Abstract
Purpose
In Honduras, the breast cancer burden is high, and access to women’s health services is low. This project tested the connection of community-based breast cancer detection with clinical diagnosis and treatment in a tightly linked and quickly facilitated format.
Methods
The Norris Cotton Cancer Center at Dartmouth College partnered with the Honduran cancer hospital La Liga Contra el Cancer to expand a cervical cancer screening program, which included self-breast exam (SBE) education and clinical breast exams (CBEs), to assess patient attitudes about and uptake of breast cancer education and screening services. The cervical cancer screening event was held in Honduras in 2013; 476 women from 31 villages attended.
Results
Half of the women attending elected to receive a CBE; most had concerns about lactation. Clinicians referred 12 women with abnormal CBEs to La Liga Contra el Cancer for additional evaluation at no cost. All referred patients were compliant with the recommendation and received follow-up care. One abnormal follow-up mammogram/ultrasound result was negative on biopsy. One woman with an aggressive phyllodes tumor had a mastectomy within 60 days. Multimodal education about breast cancer screening maximized delivery of women’s health services in a low-tech rural setting.
Conclusion
The addition of opportunistic breast cancer education and screening to a cervical cancer screening event resulted in high uptake of services at low additional cost to program sponsors. Such novel strategies to maximize delivery of women’s health services in low-resource settings, where there is no access to mammography, may result in earlier detection of breast cancer. Close follow-up of positive results with referral to appropriate treatment is essential.
INTRODUCTION
Breast cancer is the most common cancer and kills more women than any other type of cancer in Latin America. Each year, approximately 115,000 women in Latin America are diagnosed with breast cancer, and approximately 37,000 women die as a result of the disease.1 Cervical cancer is the second-most common cancer among women in Latin America; 68,000 women are newly diagnosed annually, and 32,000 women die as a result of the disease each year.2 Together breast and cervical cancers account for nearly a quarter of annual cancer-related deaths in the region.3
Women in rural areas of Honduras have limited access to cancer education, screening, and care. Mammography is generally not available in the public sector, and less than 42% of the target population is covered by cervical cancer screening.3 However, inexpensive, community-based educational programs have been shown to increase cervical cancer knowledge and improve screening behavior in rural Honduras.4
We decided to apply this concept of community-based educational programs to breast cancer screening in Honduras, where a high proportion of patients present with late-stage disease. Although data are scarce, some reports suggest that presentation with late-stage disease is as high as 78%.5 In contrast, in the United States, the majority of breast cancer occurrences are detected in stages I or II, and advanced or metastatic disease is reported in 35% of cases.6
Studies that showed clinical breast exams (CBEs) and self-breast exams (SBEs) to be unhelpful in reducing stage at diagnosis7-10 have considered only developed countries or urbanized areas, where mammography is more routinely accessible. It follows then, that earlier detection, facilitated by education, CBE, and SBE, could lead to earlier surgery and result in substantial improvements in survival throughout the developing world, similar to survival improvements seen in the United States with implementation of CBE prior to the development of mammography.5 In fact, evidence-based recommendations by The Breast Global Health Initiative for culturally appropriate screening methods in low-resource areas call for reliance on the CBE in combination with active surveillance.11 To operationalize that recommendation in low-resource settings like rural Honduras, a strategy for active surveillance should consider training women to recognize problems with their breasts by using SBE and to alert health providers if they have any concerns.
In Honduras specifically, cervical cancer represents 42% of all cancer occurrences; breast cancer rates are rapidly increasing, and it is the second-most common cancer in women (data on file, La Liga Contra el Cancer Honduras, San Pedro Sula, Honduras). Approximately half of the Honduran population live in rural and remote areas, though virtually everyone lives within a 3- to 4-hour bus ride of one of the two major cities. Of the rural dwellers, 63% live in poverty, and 50% live in extreme poverty.13 An international comparison of rural and urban access to mammography indicated that a lower breast cancer survival rate in rural women may be a result of access and health care utilization.14 With no prospect for population-wide screening mammograms, and with only one cancer center, the country of Honduras is in dire need of a thoughtful, evidence-based plan to address screening and prevention with sustainable training and technology.15
The services of La Liga Contra el Cancer (LLC) are available on a sliding fee scale, and no one is turned away. In that context, this pilot project asked the following questions: Was it possible to operationalize breast screening in a rural setting? Would it be possible to interest women in breast screening during a cervical cancer screening program? In women with abnormalities in need of clinical follow-up, would it be possible to successfully connect them to the cancer hospital for additional evaluation?
