Abstract
Since the “2007 summary report of child and adolescent overweight and obesity treatment” published by Barlow, many obesity intervention studies have been conducted in pediatric ambulatory care. Although several meta-analyses have been published in the interim, many studies were excluded because of the focus and criteria of these meta-analyses. Therefore, the primary goal of this article was to identify randomized case-control trials conducted in the primary care setting and to report on treatment approaches, challenges, and successes. We have developed four themes for our discussion and provide a brief summary of our findings. Finally, we identified major gaps and potential solutions, and describe several urgent key action items.
Keywords: Obesity, pediatrics, adolescents, weight management, review, randomized case-control studies
Introduction
Obesity remains a major public health threat in the United States (US), with about one in five youth (2–18 years) and one in ten children under age 2 being obese [1]. Early onset and duration of obesity have been identified as major contributors to complications related to obesity in adulthood [2]. In fact, obesity is associated with all causes mortality [3] and the top causes of mortality are lifestyle-related and preventable [4]. Therefore, strategies that affect the delivery of care from prevention to treatment and focus on early years of life may be critical.
Despite the urgency for interventions, physicians and nurses have been slow to tackle this problem and have described their lack of knowledge and skills to assess and counsel pediatric patients with obesity [5, 6]. Although certifications in pediatric nutrition are available for registered dietitians (RDs) [7, 8], few train in pediatrics and reimbursement is limited [9, 10]. In the face of these barriers, recommendations for prevention and treatment of pediatric obesity were developed for healthcare settings [11] and more recently a call of action was made for inter-professional education, training, and research [12].
The review of interventions in childhood obesity since the publication of the Expert Committee “2007 summary report of child and adolescent overweight and obesity treatment” provide an opportunity to re-evaluate these recommendations in order to identify approaches that may be effective and also to highlight current gaps. The focus of this review is on the primary care setting and we have developed four critical themes around which this review is based.
Review process
This a descriptive review of obesity treatment models for ambulatory care published since the Expert Committee “2007 summary report of child and adolescent overweight and obesity treatment” [11]. Key words in five different permutations were used to search articles on pediatric obesity interventions in the ambulatory care setting. “Randomized controlled trial obesity pediatrics” yielded 233 matches; “randomized controlled trial obesity primary care pediatrics,” yielded 46 matches; “randomized controlled trial obesity primary care adolescents,” yielded 89 matches; “randomized controlled trial obesity primary care children,” yielded 200 matches; and “randomized controlled trial weight management primary care pediatrics,” yielded 34 matches. We identified a total of 599 articles and narrowed the search to 108 relevant abstracts of obesity interventions that were implemented in the primary care setting since 2007.
Our primary goal was to identify randomized case-control trials conducted in the ambulatory care setting and report on treatment approaches, challenges, and success. Therefore, we excluded studies that had no outpatient clinic component, for example studies that solely took place in the community. Likewise, our focus was on comprehensive interventions and therefore we excluded studies that lacked an educational or behavioral component (e.g. compared two types of diet only) or focused on weight loss medication or weight loss surgery. Other exclusion criteria were not used to allow for exploration of novel methods and identification of research gaps and priorities. We also conducted a manual review of the abstracts’ references to identify additional relevant articles and “PubMed” articles to highlight findings from these reviews in our discussion.
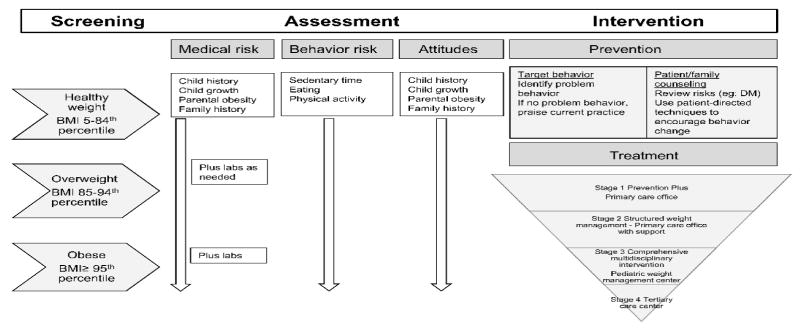
We classified the studies according to the treatment stages defined by Expert Committee where possible. (Figure 1) Study characteristics examined included child demographics, study period, treatment and control arm data including contact hours, inclusion and exclusion data, recruitment and drop out data, as well as anthropometric outcomes measures including BMI and BMI z-scores. At least two authors reviewed all RCTs. Discrepancies were resolved using a consultation and consensus approach. Of the 108 abstracts and their references, 45 randomized case-control trials were identified as meeting our criteria. (Appendix) We identified several themes for further discussion using a question format.
Figure 1. Stages of prevention and treatment approaches in pediatric obesity.
Source: Adapted from [11]
Question 1: Whom do the studies target and in what settings?
This section provides a summary of the state of the evidence based on the populations targeted in each study, including age group, weight classification, socioeconomic background, the focus of the treatment (parent, child, or both) and whether the allocated treatment was individual or group-based. Other methodologies, such as location and support of the intervention, are also discussed in this section.
Age group
The majority of interventions reviewed were conducted among school-age children (6–10 year old) and adolescent (11–21 years old) patients. Fewer were conducted in the preschool-age population (3–5 years old). Only a handful of studies were dedicated to interventions among infants and toddlers (0–2 years old) but more than in a previous USPTF meta-analysis [13]. This is especially important since the first 1000 days, from pregnancy to a child’s second birthday, have been identified as a critical period for nutritional interventions’ impact on health outcomes [14, 15].
More intensive multidisciplinary studies [16, 17] demonstrated significant reductions in weight measures compared to standard of care. Although system-based treatment interventions in early childhood that used motivational interviewing without a multidisciplinary approach did not show significant reductions in weight measures, [18] one study showed significantly less increase in weight measures. [18] As a result, Foster (2015) stated in their systematic review of treatment interventions for early childhood obesity that there is evidence supporting “Stage 3” interventions for obesity treatment in early childhood but little evidence to support other stages in this age group [19].
Weight classification
Most of the programs sought participants who met criteria for overweight and obesity based on BMI or weight-for-length using national or international references. A total of twenty one initiatives targeted both overweight and obese patients in primary care settings [16, 18, 20–38]. A total of thirteen initiatives targeted only obese patients [39–51]. One program focused on children with BMI z-score 0–3 [52] and another two targeted more severely obese individuals defined using BMI ≥97th percentile [53, 54] or z-score >=3 [55]. Finally, five studies focused on pregnant women and their offspring regardless of BMI [56–60].
