (<12,000 households), semi-urban (12,000–20,000 households) or urban (>20,000 households). Participants’ highest occupational attainment was categorised based on the International standard classification of occupations (International Labour Organisation, 1988). Social engagement was assessed using items derived from the World Health Organization Disability Assessment Schedule, version 2 (World Health Organization, 1999). Participants were asked the following two questions: “During the last 30 days, how much did you join in family activities such as eating together, talking with family members, visiting family members, working together?” and “During the last 30 days, how much did you join in community activities such as festivities, religious activities, talking with community members, working together?” Answers were rated as 1 (not at all), 2 (a little bit), 3 (quite a bit), and 4 (a lot). In this study, participants who answered “not at all” to either questions were rated as having poor social engagement.
For the assessment of physical activity, respondents were first asked about the presence of any difficulties with movements from one place to another in the past 30 days. They were then asked about the degree of difficulties they had in doing some more rigorous activities such as riding a bicycle or farm work in the same period of time. In each instance, they were given five options: None, Mild, Moderate, Severe, and Extreme/cannot do. The presence of chronic medical conditions such as arthritis, stroke, angina, diabetes, chronic lung disease, or cancer was ascertained using standard symptom-based questions (National Health Statistics, 1994). Participants were classified as ever having smoked or not, and ever used alcohol or not based on self-report. Those who answered in the affirmative were further asked about the frequency/ intensity of these activities. Information about the exact amount of tobacco or alcohol consumed was not elicited. Over the course of interview, three measurements of mid-upper arm circumference (MUAC) were taken at intervals. We have used these measurements to derive appropriate weight categories, following references developed in a study conducted among a sub-Saharan African older adult population (Charlton, Kolbe-Alexander, & Nel, 2005).
Statistical methods
The sample for the mortality study included individuals who provided baseline data between November 2003 and August 2004 and were followed up in three waves: 2007, 2008 and 2009. A participant was considered to have reached an endpoint when they have completed assessments in 2009 or when the research interviewer was reliably informed about their death, usually by a member of the household. Participants with no records of death and who did not complete 2009 assessments were censored.
The demographic characteristics of those who survived, died, or were censored were compared using Pearson chi-square test, with a Rao and Scott correction (Rao & Scott, 1981) to account for the survey design.
Person years at risk were calculated as the period between baseline and follow-up assessments for those who survived, and between baseline and the mid-point of each interval for those who died or were censored in each wave. This corresponds to the actuarial adjustment approach of a life table (i.e., censored observations contribute half of the number of person years at risk during each wave). To explore the sensitivity of our analysis to this assumption, we calculated person years for those who died or were censored using the interval from baseline to the last wave in which the person was followed up. This corresponds to the product limit estimator assumption for Kaplan-Meier analyses (i.e., they contribute to the cumulative proportion of dying overtime). The mortality rates with 95% confidence interval for both actuarial and Kaplan-Meir approaches are presented.
Specific mortality estimates for each demographic and living condition categories were calculated by dividing the number of deaths by the total person years for that category. Estimates of mortality of participants who were in the lowest economic category relative to the other groups were determined. These estimates are reported per 1000 person-years, with 95% confidence intervals.
The dataset had two types of missing data problems: missing responses and loss to follow-up. For the former, some baseline variables had missing values when respondents did not answer certain questions such as those relating to occupational status. The latter missing data problem was for individuals who only had baseline assessment and no ascertained death information. Because the missing data pattern was not uniform, we performed multiple imputations using the iterative chained equations approach (White, Royston, & Wood, 2011) to impute the missing items, the death information and survival time for those with only baseline assessment. The imputation models included key baseline characteristics, outcome variables (except for when imputing the indicator for death), sample design variables, and sampling weights. Inference from the multiple imputed data was based on the Rubin approach (Rubin, 1987).
The effect of baseline demographic, living condition and SEP on mortality during follow-up was estimated by using the entire baseline sample. Because of the quality of the survival data, we used the discrete time version of the Cox regression model for time invariant explanatory variables to derive estimates of hazard ratios assuming proportional hazards. We first performed an unadjusted analysis (Model I). Next, two sets of multivariable analyses were carried out. We adjusted for the effect of age, gender, and education, on mortality in Model II. In model III, we adjusted for variables, such as weight, social engagement, physical activities, and location (i.e., whether urban, semi-urban or rural), in addition to variables in model II. These were factors that might have significantly affected both survival to the end point of 2009, and death before this end-point. A significance level of p<0.05 was used throughout the analyses. Coefficient estimates and 95% confidence intervals are presented for the regression models.
Data were analysed using Stata version 13.0 (StataCorp, 2013). The survey commands in Stata were used to account for the study sampling scheme. For this, we used the PSU identifier variable, strata, and the sampling weights. The secondary and subsequent sampling units were not incorporated in the command because all SSU’s within each PSU were included, and sampling within the SSU was simple random; thus there was no finite population correction for the PSU. Given these considerations, all subsequent sampling design features were ignored.
