Abstract
OBJECTIVES:
The objective of this study is to evaluate the impact of two educational interventions that are demonstration versus pictorial Leaflet in patients using metered-dose inhaler (MDI).
MATERIALS AND METHODS:
This interventional study was done in patients who were prescribed drugs through MDI at Tuberculosis and Chest Department. The patients were enrolled in Group A or Group B as per random number table method. The method of use of MDI was assessed using a checklist based on the technique described in the WHO Guide to good prescribing. Patients in Group A were taught the use of MDI by demonstration of the technique by the investigator. Patients in Group B were educated about the technique by a pictorial leaflet based on the technique. Patients were followed up after 15 days and assessed for correct technique for use of the MDI.
RESULTS:
A total 100 patients were included in the study and were allotted to Group A (47) and Group B (53). Ninety-five percent of the patients had been taught by the treating physician about the method of use of MDI. All the patients at the baseline placed the lips tightly around the mouthpiece and held the aerosol as indicated in the manufacturer's instructions while the step least followed was coughing up the sputum before inhalation. The average steps correctly followed by the patients in Group A and B at baseline were 5.17 ± 2.07 and 5.11 ± 2.04, respectively. These improved significantly to 9.19 ± 0.67 and 6.67 ± 0.63 in Group A and B, respectively, postintervention. The five essential steps of using MDI were followed by 25.53% and 26.41% patients preintervention. An improvement in the technique of use of MDI was observed in 85.11% and 49.06% patients (P = 0.003) postintervention. All the ten steps of the technique were followed by 34.04% patients from Group A and none from Group B at postintervention evaluation (P = 0.0001).
CONCLUSION:
The inhalation technique for the use of MDI used by the patients is inappropriate. Educational interventions such as demonstration or pictorial leaflet help ensure a better use of the MDI.
Keywords: Bronchial asthma, chronic obstructive pulmonary disease, educational intervention, metered-dose inhaler
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) are estimated to affect about 300 million and 210 million people worldwide, respectively.[1] Asthma has become one of the major public health burdens with increasing prevalence in the developing countries.
Drug administration using metered-dose inhaler (MDI) device is the mainstay of therapy in asthma and COPD. The device offers advantages such as convenience, portability, and quick local action. It is affordable and causes less systemic adverse effects.[2] A major factor governing the efficiency of inhalation medication is the technique of inhalation. Appropriate inhalation technique is crucial for optimum delivery of drug to the airways.[3] Patients with asthma and COPD admitted in emergency departments are found to demonstrate a high level of improper MDI technique suggesting a correlation between poor technique and emergency visits.[4] The efficacy of the medicine decreases and the symptoms aggravate due to inappropriate technique.[5]
Owing to lack of knowledge and complexity of inhalation technique, a high rate of inappropriate inhalation technique has been reported from the previous studies. The method of inhalation technique was correct in only 65.5% patients in a study carried out by Şen et al.[6] and 36.3% in a study carried out by Chauhan et al.[7]
The WHO recommends the following sequential steps for use of MDI, of which those marked (*) are the essential steps:[8]
Cough up as much sputum as possible
Shake the aerosol before use*
Hold the aerosol as indicated in the manufacturer's instructions (this is usually upside down)
Place the lips tightly around the mouthpiece*
Tilt the head backward slightly
Breathe out slowly, emptying the lungs of as much air as possible*
Breathe in deeply and activate the aerosol, keeping the tongue down
Hold the breath for ten to fifteen seconds*
Breathe out through the nose*
Rinse the mouth with water.
Successful asthma management depends10% on medication and 90% on education. Lack of patient education about inhalation technique leads to erroneous inhalation which contributes to morbidity and mortality in these patients.[9] Thus, patient education is a key component of asthma management. Educational initiatives have shown to improve the accuracy of inhalation technique.[5] Asthma education empowers patients to manage their disease and increase their awareness about complications. Different education methods for MDI administration technique include verbal and written instructions, physical demonstration, illustrations, audio-visual demonstration and internet based, interactive, and multimedia tutorials.[10]
There are a few studies done to evaluate the deficiencies in the technique of use of MDI. Such information is essential to plan an educational protocol for the patients using MDI. Hence, this study was done to evaluate the technique used by patients using the MDI and to evaluate the impact of two different educational interventions on this technique. The study was planned in patients of asthma or COPD.