Socio-economic status
Few studies that included minority participants existed when the 2010 USPTF meta-analysis was performed [13]. However, that meta-analysis included one major study that focused on a diverse population conducted among obese children and adolescents (8–16 years old) in an urban specialty clinic setting in the US [51]. Although the intervention showed benefit for anthropometric outcomes at 12-months, including BMI, BMI z-score, body fat, plasma lipids, and insulin sensitivity, the data were not examined according to ethnicity.
Since then, other studies including diverse populations have also been conducted in the ambulatory care setting [18, 20, 21, 24, 25, 29–31, 39, 43, 50, 51,]. Hofsteenge [28] conducted an RCT of 122 adolescents aged 11–18 years after a brief evaluation in a tertiary weight management program. Using post hoc analysis, these authors found that change in BMI z-score, blood pressure, and HDL were significant only in a population of western descent but not that of non-western descent. The authors postulated that the difference among ethnic groups might be due to differing cultural norms of physical appearance and healthy body weight.
More studies provide data on either income or insurance status of the families [18, 23, 24–26, 30, 32, 35, 37, 40, 46, 47, 53, 55–58, 61]. For example, Taveras et al. (2011) [18] studied 471 children age 2–6.9 years old. In post hoc analyses, they found that BMI was significantly improved among girls and children living in lower-income households (<$50,000). More studies are being conducted in diverse or underserved populations, an important advancement given their vulnerability. However, an analysis of differential effects of the interventions are rarely presented.
Parental and child involvement
Parental involvement and parent-tailored approaches were a large component of the design and implementation of the programs reviewed, as would be expected given the importance of addressing the parent-child dyad in the pediatric ambulatory care setting. Most of the studies incorporated strategies aimed at the parent-child dyad but also at each one separately. One study explicitly examined the impact of parent involvement vs. no involvement [46]. Using a sample of 357 Iranian adolescents aged 14–18 years followed for one-year, there was a significant decrease in BMI z-score, but not in BMI, for adolescents who received MI with parental involvement versus MI alone or passive assessments [46]. Although parental involvement for pre-adolescents has been standard of care based on former research studies conducted outside of outpatient clinic by Epstein [62], the Iranian study points toward the benefit of parental involvement in adolescents [46]. Such a study would need to be replicated in other populations, which likely have very different norms for family behavior and parenting.
Individual and group treatment
We observed eleven studies that included interventions delivered in individual counseling sessions without supplemental group education sessions [22, 32, 35, 38, 40, 42, 49, 54, 57, 58, 61]. Of these, six [22, 32, 35, 38, 58, 61] used phone calls, written educational materials and/or home visits to supplement the counseling sessions. Five [35, 42, 54, 58, 61] were successful in improving weight status compared to the control group; however half of the group interventions used supplemented face-to-face clinical visits and the studies varied in intensity and design. From these findings, clinical counseling sessions may be an effective alternative to group sessions, but the differences in design limit our ability to draw conclusions as to the efficacy of individual counseling sessions compared to group sessions.
Location of Intervention
The studies reviewed were predominantly conducted in the US and Australia with a few conducted throughout North America, Europe, and the Middle East. The interventions were predominantly conducted in urban settings, although some focused on rural populations.
The interventions were mostly located in outpatient pediatric primary care clinics [18, 22, 25, 26, 32, 35–39, 41, 45–49, 52, 60, 61], outpatient weight management clinics [21, 28, 50, 51], hospital-based outpatient obesity clinics [54], and community health centers [20]. One arm of an intervention took place in a high school [33] and one arm of an intervention took place in a school health center [43, 44]. Another intervention had one arm that included an inpatient component [55]. For some approaches, interventions extended beyond clinic walls and involved phone coaching [30–32, 37, 48], text messaging [48], telemedicine [24], home visits [17,47, 48, 57, 58] and communication with families via newsletters, manuals, automated phone, and educational audio tapes [22, 25, 30, 32, 35, 37, 40, 44, 61].
Studies in primary care settings that include multidisciplinary specialty protocols, home visits, and telemedicine looked especially promising (Appendix). Additional support from technology may increase contact time with families and play a role in family satisfaction [24, 63]. Given the paucity of pediatric obesity studies using supportive technologies, it is currently difficult to draw conclusions on the best method to support primary care providers.
Question 2: What are the program characteristics associated with reduction in weight status?
Since 2007, study findings have suggested that multiple treatment options may be effective in improving weight status and metabolic measures in the pediatric population. Although interventions differed in their delivery and locations, those that were of greater intensity and included supporting providers (e.g. RD) tended to be more successful.
Intensity and duration of Intervention
To the best of our knowledge, there is no randomized clinical trial specifically comparing different intensities of a behavioral intervention on anthropometric outcomes. Former reviews have summarized the anthropometric outcomes of various behavioral studies by pooling data from studies with similar level of intensities [13]. In the USPTF meta-analysis [13], authors used hours of contact as a proxy for treatment intensity. Categories of intensity were defined subjectively as very low (<10 hours), low (10–25 hours), moderate (26–75 hours), or high (>75 hours). The pooled interventions that included a medium- to high-intensity behavioral component for obese children and adolescents (≥6 y old) with BMI above the 95–97th percentile [64] were associated with modest average short term weight improvements in mean BMI change (range: 1.9–3.3 kg/m2) and were typically conducted in specialty clinics or similar settings [13]. These authors suggested that lower-intensity interventions that could be implemented in primary care had more modest and less consistent improvements in BMI.
We further classified the outpatient clinical interventions identified since 2007 based on the stages of obesity treatment defined in Barlow et al. (2007) [11]. The majority of approaches reviewed typically fit best the “stage two” treatment (“structured weight management”), which is based in ambulatory care clinics but includes support from specialists such as dietitians or outpatient physical activity programs [16, 20, 21, 24–26, 32–36, 38, 39, 40, 42, 45–47, 49, 52, 53, 56, 61]. Less intense interventions focused on dietary and physical activity education and/or behavior modification. However, as the approaches intensified, they notably involved more follow-up, multidisciplinary teamwork, and behavioral interventions, including cognitive behavioral therapy (CBT), and parenting skills training and counseling.