Results
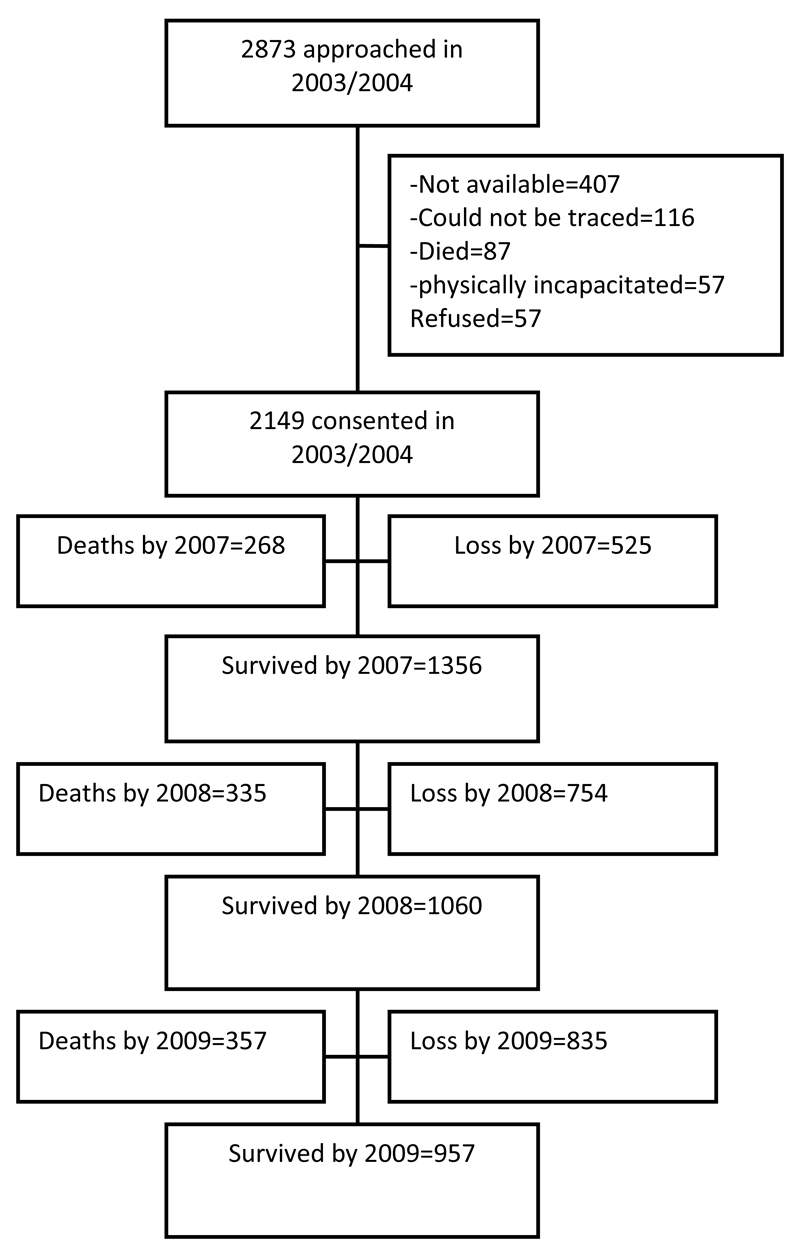
The 2149 individuals aged 65 years or older who constituted the cohort for the follow-up waves provided 7657 person years of follow up using the actuarial approach and 7183 person years using the Kaplan-Meier approach. Figure 1 shows the detail of study recruitment and follow-up, including the number of participants at each data collection wave and those who were lost to follow-up. The mean age of those who were followed up until 2009 was 74.4 (± 8.8) years, with a median of 73.0 years.
Figure 1. Study participants’ flow chart.
Table 1 (also see supplementary table 1) provides the details of the characteristics of the study participants, those who died, survived to the end point, and those who were censored. We note that the differences in the numbers of deaths recorded in the three follow-up waves are due in part to varying lengths of follow-up for each wave and a relatively high attrition in 2008 (over a quarter of attrition across the 5 years).