By conducting a multimodal opportunistic breast cancer screening intervention during a cervical cancer screening program in rural Honduras, our objectives were to improve breast cancer awareness; to teach patients how to perform SBEs; to strengthen connections between rural women and Honduran providers to ensure continuity of care; to link patients who had abnormal findings on CBEs to appropriate services for diagnosis and treatment; and to test the efficacy of a community-based breast cancer education and screening program in rural Honduras.
METHODS
A team of health professionals and staff from the Norris Cotton Cancer Center (NCCC) at Dartmouth-Hitchcock Medical Center in New Hampshire joined Honduran oncologists from LLC and were assisted by medical students from Honduras and the United States to explore the effectiveness of rural-based cancer screening in Honduras. Local village leaders committed to hosting the program, because, as they said, “It would be an honor to be able to benefit women’s health.” They arranged for use of classroom space for screening, provided volunteers, coordinated meals, housed medical students and clinicians in their homes, and consulted throughout the planning process. Significantly, they were also the sole source of marketing for the event, which relied on word of mouth. In this setting, where there is no mail, no television, no bulletin boards, and no newspapers, word-of-mouth advertising is traditional and effective. In the preceding weeks, village leaders called in to pre-register women from their respective villages. Ultimately, women from 31 surrounding village communities participated. The Honduran national identifier, a 13-digit number, of each participant was used as the study identification number for each participant.
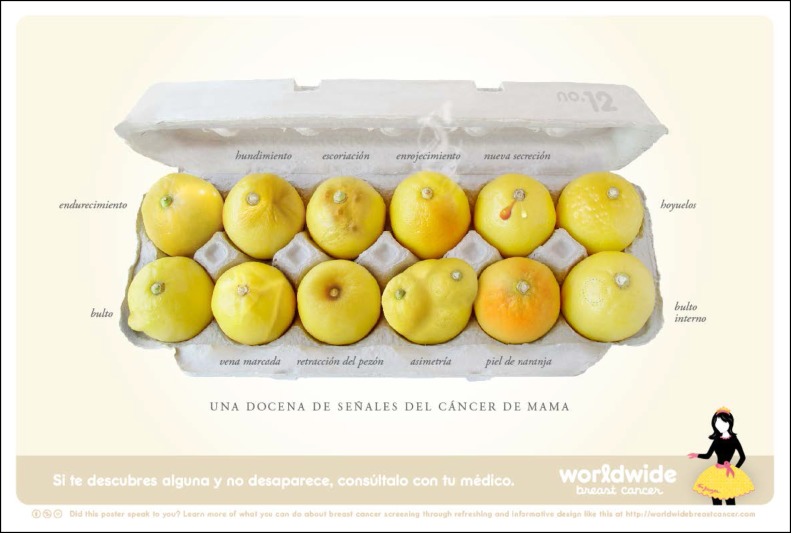
Preparations included a makeshift clinic in school classrooms fashioned by constructing cubicles with a wooden framework and hanging bedsheets for walls (Fig 1). Exam tables that could later be converted to elementary school desks were fabricated by local carpenters. Printed graphic materials for the mini-class on breast screening were copied and laminated for use (Fig 2).
Fig 1.
Local men harvested and milled wood to make the structures of the exam cubicles that were clothed with bedsheets.
Fig 2.
Lemons are stand-ins for breasts, and Spanish language captions describe potential problems (used with permission of Corrine Ellsworth Beaumont22).
Onsite, oncologists demonstrated SBE teaching methods to local female leaders, who served as peer educators for the SBE mini-class throughout the day (Fig 3). The lemons graphics (Fig 2) were used to teach visual cues of breast problems. After the SBE mini-class, women who requested a CBE were given the exam.
Fig 3.
A village leader used prepared materials to illustrate potential problems in breast health and to encourage women to inspect their breasts.
The methods of the cervical cancer screening event have been reported separately (Onega et al, manuscript in preparation) and included the following four components in the listed order: registration and consent process, and administration of a survey designed by NCCC epidemiologists and conducted by Honduran medical students; cervical cancer screening, which included traditional Pap tests, buccal cervical swabs for high-risk human papillomavirus typing at NCCC, onsite colposcopy and biopsy as needed, and referral to LLC as needed; breast cancer education and screening, which included learning the SBE from trained Honduran oncologists and/or local peer educators, provision of graphic materials to illustrate problems in the breast, use of standard breast models to practice the SBE, receipt of a CBE, and referral to LLC, when appropriate; and communal luncheon at the local community education center.
