Increased pulse wave velocity (PWV) is associated with incidence of stroke and coronary diseases, independent of other cardiovascular risk factors [1], [2], [3]. Therefore, the measurement of PWV is recommended in many current guidelines for the management of hypertensive patients [4], [5]. Recently, we constructed a novel mathematical transformation function (TF) for central blood pressure (CBP) values estimated by non-invasive oscillometric blood pressure (BP) measurements [6]. In the present study, we reconstructed TF in coronary artery disease (CAD) patients, who have different arteriosclerotic characteristics from healthy subjects [7]. Furthermore, we examined whether there is association of PWV with estimated CBP and pulse pressure (PP), obtained by new constructed TF in CAD patients.
We recruited 70 consecutive CAD patients (male: n = 54 [77%] and female: n = 16 [23%], average: 70.7 ± 8.6 years old), who were referred to Kumamoto University Hospital and diagnosed by coronary angiography (CAG). The study protocol was in agreement with the guideline of the ethical committee of Kumamoto University, and written informed consent was obtained from each patient or the family of the subject. PWV values in CAD patients were measured on admission using a device for PWV/ABI Form (Omron Colin Co., Ltd., Tokyo, Japan). The method of PWV measurements was reported previously [8].
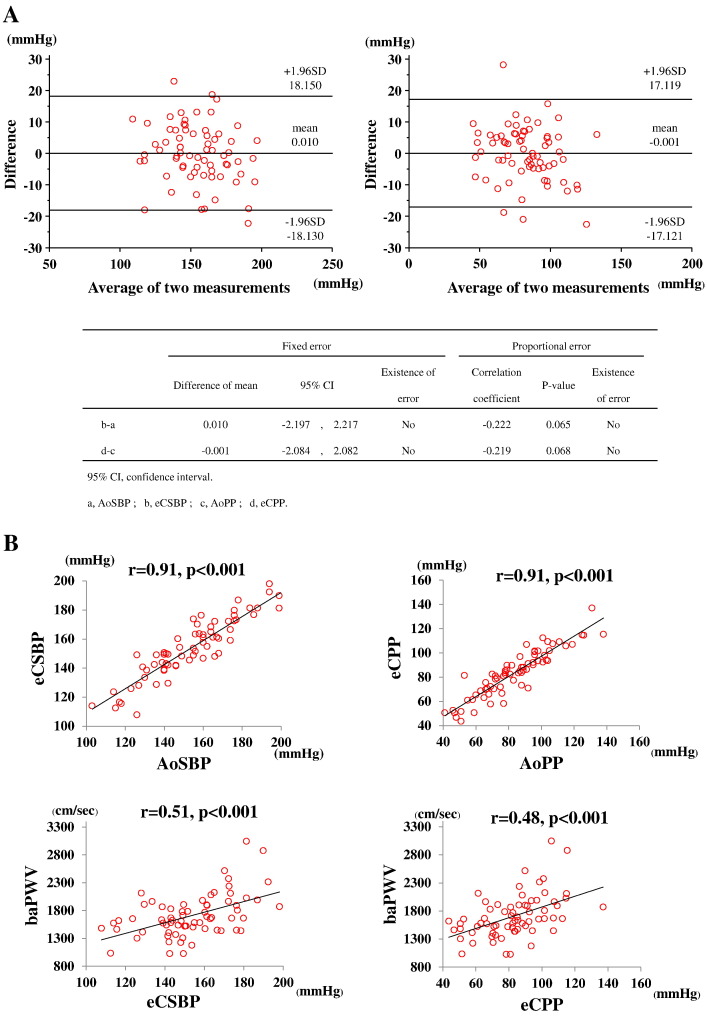
During heart catheterization, we measured CBP and constructed TF as reported previously [6]. Briefly, either a 5 or 6 French Judkins-type catheter (Togo Medikit, Hyuga, Japan) was placed into the ascending aorta of the patients, and the CBP was measured and recorded prior to the initial CAG and administration of any cardiovascular agents. Simultaneously with the measurement of CBP by a catheter, we wrapped a cuff around the left upper arm of supine-positioned patients and measured the brachial BP oscillometrically using a Pasesa AVE-1500 (Shisei Datum, Tokyo, Japan). We also measured an arterial velocity pulse index (AVI) [6] and an arterial pressure-volume index (API) [9] in CAD patients, and obtained TF between the invasive CBP values and non-invasive oscillometric BP values in each patient. We made a correlation matrix to investigate the correlation among several independent variables. The independent variables, which had significant correlations with aortic systolic BP (AoSBP) were age, systolic BP (= brachial BP, PSBP), diastolic BP (PDBP), AVI and API values obtained in this matrix. To examine multiple regression equation, we used AoSBP as a dependent variable and adopted the five above-mentioned variables as independent variables. We also adopted aortic pulse pressure (AoPP) as a dependent variable for the five independent variables: age, PSBP, pulse pressure (PPP), AVI and API. Using these statistical analyses, we obtained intercepts and coefficients for each independent variable and constructed the following formulas: estimated central SBP (eCSBP) = 0.1152 ∗ age + 0.7512 ∗ PSBP + 0.3095 ∗ PDBP + 0.1884 ∗ AVI + 0.4001 ∗ API − 0.1105, estimated central PP (eCPP) = 0.1496 ∗ age + 0.1088 ∗ PSBP + 0.7312 ∗ PPP + 0.2163 ∗ AVI + 0.3649 ∗ API − 12.3859. Data, analyzed using the method by Bland and Altman, revealed good agreement between AoSBP and eCSBP (mean difference: 0.010 ± 9.255) and between AoPP and eCPP (mean difference: − 0.001 ± 