Table 1. Baseline characteristics of participants (N=2149).
| Characteristics | Survived N=957 (%) | Died N=357 (%) | Censored N=835 (%) | Design based F statistic | p-value |
|---|---|---|---|---|---|
| Age group | |||||
| 65-69 | 318 (36.7) | 80 (30.9) | 304 (41.8) | 4.46 | 0.003 |
| 70-74 | 259 (32.3) | 68 (25.6) | 168 (25.2) | ||
| 75-79 | 135 (18.5) | 50 (19.6) | 110 (16.2) | ||
| 80+ | 245 (12.5) | 159 (24.0) | 253 (16.9) | ||
| Gender | |||||
| Male | 464 (60.3) | 173 (58.2) | 364 (55.4) | 1.37 | 0.270 |
| Female | 493 (39.7) | 184 (41.8) | 471 (44.6) | ||
| Residence | |||||
| Urban | 233 (24.2) | 106 (33.1) | 216 (25.9) | 1.99 | 0.120 |
| Semi-urban | 403 (42.3) | 138 (39.2) | 329 (41.5) | ||
| Rural | 321 (33.5) | 113 (27.7) | 290 (32.6) | ||
| Education | |||||
| ≥13 | 69 (7.50) | 34 (8.4) | 63 (8.59) | 0.54 | 0.697 |
| 7-12 | 117 (13.5) | 47 (13.2) | 102 (11.9) | ||
| 1-6 | 239 (26.0) | 93 (28.8) | 201 (24.0) | ||
| 0 | 532 (53.0) | 183 (49.6) | 469 (55.5) | ||
| Socio-economic position | |||||
| High | 115 (16.1) | 40 (17.1) | 69 (9.8) | 5.22 | <0.001 |
| High-average | 240 (30.0) | 77 (29.6) | 178 (26.2) | ||
| Low-average | 351 (34.3) | 110 (24.9) | 302 (37.9) | ||
| Low | 251 (19.6) | 130 (28.5) | 286 (26.1) | ||
| Occupational attainment | |||||
| Semi-Skilled/higher level | 103 (15.0) | 40 (14.2) | 78 (12.9) | 0.49 | 0.718 |
| Elementary | 349 (42.9) | 135 (46.8) | 310 (46.4) | ||
| Trade | 427 (42.2) | 145 (39.0) | 342 (40.7) | ||
| Medical morbiditya | |||||
| Absent | 674 (69.5) | 248 (66.9) | 599 (68.7) | 0.25 | 0.774 |
| Present | 283 (30.5) | 109 (33.1) | 236 (31.3) | ||
| Tobacco smoking | |||||
| Daily | 100 (9.1) | 44 (13.2) | 78 (10.0) | 0.83 | 0.473 |
| Less than daily | 301 (38.1) | 110 (35.2) | 242 (35.0) | ||
| Never | 135 (18.5) | 50 (19.6) | 110 (16.2) | ||
| Alcohol consumption | |||||
| Regular (at least weekly) | 155 (20.6) | 49 (19.0) | 131 (20.8) | 0.13 | 0.917 |
| Occasional (<weekly) | 260 (27.0) | 98 (28.9) | 214 (27.8) | ||
| Never | 498 (52.5) | 195 (52.0) | 407 (51.4) | ||
| Weight | |||||
| Underweight | 58 (5.0) | 59 (12.9) | 81 (8.9) | 3.15 | 0.014 |
| Normal weight | 452 (47.1) | 182 (52.8) | 400 (49.0) | ||
| Overweight | 265 (30.0) | 68 (20.8) | 198 (26.2) | ||
| Obese | 175 (18.3) | 47 (13.5) | 136 (15.8) | ||
| Social engagementb | |||||
| Poor | 58 (4.1) | 34 (7.3) | 72 (6.6) | 2.57 | 0.095 |
| Good | 874 (95.9) | 307 (92.7) | 720 (93.4) | ||
| Physical activity | |||||
| Low | 306 (27.7) | 159 (38.5) | 295 (29.6) | 3.21 | 0.033 |
| Moderate | 485 (50.8) | 160 (48.9) | 391 (50.0) | ||
| High | 166 (21.5) | 38 (12.7) | 149 (20.4) | ||
Include several chronic medical and pain conditions common in the study setting
Include participation in family and community activities
Note: Percentages are weighted.
In all, about a quarter of the participants in the ISA were categorized as belonging to the lowest SEP. Women were generally poorer than men. The details of the distribution of living conditions, including household possessions (wealth), floor and wall finishing, as well as sources of water and energy supply are shown on table2 and figure 2.
Table 2. Distribution of household possessions and Living conditions in the Ibadan study of Ageing.
| Percentagesa | ||
|---|---|---|
| Measuresb | Men | Women |
| Occupational attainment | ||
| Semi-Skilled/higher level | 21.3 | 4.4 |
| Elementary | 59.2 | 23.4 |
| Trade | 19.6 | 72.2 |
| Number of household possessions (wealth index) | ||
| >10 | 17.1 | 10.8 |
| 6-10 | 34.8 | 22.6 |
| 3-5 | 32.4 | 38.4 |
| <3 | 15.7 | 28.2 |
| Living condition | ||
| Floor type | ||
| Hard | 85.7 | 85.2 |
| Earthen (clay) | 14.3 | 14.8 |
| Source of water supply | ||
| Protected (Piped/tubed) | 71.9 | 76.4 |
| Unprotected (open stream/ rain) | 28.1 | 23.6 |
| Source of light supply | ||
| Electricity | 49.2 | 49.5 |
| Fossil (Paraffin/Kerosine/wood) | 50.8 | 50.5 |
| Source of energy for cooking | ||
| Electricity | 7.9 | 7.8 |
| Paraffin/Kerosine fuel | 32.0 | 33.5 |
| Wood/Charcoal fuel | 60.0 | 58.7 |
Percentages were based on respondents with no missing data and weighted by sampling weights.