Women self-selected, and participation was limited to women older than age 18 years, because women in that age group fell within the Honduran cervical cancer screening guidelines.
One local leader advertised the screening event by telephoning or visiting a leader in each of 15 surrounding communities. A physician in family practice 90 minutes away spoke on the radio about the importance of screening and this opportunity for free screening. Village leaders returned rosters of how many women were expected to attend from their communities. There was no attempt to schedule arrivals or make appointments; however, when the total number of expected women exceeded 200, a second free bus to circulate throughout participating villages was added to accommodate participants.
The cancer screening was conducted over 2 days, on October 27-28, 2013. In addition to women from the 15 target communities, women from 16 additional surrounding rural village communities arrived at the screening site, and all were given the opportunity to participate in a study with an epidemiologic survey, cervical cancer screening, and breast cancer education. Regardless of whether they agreed to participate in the study or to contribute a cervical specimen, all women were offered access to all cancer screening services. After they provided consent, participants proceeded to cervical cancer screening and then moved to the breast education area.
RESULTS
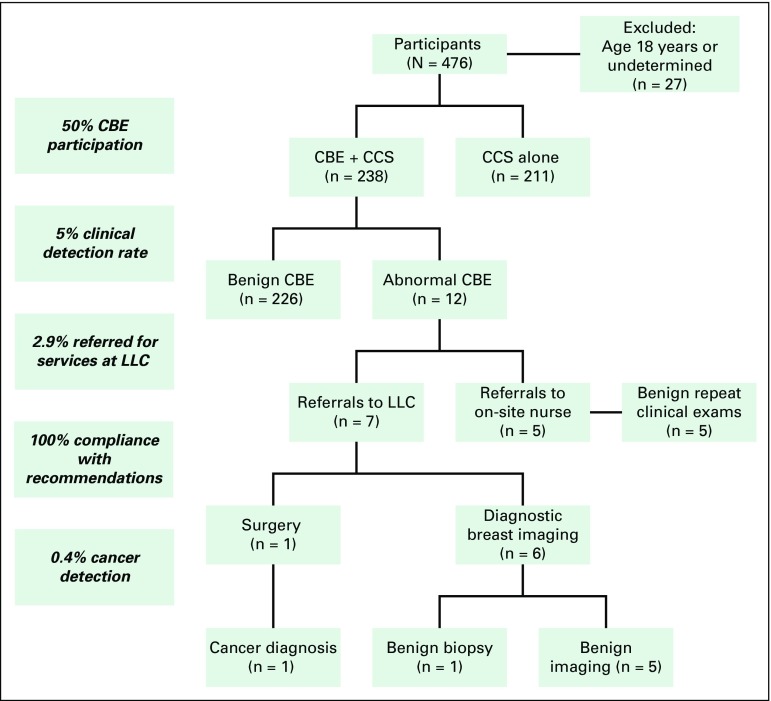
A total of 476 women availed themselves of services at the La Jornada cervical and breast cancer screening event. Honduran medical students administered NCCC-designed demographic surveys to women who attended the screening as part of a concurrent epidemiologic study (Onega et al, manuscript in preparation). Of the 476 attendees, 473 consented to complete surveys; 14 attendees were subsequently excluded because they were younger than age 18 years, and 10 more were excluded because of missing birth dates. Therefore, demographic data were collected and reported for 449 attendees. Basic demographic data for these 449 women, listed in Table 1, illustrate the characteristics of the population under study. We were not able to stratify by breast screening attendance because of the opportunistic nature of the breast cancer screening and education.
Table 1.
Demographic Data for Participants in La Jornada Cervical Cancer Screening Project
During the education sessions, participants practiced proper SBE technique using standard breast models that have embedded pellets to simulate breast tissue abnormalities. They also examined lemons graphics while they talked to each other about their own various breast problems or concerns. We were unable to determine the exact number of women who attended the breast education sessions.
