Abstract
Mandibular skeletal deformities are mostly corrected by Sagittal Split Ramus Osteotomy. One of the main complications of Bilateral Sagittal Split Ramus Osteotomy is impairement of sensory function of Inferior Alveolar Nerve.
Objectives
To evaluate the occurrence of neurosensory disturbance by comparing the subjective and objective assessment of neurosensory responses after bilateral sagittal split ramus osteotomy.To assess the progress of recovery from the first post operative day till six months. To explain the factors causing neurosensory disturbances.
Method
A series of 24 patients with clinically and radiographically diagnosed mandibular skeletal deformity were treated with Bilateral Sagittal Split Ramus Osteotomy. For evaluation of the neurosensory responses, the parameters consist of subjective and objective test in order to compare the subjective and objective assessment.
Results
On the first post operative day neurosensory disturbances were seen in all the patients. Recovery of sensation was seen in all the patients at the end of this study.
Conclusion
The incidence of functional nerve disturbances is acceptable, since the progression towards recovery is inevitable. Prolonged neurosensory disturbance is greatly related to the degree of manipulation of the inferior alveolar nerve.
Keywords: Bilateral sagittal split ramus osteotomy, Orthognathic surgery, Neuro sensory evaluation of inferior alveolar nerve
1. Introduction
Bilateral Sagittal Split ramus osteotomy(BSSRO) is one of the most popular surgeries to correct mandibular skeletal deformities. Hullihen is regarded as the first surgeon to describe some type of mandibular orthognathic surgery.1 Sagittal split ramus osteotomy was first introduced by Schuchardt in 19422 in which he made a through and through cut in the body of the mandible and advanced. The pterigomasseteric sling was preserved and the fragments were stabilized with upper border wiring. After three weeks the mandible relapsed to its original position. In 19572 Trauner & Obwegeser described the procedure, in which, they made a medial horizontal cut just above the level of mandibular foramen and vertical cut on the anterior border of the ramus. The oblique cut was made on the angle of mandible. This technique was considered as a good procedure. But the bone contact was poor and aseptic necrosis was noted in the angle region due to extensive stripping of the pterigomasseteric sling. It was later modified by DalPont in 1961,3 who made the oblique cut on the molar region and found difficult with setbacks. Hunsuck in 1968,4 shortened the medial horizondal cut just posterior to the foramen which prevents the shattering the ramus in setback procedures. Gallo et al. in 1976,5 and Epker in 19776 made the anterior vertical cut involving the lower border of the mandible. The split was kept more laterally in order to separate the fragments easily and also provides greater protection for the inferior alveolar nerve. Blood supply for the fragments is also maintained by prevention of the pterigomasseteric sling stripping.
In BSSRO, the osteotomy is performed in close proximity to the inferior alveolar nerve (IAN) and therefore it will easily result in a postoperative neurosensory disturbance of the lower lip and7, 8 Postoperative paresthesia is generally considered to be caused by mechanical damage of the sensory fibers of the IAN. Conversely, paresthesia seems to occur even when the nerve remains visibly intact during the operative procedure.9, 10 To predict the prognosis of neurosensory disturbances before and after the surgery, more attention to the factors affecting neurosensory disturbances has to be evaluated. Furthermore, special care should be given to the exact site of the mandibular nerve in preventing and minimizing damage to the IAN during surgery. Apart from being the most versatile technique, transient neurosensory deficit remains the major disadvantage following the surgery.
At the end of long term follow-up Walter and Gregg in 197911 observed 100% of neurosensory disturbances in BSSRO cases in the subjective assessment. But objectively such disturbances were found only in 84.6% cases. Zaytoun in 198612 observed 68% in one year post-operative follow-up. Koblin and Reil in 197413 reported 73% of patients with normal sensation at the end of third year. Macintosh in 198114 reported only 9% of patients with residual paresthesia of the lower lip at the end of 1 year. Pepersack and Chausse in 197815 reported 64.2% of patients with, altered sensation in the lower lip. But all these reports implied large discrepancies when simultaneous objective analysis was done. However, studies reported recently show a decreasing incidence of neurosensory deficits in general.
In clinical follow-up, there is an urgent need for bedside methods to test the neurosensory disturbance after BSSRO. In prevention of neurosensory disturbance following BSSRO, more knowledge is required regarding the different factors causing sensory disturbance. Hence the target of this study is to assess neurosensory response after Bilateral Sagittal Split Ramus Osteotomy by regular follow up for a maximum period of six months.
2. Aims and Objectives
-
1.
To notice the occurrence of neurosensory disturbance on the lower lip and chin after bilateral sagittal split ramus osteotomy.
-
2.
Comparison of subjective and objective assessment of neurosensory responses following bilateral sagittal split ramus osteotomy.
-
3.
Assessment of the progress of the recovery from the first post operative day till six months.
-
4.
To describe the factors causing neurosensory disturbances after bilateral sagittal split ramus osteotomy.
3. Materials and methods
A total of twenty four patients with clinically and radiographically diagnosed mandibular skeletal deformity were treated with Bilateral Sagittal Split Ramus Osteotomy in the Department of Oral and Maxillofacial surgery, from 2009 to 2013.
Among the 24 patients (Table 1), 16 patients were males and 8 were females. Preoperative assessment of all these 24 patients showed absolutely no history of trauma and sensory disturbances in any form. Orthopantomogram was taken for all the 24 patients to locate the mandibular canal position and also the third molar status. Lateral cephalometric radiograph was taken for all the patients and Burstone cephalometric analysis was carried out.
Table 1.