Missing responses were corrected in subsequent analyses by multiple imputations using the iterative chained equations approach
Figure 2. The distribution household possessions of participants in the study.
The annual mortality rate for the sample was 4.7% (95% C.I= 4.2-5.2) using the actuarial approach and 5.0% (95% CI= 4.5-5.5) using the Kaplan-Meier approach (Table 3). We note that the two approaches produced similar results. Being 80 years or older (H.R= 1.9, 95% C.I= 1.3-1.7), and belonging to the lowest SEP (H.R= 1.5, 95% C.I= 1.1-2.1) relative to the other categories were the main predictors of mortality in unadjusted analyses (Tables 3 and 4).
Table 3. Mortality rates and (un-adjusted) hazard ratio over 5 years (N=2149).
| Actuarial approach | Kaplan-Meier approach | ||||
|---|---|---|---|---|---|
| Baseline characteristics | Deaths over 5 years | Mortality rate per 1000 person-years (95% C.I) | Unadjusted HR (95%C.I) | Mortality rate per 1000 person-years (95% C.I) | Unadjusted HR (95%C.I) |
| Overall | 357 | 46.6 (42.0-51.7) | n.a. | 49.7 (44.8-55.1) | n.a. |
| Demographics | |||||
| Age group | |||||
| 65-69 | 80 | 32.1 (25.8-40.0) | Reference | 35.7 (28.7-44.5) | Reference |
| 70-74 | 68 | 36.6 (28.9-46.4) | 1.1 (0.7-1.5) | 38.6 (30.4-47.0) | 1.0 (0.7-1.4) |
| 75-79 | 50 | 45.6 (34.6-60.2) | 1.3 (0.8-2.2) | 47.8 (36.2-63.0) | 1.2 (0.7-2.1) |
| 80+ | 159 | 71.9 (61.4-83.9) | 1.9 (1.3-2.7)* | 74.4 (63.7-86.9) | 1.8 (1.3-2.7)* |
| Gender | |||||
| Male | 173 | 48.0 (41.4-55.8) | Reference | 50.6 (43.6-58.8) | Reference |
| Female | 184 | 45.4 (39.3-52.4) | 1.0 (0.7-1.4) | 48.9 (42.3-56.5) | 1.1 (0.8-1.5) |
| Site | |||||
| Urban | 106 | 56.4 (46.6-68.2) | Reference | 60.4 (49.9-73.0) | Reference |
| Semi-urban | 138 | 43.0 (36.4-50.9) | 0.7 (0.5-1.0) | 45.5 (38.5-53.8) | 0.7 (0.5-1.0) |
| Rural | 113 | 43.9 (36.5-52.8) | 0.6 (0.4-1.0) | 47.1 (39.2-56.7) | 0.6 (0.4-0.9) |
| Education | |||||
| ≥13 | 34 | 60.0 (42.9-84.0) | Reference | 62.8 (44.9-87.0) | Reference |
| 7-12 | 47 | 48.9 (36.8-65.1) | 0.9 (0.6-1.6) | 51.6 (38.8-68.7) | 0.9 (0.5-1.5) |
| 1-6 | 93 | 49.3 (40.3-60.5) | 1.1 (0.6-1.8) | 52.3 (42.7-64.1) | 1.0 (0.6-1.7) |
| 0 | 183 | 43.1 (37.3-49.8) | 0.9 (0.5-1.4) | 46.3 (40.0-53.5) | 0.9 (0.5-1.4) |
| Occupational attainment | |||||
| Semi-Skilled/higher level | 40 | 49.6 (36.4-67.7) | Reference | 52.2 (38.3-71.1) | Reference |
| Elementary | 135 | 46.8 (39.5-55.4) | 1.0 (0.6-1.7) | 49.3 (41.6-58.3) | 1.0 (0.6-1.7) |
| Trade | 145 | 44.2 (37.6-52.1) | 1.0 (0.6-1.4) | 47.2 (40.1-55.6) | 1.0 (0.7-1.4) |
| Number of household possessions (wealth) | |||||
| >10 | 40 | 47.4 (34.7-64.6) | Reference | 49.0 (35.9-66.7) | Reference |
| 6-10 | 77 | 42.5 (34.0-53.2) | 0.9 (0.6-1.3) | 45.2 (36.1-56.5) | 0.9 (0.6-1.3) |
| 3-5 | 110 | 39.4 (32.7-47.5) | 0.6 (0.5-0.8) | 42.2 (35.0-50.8) | 0.7 (0.5-0.8) |
| <3 | 130 | 58.9 (49.6-69.9) | 1.1 (0.8-1.5) | 63.3 (53.3-75.2) | 1.2 (0.8-1.7) |
| Living condition | |||||
| Floor type | |||||
| Hard | 298 | 49.2 (44.0-55.2) | Reference | 51.8 (46.2-58.0) | Reference |
| Earthen (clay) | 48 | 39.8 (30.0-52.9) | 0.8 (0.5-1.2) | 43.2 (32.6-57.4) | 0.8 (0.5-1.3) |
| Source of water supply | |||||
| Protected (Piped/tubed) | 241 | 44.7 (39.4-50.7) | Reference | 47.2 (41.6-53.6) | Reference |