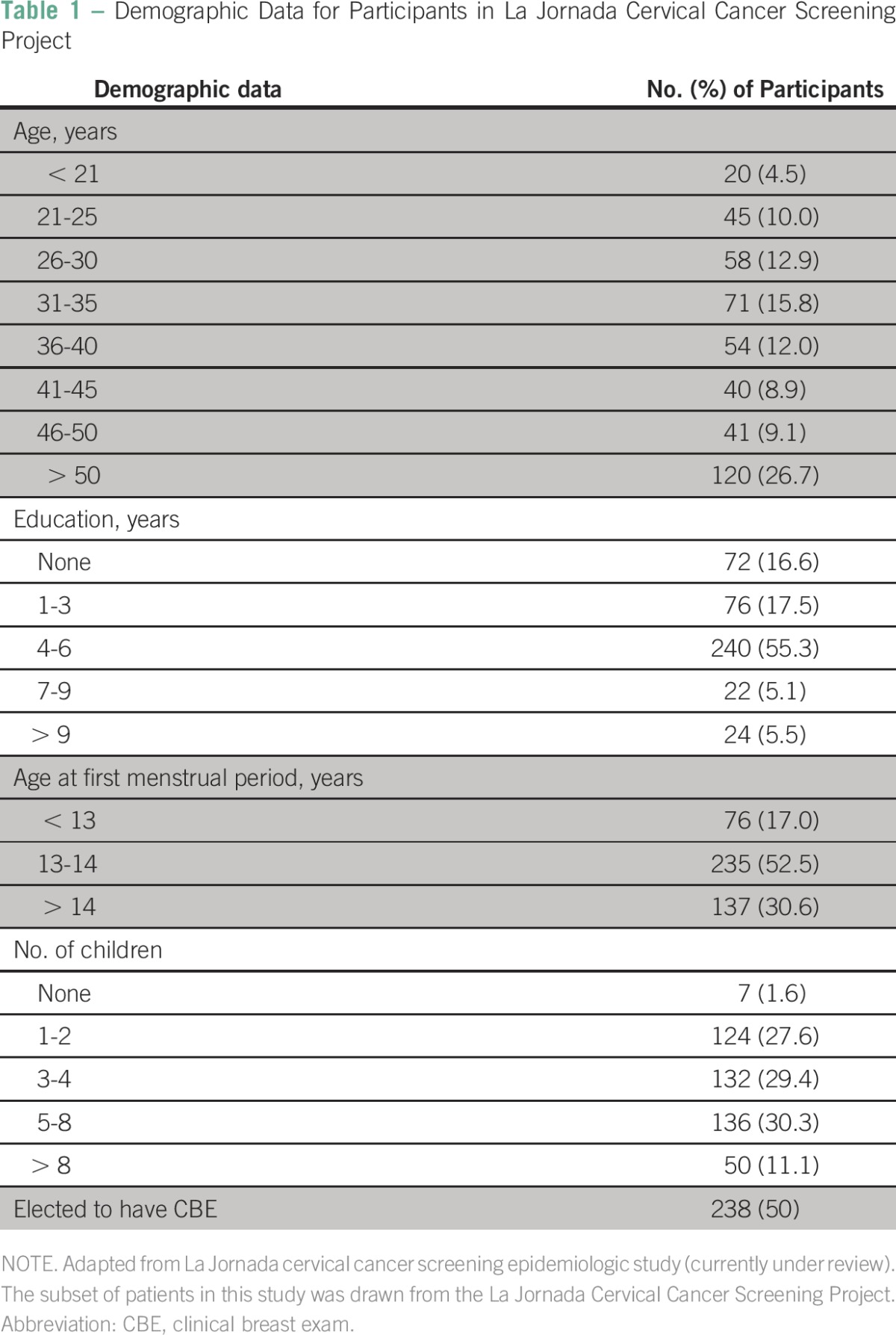
After learning about signs and symptoms of breast cancer and the SBE technique, 238 women (50% of La Jornada attendees) requested and received a CBE. Most had concerns related to lactation, and some had lactation-related changes in their breasts that they feared could be due to cancer. Twelve women (5%) had problems with their breasts deemed by the examining clinician to be unrelated to lactation. Five were referred to the onsite primary care clinic, and seven (2.9%) were referred for services at LLC. Of the seven referred to LLC, all (100%) were compliant with the recommendation: one had a mastectomy within 60 days for a malignant phyllodes tumor; the other six had mammograms, one of which was biopsied, and all six were ultimately benign.