Total number of patients.
| Sl. No | Procedure | Males | Females | Total |
|---|---|---|---|---|
| 1 | BSSRO | 14 | 6 | 20 |
| 2 | Lefort 1 osteotomy + BSSRO | 2 | 0 | 2 |
| 3 | Anterior maxillary osteotomy + BSSRO | 0 | 2 | 2 |
| Total | 24 | |||
General anaesthesia was administrated with naso endotracheal intubation. The surgical technique carried out for all the patients were Hunsuck's medial short lingual split and Epker's lower border split. Intra operative inferior alveolar nerve encounter was recorded (Table 2) and fixation of the osteotomised fragments was done by mini plates with mono cortical screws. None of the patients had an unfavourable split, undue hemorrhage and hence no blood transfusion was required during the surgery.
Table 2.
Nerve encounter during surgery.
| Nerve Status | Right Side |
Left Side |
||
|---|---|---|---|---|
| Nil | Yes | Nil | Yes | |
| Nerve Not Seen | 8 | 16 | 12 | 12 |
| 33.33% | 66.67% | 50.00% | 50.00% | |
| Nerve Seen in Distal Fragment | 20 | 4 | 16 | 8 |
| 83.30% | 16.70% | 66.67% | 33.33% | |
| Nerve Transected and Sutured | 24 | 0 | 24 | 0 |
| 100.00% | 0.00% | 100.00% | 0.00% | |
| Nerve Dissected from Proximal Fragment | 20 | 4 | 20 | 4 |
| 83.30% | 16.70% | 83.30% | 16.70% | |
| Chi Square | 16.001 | 8.889 | ||
| P value | <0.01 | <0.05 | ||
Reviews were planned on the first postoperative day, first week, first month, third month, and sixth month.,All the patients were reviewed for occlusion, neurosensory function and profile changes during these visits. Panaromic radiographs were taken for all the patients to assess the position of the fixation screws in relation to the mandibular canal.
The subjective assessment includes, i) Tingling sensation. ii) Numbness. iii) Altered sensation. iv) Absence of sensation in the lower lip and in the chin region. During every follow-up, each patient was asked to complete a questionnaire indicating if they had any alterations in sensation of their lower lip or in the mental region of the skin.
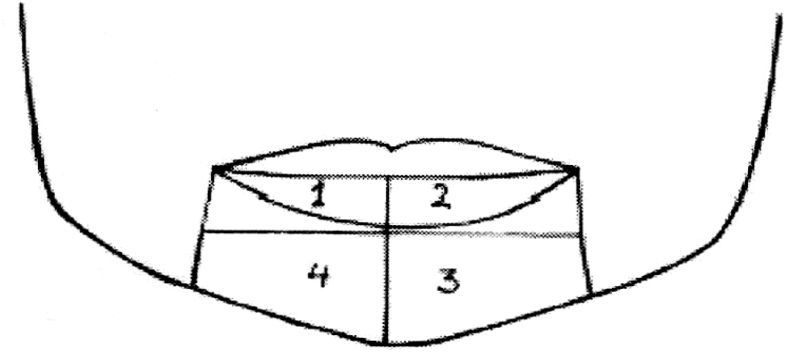
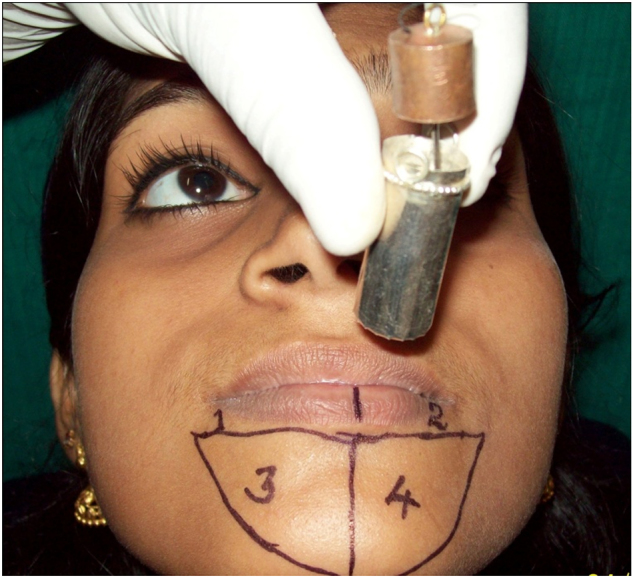
After obtaining the subjective test results, objective tests were conducted. Patients were seated and relaxed comfortably in the dental chair. Four separate zones were marked in the lower lip and chin region (Fig. 1).
Fig. 1.
Four zones for testing of nerve function.
The upper two zones indicate the areas innervated by labial branch of inferior alveolar nerve and the lower two zones denote the areas, innervated by mental branch of inferior alveolar nerve. Each zone was measured separately. Test was performed over a one centimeter area above and beneath the labio-mental fold on both sides of the chin. Each of the four facial zones was stimulated three times; a correct response was considered two out of the three appropriate responses. During the test, patients were asked to close their eyes and separate their lips comfortably.
Five distinctive tests were carried out for the assessment of mechanoceptive and nociceptive responses, and finally the sensitivity test was done.
I. Mechanoceptive tests.
1. Light touch.
-
a)
Static light touch
-
b)
Brush directional stroke
2. Static two point discrimination.
II Nociceptive tests.
1. Pin pressure nociception.
2. Thermal discrimination test.
-
a)
Hot test
-
b)
Cold test
3.1. Mechanoceptive tests.
3.1.1. Light touch
-
a)
Static light touch:- The instrument used for testing light touch is a camel hair brush (Fig. 2). This test assesses the integrity of the cells which are innervated by myelinated afferent A-Beta axons. These receptors adapt slowly, and their putative sensory modality is pressure. The large myelinated A Beta fibers are highly susceptible to compression injury.
Fig. 2.
Instrument for testing light touch.
3.2. Method
Patient is placed in comfortable and relaxed position with eyes closed. The hair tuft is applied in the chosen zones. Stimulus is indicated to the examiner by the patient by raising a finger. The results of each test should be compared with those obtained from the normal site like infra orbital region.