Several studies showed that lower intensity interventions were less effective [20, 35, 41, 49]. Mean change in BMI z-score were not significantly better in the intervention compared to the control arm of these studies (−0.20 to 0.0 s.d) [20, 41, 49]. Resnicow (2015) [35] was able to find some changes in lower intensity intervention groups: mean change BMI percentile from baseline was −1.8 for usual care, −3.8 for PCPs care, and −4.9 for PCP and RD care. However, a greater effect was found in a few studies. Looney (2014) [30] demonstrated that less than 2.5 contact hours, which included growth monitoring and behavioral change coupled with newsletters, could improve mean BMI z-score (average −0.16 s.d.) compared to standard of care in a predominately Caucasian and higher-income population (household income >$50,000/year). Pakpour (2015) [46] was also able to achieve a reduction in weight status using 4–5 hours of motivational interviewing in an Iranian population (mean BMI z-score 2.58±0.61 s.d. vs. 2.76±0.70, p=.02). These authors’ findings suggest that particular interventions may vary in effectiveness depending on the target population.
In addition to intensity of treatment, duration of treatment varied according to studies.. In Whitlock’s review [13] short-term weight outcomes were defined based on a study period lasting 6–12 months while weight maintenance was defined as a study period lasting 1–5 years after the beginning treatment. Overall, the average duration of the interventions we have identified since 2007 was 9.5 months and the average follow-up time was 15 months. The shortest intervention was a 5-month pilot study in adolescents [21] and the longest were 24-month [35, 47, 48]. Although, long term programs showed a lack of sustainability but no study included a long term maintenance program [58].
Primary care intervention with and without support
The intervention in most studies included another healthcare provider in addition to the primary care provider. Only two studies [22, 48] solely examined the efficacy of a PCP treating obesity without supportive staff. Despite support from technology, neither Taveras (2015) [48] nor McCallum (2007) [22] PCP-only interventions were found to be successful in reducing weight status. These interventions can be viewed as low-intensity, which may be an important factor in the lack of those studies efficacy. Interventions reliant solely on PCPs would not likely be sustainable given the PCPs time and cost constraints compared to allied health care professionals.
The variety of healthcare specialists used in the multidisciplinary interventions examined was broad. RDs and nutritionists played key roles in dietary counseling and education, while nurses and nurse practitioners delivered education and met with patients and families to track progress in hospital-based clinics [54]. Other supportive staff included exercise specialists and physical therapists, clinical psychologists, counselors, and social workers. To the best of our knowledge, there is no study comparing PCP and PCP with supportive staff using equal contact hours.
In summary, successful interventions used additional health care providers. Uniformly, supporting providers were used to increase the number of contact hours available to subjects. They were used to conduct group and individual visits, home visits, telemedicine visits, and follow up by phone. However, real-world implementation of web-based shared care software appeared to be challenging [65].
Question 3: Where are the research problems and gaps?
Prior to the expert committee recommendations in 2007, weight studies predominantly focused on elementary school-aged children, Caucasians, and urban areas. Nevertheless, several investigators called for studies in minorities and underserved populations [66, 67]. Recent RCTs in US primary care settings have started to enlarge their focus. Future study designs should include stratification of data by race/ethnicity and by income or insurance status.
As illustrated in the Healthy Hawks study (2013), program attrition rates are especially common in pediatric lifestyle interventions targeting minorities and populations from underserved areas [68]. Dhaliwal et al. [69] recently examined the reasons for program attrition using data from twenty three pediatric obesity programs. A few consistent predictors of attrition included pediatric patients from families who were recipients of public health insurance and children were older. Given the levels of program attrition, identifying patients and families who are more likely to adhere to their treatment goals is critical. Recently, pretreatment readiness scales and behaviors such as exercise have been used to predict program adherence [70], however more studies are needed. Better definitions and characterization of attendance and adherence rates are needed.
Another concern is the generalizability of outpatient clinic RCTs: one example is the study of Berkowitz (2013) where 43% (133/306) of patients recruited from two clinics electronic medical records and public announcement were excluded during evaluation [22]. Another example is that of Stark (2014) [47], where 84% (235/277) of the population of preschoolers in three practices met age and BMI percentile criteria but were either excluded, unable to contact, or declined. More consistent definitions for treatment program eligibility, inclusion and exclusion criteria in outpatient clinics are needed.
The field would also benefit from agreement on a uniform clinical outcome measure for weight status. Since 2007, the most frequently used outcomes were absolute values and z-scores of BMI for children aged 2–18 years old and weight-for-length in children younger than 2 years of age. Improvement in anthropometric parameters is difficult to interpret in children because they continue to growth. Greater decreases in weight are required to achieve good health in adolescents compared to toddlers. In addition, because of a paucity of empiric data above the 97th percentile, categorization of children with BMI above that percentile is not accurate [71–74]. For individuals with severe obesity, large changes in BMI is required to see a change in unit of percentile or standard deviation. Therefore, other weight measures may be required to estimate changes in weight measures (average and rates) [71–75].
As reported in other conditions [76], behavioral interventions and system-based strategies require clinical trials to evaluate their efficacy but also a real-world situation to evaluate their effectiveness. Real-world weight clinics are characterized by referral of patients who are less healthy than those who participate in trials [77] in addition to low enrollment [78] and high degree of attrition [79]. Therefore, observational studies in a real-world setting need to be better defined.
Question four: Are the interventions applicable to and sustainable in clinical practice?
Our review of the literature suggests that effective interventions depend on intervention intensity and staff availability; the more successful programs provide frequent visits and employ non-physician clinical staff such as RDs, RNs, and mental health professionals. This section explores whether these two elements can be disseminated to clinics outside of research protocols and whether these practices are sustainable.
Families’ logistical challenges
Attendance at programs requiring frequent visits may pose a challenge to some families. Attrition rates in weight management programs tend to be high (27–73%) [80]. With few exceptions, the RCTs in our review showed high attrition rates. Risk factors for attrition do include not only family insurance and older age [69], but also missing school, distance from home, scheduling conflicts, transportation and parking, clinic environment, child not ready to change, frequency of visits (too low or too high), program content (tools, individual rather than family focus, exercise interventions) [79]. Families have recommended programs that focus more on “physical activity within appointments, a family-centered approach, interactive learning environments, age-appropriate information for children and parenting support” [80]. In addition, lack of program satisfaction is a major contributor to attrition rates [63].