The patient with the locally advanced phyllodes tumor went on to receive postmastectomy radiation therapy and had a disease-free interval of greater than 12 months. Unfortunately, she did experience recurrence with metastatic disease and died in March 2015. CBE participation and results are summarized in Fig 4.
Fig 4.
Clinical breast exam (CBE) participation and results. CCS, cervical cancer screening (results published elsewhere); LLC, La Liga Cancer Center.
DISCUSSION
The high participation rate in breast cancer screening (50%) during this rural cervical cancer screening event in Honduras demonstrates the potential of our opportunistic breast cancer education and screening strategy to optimize the delivery of women’s health services in a low-resource setting. This model provided the connection of detection, diagnosis, and treatment in a tightly linked and quickly facilitated format. Follow-up results indicated that it is possible to successfully link women with abnormalities in need of clinical follow-up to the country’s cancer hospital for additional evaluation. In a population of women in Honduras without access to breast cancer screening of any type, this appears to be a low-cost, high-yield method for providing services, linking women to care, and empowering them to seek help if they have suspicious findings on self-exam. The recent Lancet Oncology Commission on Latin America17 suggests that implementation of screening schemes to link rural dwellers to cancer treatment should reduce delays in diagnosis and treatment abandonment.
Country-wide data on breast cancer incidence in Honduras are limited because of the lack of standardized national screening policies and care. However, LLC has been providing cancer care for women since 1965, and we look to their records for insight. From 2009 to 2012 at LLC, 234 occurrences of breast cancer were diagnosed; 97.4% were invasive cancers. A mere 6% were noninvasive breast cancers. Only 7% of cancers were stage 0 (noninvasive) or 1; 43% were stages 2 and 3, and 44% were not classifiable because of a lack of information after diagnosis, surgical treatment, and pathology (unpublished data). This is in stark contrast to the United States, where screening mammography is routine and where, from 1995 to 2010, 26.6% of breast cancers diagnosed were noninvasive.18 The prevalence of late-stage diagnoses in Honduras reflects the lack of access to breast cancer education and screening there.
LLC and NCCC priorities were to mitigate this lack of access and work with local leaders to attract and accommodate women by reducing barriers to participation. The concept of one-stop shopping or opportunistic screening is similar to that of a project in Colombia that involved clinical exam and education19 and was used in this pilot project to build breast cancer education and screening into what was advertised locally as a cervical cancer screening event.
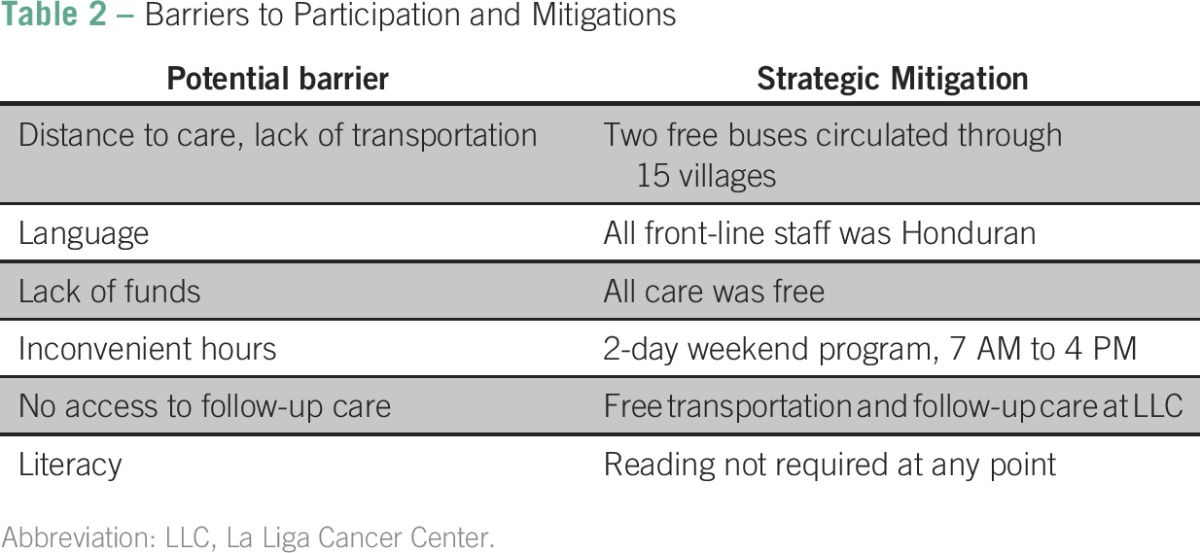
Barriers to care for people in rural Latin America are common and include language, long waits, lack of funding for medication, inconvenient clinical hours, and transportation.20 The development of strategies to mitigate these barriers was essential to implementation of this project. During planning meetings in El Rosario, local barriers were identified, and strategies to surmount them were developed. Strategies ranged from the routing of the free bus to step-by-step plans for follow-up for those referred for additional services. This local specificity was critical to the success of the program. Table 2 describes how the collaborative group of local leaders, providers, and investigators addressed each barrier as it related to the community situation.
