Abstract
We present a 21-year-old female whose clinical presentation and investigations were suggestive of takotsubo cardiomyopathy. On cardiac MRI, there was delayed gadolinium enhancement in apical and mid-segments with sparing of the base. Patient is in class III symptoms with ejection fraction of 24% at 1 year follow-up. This variant form of takotsubo cardiomyopathy with delayed contrast enhancement is associated with irreversible left ventricular dysfunction and poor outcome.
Background
Takotsubo cardiomyopathy is a reversible form of cardiomyopathy, which has a favourable outcome.1 The classical cardiac MR (CMR) finding in this condition is the absence of delayed contrast enhancement. We present an uncommon variant form of takotsubo cardiomyopathy, which is characterised by extensive myocardial necrosis and delayed gadolinium enhancement on CMR imaging. This report highlights not only the prognostic value of CMR but also the poor outcome associated with this variant form of stress cardiomyopathy.
Case presentation
A 21-year-old female had intermittent anginal type of chest pain for 2 days. She did not consult any doctor for the same. This episode was followed by breathlessness, which progressed from class II to IV over 2 month’s duration. On admission, she was dyspnoeic with heart rate of 110/min and blood pressure of 90/60 mm Hg. Cardiac examination revealed elevated jugular venous pressure, S3 gallop and bilateral basal crepitaions. There was no history of diabetes, hypertension or any family history of coronary artery disease (CAD). She does not smoke or consume alcohol. One week prior to the onset of chest pain, she had appeared for her university examinations, which was a stressful phase. There was no history of febrile illness in the preceding 6 months.
Investigations
The baseline blood investigations including thyroid and lipid profiles were normal. Cardiac biomarkers (creatine phosphokinase-muscle band, troponins) were not elevated. Screening test for pheochromocytoma was negative. Her electrocardiogram showed evolved inferolateral myocardial infarction pattern (figure 1). Echocardiography revealed dilated left ventricle (LV) (with the ejection fraction (EF) of 24%) with hypercontractile basal segments and apical ballooning (figure 2) (video 1). Her coronary angiogram was normal. A diagnosis of takotsubo cardiomyopathy was made as the patient fulfilled the modified Mayo clinic diagnostic criteria.2 Rest Technetium-99m sestamibi scan showed fixed perfusion defects confined to mid and apical segments (figure 3). CMR imaging confirmed the apical ballooning (figure 4) (video 2) but showed delayed enhancement of gadolinium in the entire thinned out apical and mid-segments with sparing of the base (figure 5).
Figure 1.
Electrocardiogram showing Q waves in LII, III, aVf, V4–V6, with ST coving in V4–V6, which is suggestive of evolved inferolateral myocardial infarction.
Figure 2.
Echocardiogram in apical four-chamber view, demonstrating the contraction in basal segments with ballooning of the apex.
Figure 3.
Rest technetium-99m sestamibi scan showing fixed perfusion defects involving the entire mid and apical segments with sparing of the base.
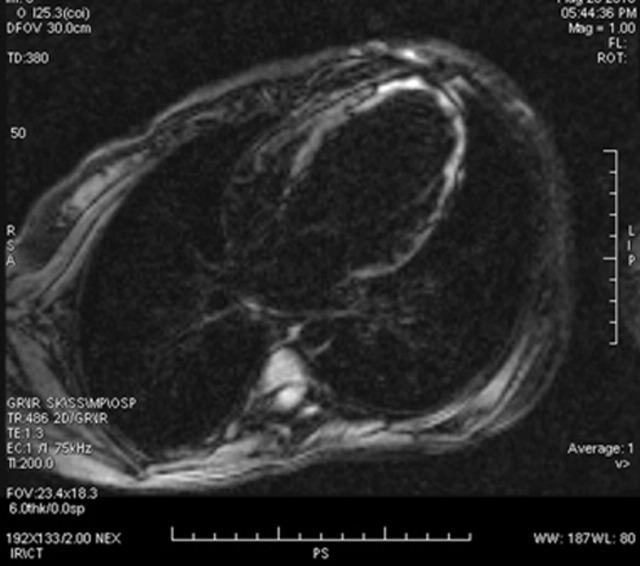
Figure 4.
MRI showing the ballooning of apex during systole.
Figure 5.
Cardiac MR demonstrating diffuse delayed gadolinium enhancement of thinned out mid and apical segments. Note the sparing of the basal segments.
Video 1.
Echocardiogram in apical four-chamber view demonstrating the contraction in basal segments with ballooning of the apex.
Video 2.
Cine MRI showing the ballooning of apex during systole.
Differential diagnosis
The differential diagnosis includes CAD and myocarditis.3 CAD is unlikely in this patient because not only the coronary arteries were normal but the pattern of myocardial involvement is not confined to the territories supplied by the epicardial coronary arteries. In myocarditis, the myocardial involvement tends to be patchy and most often affects the subepicarial region. Diffuse necrosis of mid and apical segments with sparing of basal segments is not consistent with myocarditis.
Treatment
Patient was initially treated with intravenous dobutamine and diuretics. Subsequently, she was switched to oral furosemide, spironolactone, digoxin, ramipril and carvedilol in optimal doses.
Outcome and follow-up
Although her symptoms improved, she continues to be in NYHA class III symptoms with 24% EF at 1 year follow-up.
Discussion
Takotsubo cardiomyopathy constitutes 1–2% of all suspected cases of acute myocardial infarction. Although stress is an important precipitating factor, it is not present in all patients. In view of the reversible nature of LV dysfunction and good prognosis, it is classified as reversible cardiomyopathy. CMR is a valuable tool to identify the aetiology of cardiomyopathy and helps in differentiating CAD and myocarditis. Most commonly, there is absence of delayed gadolinium enhancement in CMR. This suggests the presence of viable myocardium inspite of LV dysfunction. The LV function tends to improve on follow-up. Recently, a variant form that is characterised by delayed enhancement of contrast in CMR has been reported in takotsubo cardiomyopathy4 and it typically spares the basal segments. Immunohistological studies had documented excessive collagen-1 in this subset of patients. This variant probably denotes an extreme form of takotsubo cardiomyopathy with non-viable myocardium, irreversible LV dysfunction and poor outcome as demonstrated in this report.
Learning points.
-
▶
Takotsubo cardiomyopathy is not always reversible.
-
▶
CMR is a useful tool not only to diagnose but also to determine the prognosis.
-
▶
Variant form of takotsubo cardiomyopathy with delayed contrast enhancement is associated with irreversible LV dysfunction and poor functional outcomes.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Akashi YJ, Goldstein DS, Barbaro G, et al. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation 2008;118:2754–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008;155:408–17. [DOI] [PubMed] [Google Scholar]
- 3.Eitel I, Behrendt F, Schindler K, et al. Differential diagnosis of suspected apical ballooning syndrome using contrast-enhanced magnetic resonance imaging. Eur Heart J 2008;29:2651–9. [DOI] [PubMed] [Google Scholar]
- 4.Rolf A, Nef HM, Möllmann H, et al. Immunohistological basis of the late gadolinium enhancement phenomenon in tako-tsubo cardiomyopathy. Eur Heart J 2009;30:1635–42. [DOI] [PubMed] [Google Scholar]