Family perception of treatment need
One recent study investigated why parents do not initiate enrollment in pediatric obesity programs after being referred by their primary care provider [78] and found five main themes: no perceived need for care, no perceived need for further actions, no intention to initiate the recommended care, initiation barriers, and situational factors. For those who had barriers to initiating enrollment, the main reasons included lack of time/schedule conflicts, distance/transportation problems, and misperception about the program. In that study [78], parents also listed associated costs (psychological, educational and financial), perceived lack of effectiveness (diet and lifestyle changes won’t work), perceived lack of control (“I can’t change my child’s behavior”), and preference for an alternative source of management (“doing it on their own”). Parents likely need to feel that enrollment in a program is worthwhile and is producing the expected results to remain enrolled, especially if there are costs associated with enrollment. Further studies are needed that address logistical barriers in order to improve program enrollment, adherence, satisfaction, and attrition.
Program costs
Wright et al (2014) [81] looked at the cost of a primary care-based childhood obesity intervention. Their intervention included four in-person visits and two phone calls, and estimated an average $30 of parent-incurred cost per child for participation. These costs would be expected to be prohibitive for low income families as the number of visits and travel time increase.
Using “Cost Per Quality-Adjusted Life-Year (QALY) Saved”, Cawley (2010) [82] notes that two of the most cost effective ways to prevent obesity in children are programs promoting healthy eating and physical activity in elementary schools (Coordinated Approach to Child Health [CATCH]) and middle schools (Planet Health). While treatment options that meet the needs of busy families need to be further studied, efforts toward community-based prevention may be the key to addressing the obesity epidemic on the whole.
The healthcare perspective
Increasing the frequency of visits to manage pediatric obesity could face several barriers to implementation in clinical practice. Primary care providers are ill-equipped to provide nutrition and dietary counseling given their limited education in medical school [83–85] and training during residency [86]. Therefore there is a need for intra- and inter-professional medical nutrition education and training of clinicians in primary care settings [12, 87]. Given the PCP’s demands, their limited training in pediatric obesity, and the need for high intensity treatment, support from allied health professionals is critical.
The more successful interventions reviewed in this article often used allied health care professionals to conduct visits, which increased the number of contact hours and improved weight measure outcomes. While studies did not compare which type of allied health care professional would be most effective, one could argue that RDs would be best equipped to promote healthy eating. While RDs have been proven effective for treating patients with a variety of medical nutrition conditions, they are rarely integrated into primary care teams [88]. In addition, low reimbursement of obesity interventions and high overhead costs are of concern to hospitals administrators [89, 90]. Lee et al. (2010) [91] showed that Medicaid in ten states addressed childhood nutritional and behavioral therapy reimbursement and billing codes for obesity, Medicaid in ten states did not address it, and Medicaid in the remaining 30 states had unclear guidelines. Another reason for infrequent use of allied health care professionals could be the lack of team exposure during training, however the movement toward “patient centered medical home” and more innovative payment models [88] as well as inter-professional training in medical nutrition [12;87–89] may provide the opportunity to overcome this barrier.
With the Affordable Care Act allowing for a change in the delivery care and opportunities to focus on prevention, an integration of clinical and community care to prevent and manage obesity has been proposed [92]. Such Integration of services would likely allow for more involvement of allied health care professional and community liaisons to affect the current obesity epidemic. As our health care system evolves, new opportunities to prevent and treat pediatric obesity are arising. Systems that rely on frequent visits to PCPs may not be feasible or the most effective. Increasing contact using a variety of health care professionals with support from new technologies may become a more sustainable model for the prevention and treatment of childhood obesity that isn’t burdensome on families.
Conclusions and recommendations
In summary, this review showed that weight reduction in primary care clinics improves with the level of intensity of the intervention, which often requires additional staff and technologies. During this review, we have identified multiple gaps and we are proposing several solutions. (Table 1) There is an urgent need for uniform definitions of outcomes such as weight, adherence, compliance, and attrition measures. Future studies should include strategies to improve program enrollment and attrition rates as well as use new technologies, which may also improve satisfaction. In addition, inter-professional education and training as well inter-professional approaches to the prevention and treatment of obesity is critical. Long term studies including weight maintenance strategies are needed. Finally, special attention must be given to underserved populations including non-English speaking populations and multidisciplinary interventions in early childhood obesity. This review points at multiple areas including:
Table 1.
Gap areas that are limiting study comparisons and proposed solutions
| Gap areas | Proposed solutions |
|---|---|
| Lack of standardization of outcome measures across studies |
|
| Lack of population characterization and adjustment for potential confounding factors |
|
| Lack of a clear definition of a real-world study |
|
| Lack of studies targeting groups with special needs |
|
| Limited use of new technologies to facilitate weight management |
|
| Lack of dedicated supporting staff |
|
| Lack of inter-professional education/training and research |
|
| Need to define a chronic care model |
|
Standardization of outcome measures to allow for better comparisons between studies and population groups (minorities, poverty status, etc.)
Use of innovative study approaches to improve weight and adherence measures using a combinations of settings and staff to assure intensity and continuity of care, as well as new methodologies to increase family satisfaction and decrease attrition rates
Develop an inter-professional approach to education and training in medical nutrition and lifestyle behaviors
Supplementary Material
Acknowledgments
The NFL program receives funding from the New Balance Foundation for educational and research activities.
Footnotes
Conflict of interest
The authors do not report any conflict of interest.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lakshman R, Elks CE, Ong KK. Childhood obesity. Circulation. 2012;126(14):1770–1779. doi: 10.1161/CIRCULATIONAHA.111.047738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danaei G, Ding EL, Mozaffarian D, et al. The Preventable Causes of Death in the United States: Comparative Risk Assessment of Dietary, Lifestyle, and Metabolic Risk Factors. In: Hales S, editor. PLoS Medicine. 4. Vol. 6. 2009. p. e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: Attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–4. [PubMed] [Google Scholar]
- 6.Nelson JM, Vos MB, Walsh SM, O’Brien LA, Welsh JA. Weight management-related assessment and counseling by primary care providers in an area of high childhood obesity prevalence: current practices and areas of opportunity. Child Obes. 2015;11(2):194–201. doi: 10.1089/chi.2014.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shadix K, Bell-Wilson JA. Finding Your Niche — Certification Options for the RD. Today’s Dietitian. 2007;9(3):40. http://www.todaysdietitian.com/newarchives/tdmar2007pg40.shtml. [Google Scholar]
- 8.Commission of Dietetic Registration (CDR), the credentialing agency for the Academy of Nutrition and Dietetics (AND): Board Certification as a Specialist in Pediatric Nutrition: Eligibility Application Instructions. [Last accessed, November 27, 2015]; https://admin.cdrnet.org/vault/2459/web/files/Pediatric%20Specialty%20ApplicationBooklet%206-2014.pdf.