Materials and Methods
This was a prospective, continuous, interventional, comparative study conducted at the outpatient department (OPD) of tuberculosis and chest disease (TBCD) of a tertiary care hospital in Ahmedabad. Prior permission was obtained from the Institutional Ethics Committee and from the Head TBCD of the hospital. Adult patients (>18 years) who were diagnosed to suffer from asthma or COPD and were prescribed inhalational drugs using MDI were screened and enrolled after obtaining the written informed consent. Pregnant women and children, patients having respiratory disease other than asthma and COPD, and those who were not prescribed drugs that required the use of MDI were excluded from the study. In the preinterventional phase, the investigator attended the OPD and enrolled the patients. The demographic details such as age, gender, smoking habits, educational status, monthly income, duration of disease, duration of treatment, details of drug treatment, and frequency of hospitalization were recorded. Patient's knowledge about the disease, frequency of demonstration of use of inhaler technique by the doctor and the method of demonstration was recorded. The patient was provided a dummy MDI with an empty canister and was asked to demonstrate the inhalation technique to the investigator. The technique was scored as per a checklist based on the ten steps of use of MDI recommended by the WHO. An MDI administration technique comprises ten steps, of which five are essential. A score of 1 was assigned to each step performed correctly whereas a wrongly performed step was allotted a score 0. During the interventional phase, the patients were randomized into two groups, i.e., Group A and Group B using computer generated random number tables. A week after, the initial baseline assessment, patients in Group A were taught the technique of use of MDI for drug administration by the investigator who demonstrated the technique to the patient. The queries of the patient if any were answered by the investigator. Similarly, for patients in a Group B, the investigator showed a pictorial leaflet with pictures about the use of MDI along with detailed instructions for its use. The pictorial leaflet was prepared by the investigator and validated in a pilot study conducted among 10 healthy controls, 5 of who were literate, and 5 illiterate. The patients were encouraged to raise any query about the use of MDI. The patients were asked to return 15 days postintervention and instructed to demonstrate the steps of using the MDI. The patients were evaluated and scored in the same manner as the preintervention phase.
Statistical analysis
The data were entered in Microsoft Excel 2007 and analyzed using GraphPad Instat 3. Data were analyzed using Student's t-test (paired and unpaired), Chi-square test, and Fisher's exact test. P < 0.05 was considered statistically significant.
Results
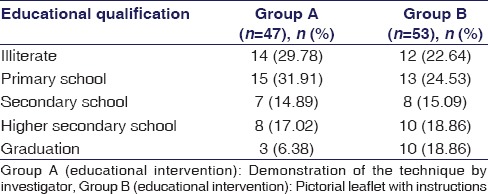
This was an interventional study carried out in patients suffering from bronchial asthma (BA) or COPD, who were prescribed drugs that required the use of MDI. A total 100 patients were included in the study and divided into two groups using computerized random number tables. A total of 47 patients were included in Group A, of which 32 patients were of COPD, and 15 patients were of BA. A total of 53 patients were included in Group B, of which 33 patients were of COPD, and 20 patients were of BA. The mean age of patients in Groups A and B was 49.47 ± 1.95 years and 44.70 ± 2.19 years, respectively. No significant difference was found (P > 0.05) in the mean age of the two groups. The M:F ratio was 2.6:1 in Group A and 2.1:1 in Group B. Fourteen (29.78%) and 20 (37.73%) patients in Groups A and B, respectively were smokers. The educational qualification of the patients in both groups is mentioned in Table 1.
Table 1.
Educational qualification of the patients using metered-dose inhaler (n=100)
Of the 100 patients, 31 (65.95%) from Group A and 29 (54.71%) patients from Group B had sedentary occupation while 16 (34.04%) and 22 (41.50%) patients had nonsedentary occupations, respectively. Duration of diagnosis of disease was 5.93 ± 0.91 years in Group A and 4.15 ± 0.69 years in Group B. Most commonly prescribed drug in Group A was ipratropium bromide + salbutamol sulfate (36.17%), followed by budesonide + formoterol (31.56%), levosalbutamol + ipratropium bromide (19.15%), tiotropium bromide (4.26%), fluticasone propionate + formoterol fumarate (4.26%), and formoterol + tiotropium bromide (2.13%). The most commonly prescribed drug in Group B was budesonide + formoterol (37.74%), followed by fluticasone propionate + formoterol fumarate (18.87%), ipratropium bromide + salbutamol sulfate (15.09%), tiotropium bromide (9.44%), formoterol + tiotropium bromide (3.78%), and salbutamol (3.78%).