-
a)
Brush directional stroke: This is a test of proprioception and assesses the integrity of large A – Alpha and A-Beta myelinated axons. The sensory modalities are vibration, touch and flutter.The same device which is used for static light touch is used. The brush is moved from right to left or vice versa. The stroke should be for 1 cm and repeated 3 times in each zone. The patient is asked to imply the direction of stroke. Atleast 2 out of 3 correct responses were considered as normal response.
3.2.1. Static two point discrimination (2-P)
This test assesses the quantity and density of functional sensory receptors and afferent fibers. If sharp points are used, the small myelinated A-Delta and unmyelinated C fibers are assessed. If blunt points are used, the larger myelinated A-Alpha fibers are assessed.
3.3. Method
Each zone was measured with a sharp millimeter caliper. The test was conducted by beginning with the points closed and progressively opening them in 1 mm increments until the patient could discriminate two separate points of contact. This distance was then recorded. Care was taken to ensure that the points touched the cutaneous surface at the same time. Distances two millimeters greater than the preoperative value were considered abnormal (Fig. 3).
Fig. 3.
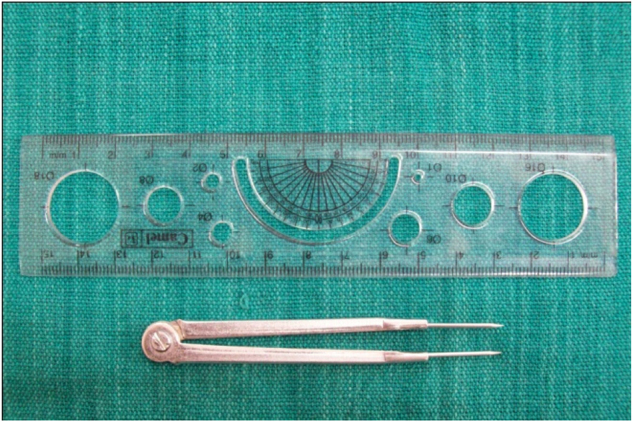
Instruments for testing two point discrimination.
3.4. Nociceptive tests
3.4.1. Pin pressure nociception (PIN).
This test assesses the free nerve endings and small myelinated A-Delta and C fibers that innervate the free nerve endings responsible for nociception. In PIN, each zone was measured with needles weighting from 0.5 g to 15 g. A set of needles were constructed for this investigation (Fig. 4). The needles pressed the measured zone through the loop by their own weight. To ensure this, the needles were hung on a thread and allowed to pass freely through the loop and touch the tested zone. The lightest needle that the patient felt sharp was then recorded (Fig. 5, Fig. 6). If the difference from preoperative value was more than 1 g, the result was estimated as abnormal.
Fig. 4.
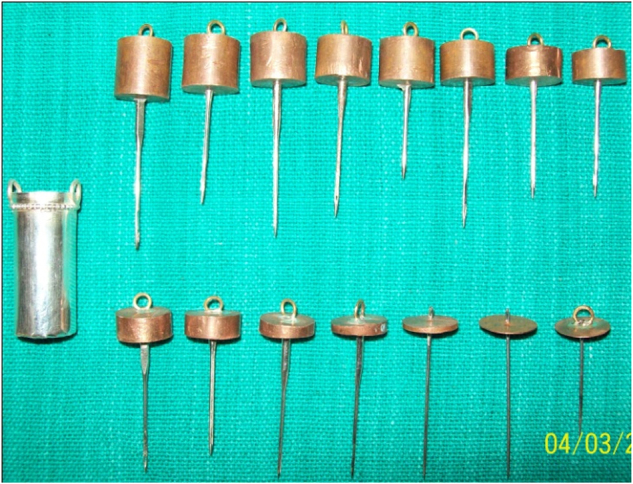
Specially fabricated set of needles weighing 0.5 g to 15 g and the loop.
Fig. 5.
Patient tested for pin pressure nociception.
Fig. 6.
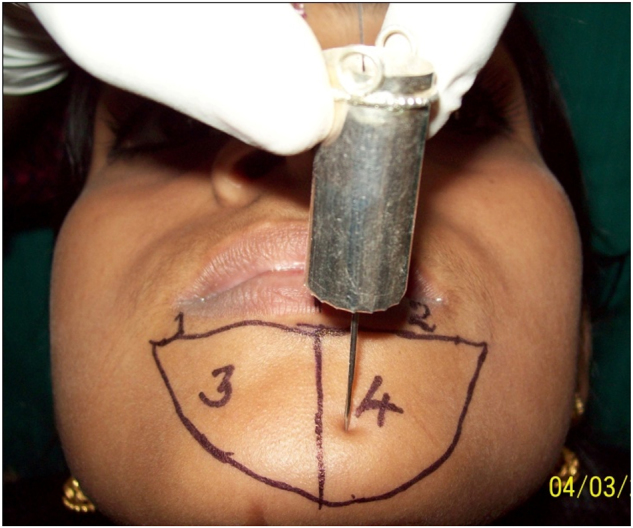
Needle suspended and passed passively through the loop to touch the patient by its weight.
3.4.2. Thermal Discrimination test
This is a useful test of sensation. It assesses integrity of small myelinated and unmyelinated fibers. Warmth sensation is attributed to A-Delta fibers and Cold to C fibers.
-
a)
Cold discrimination.
A small glass test tube containing water at 15 °C is placed on the selected zone.This is repeatedly done three times in each zone and the response is considered positive if two correct answers of cool/cold or normal/not–cold or mere touch is obtained.
-
•
Hot discrimination.
A small glass test tube containing water at 50 °C is placed in the chosen areas. The patient is asked to indicate whether they felt a hot, cold, or merely a touch.