- 9.Kyle T. ConscienHealth. Oral abstract presentation at: The Obesity Society Annual Meeting at ObesityWeekSM; November 2–6, 2015; Los Angeles, CA. 2015. www.obesityweek.com. [Google Scholar]
- 10.Lesser LI, Krist AH, Kamerow DB, Bazemore AW. Comparison between US Preventive Services Task Force recommendations and Medicare coverage. Ann Fam Med. 2011;9:44–9. doi: 10.1370/afm.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barlow SE Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 12.Kris-Etherton PM, Akabas SR, Bales CW, Bistrian B, Braun L, Edwards MS, Laur C, Lenders CM, Levy MD, Palmer CA, Pratt CA, Ray S, Rock CL, Saltzman E, Seidner DL, Van Horn L. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am J Clin Nutrit. 2014;99(5):1153S–1166S. doi: 10.3945/ajcn.113.073502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125(2):e396–418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 14.Bryce J, Coitinho D, Darnton-Hill I, Pelletier D, Pinstrup-Andersen P Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: effective action at national level. Lancet. 2008;371:510–526. doi: 10.1016/S0140-6736(07)61694-8. [DOI] [PubMed] [Google Scholar]
- 15.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, Uauy R Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet. 2013;382(9890):427–451. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 16.Bocca G, Corpeleijn E, Stolk RP, Sauer PJ. Results of a Multidisciplinary Treatment Program in 3-Year-Old to 5-Year-Old Overweight or Obese Children: A Randomized Controlled Clinical Trial. Arch Pediatr Adolesc Med. 2012;166(12):1109–1115. doi: 10.1001/archpediatrics.2012.1638. [DOI] [PubMed] [Google Scholar]
- 17.Stark LJ, Spear S, Boles R, et al. A pilot randomized controlled trial of a clinic and home-based behavioral intervention to decrease obesity in preschoolers. Obesity. 2011;19:134–141. doi: 10.1038/oby.2010.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taveras EM, Gortmaker SL, Hohman KH, Horan CM, Kleinman KP, Mitchell K, Price S, Prosser LA, Rifas-Shiman SL, Gillman MW. Randomized Controlled Trial to Improve Primary Care to Prevent and Manage Childhood Obesity: The High Five for Kids Study. Arch Pediatr Adolesc Med. 2011;165(8):714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foster BA, Farragher J, Parker P, Sosa ET. Treatment Interventions for Early Childhood Obesity: A Systematic Review. Academic Pediatrics. 2015;15(4):353–361. doi: 10.1016/j.acap.2015.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arauz Boudreau AD, Kurowski DS, Gonzalez WI, Dimond MA, Oreskovic NM. Latino families, primary care, and childhood obesity: a randomized controlled trial. Am J Prev Med. 2013;44(3 Suppl 3):S247–57. doi: 10.1016/j.amepre.2012.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ball G, Mackenzie-Rife KA, Newton MS, Alloway CA, Slack JM, Plotnikoff RC, Goran MI. One-on-one lifestyle coaching for managing adolescent obesity: Findings from a pilot, randomized controlled trial in a real-world, clinical setting. Paediatrics & Child Health. 2011;16(6):345–350. doi: 10.1093/pch/16.6.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCallum Z, Wake M, Gerner B, Baur LA, Gibbons K, Gold L, Gunn J, Harris C, Naughton G, Riess C, Sanci L, Sheehan J, Ukoumunne OC, Waters E. Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int J Obes (Lond) 2007;31(4):630–6. doi: 10.1038/sj.ijo.0803509. [DOI] [PubMed] [Google Scholar]
- 23.Boutelle KN, Norman GJ, Rock CL, Rhee KE, Crow SJ. Guided self-help for the treatment of pediatric obesity. Pediatrics. 2013;131(5):e1435–42. doi: 10.1542/peds.2012-2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis AM, Sampilo M, Gallagher KS, Dean K, Saroja MB, Yu Q, He J, Sporn N. Treating Rural Pediatric Obesity Through Telemedicine: Outcomes From a Small Randomized Controlled Trial. Journal of Pediatric Psychology. 2013;38(9):932–943. doi: 10.1093/jpepsy/jst005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Debarr LL, Stevens VJ, Perrin N, Wu P, Pearson J, Yarborough BJ, Dickerson J, Lynch F. A Primary Care–Based, Multicomponent Lifestyle Intervention for Overweight Adolescent Females. Pediatrics. 2012;129(3):e611–e620. doi: 10.1542/peds.2011-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Diaz RG, Esparaza-Romero J, Moya-Camarena SY, Robles-Sardin AE, Valencia ME. Lifestyle intervention in primary care settings improves obesity parameters among Mexican youth. J Am Diet Assoc. 2010;110(2):285–90. doi: 10.1016/j.jada.2009.10.042. [DOI] [PubMed] [Google Scholar]
- 27.Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve-month effectiveness of a parent-led, family-focused weight-management program for prepubertal children: a randomized, controlled trial. Pediatrics. 2007;119(3):517–25. doi: 10.1542/peds.2006-1746. [DOI] [PubMed] [Google Scholar]
- 28.Hofsteenge GH, Chinapaw MJM, Delemarre-van de Waal HA, Weijs PJM. Long-term effect of the Go4it group treatment for obese adolescents: a randomised controlled trial. Clin Nutr. 2014;33(3):385–91. doi: 10.1016/j.clnu.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Lloyd-Richardson EE, Jelalian E, Sato AF, Hart CN, Mehlenbeck R, Wing RR. Two-Year Follow-up of an Adolescent Behavioral Weight Control Intervention. Pediatrics. 2012;130(2):e281–e288. doi: 10.1542/peds.2011-3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Looney SM, Raynor HA. Examining the effect of three low-intensity pediatric obesity interventions: a pilot randomized controlled trial. Clin Pediatr (Phila) 2014;53(14):1367–74. doi: 10.1177/0009922814541803. [DOI] [PubMed] [Google Scholar]