| Unprotected (river/stream/ rain) | 107 | 56.9 (47.1-68.7) | 1.3 (0.9-1.8) | 60.1 (49.7-72.6) | 1.3 (0.9-1.8) |
| Energy source for cooking | |||||
| Electricity | 38 | 65.9 (47.9-90.5) | Reference | 69.2 (50.4-95.1) | Reference |
| Paraffin/Kerosine | 121 | 51.6 (43.2-61.8) | 0.8 (0.6-1.2) | 54.6 (45.7-65.3) | 0.8 (0.6-1.3) |
| Wood/Charcoal | 188 | 43.2 (37.5-49.9) | 0.6 (0.4-0.9) | 45.7 (39.6-52.7) | 0.6 (0.4-0.9) |
| Source of energy for light | |||||
| Electricity | 152 | 46.4 (39.6-54.4) | Reference | 49.1 (41.9-57.6) | Reference |
| Fossil (Paraffin/Kerosine/wood) | 194 | 48.5 (42.2-55.9) | 1.0 (0.8-1.3) | 51.3 (44.5-59.0) | 1.0 (0.8-1.3) |
Table 4. Association between low socio-economic position and mortality.
| Socio-economic positions | H.R (95% C.I)a |
|---|---|
| Higher | Reference |
| Lowest | Model I: 1.5 (1.1-2.1)* |
| Model II: 1.5 (1.1-2.1)* | |
| Model III: 1.6 (1.2-2.2)* | |
| Model III Covariates | H.R (95% C.I)a |
| Age over 80 years | 1.7 (1.1-2.5)* |
| Female gender | 0.8 (0.6-1.2) |
| No formal Education | 0.9 (0.5-1.8) |
| Urban place of residence | 0.7 (0.5-1.1) |
| Rural place of residence | 0.6 (0.4-0.8) |
| Underweight | 1.4 (0.9-2.2) |
| Overweight | 0.8 (0.5-1.2) |
| Obese | 0.8 (0.5-1.2) |
| Poor social engagement | 1.3 (0.8-2.0) |
| Moderate Physical activity | 0.5 (0.9-2.5) |
| Poor physical activity | 2.0 (1.1-3.8)* |
Model I= Unadjusted; Model II= adjusted for age, gender, and education; Model III = adjusted for age, gender, education, Residence, weight, social engagement, and physical activities.
Based on discrete time proportional hazard model with multiply imputed data
In multivariate analyses in which age, gender, education, residential areas, body weight, physical activity level, and social engagement at baseline were controlled for, belonging to the lowest SEP was significantly associated with mortality over the study period (HR= 1.5, 95% CI= 1.1-2.1), (table 4). These analyses were not sensitive to whether actuarial or Kaplan Meier approaches were used (see supplementary table 2).
Discussion
In this study, we recorded 357 deaths in 5 years, translating to an annual mortality rate of 4.7% to 5.0% depending on the methods used. Belonging to the lowest SEP was consistently associated with a higher mortality. This result was independent of whether we considered the risk of dying at each wave, or cumulatively over the 5 years of follow-up.
The annual mortality rate estimated in this study is slightly lower than rates of between 5.3% and 5.9% reported in some studies conducted in Western Europe and North America (Benabarre et al, 2014, Ganguli, 2002). Important differences in sample size and method of mortality data collection are of relevance. For instance, in the study by Benabarre et al (Benabarre et al, 2014), mortality data of 293 older adults living in a Spanish province were derived from registry of health records. Similar to many developing countries, there is no mandatory vital registration of deaths in Nigeria. Research supervisors had to conduct regular and frequent visits to the participating households and keep records of the dead whenever this was reported. Given the possible effect of this limitation on the quality of our survival data, we have used a discrete, rather than continuous, time approach for subsequent estimation of mortality risks in this study.