In the sensitivity test, the sensitivity of all the mandibular teeth on the right and left side of the mandible were measured by using “DIGI TEST”; Pulp Vitality Tester (Model No. D 626 D, Parkell Electronics, NewYork, USA). The scale of the vitality tester was from 0 to 64. The first measurement of each tooth was recorded. The teeth that failed to respond to the sensitivity test preoperatively were excluded as well as the third molars. The sensitivity was estimated to be postoperatively normal if all the preoperatively included teeth on the side reacted positively to the sensitivity test. If one or more teeth did not react positively to the sensitivity test, the result was recorded as abnormal.
The tests were conducted in an outpatient setup using the equipments which were made as per the standardization recommended by various authors in their literature.16, 17, 18
Data were analyzed using computer software, Statistical Package for Social Sciences (SPSS) version 10 and are expressed in its frequency and percentage. To elucidate the associations and comparisons between different parameters, Chi square (χ2) test was used as nonparametric test. For all statistical evaluations, a two-tailed probability of value, <0.05 was considered significant.
4. Results
4.1. Subjective test results
4.1.1. Tingling Sensation
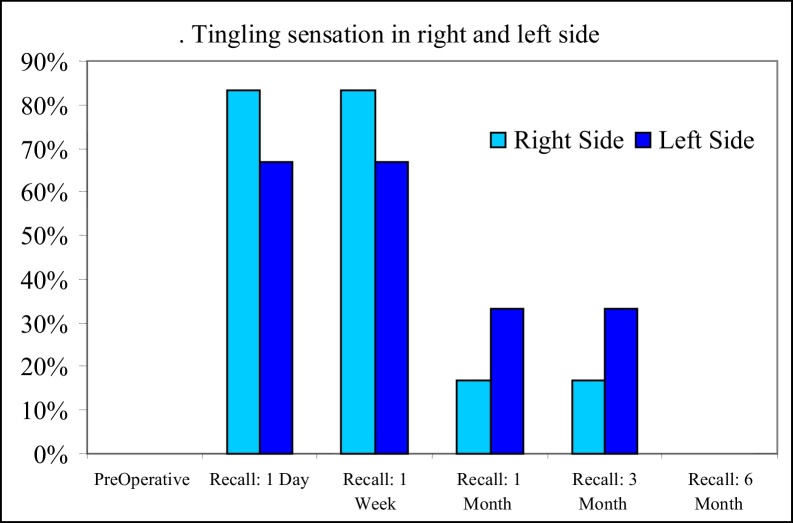
On the first post operative day, 20 patients (83.30%) had tingling sensation, 16 bilaterally (66.70%) and 4 on the right side (16.70%) (Table 3 & Fig. 7). At the end of the first week the results remained unchanged. At the end of the first month, 4 patients (16.70%) had tingling sensation on the right side and 8 patients (33.30%) had tingling on the left side. The observations remained same till the end of third month. By sixth month no patient has tingling sensation. The test is significant with p value < 0.001.
Table 3.
Tingling sensation subjective test.
| Tingling Sensation Observation | Right Side |
Left Side |
||
|---|---|---|---|---|
| Nil | Yes | Nil | Yes | |
| PreOperative | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Recall: 1 Day | 4 | 20 | 8 | 16 |
| 16.70% | 83.30% | 33.30% | 66.70% | |
| Recall: 1 Week | 4 | 20 | 8 | 16 |
| 16.70% | 83.30% | 33.30% | 66.70% | |
| Recall: 1 Month | 20 | 4 | 16 | 8 |
| 83.30% | 16.70% | 66.70% | 33.30% | |
| Recall: 3 Month | 20 | 4 | 16 | 8 |
| 83.30% | 16.70% | 66.70% | 33.30% | |
| Recall: 6 Month | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Chi Square | 42.000 | 24.00 | ||
| p value | <0.001 | <0.001 | ||
Fig. 7.
Tingling sensation in right and left side.
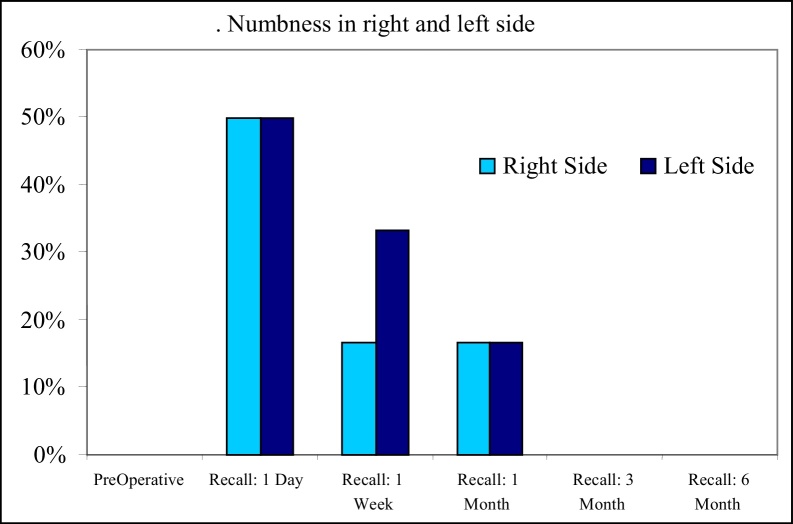
4.1.2. Numbness
50% of patients complained of numbness on the right side and 50% on the left side on the first post operative day (Fig. 3). In the first week, 4 patients (16.70%) had numbness on the right side and 8 patients (33.3%) had numbness on the left. At the end of first month, 4 patients (16.70%) had numbness on the right side alone and 4 patients (16.70%) on the left side alone. At three months post operatively the numbness resolved completely for all the patients (Table 4 & Fig. 8).
Table 4.
