Abstract
Background
In the recent literature on cancer survivorship, positive changes are emphasized in the aftermath of trauma. However, there is insufficient research on older-adult survivors and more complex transformations.
Objective
Consistent with nursing researchers’ views about the duality of cancer survivor experiences, this research examined both positive and negative posttraumatic transformations (PTTs) among long-term survivors. Demographic, stress, and appraisal-related predictors of transformations were considered.
Methods
Using cross-sectional survey design, interviews were conducted with 288 survivors of breast, colorectal, and prostate cancer. The sample, obtained from a hospital tumor registry, was 58% female, 33% African American, and 67% white (mean age, 72.5 [SD, 7.6] years). Demographic characteristics, cumulative stress exposure, appraisals of stress, and self-reported PTTs were measured.
Results
Most respondents reported diverse transformations attributed to their illness experience. Demographic characteristics and stress appraisals were more strongly associated with PTT outcomes than was cumulative stress exposure. Appraisals of the cancer experience as stressful, as generating worry, and as stigmatizing were significantly associated with diverse PTT outcomes.
Conclusion
Many long-term older cancer survivors report PTT reflecting altered perspectives on life. Posttraumatic transformations are related to the view that cancer is a continuing worrisome and stigmatizing experience.
Implications for Practice
Nurses have a unique opportunity to discuss with patients the potentially life-changing nature of the cancer experience in a manner that allows for understanding and acceptance of complex changes, incorporating benefit finding along with acknowledgement of loss and suffering. This type of discussion can enhance cancer survivors’ mental health.
Keywords: Cancer survivorship, Coping, Posttraumatic transformation, Psychological adaptation, Stress appraisal
Background
This study investigates how older adults, who are long-term cancer survivors, evaluate the impact of their cancer experience on their identity. We describe survivors’ reports of transformations in life perspectives and values. We also examine antecedents of such transformations, including demographic, cumulative stress–related, and appraisal-related factors. We test a conceptual model that links changes in life perspectives after cancer to demographic characteristics of survivors and objective indicators of stress severity on the one hand and to appraisals of stress, worry, and stigma on the other (Figure). Our study represents an important contribution to understanding aspects of cancer survivorship among older adults, among whom cancer is prevalent. This group may be particularly vulnerable to late effects of cancer based on functional limitations and cumulative stresses they confront and based on lack of attention by health care providers after transition to long-term survivor status.1
Figure.
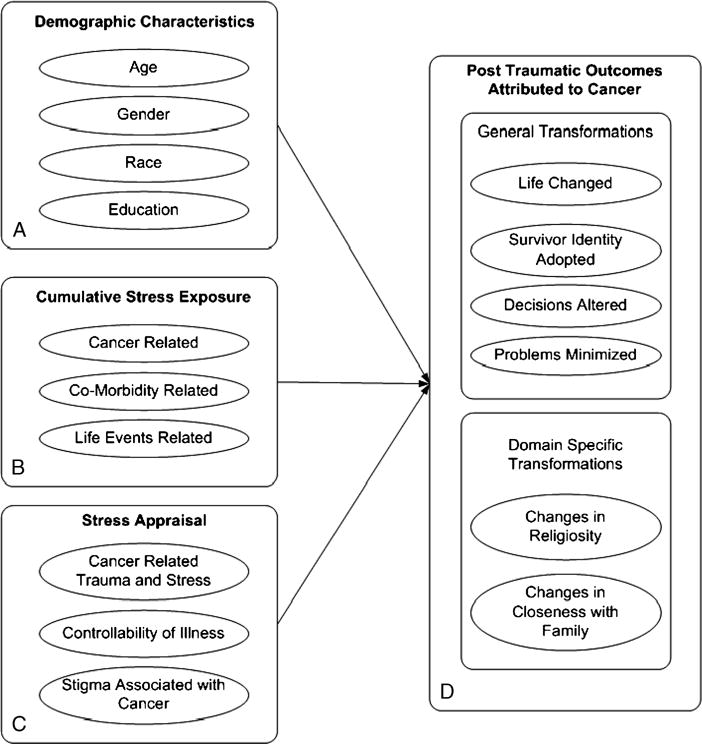
Conceptual model of Components and Antecedents of PTT.
Nurse researchers have noted that long-term cancer survivors may have resolved many of the somatic concerns associated with cancer, but can benefit from help in dealing with the social, psychological, and particularly the existential challenges of their illness experience.2 It is now recognized that research is needed focusing on patient perspectives to help develop clinical practice guidelines, which are currently lacking for the posttreatment period of long-term survivorship.3,4 Our article aims to contribute to the development of such guidelines.
Nursing professionals have been at the forefront of understanding both conceptual and clinical dimensions of cancer survivorship in late life.5,6 Specifically, nurse theorists have recognized that cancer “is a life-changing experience with a duality of positive and negative aspects.”7(p499) In this article, we take a position consistent with this view as we explore the experience of diverse transformations of older-adult cancer survivors and consider antecedents of specific transformations. We refer to self-reported changes in life perspectives, beliefs, and identities attributed to the cancer experience as posttraumatic transformations (PTTs).