The mortality rate recorded is also slightly lower than that reported from a previous study conducted among older adults living in Idikan, a densely populated inner city community in Ibadan, South-western Nigeria (Perkins et al., 2002). In that study, 34% of the participants died over the course of 5 years. There is thus a 7% difference in the mortality rates estimated in the two studies. Given the global increase in life expectancy of about 4 years per decade (Wang et al, 2012), it may be misleading to directly compare two studies conducted over a decade apart, even when the number of years of follow-up are similar. The present report is based on a sample of older individuals spread over communities in which about 22% of the Nigerian population resided at the time of study. The sample in the previous study in Ibadan (Perkins et al., 2002) is very likely to have a higher proportion of persons from the lowest SEPs compared with the one reported here. Nevertheless, we could not rule out the possibility that missing or unavailable information may have led to an under-estimation of the number of deaths in the present study. We conducted multiple imputations using the iterative chained equation approach (White et al., 2011) to correct for the variety of missing information identified in the study. Additional sensitivity analyses were conducted using both the actuarial adjustments (life tables) and product limit estimator assumptions (Kaplan-Meier) for the calculation of the person years at risk. The results of these analyses were not very sensitive to the different approaches.
We note that economic measures of floor type, source of water and energy supply were not significantly associated with mortality in this study. This finding may not be surprising because these measures are known to reflect urban versus rural distribution (Rutstein, 2008), especially in LMICs (Howe et al., 2012), rather than being direct indicators of the SEP of participants. In keeping with this observation, we found that about three quarter of the participants living in households with earthen floor finishing in this sample, as an example, were resident in rural locations.
In contrast to the broader indices of living conditions, belonging to the lowest SEP (as estimated using the possession of 21 household items), was associated with mortality. This particular relationship was not sensitive to whether actuarial or product limit estimator approaches were used in the calculation of the mortality rates. While this finding is largely in keeping with global trends(Blakely & Wilson, 2006; Phelan et al., 2004; Rosero-Bixby & Dow, 2009; Signorello et al., 2014), some recent reports from high income regions of the world (Feinglass et al., 2007; Hoyert & Xu, 2012) suggest that socioeconomic disparity in all-cause mortality in older adults is fast becoming less pronounced. This trend has also been noted in some LMICs (Rosero-Bixby & Dow, 2009) where economic disparities among the older population have been reduced through social welfare schemes and equitable access to health care. Studies reporting persisting socioeconomic differences in mortality rates in such countries (Signorello et al., 2014) have often been those employing less conservative analytic approaches, such as, comparing the lowest with the highest SEP. In countries such as Nigeria where the wealthiest 18% controls half of the national income, while the poorest 20% share only 4% of the national wealth (Ogujiuba, 2014), estimating socioeconomic impact on mortality rates by comparing the richest with the poorest may produce larger and inflated differences between the two groups. Therefore, and in consideration of the fact that SEP may be distributed in a continuum between the poorest and the richest, we have compared the lowest with higher SEP categories.
Although the literature on the predictors of mortality in the general population of older adults appears inconclusive, we found that being older than 80 years and engaging in low physical activity were associated with higher risk of mortality (Table 4). This is in keeping with previous studies (Benabarre et al., 2014; Pijpers, Ferreira, van de Laar, Stehouwer, & Nieuwenhuijzen Kruseman, 2009). Being older than 80 years and engaging in low physical activities are fairly consistent risk factors for morbidity (Stenholm et al., 2015). In a setting like Nigeria where health insurance is almost non-existent and out-of-pocket payment for health care is the rule, belonging to the lowest economic category will compound the impact of physical morbidity on the older adults by limiting their access to quality health care. However, rates of co-morbid medical conditions were not found to significantly differentiate between those who survived to the end point of this study and those who died, or those who were lost to follow-up.
In the light of evidence from other settings where SEP differentials in mortality have narrowed following the introduction of packages that provide socio-economic buffers and guaranteed equitable access to quality health care for the poorest older adults (Rosero-Bixby & Dow, 2009), we think that the SEP differential in mortality found in this study may be due to the prevailing poverty, rapid social changes, and general absence of organized support for the most vulnerable older adults in the setting of our study. In the context of rapid socioeconomic changes taking place in Nigeria, and many developing countries in sub-Saharan Africa, the traditional extended family system which provided important buffers for older adults in such settings is fast eroding. Many younger members of extended households drift to urban locations to seek better economic opportunities, leaving behind the older and often weaker members. The situation identified in this study is therefore unlikely to be very different in other low income and transitional economies, especially those in sub-Saharan Africa.