Numbness subjective test.
| Numbness Observation | Right Side |
Left Side |
||
|---|---|---|---|---|
| Nil | Yes | Nil | Yes | |
| PreOperative | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Recall: 1 Day | 12 | 12 | 12 | 12 |
| 50.00% | 50.00% | 50.00% | 50.00% | |
| Recall: 1 Week | 20 | 4 | 16 | 8 |
| 83.30% | 16.70% | 66.70% | 33.30% | |
| Recall: 1 Month | 20 | 4 | 20 | 4 |
| 83.30% | 16.70% | 83.30% | 16.70% | |
| Recall: 3 Month | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Recall: 6 Month | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Chi Square | 19.045 | 19.002 | ||
| p value | <0.01 | <0.01 | ||
Fig. 8.
Numbness in right and left side.
None of the patients complained of Burning sensation, Altered sensation or No sensation throughout the entire study.
4.2. Objective test results
4.2.1. Light touch
The light touch test was found to be significant (P < 0.001) before and after surgical intervention. Before the surgery all 24 patients (100%) had light touch sensation on both right and left lip. After surgery, within 24 hours, the light touch sensation had reduced to 4 patients (16.7%) and 20 patients (83.3%) had no light touch sensation in both right and left lip. After one week, majority of the patients had light touch sensation. 16 patients (66.7%) had light touch sensation in the right lip and 12 patients (50%) had sensation in left lip after one week of surgery. The light touch sensation increased to 83.3% and 66.7% in right and left lip respectively during first and third month of follow up. All the 24 patients (100%) had light touch sensation in both sides of the lip during 6th month of follow up. In the chin region, 4 patients had light touch sensation on the first post operative day. This increased to 83.3% on the right and to 50.0% on the left at the end of first month. At the third month of recall 50.0% had sensation on the right chin, where as 100% had sensation on the left.
4.2.2. Brush directional stroke
The brush directional stroke test was found to be significant (P < 0.001) before and after surgical intervention. Before surgery all 24 patients (100%) had brush directional stroke on both right and left lip. One day after surgery the brush directional stroke sensation had reduced to 8 patients (33.3%) on either side. After one week, it increased to 50 .0% on the left and remained the same on the right lip. At the end of first month 50.0% patient retained the sensation on left side, where as on the right side it decreased to 16.70%. At the end of third month 83.3% could detect the direction of stroke on either side of the lip. The values raised 100% on either side at the end of sixth month.
In the chin region, 8 patients had sense of direction on the right and left side on the 1st operative day which increased to 66.7% at the end of first week. At the end of first month 66.7% could detect the direction on the right chin where as 83.3% detected the direction on the left chin. The values raised to 100% at the end of third month and remained the same through out the study.
4.2.3. Static two point discrimination.
Preoperatively, all the 24 patients could discriminate between 2 points of simultaneous contacts both in chin and lip region At the end of first day 4 patients (16.7%) had two point discrimination on the right side and 8 patients on the left side of lip. At the first week follow up, 66.7% could differentiate two points on the right lip and 50.0% on the left lip. At the first month it rose to 83.3% on right lip and remained the same on the left. In the third month recall the value was 50% and 66.7% on the right and left lip respectively. At six month recall all the 24 patients could differentiate two points of contacts on right side where as only 20 patients (83.3%) on the left side.
In the chin region only 4 patients could differentiate 2 points on the right chin where as 8 patients differentiate on the left side. At the end of first week 50.0% of patients could differentiate 2 points on either side. The values raised to 66.70% on the first month. The values increased to 83.3% on the right side and remained the same throughout. Values on left remained as 66.7% from the first month, till the end of study.
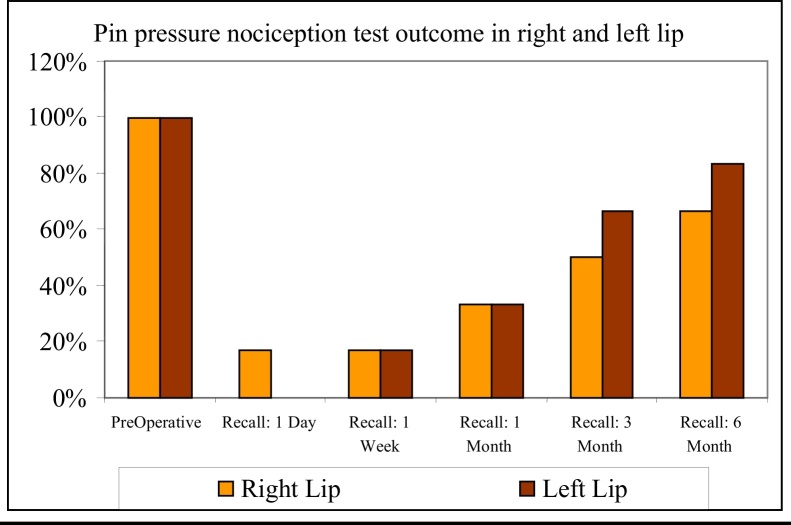
4.2.4. Pin pressure nociception
All the 24 patients responded positively for Pin pressure nociception test pre operatively. In the first post op day only 4 patients responded positively on the right lip. On the left side all the 24 patients did not respond at all. At the end of first week a positive response of 16.7% was obtained on the either side of the lip. At one month recall this value increased to 33.3% on either side. At 3rd month the value was 50.0% on the right and 66.7% on the left. At the final recall the value was 63.7% on right and 83.3% on the left side. The test showed high significance with p value < 0.001 (Table 5 & Fig. 9).
Table 5.