The physician had demonstrated the MDI technique while prescribing the inhaler in 95.74% and 100% patients in Group A and B, respectively. The average frequency of demonstration was 1.85 ± 0.10 and 1.62 ± 0.09 times per year for Group A and B, respectively. Patients who had actually performed the technique in front of the physician were 24 (51.06%) and 21 (44.68%) in Group A and B, respectively.
The steps of MDI administration technique correctly followed by patients in Group A and Group B during the pre- and post-intervention are illustrated in Figures 1 and 2, respectively.
Figure 1.
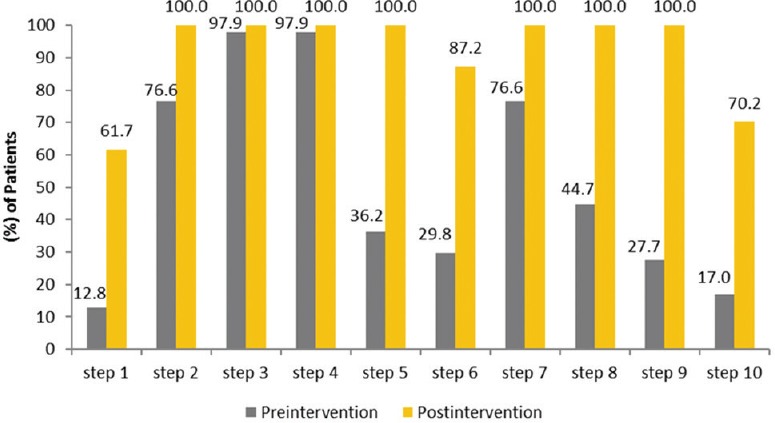
Steps of metered-dose inhaler administration technique correctly followed by patients at the pre- and post-intervention in Group A (n= 47). Group A: Educational intervention: Demonstration of the technique of MDI administration by the investigator, pairedt-test,P< 0.0001
Figure 2.
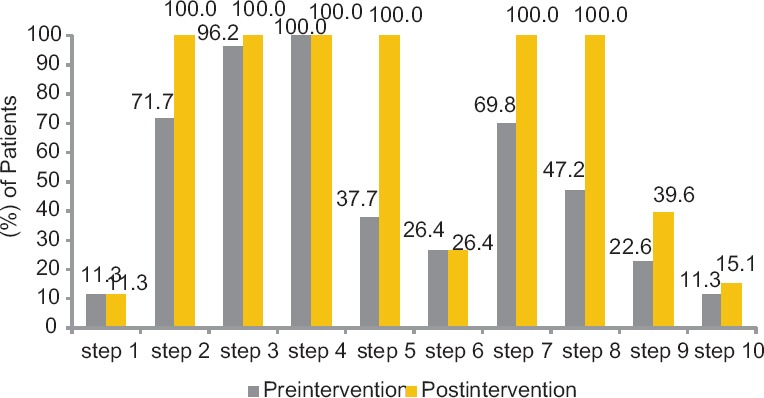
Steps of metered-dose inhaler administration technique correctly followed by the patients at the pre- and post-intervention in Group B (n= 53). Group B: Educational intervention: Pictorial leaflet with instructions shown to the patients, test-Pairedt-test,P< 0.001
The most commonly followed steps were Step 3 of “holding the aerosol as indicated in the manufacturer's instruction” (100%) and Step 4 of “placing the lips tightly around the mouthpiece” (100%) in Group A. The least followed step was Step 1 (12.77%), i.e., “cough up as much sputum as possible before starting the inhalation” and Step 10 “Rinse the mouth with water.” The average number of steps followed correctly at preintervention in Group A was 5.17 ± 0.30. The score improved to 9.19 ± 0.09 at postintervention (P < 0.001), thereby suggesting that this educational intervention improved the technique of using the MDI.