We have estimated the SEP of the participants using household possessions. This asset-based approach is acknowledged to be a fairly stable measure of SEP of older people living in LMICs(Ferguson et al., 2003; Rutstein, 2008). Such stability may be of value in studies conducted in settings, such as Nigeria, with large subsistent farming populations, especially in the rural areas. In such locations, other measures of SEP, for example current income or expenditure, may exhibit seasonal fluctuations. Furthermore, the more stable indices of SEP may better reflect longer term SEP, which appears to be more relevant to mortality (Blakely & Wilson, 2006), when compared with indices of current SEP. On the other hand, indices of living conditions, such as type of floor finishing, sources of water and energy supply, appear to reflect rural and urban distribution of the participants, rather than their true SEP. Thus, the use of these indices in studies of SEP may produce confounded results.
In the context of our study, it is likely that the possession of household items reflects more closely the availability of the financial resources necessary for older adults to meet the basic essentials of life. Falling below a certain minimum number of household items probably indicates a level of absolute poverty where basic essentials, such as good nutrition and access to health care, become unaffordable. Older adults in such situation may become vulnerable to ill-health, and may be unable to access the care they need when ill-health sets in. For such older persons, it is likely that deliberate policies that provide some regular stipend and facilitate better access to health care will be important in reducing mortality risks.
This study is based on a fairly large sample of older adults derived from a wide geographical area. Along with the careful sampling procedure, this should allow for a wider generalization of the findings. Nevertheless, there was substantial attrition, mostly due to non-availability of some participants during the follow-up waves. Those who were lost to follow-up were more likely to belong to the lower SEPs. Although we have made attempts at statistical correction of the missing information, this factor may still have affected the estimation of both SEP and mortality in this study.
Conclusions
Even though we have relied on conservative estimates of both SEP and mortality, we have found a stable socioeconomic differential in mortality estimated over five years in this representative sample of community dwelling older adult Nigerians. Recent studies in the elderly populations of high income countries have reported a consistent narrowing of the socioeconomic disparity in mortality. Similar findings have been reported in LMICs where social welfare programmes and improved access to health care have reduced socioeconomic inequality among older adults. This observation would suggest that deliberate policies that allow for equitable access to health care, including social welfare schemes, may have direct impact in reducing mortality risks among older adults, especially those in the lowest SEP.
Acknowledgments
Source of Research Support:
This work was supported by the Wellcome Trust‘(grant no: WT079662MF)’
References
- Adeyi O, Smith O, Robles S. Public policy and the challenge of chronic non-communicable diseases. Washington D.C: World Bank; 2007. p. 208. [Google Scholar]
- Beckett M. Converging health inequalities in later life--an artifact of mortality selection. J Health Soc Behav. 2000;41(1):106–119. [PubMed] [Google Scholar]
- Benabarre S, Olivera J, Lorente T, Rodriguez M, Barros-Loscertales A, Pelegrin C, Rodriguez J. Psychiatric symptoms are not an independent mortality risk factor in community-living elderly people. Int Psychogeriatr. 2014;26(6):911–920. doi: 10.1017/S1041610214000143. [DOI] [PubMed] [Google Scholar]
- Blakely T, Wilson N. Shifting dollars, saving lives: what might happen to mortality rates, and socio-economic inequalities in mortality rates, if income was redistributed? Soc Sci Med. 2006;62(8):2024–2034. doi: 10.1016/j.socscimed.2005.08.059. [DOI] [PubMed] [Google Scholar]
- Central Bank of Nigeria. Annual Report and Statement of Accounts for the year Ended 31st December 2011. 2011. [Google Scholar]
- Charlton KE, Kolbe-Alexander TL, Nel JH. Development of a novel nutrition screening tool for use in elderly South Africans. Public Health Nutr. 2005;8(5):468–479. doi: 10.1079/phn2005783. [DOI] [PubMed] [Google Scholar]
- Feinglass J, Lin S, Thompson J, Sudano J, Dunlop D, Song J, Baker DW. Baseline health, socioeconomic status, and 10-year mortality among older middle-aged Americans: findings from the Health and Retirement Study, 1992 2002. J Gerontol B Psychol Sci Soc Sci. 2007;62(4):S209–217. doi: 10.1093/geronb/62.4.s209. [DOI] [PubMed] [Google Scholar]
- Ferguson B, Tandon A, Gakidou E. Estimating Permanent income using Indicator variables. In: Murray C, Evans D, editors. Health systems Performance Assessment: diabetes, methods and empericism. Geneva: World Health Organisation; 2003. pp. 747–760. [Google Scholar]