Pin Pressure Nociception Observations-(LIP).
| Pin Pressure Nociception Observations | Right Lip |
Left Lip |
||
|---|---|---|---|---|
| Nil | Yes | Nil | Yes | |
| PreOperative | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Recall: 1 Day | 20 | 4 | 24 | |
| 83.30% | 16.70% | 100.00% | ||
| Recall: 1 Week | 20 | 4 | 20 | 4 |
| 83.30% | 16.70% | 83.30% | 16.70% | |
| Recall: 1 Month | 16 | 8 | 16 | 8 |
| 66.70% | 33.30% | 66.70% | 33.30% | |
| Recall: 3 Month | 12 | 12 | 8 | 16 |
| 50.00% | 50.00% | 33.30% | 66.70% | |
| Recall: 6 Month | 8 | 16 | 4 | 20 |
| 33.30% | 66.70% | 16.70% | 83.30% | |
| Chi Square | 25.189 | 37.000 | ||
| p value | <0.001 | <0.001 | ||
Fig. 9.
Pin pressure nociception test outcome in right and left lip.
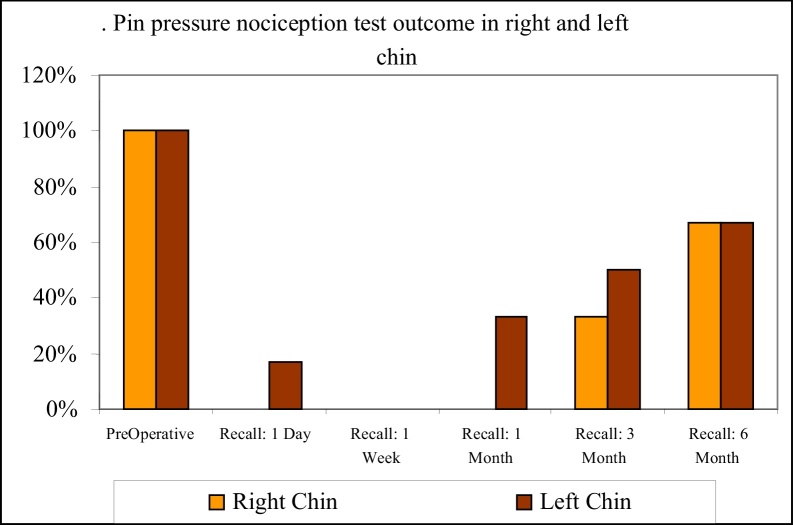
In the chin region, no patient responded to this test on the right side where as 4 patients (16.7%) responded positively on the left. In the first week follow up no patients responded. At end of one month 8 patients (33.3%) responded on the left side and no response was seen on the right side. At three months follow up, the values were 33.7% at the right and 50.0% on the left sides respectively. At the final recall the value increased to 66.7% on either side (Table 6 & Fig. 10).
Table 6.
Pin Pressure Nociception Observations. (Chin).
| Pin Pressure Nociception Observations | Right Chin |
Left Chin |
||
|---|---|---|---|---|
| Nil | Yes | Nil | Yes | |
| PreOperative | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Recall: 1 Day | 24 | 20 | 4 | |
| 100.00% | 83.30% | 16.70% | ||
| Recall: 1 Week | 24 | 24 | ||
| 100.00% | 100.00% | |||
| Recall: 1 Month | 24 | 16 | 8 | |
| 100.00% | 66.70% | 33.30% | ||
| Recall: 3 Month | 16 | 8 | 12 | 12 |
| 66.70% | 33.30% | 50.00% | 50.00% | |
| Recall: 6 Month | 8 | 16 | 8 | 16 |
| 33.30% | 66.70% | 33.30% | 66.70% | |
| Chi Square | 48.000 | 31.500 | ||
| p value | <0.001 | <0.001 | ||
Fig. 10.
Pin pressure nociception test outcome in right and left.
4.2.5. Thermal Test
All the patients responded to both cold and hot discrimination test pre operatively. In the lip region, at the first post op day, 16.7% identified the hot sensation on the right side where as 33% identified on the left side. The value gradually rose to 66.7% on the right side and 100% on the left side. In the chin region, at the end of 6th month, 66.7% of patients could identify the hot temperature on either side. Cold sensation was correctly identified on the lip region by 83.3% patients at the 6th month follow up on either side. In the chin region 66.7% patients identified cold sensation on the right side and 50.0% on the left at 6 months.
4.2.6. Sensitivity test
In Sensitivity test all the patients responded positively in the pre op period. At the first post op day only 4 patients responded positively and the values remained as 33.30% on either side till the end of first month. At the end of sixth month all patients responded on the right side and only 20 patients responded on the left side.
5. Discussion
Transient neurosensory deficit is the commonest complication of Bilateral Sagittal Split Ramus Osteotomy (BSSRO), due to intraoperative manipulation of the inferior alveolar nerve, traction during mobilisation of the osteotomised fragments, postoperative edema and compression of nerve by fixation devices.
On the first post operative day of this study, almost all of the patients had bilateral neurosensory deficit. The subjective assessment was reevaluated and objective tests were conducted. On the first post operative day, 85% of the patients did not respond to light touch test and the static two point discrimination was 15 mm. Similarly, pin pressure nociception test was negative for 85% of patients and 25% patients indicated a slight response for hot and cold touch.
The return of neurosensory response was seen in all the 24 patients at the end of six months.,The neurosensory response returned to the presurgical situation in almost all the patients by six months, irrespective of type of nerve damage during osteotomy. In a study conducted by L.George Upton19, he found recovery of sensitivity in all of his patients within 8 months and neuropraxia was found to be recovered within several days to a week.
In our study, 16 patients (66.7%) responded to static light touch test on the first postoperative week. Among these patients, the inferior alveolar nerve was not seen during surgery. At the end of one week 66.7% did not respond to brush directional stroke. Such diminished neurosensory response to brush directional stroke is due to surgical edema and absence of such a response on the first week is not indicative of sensory disorder because of the higher percentage presence of static light touch.