The steps followed correctly by most patients in Group B were Step 4, i.e., placing the lips tightly around the mouthpiece (100%), followed by Step 3 i.e., “hold the aerosol as indicated in the manufacturer's instructions” (96.23%). The least followed steps were Step 1 and Step 10 (11.32%) “cough up as much sputum as possible” and “rinse the mouth with water.” Step 9, i.e., to breathe out through the nose was better followed by the patients in demonstration Group. In Group A, the step was followed by 13 patients in the preintervention phase which improved to 47 patients in the postintervention phase. While in Group B, 12 patients followed the steps correctly which increased to 21 patients in the postintervention phase. When both the Groups were compared for accuracy of Step 9 in the postintervention phase, a significant improvement was observed in Group A as compared to Group B (P < 0.001, Chi-square test).
The average steps followed at preintervention and postintervention in Group B were 5.11 ± 0.29 and 6.67 ± 0.09, respectively, p < 0.001, (Paired t-test). The average number of steps correctly followed at preintervention were similar in both Groups (Group A = 5.17 ± 0.30 and Group B = 5.11 ± 0.28, P = 0.8843, unpaired t-test).
During the postintervention phase, the average number of steps correctly followed by patients of Group A were significantly higher as compared to patients of Group B (Group A = 9.19 ± 0.10 vs. Group B = 6.67 ± 0.09, P < 0.001, unpaired t-test).
The 5 important essential steps of MDI technique followed by patients of Group A and Group B at the pre- and post-intervention are illustrated in Figure 3.
Figure 3.
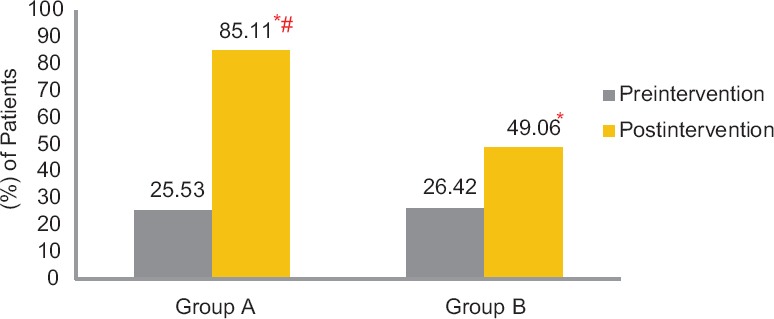
Five important essential steps for the use of metered-dose inhaler followed by patients in the pre- and post-intervention phase (n= 100). Group A: Educational intervention: Demonstration of the technique of MDI administration by the investigator. Group B: Educational intervention: Pictorial leaflet with instructions shown to the patients. Group A: Preintervention versus postintervention (*P= 0.001, Chi-square test). Group B: Preintervention versus postintervention (*P= 0.027, Chi-square test). Preintervention: Group A versus Group B (P> 0.05, Chi-square test). Postintervention: Group A versus Group B (#P= 0.003, Chi-square test)
Twelve patients (25.53%) in Group A followed all 5 essential steps at preintervention. Postintervention, 40 (85.11%) patients followed all these steps (P < 0.001). In Group B, 14 (26.41%) patients followed all 5 essential steps at preintervention. After educational intervention, 26 (49.05%) patients followed all these steps (P = 0.0275). At preintervention, no significant difference was observed between the number of patients following the 5 essential steps for using the MDI in Group A and B (P > 0.05), however, at the postintervention 40 patients from Group A and 26 patients from Group B, followed all the 5 essential steps for using the MDI (P = 0.003).
No patient from Group A followed all the ten steps at preintervention, however, 16 (34.04%) patients followed all the ten steps at postintervention (P < 0.001) as compared to preintervention. In Group B, no patient followed all the ten steps at preintervention as well as at the postintervention. During postintervention, 16 patients from Group A and 0 patients from Group B followed all the ten steps. A number of patients following all the ten steps in postintervention phase were significantly higher in Group A as compared to Group B (P = 0.0001, Fisher's exact test).