- Gureje O, Kola L, Afolabi E. Epidemiology of major depressive disorder in elderly Nigerians in the Ibadan Study of Ageing: a community-based survey. Lancet. 2007;370(9591):957–964. doi: 10.1016/S0140-6736(07)61446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gureje O, Ogunniyi A, Kola L, Afolabi E. Functional disability in elderly Nigerians: Results from the Ibadan Study of Aging. J Am Geriatr Soc. 2006;54(11):1784–1789. doi: 10.1111/j.1532-5415.2006.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe LD, Galobardes B, Matijasevich A, Gordon D, Johnston D, Onwujekwe O, Hargreaves JR. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol. 2012;41(3):871–886. doi: 10.1093/ije/dys037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyert DL, Xu JQ. National Vital Statistics Report. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2012. Deaths: preliminary data for 2011; p. 52. [PubMed] [Google Scholar]
- International Labour Organisation. Fourteenth International Conference of Labour Statisticians: report of conference; Geneva: International Labour Organisation; 1988. [Google Scholar]
- Kish L. A procedure for objective Respondent selection within the Household. Journal of the American statistical Association. 1949;247:380–387. [Google Scholar]
- National Health Statistics. Evaluation of National Health Interview Survey Diagnostic Reporting. Vital Health Statistics. 1994;120:1–116. [PubMed] [Google Scholar]
- Ogujiuba K. Poverty Incidence and Reduction Strategies in Nigeria: Challenges of Meeting 2015 MDG Targets. J Economics. 2014;5(2):201–217. [Google Scholar]
- Perkins AJ, Hui SL, Ogunniyi A, Gureje O, Baiyewu O, Unverzagt FW, Hendrie HC. Risk of mortality for dementia in a developing country: the Yoruba in Nigeria. Int J Geriatr Psychiatry. 2002;17(6):566–573. doi: 10.1002/gps.643. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. "Fundamental causes" of social inequalities in mortality: a test of the theory. J Health Soc Behav. 2004;45(3):265–285. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- Pijpers E, Ferreira I, van de Laar RJ, Stehouwer CD, Nieuwenhuijzen Kruseman AC. Predicting mortality of psychogeriatric patients: a simple prognostic frailty risk score. Postgrad Med J. 2009;85(1007):464–469. doi: 10.1136/pgmj.2008.073353. [DOI] [PubMed] [Google Scholar]
- Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: Chi-squared tests for goodness of fit and independence in two-way tables. Journal of the American Statistical Association. 1981;76:221–230. [Google Scholar]
- Rosero-Bixby L, Dow WH. Surprising SES Gradients in mortality, health, and biomarkers in a Latin American population of adults. J Gerontol B Psychol Sci Soc Sci. 2009;64(1):105–117. doi: 10.1093/geronb/gbn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons; 1987. [Google Scholar]
- Rutstein SO. The Demographic and Health Surveys (DHS) Wealth Index: Approaches for Rural and Urban Areas. Calverton, Maryland, USA: Demographic and Health Research, United States Agency for International Development; 2008. [Google Scholar]
- Signorello LB, Cohen SS, Williams DR, Munro HM, Hargreaves MK, Blot WJ. Socioeconomic status, race, and mortality: a prospective cohort study. Am J Public Health. 2014;104(12):e98–e107. doi: 10.2105/AJPH.2014.302156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- Stenholm S, Westerlund H, Head J, Hyde M, Kawachi I, Pentti J, Vahtera J. Comorbidity and functional trajectories from midlife to old age: the Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2015;70(3):332–338. doi: 10.1093/gerona/glu113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turra CM, Goldman N. Socioeconomic differences in mortality among U.S. adults: insights into the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2007;62(3):S184–192. doi: 10.1093/geronb/62.3.s184. [DOI] [PubMed] [Google Scholar]
- United Nations International Children's Emergency Fund. Country Statistics. [Retrieved December 15th, 2014];2008 www.unicef.org/infobycountry/niger_statistics.
- Uwakwe R, Ibeh CC, Modebe AI, Bo E, Ezeama N, Njelita I, Prince MJ. The epidemiology of dependence in older people in Nigeria: prevalence, determinants, informal care, and health service utilization. A 10/66 dementia research group cross-sectional survey. J Am Geriatr Soc. 2009;57(9):1620–1627. doi: 10.1111/j.1532-5415.2009.02397.x. [DOI] [PubMed] [Google Scholar]
- Velkoff VA, Kowal PR. Population aging in sub-Saharan Africa: Demo-graphic dimensions 2006. In: U.S. Census Bureau, editor. Current Population Reports. Washington, DC: U.S. Government Printing Office; 2007. [Google Scholar]
- Wang H, Dwyer-Lindgren L, Lofgren KT, Rajaratnam JK, Marcus JR, Levin-Rector A, Murray CJ. Age-specific and sex-specific mortality in 187 countries, 1970-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2071–2094. doi: 10.1016/S0140-6736(12)61719-X. [DOI] [PubMed] [Google Scholar]
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- World Health Organisation. The World Health Report 2008: primary health care- now or never. Geneva: World Health Organisation; 2008. [Google Scholar]
- World Health Organization. WHO-Disability Assessment Schedule II. Geneva, Switzerland: World Health Organization; 1999. [Google Scholar]