We thank Bray and colleagues for their interest in our recent article evaluating the utility of gadolinium for the assessment of inflammatory sacroiliitis in children1. We agree that lower back pain can be secondary to many causes other than sacroiliitis, including apophyseal joint inflammation, among others. We also agree that in some cases additional investigation with lumbar imaging is warranted. Our study was focused on evaluation of the sacroiliac joints and did not include any assessment of spinal imaging. It is not our practice to routinely image the lumbar spine in the evaluation of back pain in our patients or to uniformly use contrast for such imaging for the following reasons:
First, the incremental diagnostic value of spinal imaging in addition to sacroiliac imaging in adults with non-radiographic spondyloarthritis is minimal 2. In fact, the use of both sacroiliac and spinal imaging increased the misclassification of control subjects as having spondyloarthritis 2. In addition, in our clinical experience spinal involvement in the absence of sacroiliitis is uncommon. In the Vendhan et al article there is a significantly higher prevalence of inflammatory sacroiliitis than previously reported in children with enthesitis related arthritis and similar disease duration (79% versus 34–52%) 3–5. Given this substantial difference in prevalence of sacroiliitis from prior studies the generalizability of the reported prevalence of inflammatory lesions in the lumbar spine of children is questionable.
Second, when imaging the lumbar spine in selected individuals, we do not necessarily agree that contrast is always required. Active spinal inflammatory lesions can be evaluated using T1 post-contrast imaging or fluid sensitive sequences. A study in adults by Baraliakos et al evaluated the correlation of spinal inflammation scores from fluid sensitive and post-contrast sequences 6. In this study correlation between the 2 imaging techniques was quite good (r=0.84). Inflammatory spinal lesions were detected solely with post-contrast sequences in 6% of vertebral units. Inflammatory spinal lesions were also detected solely with fluid sensitive sequences in 10% of vertebral units. The overall conclusions of this study were that both fluid sensitive and post-contrast sequences performed well and that the lack of a gold standard precludes concluding which technique is more accurate. Whether a similar situation exists for children is still unclear. Although Vendhan et al 7 conclude that contrast is necessary for evaluation of spinal inflammatory lesions in children there are several ways in which imaging techniques could have been optimized allowing for a better comparison. Use of multiplanar imaging or thinner slice imaging could not only greatly improve recognition of signal abnormalities on fluid sensitive sequences, but also differentiation of normal versus abnormal enhancement on post-contrast images. There are a number of caveats of postcontrast spinal imaging that may falsely mimic inflammatory arthritic processes (figure). Many of these are the result of normal or variant venous enhancement in the spinal and paraspinaltissues. Vendhan et al. used 4 mm thick slices. Standard slice thickness at our own institution and that used in the Baraliakos study is 3 mm. Increased slice thickness and lack of multiplanar imaging may affect sensitivity and specificity of detection of bone marrow edema and accurate assessment of enhancement.
Figure 1.
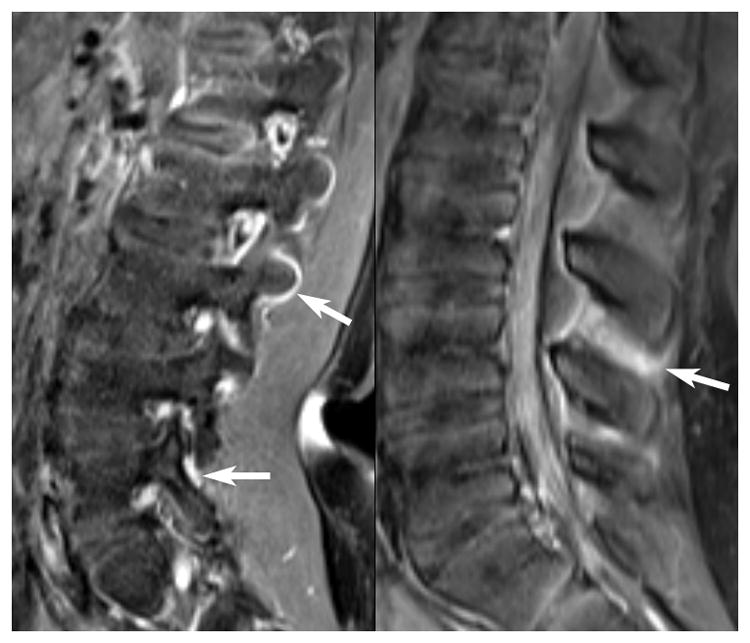
(A,B) Sagittal T1-weighted fat saturated post contrast images in two children, each with a history of a primary brain tumor and being followed for intrathecal maetstases. There is no history of back pain. Images demonstrate normal enhancement of the soft tissues and paraspinal venous structures (arrows) which can falsely mimic an inflammatory arthritis.