8.735) without any systematic bias (Fig. 1A). In addition, both correlations were not statistically different (r = − 0.222, p = 0.065 and r = − 0.219, p = 0.068, Fig. 1A upper left panel and upper right panel, respectively), indicating no statistical difference between both methods. Thus, we clearly demonstrated the accuracy of eCSBP and eCPP values calculated by TF of conventional non-invasive oscillometric BP measurements. Moreover, the estimated CSBP and CPP were significantly and strongly correlated with baPWV values (r = 0.51, p < 0.001 and r = 0.48, p < 0.001, respectively, Fig. 1B lower panel).
Fig. 1.
The correlations of estimated CBP with AoBP and baPWV
Panel A shows Bland–Altman plots between AoSBP and eCSBP (upper left panel), and AoPP and eCPP (upper right panel).
B upper panel shows the correlations between estimated CSBP and AoSBP (upper left panel), and between estimated CPP and AoPP (upper right panel).
B lower panel shows the correlations between estimated CSBP and baPWV (lower left panel), and between estimated CPP and baPWV (lower right panel).
CBP; central blood pressure, AoBP; aortic blood pressure, baPWV; brachial-ankle pulse wave velocity, CSBP; central systolic blood pressure, AoSBP; aortic systolic blood pressure, CPP; central pulse pressure, AoPP; aortic pulse pressure.
Augmentation index (AI) is also known to be an index of indicating vascular stiffness [10]. This tonometry method generally needs to measure BP pulse wave from body surface, so it is required to detect artery positions accurately and to press arteries which enable to make slightly flat position without occlusion of arteries. The tonometry methods are not always easy, and are prone to examiner-dependent manner. In this study, hence, we proposed new TFs estimating accurate CBP by oscillometric measurements, which have less measurement errors dependent on the examiner. Moreover, AI is generally influenced by aging, and it is less significant to monitor in the elderly [11]. Because the average age of patients in this study was 71 years old, AIs of these patients have possibility to reach a plateau. Hence, we further examined 13 relatively younger patients (less than 60 years old; male: n = 9 [69%]; average: 52.4 ± 10.5 years old), and applied TFs in relatively younger patients to examine the accuracy of these TFs. As a result, both estimated CSBP and CPP were significantly and strongly correlated with AoSBP and AoPP respectively (r = 0.86, p < 0.001 and r = 0.84, p < 0.001, respectively, figures not shown) also in these patients. Thus, we demonstrated the accuracy of estimated CSBP and CPP values, independent of aging. Furthermore, the brachial BP, aortic BP and eCSBP were 139.71 ± 20.5 mm Hg, 153.9 ± 22.3 mm Hg, and 153.9 ± 20.3 mm Hg, respectively, and these associations with baPWV were shown in Table 1. The associations of PWV with eCBP and eCPP were stronger than those with other BP parameters.
Table 1.
The relationships among brachial, aortic BP and eCSBP, and between baPWV and these BP parameters.
| Correlations | r value | p value |
|---|---|---|
| Brachial BP vs. eCSBP | 0.99 | p < 0.01 |
| Aortic BP vs. eCSBP | 0.91 | p < 0.01 |
| eCSBP vs. baPWV | 0.51 | p < 0.01 |
| Brachial BP vs. baPWV | 0.51 | p < 0.01 |
| Aortic BP vs. baPWV | 0.48 | p < 0.01 |
BP; blood pressure, baPWV; brachial-ankle pulse wave velocity, eCSBP; estimated central systolic blood pressure.