- 31.Magarey AM, Perry RA, Baur LA, Steinbeck KS, Sawyer M, Hills AP, Wilson G, Lee A, Daniels LA. A parent-led family-focused treatment program for overweight children aged 5 to 9 years: the PEACH RCT. Pediatrics. 2011;127(2):214–22. doi: 10.1542/peds.2009-1432. [DOI] [PubMed] [Google Scholar]
- 32.O’Connor TM, Hilmers A, Watson K, Baranowski T, Giardino AP. Feasibility of an obesity intervention for paediatric primary care targeting parenting and children: Helping HAND. Child Care Health Dev. 2013;39(1):141–9. doi: 10.1111/j.1365-2214.2011.01344.x. [DOI] [PubMed] [Google Scholar]
- 33.Quattrin T, Roemmich JN, Paluch R, Jihnhee Yu, Epstein LH, Ecker MA. Treatment Outcomes of Overweight Children and Parents in the Medical Home. Pediatrics. 2014;134(2):290–297. doi: 10.1542/peds.2013-4084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raynor HA, Osterhold KM, Hart CN, Jelalian E, Vivier P, Wing RR. Efficacy of U.S. Pediatric Obesity Primary Care Guidelines: Two Randomized Trials. Pediatric obesity. 2012;7(1):28–38. doi: 10.1111/j.2047-6310.2011.00005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Resnicow K, McMaster F, Bocian A, Harris D, Zhou Y, Snetselaar L, Schwartz R, Myers E, Gotlieb J, Foster J, Hollinger D, Smith K, Woolford S, Mueller D, Wasserman RC. Motivational interviewing and dietary counseling for obesity in primary care: an RCT. Pediatrics. 2015;135(4):649–57. doi: 10.1542/peds.2014-1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Small L, Bonds-McClain D, Melnyk B, Vaughan L, Gannon AM. The Preliminary Effects of a Primary Care-based Randomized Treatment Trial with Overweight and Obese Young Children and Their Parents. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2014;28(3):198–207. doi: 10.1016/j.pedhc.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stovitz SD, Berge JM, Wetzsteon RJ, Sherwood NE, Hannah PJ, Himes JH. Stage 1 Treatment of Pediatric Overweight and Obesity: A Pilot and Feasibility Randomized Controlled Trial. Childhood Obesity. 2014;10(1):50–57. doi: 10.1089/chi.2013.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wake M, Baur LA, Gerner B, Gibbons K, Gold L, Gunn J, Levickis P, McCallum Z, Naughton G, Sanci L, Ukoumunne OC. Outcomes and costs of primary care surveillance and intervention for overweight or obese children: the LEAP 2 randomised controlled trial. BMJ: British Medical Journal. 2009;339:b3308. doi: 10.1136/bmj.b3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berkowitz RI, Rukstalis MR, Bishop-Gilyard CT, Moore RH, Gehrman CA, Xanthapoulous MS, Cochran W, Louden D, Wadden T. Treatment of Adolescent Obesity Comparing Self-Guided and Group Lifestyle Modification Programs: A Potential Model for Primary Care. Journal of Pediatric Psychology. 2013;38(9):978–986. doi: 10.1093/jpepsy/jst035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wright JA, Phillips BD, Watson BL, Newby PK, Norman GJ, Adams WG. Randomized trial of a family-based, automated, conversational obesity treatment program for underserved populations. Obesity (Silver Spring) 2013;21(9):E369–78. doi: 10.1002/oby.20388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boodai SA, McColl JH, Reilly JJ. National Adolescent Treatment Trial for Obesity in Kuwait (NATTO): project design and results of a randomised controlled trial of a good practice approach to treatment of adolescent obesity in Kuwait. Trials. 2014;15:234. doi: 10.1186/1745-6215-15-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Danielsen YS, Nordhus IH, Júlíusson PB, Mæhle M, Pallesen S. Effect of a family-based cognitive behavioural intervention on body mass index, self-esteem and symptoms of depression in children with obesity (aged 7–13): a randomised waiting list controlled trial. Obes Res Clin Pract. 2013;7(2):e116–e128. doi: 10.1016/j.orcp.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 43.Kalvainen MP, Korppi MO, Nuutinen OM. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int J Obes (Lond) 2007;31(10):1500–8. doi: 10.1038/sj.ijo.0803628. [DOI] [PubMed] [Google Scholar]
- 44.Kalvainen M, Utrianien P, Vanninen E, Korppi M, Nuutinen O. Impact of childhood obesity treatment on body composition and metabolic profile. World J Pediatr. 2012;8(1):31–7. doi: 10.1007/s12519-011-0324-2. [DOI] [PubMed] [Google Scholar]
- 45.Marlid S, Gronowitz E, Forsell C, Dahlgren J, Friberg P. A controlled study of lifestyle treatment in primary care for children with obesity. Pediatr Obes. 2013;8(3):207–17. doi: 10.1111/j.2047-6310.2012.00105.x. [DOI] [PubMed] [Google Scholar]
- 46.Pakpour AH, Gellert P, Dombrowski SU, Fridlund B. Motivational interviewing with parents for obesity: an RCT. Pediatrics. 2015;135(3):e644–52. doi: 10.1542/peds.2014-1987. [DOI] [PubMed] [Google Scholar]