Table 2.
Barriers to Participation and Mitigations
Two thirds of women who attended the cancer screening were younger than age 45 years, which suggests that younger women have more interest in education about cancer or a greater willingness and ability to participate in opportunities for health screening that are free and conveniently available. Although this age group has the lowest risk of breast cancer, this is an excellent group in which to begin education programs with lactation consultations and SBEs. Indeed, most participants in the breast program were lactating women who had specific questions related to breast tenderness and signs of cancer. This indicates a high level of awareness about breast cancer as well as an opportunity for educational interventions. Furthermore, the women younger than 45 years may share what they learned with older women in the word-of-mouth tradition that was highly effective at marketing the La Jornada event. Future clinics specifically for breast cancer screening could be targeted to those older than age 50 years to increase the sensitivity of the intervention.
In conclusion, as cancer deaths increase in low- and middle-income countries, there is new emphasis on the need for cancer screening, but access to and delivery of care are primary challenges. Routine screening by mammogram or ultrasound of asymptomatic women is not feasible in many areas of the world and is likely not cost effective, especially given emerging concerns for the potential for over-diagnosis.21 Palpable masses, however, are a distinct category, and earlier detection of palpable masses may result in significant improvements in outcomes.
Since this screening event, LLC has incorporated the technique of SBE education followed by optional CBE into their ongoing brigade-style outreach clinics for cervical cancer screening that they coordinate with Honduran oncologists and medical students on 40 weekends annually around their city. This demonstrates that the model is reproducible and effective at maximizing the use of existing resources.
This project found that women from rural areas were highly receptive to education and screening. Collaboration between local leaders and institutions can improve cancer care by providing access to technology for those with a demonstrated need and opens the door for more portable, novel technologies to be developed to assist with record keeping, data collection, and earlier detection. NCCC and LLC will collaborate with local leaders again in 2016 to extend this research project. The next breast screening will also be embedded in a cervical cancer screening program and is scheduled for April 23-34, 2016, in El Rosario, Yoro, Honduras, with plans to separate lactating women into another educational track and to focus on CBEs for women older than 50 years. More research and insight are needed to tailor screening policies in resource-poor communities.
ACKNOWLEDGMENT
This study was performed in the community of El Rosario in the state of Yoro, Honduras, with follow-up care at La Liga Contra el Cancer in San Pedro Sula, Honduras. Analysis and writing were completed at the Norris Cotton Cancer Center at Dartmouth.
Paul Manganiello, MD, assisted with clinical breast exams. Ana Barientos, MD, and Silvia Portillo, MD, taught the breast self-exam. Corrine Beaumont, PhD, founder of Worldwide Breast Cancer, provided lemons instructional graphics. Suzanne Burgos, PA, provided care for women who needed immediate consultation. Christine Averill, Salvdore Barrientos, Marco Tulio Martinez Jr, MD, and Roberto Zelaya, MD, provided on-site interpretation. Dean Seibert, MD, provided public health expertise.
Footnotes
Funded by the Norris Cotton Cancer Center (to T.L.O.), with its base of research at the Geisel School of Medicine at Dartmouth and of clinical care for patients at Dartmouth-Hitchcock Medical Center.
Authors' disclosures of potential conflicts of interest and contributions are found at the end of this article.