In summary, we maintain that contrast is not necessary when evaluating the sacroiliac joints in children. The decision to also image the lumbar spine should be based upon the clinical situation. Additional studies are greatly needed to further evaluate the prevalence of spinal inflammatory lesions in an unselected group of children with spondyloarthritis, the incremental value of contrast for spinal imaging using optimized techniques, and also to replicate our own study’s findings in a larger cohort of children.
Acknowledgments
Grant Support: Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R03-AR062665. The content is solely the responsibility of the authors and dose not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Pamela F Weiss, Division of Rheumatology, Department of Pediatrics, Center for Pediatric Clinical Effectiveness, Children’s Hospital of Philadelphia, Philadelphia, PA.
Arastoo Vossough, Department of Radiology, Children’s Hospital of Philadelphia, Philadelphia, PA.
Nancy A Chauvin, Department of Radiology, Children’s Hospital of Philadelphia, Philadelphia, PA.
References
- 1.Weiss PF, Xiao R, Biko DM, Johnson AM, Chauvin NA. Detection of Inflammatory Sacroiliitis in Children With Magnetic Resonance Imaging: Is Gadolinium Contrast Enhancement Necessary? Arthritis Rheumatol. 2015 May;67(8):2250–2256. doi: 10.1002/art.39159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weber U, Zubler V, Zhao Z, et al. Does spinal MRI add incremental diagnostic value to MRI of the sacroiliac joints alone in patients with non-radiographic axial spondyloarthritis? Ann Rheum Dis. 2015 Jun;74(6):985–992. doi: 10.1136/annrheumdis-2013-203887. [DOI] [PubMed] [Google Scholar]
- 3.Stoll ML, Bhore R, Dempsey-Robertson M, Punaro M. Spondyloarthritis in a pediatric population: risk factors for sacroiliitis. J Rheumatol. 2010 Nov;37(11):2402–2408. doi: 10.3899/jrheum.100014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bollow M, Braun J, Biedermann T, et al. Use of contrast-enhanced MR imaging to detect sacroiliitis in children. Skeletal radiology. 1998 Nov;27(11):606–616. doi: 10.1007/s002560050446. [DOI] [PubMed] [Google Scholar]
- 5.Bollow M, Biedermann T, Kannenberg J, et al. Use of dynamic magnetic resonance imaging to detect sacroiliitis in HLA-B27 positive and negative children with juvenile arthritides. The Journal of rheumatology. 1998 Mar;25(3):556–564. [PubMed] [Google Scholar]
- 6.Baraliakos X, Hermann KG, Landewe R, et al. Assessment of acute spinal inflammation in patients with ankylosing spondylitis by magnetic resonance imaging: a comparison between contrast enhanced T1 and short tau inversion recovery (STIR) sequences. Ann Rheum Dis. 2005 Aug;64(8):1141–1144. doi: 10.1136/ard.2004.031609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vendhan K, Sen D, Fisher C, Ioannou Y, Hall-Craggs MA. Inflammatory changes of the lumbar spine in children and adolescents with enthesitis-related arthritis: magnetic resonance imaging findings. Arthritis Care Res (Hoboken) 2014 Jan;66(1):40–46. doi: 10.1002/acr.22201. [DOI] [PMC free article] [PubMed] [Google Scholar]