- 47.Stark LE, Clifford LM, Towner EK, Filigno SS, Zion C, Bolling C, Rausch J. A pilot randomized controlled trial of a behavioral family-based intervention with and without home visits to decrease obesity in preschoolers. J Pediatr Psychol. 2014;39(9):1001–12. doi: 10.1093/jpepsy/jsu059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taveras EM, Marshall R, Kleinman KP, Gillman MW, Hacker K, Horan CM, Smith RL, Price S, Sharifi M, Rifas-Shiman SL, Simon SR. Comparative Effectiveness of Childhood Obesity Interventions in Pediatric Primary Care: A Cluster-Randomized Clinical Trial. JAMA Pediatr. 2015;169(6):535–542. doi: 10.1001/jamapediatrics.2015.0182. [DOI] [PubMed] [Google Scholar]
- 49.Wake M, Lycett K, Clifford SA, Sabin MA, Gunn J, Gibbons K, Hutton C, McCallum Z, Arnup SJ, Wittert G. Shared care obesity management in 3–10 year old children: 12 month outcomes of HopSCOTCH randomised trial. BMJ: British Medical Journal. 2013;346:f3092. doi: 10.1136/bmj.f3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Savoye M, Shaw M, Dziura J, Tamborlane WV, Rose P, Guandalini C, Goldberg-Gell R, Burgert TS, Cali AM, Weiss R, Caprio S. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA. 2007;297(24):2697–704. doi: 10.1001/jama.297.24.2697. [DOI] [PubMed] [Google Scholar]
- 51.Savoye M, Nowicka P, Shaw M, Yu S, Dziura J, Chavent G, O’Malley G, Serrecchia JB, Tamborlane WV, Caprio S. Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics. 2011;127(3):402–10. doi: 10.1542/peds.2010-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martinez-Andrade GO, Cespedes EM, Rifas-Shiman SL, Romero-Quechol G, Gonzalez-Unzaga MA, Benitez-Trejo MA, Flores-Huerta S, Horan C, Haines J, Taveras EM, Perez-Cuevas R, Gillman MW. Feasibility and impact of Creciendo Sanos, a clinic-based pilot intervention to prevent obesity among preschool children in Mexico City. BMC Pediatrics. 2014;14:77. doi: 10.1186/1471-2431-14-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kalarchian MA, Levine MD, Arslanian SA, Ewing LJ, Houck PR, Cheng Y, Ringham RM, Sheeta CA, Marcus MD. Family-based treatment of severe pediatric obesity: A randomized controlled trial. Pediatrics. 2009;124(4):1060–1068. doi: 10.1542/peds.2008-3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Banks J, Sharp DJ, Hunt LP, Shield JP. Evaluating the transferability of a hospital-based childhood obesity clinic to primary care: a randomised controlled trial. The British Journal of General Practice. 2012;62(594):e6–e12. doi: 10.3399/bjgp12X616319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van der Baan-Slootweg O, Benninga MA, Beelen A, van der Palen J, Tamminga-Smeulders C, Tijssen JG, van Aalderen WM. Inpatient treatment of children and adolescents with severe obesity in the Netherlands: a randomized clinical trial. JAMA Pediatr. 2014;168(9):807–14. doi: 10.1001/jamapediatrics.2014.521. [DOI] [PubMed] [Google Scholar]
- 56.Campbell KJ, Lioret S, McNaughton SA, Crawford DA, Salmon J, Ball K, McCallum Z, Gerner BE, Spence AC, Cameron AJ, Hnatiuk JA, Ukoumunne OC, Gold L, Abbott G, Hesketh KD. A parent-focused intervention to reduce infant obesity risk behaviors: a randomized trial. Pediatrics. 2013;131(4):652–60. doi: 10.1542/peds.2012-2576. [DOI] [PubMed] [Google Scholar]
- 57.Wen LM, Baur LA, Simpson JM, Rissel C, Wardle K, Flood VM. Effectiveness of home based early intervention on children’s BMI at age 2: randomised controlled trial. BMJ: British Medical Journal. 2012;344:e3732. doi: 10.1136/bmj.e3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wen LM, Baur LA, Simpson JM, Xu H, Hayes AJ, Hardy LL, Williams M, Rissel C. Sustainability of Effects of an Early Childhood Obesity Prevention Trial Over Time: A Further 3-Year Follow-up of the Healthy Beginnings Trial. JAMA Pediatr. 2015;169(6):543–551. doi: 10.1001/jamapediatrics.2015.0258. [DOI] [PubMed] [Google Scholar]
- 59.Daniels LA, Mallan KM, Nicholson JM, Thorpe K, Nambiar S, Mauch CE, Magarey A. An Early Feeding Practices Intervention for Obesity Prevention. Pediatrics. 2015 Jul;136(1):e40–9. doi: 10.1542/peds.2014-4108. [DOI] [PubMed] [Google Scholar]
- 60.Mustila T, Raitanen J, Keskinen P, Saari A, Luoto R. Lifestyle counselling targeting infant’s mother during the child’s first year and offspring weight development until 4 years of age: a follow-up study of a cluster RCT. BMJ Open. 2012;2(1):e000624. doi: 10.1136/bmjopen-2011-000624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Norman G, Huang J, Davila EP, Kolodziejczyk JK, Carlson J, Covin JR, Gootschalk M, Patrick K. Outcomes of a 1-year randomized controlled trial to evaluate a behavioral ‘stepped-down’ weight loss intervention for adolescent patients with obesity. Pediatr Obes. 2015 Feb 19; doi: 10.1111/ijpo.12013. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-Year Follow-up of Behavioral, Family-Based Treatment for Obese Children. JAMA. 1990;264(19):2519–2523. [PubMed] [Google Scholar]
- 63.Skelton JA, Irby MB, Geiger AM. A Systematic Review of Satisfaction and Pediatric Obesity Treatment: New Avenues for Addressing Attrition. Journal for healthcare quality: official publication of the National Association for Healthcare Quality. 2014;36(4):5–22. doi: 10.1111/jhq.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Centers for Disease Control and Preventions. Last accessed at http://www.cdc.gov/growthcharts/cdc_charts.htm.