At the end of first post op day, 4 patients who responded for light touch also responded for pin pressure nociception test. Static two point discrimination test showed 10 mm on the lower lip and 15 mm on the chin.
As per the literature,20, 2 factors that are believed to produce a neurosensory deficit are fixation devices,[21], 22 age of the patient, magnitude of movement of the osteotomised fragments etc. We compared all the variables that can alter the neurosensory response except age.
In this study, the role of age could not be assessed because all the 24 patients were aged 18–27 years. The other factors like intra operative nerve manipulation, magnitude of movement of the osteotomised fragments and position of the monocortical screws (by assessing with OPG) were taken into account and compared with the post surgical neurosensory function.
In this study, the degree of intraoperative nerve manipulation played a vital role in the neuro sensory recovery. In all the 16 patients the nerve was not at all seen intraoperatively, showed rapid recovery of neurosensory function (ie. within one month). Subjectively they reported tingling sensation in the lower lip and chin on the first postoperative day, which lasted for 3 weeks. At the end of one month, they had absolutely no complaints. Objective analysis correlated with subjective information are given. Light touch (both static and brush directional stroke) test showed positive results and static two point discrimination showed 10s mm in the lower lip and 15 mm in the chin. The remaining 8 patients, wherein the nerve was seen intraoperatively and nerve was manipulated, reported reduced sensation subjectively and poor objective responses. However, they regained their sensation at various intervals of time.
All the 24 patients were radiographically examined using OPG. Six patients seemed to have screws adjacent to the mandibular canal. The rest of the 18 patients had the screws totally separated from the mandibular canal.
Masaki Fujioka and Akiyoshi Hirano et al.,22 compared neurosensory disturbance and restoration after BSSRO, in monocortical screws versus bicortical screw fixation. They found the group of patients with monocortical screw fixation showed markedly less incidence of neurosensory deficit which recovered completely at the end of the 12th month.
In our study, only monocortical screws were used in all the 24 patients and post operative OPG showed no screw impingement of the mandibular canal. Hence the neurosensory deficit due to screw impingement has been ruled out.
The response to thermal discrimination was excellent and it is the first function that recovered. John Eric Bloomquist17 supports this concept of rapid progression of recovery of thermal stimuli due to faster regeneration of A delta small myelinated sensory fibers. Thermal discrimination test may be positive when all other tests showed impaired sensitivity.
Mobilisation of the osteotomised fragment is one of the contributing factors which plays vital role in neurosensory deficit. Various authors22, 23, 24 suggest different methods for assessing the neurosensory function after orthognathic surgery. Based on the reliability of the tests,difference of opinion was seen among them.
Somatosensory evoked potential was described by Ghali, Jones et al.,16 which is a non-invasive electrophysiological study of the conduction of the nerve impulse along central and peipheral pathways. This method is considered a standard and reliable objective method to assess the nerve injury. But the major drawback of this is that the extent of the nerve injury cannot be determined. This method requires equipment of higher cost and needs expert recording and interpretation. Also the microneurosurgical repair of nerve cannot be monitored using this technique.
Alex R. McDonald and Timothy Pogrel25 suggested the usage of magneto encephalography as an objective monitor for evaluation of the post-traumatic inferior alveolar nerve injuries. Using this non-invasive somatosensory monitoring of injured inferior alveolar nerve with magnetic source imaging showed appropriate cortical signal in response to repetitive lip stimulation. This test helps to differentiate between intact but damaged nerves and transacted nerves.
Hence this study outlines the extent of nerve injury grossly and progression of recovery. The recovery of sensation after BSSRO seems to be dependent on the extent of the nerve injury, magnitude of the mobilisation of the osteotomised fragments, position of the fixation screws in relation to the mandibular canal and age of the patient. Gregg et al. stated that a transected inferior alveolar nerve with a gap of >15 mm will not recover its function without interpositional nerve grafting using another nerve (greater auricular/sural nerve). However in our study no cases of nerve transected were reported and all the cases reported prompt neurosensory recovery.
Impairment of sensory function of inferior alveolar nerve after Bilateral Sagittal Split Ramus Osteotomy (BSSRO) is not always avoidable. Neurosensory disturbances were seen in all the patients on the first post operative day. Severe symptoms like pain & burning sensation was not experienced by any of the patients. Correlation of subjective symptoms and objective evaluation showed absolute coincidence, i.e. there was no false positive or negative correlation. Type of intra operative nerve manipulation, magnitude of the mobilisation of osteotomised fragments, position of the fixation screws in relation to the mandibular canal were observed as the contributing factors for neurosensory deficit. Recovery of sensation was seen in all the patients at the end of this study.
6. Conclusion
To conclude, the incidence of functional nerve disturbances is acceptable, since the progression towards recovery is inevitable. After BSSO, a prolonged neurosensory disturbance is greatly related to the degree of manipulation of the inferior alveolar nerve. Hence the risk of this transient complication should not defer the use of sagittal split ramus osteotomy technique while it is otherwise indicated.
Contributor Information
P.G. Antony, Email: drpgantony@yahoo.com.
Aneesh Sebastian, Email: draneesh2008@gmail.com.