When the education level of the patient was compared with the correct technique of use of MDI administration it was observed that 14 patients from illiterate Group (n = 26) and 38 patients from literate Group (n = 74) followed all the 5 essential steps after educational intervention (P = 0.0047, Chi-square test). The method of use of MDI has been significantly improved after educational intervention in illiterate Group. At preintervention, 1 patient followed all the 5 essential steps, and after educational intervention, 14 patients followed all the 5 essential steps (P < 0.0001, Fisher's exact test). Eleven illiterate patients (n = 14) in Group A and three illiterate patients (n = 12) in Group B followed all the five essential steps postintervention. A significant improvement was observed in number of illiterate patients of Group A who followed the five essential steps as compared to those in Group B (P = 0.01, Fisher's exact test).
Discussion
Improper and inaccurate inhalation technique complicates the management of asthma. It is a major factor that determines the efficacy of inhalation medications. Many asthma educational programs are developed for use in hospitals, health-care centers, offices, and schools to improve overall health of patients of asthma.[11] Few studies have evaluated the deficiencies in the technique of use of MDI in the Indian population. In our study, we aimed to evaluate the technique of use of MDI and assess the impact of educational interventions on the inhalation technique. Different education methods for MDI administration technique include verbal and written instructions, physical demonstration, illustrations, audio-visual demonstration and Internet-based, interactive, and multimedia tutorials.[10] Although there are multiple educational methods to improve the technique, demonstration by the physician is the only method used in practice, and that too is done only in the initial months at the time of starting the treatment. We used demonstration technique and a pictorial leaflet with verbal and written instructions regarding the technique for use of MDI for two groups of patients. These methods are feasible, easily understandable, and economical and hence were included in the study.
The majority of patients in our study used an improper inhalation technique at the preintervention. Similar results have been observed in the previous studies, which showed that 77.5% to 89.2% of patients use an improper technique for inhalation.[12,13] The majority of patients in our study (95.7%) were instructed by the physician regarding the use of inhaler, which is more than that reported by Larsen et al. (63%)[12] and Jolly et al. (58.8%).[14] Inspite of this, the technique actually used by the patients was faulty. This shows need of education about the inhalation technique while prescribing the MDI.
At preintervention phase, none of our patients performed MDI administration technique accurately (10/10 score) as per the WHO recommendations. A greater number of patients followed Step 3 (holding the aerosol as indicated in the manufacturer's instruction) and Step 4 (placing the lips tightly around the mouthpiece) in both Groups during preintervention phase. This increased marginally in the postintervention phase. The possible reason is that these patients observe pictures and pictorial leaflets showing the technique of holding the device, and hence, these two steps are performed correctly. Similar results have been observed in Foland et al. study, in which 92% of patients held the aerosol correctly and 88% of patients placed the mouthpiece correctly. Similarly, a study carried out by Chauhan et al., 98.4% of patients followed the step to place the lips tightly around the mouthpiece and 94.3% of patients held the aerosol correctly.[7,15] A greater number of patients followed Step 1 (cough up as much sputum as possible) in Group A (demonstration Group) during the postintervention as compared to Group B (pictorial leaflet Group). This may be because, during demonstration, the investigator had instructed the patient to demonstrate this step and helped the patient understand the importance of this step in clearing their airway to ensure better drug efficacy. Clearing the airway before inhalation increases the bioavailability of the drug The Step 2, i.e., “Shake the aerosol before use” was improved in both groups. This step is easy to remember once demonstrated or observed in a pictorial leaflet. An improvement was observed in Step 5, i.e., “tilt the head backward slightly” in demonstration group than the pictorial leaflet group. Tilting the head backward slightly is also an important step that prevents tongue obstructing the upper airways and causing opening of the airways. Thus, more drug could reach the lower alveoli. A greater number of patients followed Step 6 (breathe out slowly, emptying the lungs of as much air as possible) in demonstration