- 65.Lycett K, Wittert G, Gun J, Huton C, Clifford SA, Wake M. The challenges of real-world implementation of web-based shared care software: the HopSCOTCH Shared Care Obesity trail in Children. BMC Med INfor Decis Mak. 2014;14:61. doi: 10.1186/1472-6947-14-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tershakovec AM, Kuppler K. Ethnicity, insurance type, and follow-up in a pediatric weight management program. Obes Res. 2003;11(1):17–20. doi: 10.1038/oby.2003.4. [DOI] [PubMed] [Google Scholar]
- 67.Zeller M, Kirk S, Claytor R, Khoury P, Grieme J, Santangelo M, Daniels S. Predictors of attrition from a pediatric weight management program. J Pediatr. 2004;144(4):466–70. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 68.Davis AM, Daldalian MC, Mayfield CA, Dean K, Black WR, Sampilo ML. Outcomes from an urban pediatric obesity program targeting minority youth: The Healthy Hawks program. Childhood obesity. 2013;9(6):492–500. doi: 10.1089/chi.2013.0053. [DOI] [PubMed] [Google Scholar]
- 69.Dhaliwal J, Nosworthy NM, Holt NL, Zwaigenbaum L, Avis JL, Rasquinha A, Ball GD. Attrition and the management of pediatric obesity: an integrative review. Child Obes. 2014;10(6):461–73. doi: 10.1089/chi.2014.0060. [DOI] [PubMed] [Google Scholar]
- 70.Ehrmann DE, Sallinen BJ, IglayReger HB, Gordon PM, Woolford SJ. Slow and steady: readiness, pretreatment weekly strengthening activity, and pediatric weight management program completion. Child Obes. 2013;9(3):193–9. doi: 10.1089/chi.2013.0006. [DOI] [PubMed] [Google Scholar]
- 71.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI%, BMI z-score or BMI centile? Euro J Clin Nutr. 2005;59:419–25. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- 72.Woo JG. Using body mass index Z-score among severely obese adolescents: a cautionary note. Int J Pediatr Obes. 2009;4(4):405–10. doi: 10.3109/17477160902957133. [DOI] [PubMed] [Google Scholar]
- 73.Inokuchi M, Matsuo N, Takayama JI, Hasegawa T. BMI z-score is the optimal measure of annual adiposity change in elementary school children. Ann Hum Biol. 2011;38(6):747–51. doi: 10.3109/03014460.2011.620625. [DOI] [PubMed] [Google Scholar]
- 74.Kakinami L, Henderson M, Chiolero A, Cole TJ, Paradis G. Identifying the best body mass index metric to assess adiposity change in children. Arch Dis Child. 2014;99(11):1020–4. doi: 10.1136/archdischild-2013-305163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Manning S, Pucci A, Finer N. Pharmacotherapy for obesity: novel agents and paradigms. Ther Adv Chronic Dis. 2014;5:135–148. doi: 10.1177/2040622314522848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Roche N, Reddel H, Martin R, Brusselle G, Papi A, Thomas M, Postma D, Thomas V, Rand C, Chisholm A, Price D for the Respiratory Effectiveness Group. Quality Standards for Real-World Research Focus on Observational Database Studies of Comparative Effectiveness. Ann Am Thorac Soc. 2014;11(S2):S99–S104. doi: 10.1513/AnnalsATS.201309-300RM. [DOI] [PubMed] [Google Scholar]
- 77.Braet C, Mervielde J, VanderEyken W. Psychological aspects of childhood obesity: A controlled study in a clinical and non-clinical sample. J Pediatr Psychol. 1997;22:59–71. doi: 10.1093/jpepsy/22.1.59. [DOI] [PubMed] [Google Scholar]
- 78.Perez A, Holt N, Gokiert R, et al. Why don’t families initiate treatment? A qualitative multicentre study investigating parents’ reasons for declining paediatric weight management. Paediatrics & Child Health. 2015;20(4):179–184. doi: 10.1093/pch/20.4.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obes Rev. 2011;12(501):e273–e281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kitscha CE, Brunet K, Farmer A, Mager DR. Reasons for non-return to a pediatric weight management program. Can J Diet Pract Res. 2009;70:89–94. doi: 10.3148/70.2.2009.89. [DOI] [PubMed] [Google Scholar]
- 81.Wright DR, Taveras EM, Gillman MW, et al. The cost of a primary care-based childhood obesity prevention intervention. BMC Health Services Research. 2014;14:44. doi: 10.1186/1472-6963-14-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cawley J. The economics of childhood obesity. Health Aff (Millwood) 2010;29(3):364–71. doi: 10.1377/hlthaff.2009.0721. [DOI] [PubMed] [Google Scholar]
- 83.Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med. 2010 Sep;85(9):1537–42. doi: 10.1097/ACM.0b013e3181eab71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Adams KM, Butsch WS, Kohlmeier M. The State of Nutrition Education at US Medical Schools. J Biomed Educ. 2015;2015(Article ID 357627):1–7. [Google Scholar]
- 85.Kushner RF, Van Horn L, Rock CL, Edwards MS, Bales CW, Kohlmeier M, Akabas SR. Nutrition education in medical school: a time of opportunity. Am J Clin Nutr. 2014;99(5 Suppl):1167S–73S. doi: 10.3945/ajcn.113.073510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lenders CM, Deen DD, Bistrian B, Edwards MS, Seidner DL, McMahon MM, Kohlmeier M, Krebs NF. Residency and specialties training in nutrition: a call for action. Am J Clin Nutr. 2014;99(5 Suppl):1174S–83S. doi: 10.3945/ajcn.113.073528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.DiMaria-Ghalili RA, Mirtallo JM, Tobin BW, Hark L, Van Horn L, Palmer CA. Challenges and opportunities for nutrition education and training in the health care professions: intraprofessional and interprofessional call to action. The American Journal of Clinical Nutrition. 2014;99(5):1184S–1193S. doi: 10.3945/ajcn.113.073536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jortberg BT, Fleming MO. Registered dietitian nutritionists bring value to emerging health care delivery models. J Acad Nutr Diet. 2014;114(12):2017–22. doi: 10.1016/j.jand.2014.08.025. [DOI] [PubMed] [Google Scholar]
- 89.Silberberg M, Carter-Edwards L, Murphy G, et al. Treating Pediatric Obesity in the Primary Care Setting to Prevent Chronic Disease: Perceptions and Knowledge of Providers and Staff. North Carolina Medical Journal. 2012;73(1):9–14. [PMC free article] [PubMed] [Google Scholar]
- 90.Eneli I, Norwood V, Hampl S, Ferris M, Hibbeln T, Patterson K, Pomietto M, Hassink S. Perspectives on Obesity Programs at Children’s Hospitals: Insights From Senior Program Administrators. Pediatrics. 2011;128(sup 2):S86–S90. doi: 10.1542/peds.2011-0480I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lee JS, Sheer JLO, Lopez N, Rosenbaum S. Coverage of obesity treatment: a state by state analysis of medicaid and state insurances laws. Pub Health Reports. 2010;125:596–604. doi: 10.1177/003335491012500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dietz WH, Solomon LS, Pronk N, Ziegenhorn SK, Standish M, Longjohn MM, Fukuzawa DD, Eneli IU, Loy L, Muth ND, Sanchez EJ, Bogard J, Bradley DW. An Integrated Framework For The Prevention And Treatment Of Obesity And Its Related Chronic Diseases. Health Aff (Millwood) 2015;34(9):1456–63. doi: 10.1377/hlthaff.2015.0371. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.