Presented in part at the following: the 2014 Global Oncology Symposium, Dana-Farber Cancer Institute, Boston, MA; the 2014 World Cancer Congress, Melbourne, Australia; and the 2015 International Cancer Screening Network Meeting, Rotterdam, the Netherlands.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Administrative support: Linda S. Kennedy
Provision of study materials or patients: Linda S. Kennedy, Suyapa A. Bejarano
Collection and assembly of data: All authors
Data analysis and interpretation: Linda S. Kennedy, Tracy L. Onega, Derek S. Stenquist, Mary D. Chamberlin
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
Linda S. Kennedy
No relationship to disclose
Suyapa A. Bejarano
Research Funding: MSD
Tracy L. Onega
No relationship to disclose
Derek S. Stenquist
No relationship to disclose
Mary D. Chamberlin
No relationship to disclose
REFERENCES
- 1. Pan American Health Organization: A review of breast cancer care and outcomes in Latin America. http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=17994&Itemid=
- 2. American Cancer Society: Global Health Groups Announce Project to Tackle Cervical Cancer Burden in Latin America and the Caribbean, May 29, 2013. http://pressroom.cancer.org/index.php?s=43&item=439.
- 3. Pan American Health Organization: Honduras Cancer Profile 2013. http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=24070&Itemid=
- 4.Perkins RB, Langrish S, Stern LJ, et al. A community-based education program about cervical cancer improves knowledge and screening behavior in Honduran women. Rev Panam Salud Publica. 2007;22:187–193. doi: 10.1590/s1020-49892007000800005. [DOI] [PubMed] [Google Scholar]
- 5.Vorobiof DA, Sitas F, Vorobiof G. Breast cancer incidence in South Africa. J Clin Oncol. 2001;19:125S–127S. (suppl) [PubMed] [Google Scholar]
- 6.Shulman LN, Willett W, Sievers A, et al. 2010. Breast cancer in developing countries: Opportunities for improved survival. J Oncol 2010:595167, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas DB, Gao DL, Ray RM, et al. Randomized trial of breast self-examination in Shanghai: Final results. J Natl Cancer Inst. 2002;94:1445–1457. doi: 10.1093/jnci/94.19.1445. [DOI] [PubMed] [Google Scholar]
- 8.Semiglazov VF, Moiseenko VM, Manikhas AG, et al. Interim results of a prospective randomized study of self-examination for early detection of breast cancer (Russia/St.Petersburg/WHO) [in Russian] Vopr Onkol. 1999;45:265–271. [PubMed] [Google Scholar]
- 9.Jamison D., Breman J., Measham A., et al., editors. Health service interventions for cancer control in developing countries, in Disease Control Priorities in Developing Countries. New York, NY: Oxford University Press; 2006, pp 569-590. [Google Scholar]
- 10.Vainio H, Bianchini F, editors. Breast Cancer Screening. Lyon, France: IARC Press; 2002. [Google Scholar]
- 11.Anderson BO, Yip CH, Smith RA, et al. Guideline implementation for breast healthcare in low-income and middle-income countries: Overview of the Breast Health Global Initiative Global Summit 2007. Cancer. 2008;113:2221–2243. doi: 10.1002/cncr.23844. (suppl) [DOI] [PubMed] [Google Scholar]
- 12. Reference deleted.
- 13. Rural Poverty Portal: Honduras. http://www.ruralpovertyportal.org/country/home/tags/honduras.
- 14.Leung J, McKenzie S, Martin J, et al. Effect of rurality on screening for breast cancer: A systematic review and meta-analysis comparing mammography. Rural Remote Health. 2014;14:2730. [PubMed] [Google Scholar]
- 15.Goss PE, Lee BL, Badovinac-Crnjevic T, et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol. 2013;14:391–436. doi: 10.1016/S1470-2045(13)70048-2. [DOI] [PubMed] [Google Scholar]
- 16. Reference deleted.
- 17.Strasser-Weippl K, Chavarri-Guerra Y, Villarreal-Garza C, et al. Progress and remaining challenges for cancer control in Latin America and the Caribbean. Lancet Oncol. 2015;16:1405–1438. doi: 10.1016/S1470-2045(15)00218-1. [DOI] [PubMed] [Google Scholar]
- 18. American Cancer Society: Cancer facts and figures 2014. http://www.cancer.org.
- 19.Murillo R, Díaz S, Sánchez O, et al. Pilot implementation of breast cancer early detection programs in Colombia. Breast Care (Basel) 2008;3:29–32. doi: 10.1159/000114446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montgomery M. Urban poverty and health in developing countries. doi: 10.1353/dem.2005.0020. http://www.prb.org/pdf09/64.2urbanization.pdf. [DOI] [PubMed]
- 21.Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367:1998–2005. doi: 10.1056/NEJMoa1206809. [DOI] [PubMed] [Google Scholar]
- 22. Worldwide Breast Cancer: http://www.worldwidebreastcancer.com.