K. George Varghese, Email: georgekunthara@gmail.com.
References
- 1.Steinhauser E.W. Historical development of orthognathic surgery. J Cranio Maxillofac Surg. 1996;24:195–204. doi: 10.1016/s1010-5182(96)80002-3. [DOI] [PubMed] [Google Scholar]
- 2.Ylikontiola Leena, Kinnunen Jorma, Oikarinen Kyosti. factors affecting neurosensory disturbance after mandibular sagital split osteotomy. J Oral Maxillofac Surg. 2000;58:1234–1239. doi: 10.1053/joms.2000.16621. [DOI] [PubMed] [Google Scholar]
- 3.Dalpont G. Retromolar osteotomy for correction of prognathism. J Oral Surg Anesth Hosp D Serv. 1961;19:42. [PubMed] [Google Scholar]
- 4.Hunsuck E.E. A modified intraoral sagittal splitting technique for correction of mandibular prognathism. J Oral Maxillofac Surg. 1968;26:250. [PubMed] [Google Scholar]
- 5.Gallo W.J., Mosses M., Gaul J.V. Modification of the sagittal ramus split osteotomy for retrognathia. J Oral Maxillofac Surg. 1976;34:178. [PubMed] [Google Scholar]
- 6.Epker B.N. Modification in the sagittal osteotomy of the mandible. J Oral Maxillofac Surg. 1977;35:157. [PubMed] [Google Scholar]
- 7.Behrman S.J. Complications of sagittal osteotomy of the mandibular ramus. J Oral Surg. 1972;30:554–561. [PubMed] [Google Scholar]
- 8.Yoshida T., Nagamine Kobayashi Michimi N., Nakajima T., Sasakura H., Hanada K. Impairment of the inferior alveolar nerve after sagittal split osteotomy. J Craniomaxillofac Surg. 1989;17:271–278. doi: 10.1016/s1010-5182(89)80095-2. [DOI] [PubMed] [Google Scholar]
- 9.Westermark A., Bystedt H., Konow von L. Inferior alveolar nerve function after sagittal split osteotomy of the mandible: correlation with degree of intraoperative nerve encounter and other variables in 496 operations. BJOMFS. 1998;36:429–433. doi: 10.1016/s0266-4356(98)90458-2. [DOI] [PubMed] [Google Scholar]
- 10.Westermark A., Bystedt H., Von Konow L. Inferior alveolar function after Mandibular Osteotomies. BJOMFS. 1998;36:425–428. doi: 10.1016/s0266-4356(98)90457-0. [DOI] [PubMed] [Google Scholar]
- 11.Walter J.M., Jr., Gregg J.M. Analysis of postsurgical neurologic alteration in the trigeminal nerve. J Oral Surg. 1979;37:410–414. [PubMed] [Google Scholar]
- 12.Zaytoun H.S., Jr, Phillips C., Terry B.C. Long-term neurosensory deficits following transoral vertical ramus and sagittal split osteotomies for mandibular prognathism. J Oral Maxillofac Surg. 1986;44(3):193–196. doi: 10.1016/0278-2391(86)90107-2. [DOI] [PubMed] [Google Scholar]
- 13.Koblin I., Reil B. Sensitivity of the lower lip after protection or resection of the inferior alveolar nerve in progenia operations. Fortschr Kiefer Gesichtschir. 1974;18:151–154. [PubMed] [Google Scholar]
- 14.MacIntosh R.B. Experience with the sagittal osteotomy of the mandibular ramus: a 13-year review. J Maxillofac Surg. 1981;9(3):151–165. doi: 10.1016/s0301-0503(81)80036-7. [DOI] [PubMed] [Google Scholar]
- 15.Pepersack W.J., Chausse J.M. Long term follow-up of the sagittal splitting technique for correction of mandibular prognathism. J Maxillofac Surg. 1978;6(2):117–140. doi: 10.1016/s0301-0503(78)80079-4. [DOI] [PubMed] [Google Scholar]
- 16.Ghali G.E., Bruce Epker Clinical Neurosensory testing. J Oral Maxillofac Surg. 1989:1074–1078. doi: 10.1016/0278-2391(89)90184-5. [DOI] [PubMed] [Google Scholar]
- 17.Blomquist J. Eric. Per alberius, Stein/Sakssan, Predictability of neurosensory response of inferior alveolar nerve after sagittal split osteotomy, Journal of. Plastic and Reconstructive Surgery. 1998;102:325–333. doi: 10.1097/00006534-199808000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Robinson P.P., Smith K.G., Johnson F.P. Equipments & methods for sensory testing. J Oral Maxillofac Surg. 1992;30:387–389. doi: 10.1016/0266-4356(92)90206-x. [DOI] [PubMed] [Google Scholar]
- 19.Upton L.George, Rajvanakarn Manus, Hayward James R. Evaluation of the regenerative capacity of the inferior alveolar nerve following surgical trauma. J Oral Maxillofac Surg. 1987;45(3):217–222. doi: 10.1016/0278-2391(87)90117-0. [DOI] [PubMed] [Google Scholar]
- 20.Hirsch J.M., Branemark P.I. Fixture stability and nerve function after transposition and lateralization of the inferior alveolar nerve and fixture installation. BJOMFS. 1995;33:276–281. doi: 10.1016/0266-4356(95)90037-3. [DOI] [PubMed] [Google Scholar]
- 21.Bouman, Husak, Putman Screw fixation after SSRO for mandibular advancement. BJOMFS. 1995;33:231–233. [Google Scholar]
- 22.Masaki, Fugioka, Tohrufujii Comparative study of Inferior Alveolar nerve disturbance after SSRO. J Plast Recon Surg. 1997;4:37–41. [Google Scholar]
- 23.Feldman J.A., Essick G.K., Zuniga J.R. Inter examiner reliability of three subjective clinical neurosensory tests. Int J Adult Orthodontics Orthognathic Surg. 1997;12:273–285. [Google Scholar]
- 24.Zuniga John R., Meyer Roger A., Miloro M. The accuracy of clinical nuerosensory testing for nerve injury diagnosis. J Oral Maxillofac Surg. 1998;56:2–8. doi: 10.1016/s0278-2391(98)90904-1. [DOI] [PubMed] [Google Scholar]
- 25.Alex R., Mcdonald, Timothy P.L. Noninvasive somatosensory monitoring of the injured inferior alveolar nerve using magnetic source imaging. JOMFS. 1996;54:1068–1072. doi: 10.1016/s0278-2391(96)90161-5. [DOI] [PubMed] [Google Scholar]