group after patients were educated about this step. Step 7 (breathe in deeply and activate the aerosol, keeping the tongue down) and Step 8 (hold the breath for 10–15 s) were also improved in both groups. Patients were made aware of the importance of these steps in enhancing entry of the drug. Step 9 (breathe out through the nose) was better followed by the patients of demonstration group. This was a significant correction in step as in the preintervention patients were observed to breathe in and out of the mouth instead of the nose. Thus, demonstration of the technique helps improve this step. Step 10 (rinse the mouth with water) was followed by a greater number of patients of demonstration group since the investigator appraised them of the importance of water gargles in removing residual drug in the pharynx. Similar results were observed in studies conducted by Virchow et al., Basheti et al., Foland et al., and Chauhan et al.[2,7,15,16]
The mean score during preintervention was 5 in both groups. The score improved significantly in both groups (P < 0.0001). The improvement was better in the patients in whom the technique was demonstration as compared to those who were shown the pictorial leaflet (P < 0.0001). These findings are consistent with the previous studies, where physical demonstration of the technique achieved better results than written and verbal information.[14,17]
Only 25.53% patients from demonstration group and 26.41% patients from pictorial leaflet group followed all the five important essential steps of the technique of use of MDI at the preintervention which is lower than that reported by Şen et al. (65.5%).[6] This might be because of the ignorance or lack of proper instructions by the physician.[18] Educational intervention improved the scores in both groups and a significantly greater number of patients followed all the essential steps of use of MDI. The demonstration of technique of use of MDI had a better impact as an educational intervention than the use of instructional pictorial leaflets. While both the interventions significantly improved the accuracy of technique among both literate and illiterate patients, the illiterate patients benefited better by demonstration of the technique rather than the use of pictorial leaflet.
A single demonstration session had a better impact in achieving full score (34.04%) than that reported by Jolly et al. (24%) study.[14] A study conducted by Bosnic-Anticevich et al. also showed a significant improvement in the technique of use of MDI in the demonstration group. In the above-said study, a complete score was achieved by 80% patients from demonstration group as compared to 10% patients from written and verbal instructions (P < 0.05).[17] Thus, while an educational intervention may improve the technique of use of MDI, the demonstration of the technique is better in improving accuracy of the technique than use of instructional pictorial leaflets.
The study findings are consistent with the previous studies, in which better improvement was observed in the patients educated by demonstration of the technique group than through written and verbal information.[19,20] This difference is due to the fact that, some steps of MDI inhalation technique are difficult to understand and require higher skill development and understanding, which is better achieved when patients closely observe the steps being demonstrated than reading about them. During physical demonstration, the patient is more attentive, observes all the steps, and attempts to replicate them.[19,20]
This study provides useful information about different errors committed by patients using the MDI and possible interventions to correct these errors. An appropriate educational intervention will hence help correct the inhalational technique and ensure better drug delivery. This study had certain limitations. A larger sample size would be helpful for a more conclusive result. A single postintervention evaluation was done in this study. Subsequent evaluations are required to determine if the impact of interventions is sustained and whether reinforcement is necessary. Nonetheless, the findings of this study reiterate the need for better patient education regarding appropriate use of the technique of the use of MDI, particularly in the illiterate and semiliterate population. It also helps plan appropriate educational interventions to improve the use of MDI.
Conclusion
Appropriate use of MDI is vital for the delivery of accurate amount of asthma medications. Incorrect use of inhaler technique is observed in patients. Educational interventions especially, demonstration of the technique reduces the errors in inhalation technique for the use of MDI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Chronic Respiratory Diseases. [Last accessed on 2014 Apr 22]. Available from: http://www.who.int/gard/publications/chronic_respiratory_diseases.pdf .