Increased CBP causes vascular wall stress in peripheral vessels, such as the cerebral, coronary and renal arteries, and accelerates atherosclerosis in these arteries, resulting in various cardiovascular diseases. As described above, accumulating clinical evidence showed a close association between CBP and the occurrence of cardiovascular diseases in CAD and other vascular diseases [12], [13]. Because direct CBP measurements are invasive procedures using a catheter, it is very useful to measure CBP in CAD patients precisely and non-invasively demonstrated in this study for risk stratification of CAD. Furthermore, PP, as well as PWV, is associated with adverse cardiovascular events in CAD patients [10]. This study demonstrated that not only eCSBP but also eCPP had strong correlation with PWV, indicating the accuracy eCPP values calculated by new TF in CAD patients. Moreover, there were strong and significant associations of PWV with eCSBP and eCPP, suggesting the clinical significance of estimated CBP by TF, which we firstly constructed.
In conclusion, the associations between PWV and the BP parameters were calculated by using new reconstructed TF, indicating the validity of these TFs in CAD patients.
Funding sources
None.
Potential conflict of interest
None.
Acknowledgments
We would like to thank Shin-ichiro Tatae, all paramedical staff, and all medical secretaries for their kind support during this study. We would like to thank Kazuo Watanabe in the Japan Medical Fund Corporation, Tokyo, Japan, for his technical support in the measurements of the equations.
References
- 1.Vlachopoulos C., Aznaouridis K., Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–1327. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 2.Vlachopoulos C., Aznaouridis K., Terentes-Printzios D., Ioakeimidis N., Stefanadis C. Prediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: a systematic review and meta-analysis. Hypertension. 2012;60:556–562. doi: 10.1161/HYPERTENSIONAHA.112.194779. [DOI] [PubMed] [Google Scholar]
- 3.Masugata H., Senda S., Yoshikawa K., Yoshihara Y., Daikuhara H., Ayada Y. Relationships between echocardiographic findings, pulse wave velocity, and carotid atherosclerosis in type 2 diabetic patients. Hypertens Res. 2005;28:965–971. doi: 10.1291/hypres.28.965. [DOI] [PubMed] [Google Scholar]
- 4.Mancia G., Fagard R., Narkiewicz K., Redon J., Zanchetti A., Bohm M. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31:1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 5.Shimamoto K., Ando K., Fujita T., Hasebe N., Higaki J., Horiuchi M. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014) Hypertens Res. 2014;37:253–390. doi: 10.1038/hr.2014.20. [DOI] [PubMed] [Google Scholar]
- 6.Sueta D., Yamamoto E., Tanaka T., Hirata Y., Sakamoto K., Tsujita K. The accuracy of central blood pressure waveform by novel mathematical transformation of non-invasive measurement. Int J Cardiol. 2015;189:244–246. doi: 10.1016/j.ijcard.2015.03.182. [DOI] [PubMed] [Google Scholar]
- 7.Hata J., Kiyohara Y. Epidemiology of stroke and coronary artery disease in Asia. Circ J. 2013;77:1923–1932. doi: 10.1253/circj.cj-13-0786. [DOI] [PubMed] [Google Scholar]
- 8.Yamashina A., Tomiyama H., Takeda K., Tsuda H., Arai T., Hirose K. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res. 2002;25:359–364. doi: 10.1291/hypres.25.359. [DOI] [PubMed] [Google Scholar]
- 9.Komine H., Asai Y., Yokoi T., Yoshizawa M. Non-invasive assessment of arterial stiffness using oscillometric blood pressure measurement. Biomed Eng Online. 2012;11:6. doi: 10.1186/1475-925X-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goto T., Ohte N., Fukuta H., Wakami K., Tani T., Kimura G. Relationship between effective arterial elastance, total vascular resistance, and augmentation index at the ascending aorta and left ventricular diastolic function in older women. Circ J. 2013;77:123–129. doi: 10.1253/circj.cj-12-0733. [DOI] [PubMed] [Google Scholar]
- 11.McEniery C.M., Yasmin, Hall I.R., Qasem A., Wilkinson I.B., Cockcroft J.R. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT) J Am Coll Cardiol. 2005;46:1753–1760. doi: 10.1016/j.jacc.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 12.Williams B., Lacy P.S., Thom S.M., Cruickshank K., Stanton A., Collier D. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113:1213–1225. doi: 10.1161/CIRCULATIONAHA.105.595496. [DOI] [PubMed] [Google Scholar]
- 13.Roman M.J., Devereux R.B., Kizer J.R., Lee E.T., Galloway J.M., Ali T. Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension. 2007;50:197–203. doi: 10.1161/HYPERTENSIONAHA.107.089078. [DOI] [PubMed] [Google Scholar]