- 2.Virchow JC, Crompton GK, Dal Negro R, Pedersen S, Magnan A, Seidenberg J, et al. Importance of inhaler devices in the management of airway disease. Respir Med. 2008;102:10–9. doi: 10.1016/j.rmed.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 3.Dolovich MB, Ahrens RC, Hess DR, Anderson P, Dhand R, Rau JL, et al. Device selection and outcomes of aerosol therapy: Evidence-based guidelines: American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest. 2005;127:335–71. doi: 10.1378/chest.127.1.335. [DOI] [PubMed] [Google Scholar]
- 4.Hesselink AE, Penninx BW, Wijnhoven HA, Kriegsman DM, van Eijk JT. Determinants of an incorrect inhalation technique in patients with asthma or COPD. Scand J Prim Health Care. 2001;19:255–60. doi: 10.1080/02813430152706792. [DOI] [PubMed] [Google Scholar]
- 5.Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105:930–8. doi: 10.1016/j.rmed.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Şen E, Gönüllü U, Ekici Z, Kurşun N. Assessment of inhaler technique and treatment compliance of hospitalized patients and outpatients in a university hospital. Ankara Üniv Tıp Fak Mecm. 2006;59:1–6. [Google Scholar]
- 7.Chauhan A, Patel P, Gandhi A, Desai M. An evaluation of Metered-Dose inhaler administration technique in patients of asthma and chronic obstructive pulmonary disease. JAPS. 2016;6:115–8. [Google Scholar]
- 8.de Vries TP, Henning RH, Hogerzeil HV, Fresle DA. Guide to Good Prescribing. A Practical Manual. 1994. [Last accessed on 2015 Sep 19]. Available from: http://www.apps.who.int/medicinedocs/pdf/whozip23e/whozip23e.pdf .
- 9.Giraud V, Allaert FA, Roche N. Inhaler technique and asthma: Feasability and acceptability of training by pharmacists. Respir Med. 2011;105:1815–22. doi: 10.1016/j.rmed.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Nimmo CJ, Chen DN, Martinusen SM, Ustad TL, Ostrow DN. Assessment of patient acceptance and inhalation technique of a pressurized aerosol inhaler and two breath-actuated devices. Ann Pharmacother. 1993;27:922–7. doi: 10.1177/106002809302700721. [DOI] [PubMed] [Google Scholar]
- 11.Kelly CS, Shield SW, Gowen MA, Jaganjac N, Andersen CL, Strope GL. Outcomes analysis of a summer asthma camp. J Asthma. 1998;35:165–71. doi: 10.3109/02770909809068204. [DOI] [PubMed] [Google Scholar]
- 12.Larsen JS, Hahn M, Ekholm B, Wick KA. Evaluation of conventional press-and-breathe metered-dose inhaler technique in 501 patients. J Asthma. 1994;31:193–9. doi: 10.3109/02770909409044826. [DOI] [PubMed] [Google Scholar]
- 13.Thompson J, Irvine T, Grathwohl K, Roth B. Misuse of metered-dose inhalers in hospitalized patients. Chest. 1994;105:715–7. doi: 10.1378/chest.105.3.715. [DOI] [PubMed] [Google Scholar]
- 14.Jolly GP, Mohan A, Guleria R, Poulose R, George J. Evaluation of metered dose inhaler use technique and response to educational training. Indian J Chest Dis Allied Sci. 2015;57:17–20. [PubMed] [Google Scholar]
- 15.Foland AP, Stern T, Ramacciotti T, Martin J, Gilbert I, Cohn RC, et al. Improvement of Metered-Dose inhaler administration technique: The effect of training sessions at a specialized pediatric asthma compliance and technique clinic. Curr Ther Res Clin Exp. 2002;63:142–7. [Google Scholar]
- 16.Basheti IA, Natsheh AI, Ammari WG, Khater S, Qunaibi EA, Bosnic-Anticevich SZ. Education on correct inhaler technique in pharmacy schools: Barriers and needs. Trop J Pharm Res. 2015;14:715–22. [Google Scholar]
- 17.Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: The effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47:251–6. doi: 10.3109/02770900903580843. [DOI] [PubMed] [Google Scholar]
- 18.Interiano B, Guntupalli KK. Metered-dose inhalers. Do health care providers know what to teach? Arch Intern Med. 1993;153:81–5. doi: 10.1001/archinte.153.1.81. [DOI] [PubMed] [Google Scholar]
- 19.van der Palen J, Klein JJ, Kerkhoff AH, van Herwaarden CL, Seydel ER. Evaluation of the long-term effectiveness of three instruction modes for inhaling medicines. Patient Educ Couns. 1997;32(1 Suppl):S87–95. doi: 10.1016/s0738-3991(97)00100-6. [DOI] [PubMed] [Google Scholar]
- 20.Lindgren S, Bake B, Larsson S. Clinical consequences of inadequate inhalation technique in asthma therapy. Eur J Respir Dis. 1987;70:93–8. [PubMed] [Google Scholar]