The literature on trauma survivorship initially focused on posttraumatic stress disorder (PTSD), reflecting adverse psychiatric sequelae of experiencing life-threatening illness.8 As the field of traumatology matured, there was a reaction against problem-focused clinical orientations,9 and the focus shifted to the potential among survivors for benefit finding and for posttraumatic growth (PTG).10 A similar pattern has characterized the literature on cancer-related trauma and its sequelae. In contrast with earlier focus on adverse effects of cancer on psychological well-being, recent literature emphasizes the potential for positive psychological changes that can accrue as part of the cancer survivorship experience.11
Researchers interested in psychological sequelae of cancer recognize that trauma brings about significant changes in the self that may involve alterations in life outlook, resulting from efforts to integrate suffering into a renewed self-understanding.12,13 Illness-related stressors challenge one’s prior beliefs about the self and may produce coping efforts that include reframing or reinterpreting the event. Such cognitive maneuvers can lead to transformed priorities, beliefs, and identities.14 Janoff-Bulman15 explained these phenomena as changes that result from shattering, and subsequently rebuilding, one’s “assumptive world.”15(p71)
Although many emphasize PTG as reflecting positive changes in the aftermath of trauma,15 research does not support a unidimensional perspective.9 It has been argued in the nursing literature7 that meaningful theorizing about cancer survivorship must recognize the dual (negative as well as positive) aspects of the survivorship experience. Following this approach, we consider transformations in the aftermath of cancer as embodying both positive and negative elements. We propose that the life-threatening illness experience will bring about a variety of mixed, positively and negatively valenced transformations among cancer survivors.
Qualitative studies, based on exploration of cancer survivors’ experiences, have called attention to complex changes in life outlook.16,17 Transformations are viewed as results of suffering and of a search for integrating this suffering into an altered identity.13 These qualitative studies have been rich in a nuanced understanding of the lived experience of survivors, but call for follow-up quantitative research that can help examine the generalizability of findings in diverse groups of cancer survivors. The present study affords such an opportunity. It examines both the prevalence and predictors of diverse self-reported transformations in life perspectives among older-adult cancer survivors.
Survivors of cancer are likely to undergo diverse transformations. They generally recognize that this major illness has been life changing.18,19 Their survivor identity may become particularly salient, as they recognize survivorship to be a defining aspect of selfhood.20 The cancer experience can also lead to changes in decision making, such as balancing work with family priorities.21 Such changes in philosophy of life may also result in existential transformations, altering religious beliefs and practices.22
It is useful to reflect on the interpretation of such transformations as distinct from both PTSD and PTG. Posttraumatic stress disorder refers to a psychological disorder, whereas PTG focuses primarily on positive reappraisals after trauma.20 We distinguish our construct of PTT from PTG as well as PTSD, because we do not assume that all transformations fit into a fully positive or fully negative mold.7,22 We envision transformation as encompassing a spectrum of changes in one’s life perspective and identity. Understanding the long-term impact of cancer survivorship has great importance for practitioners. We propose and investigate a comprehensive and textured concept of transformations that can benefit nurses and other clinical staff who work with cancer survivors.
Rationale
To learn more about factors that influence transformation in life perspectives among cancer survivors, it is important to consider how demographic background, stress exposure, and cognitive appraisals of stressors contribute to such changes. As we understand key factors associated with transformation among cancer survivors, we can begin to identify potential risk factors that need to be further explored in prospective studies of adaptive outcomes. Subsequently, we can develop effective primary and secondary prevention efforts.
The conceptual model for the study is presented in the Figure. Based on prior work on cumulative stress exposure23 and the literature on stress appraisals,24 we hypothesized that diverse aspects of PTT would each be influenced by demographic characteristics, cumulative stress exposure, and cognitive appraisal of the illness experience among cancer survivors.
Demographic characteristics can filter how individuals experience and view trauma and can influence subsequent changes in life perspectives. Age, sex, race, and educational level have been found to be associated with responses to stress.25 Among cancer survivors, Lechner and colleagues26 found associations between sociodemographic variables and benefit finding after cancer. Specifically, older women were reported to experience less emotional distress and fewer family problems after breast cancer than did younger women.27 Racial disparities in psychosocial cancer outcomes have also been documented.28 Furthermore, demographic characteristics that reflect resources, such as higher education and being married, have been found to relate to greater growth after trauma.29
The cumulative nature of stress exposure may also shape the impact of the illness experience on psychological well-being.20 For long-term cancer survivors, such stress exposure includes severity of the original cancer, enduring cancer-related symptoms, current functional limitations (that reflect comorbidities), and recent non–illness-related stressful life events.30 In prior research in this sample of cancer survivors, cancer severity was determined to be associated with diminished psychological well-being.29
Negative appraisals resulting in lower self-esteem can be associated with a negative outlook among cancer survivors.31 A major aspect of trauma that calls for transformation of the self is worry about the recurrence of cancer, symbolizing the uncontrollability of survivors’ future.31 It has also been recognized that cancer continues to be a stigmatizing illness, based on long-held cultural beliefs about its link to suffering and its threat to life.32 Perceptions of stigma pose threats to identity that, in turn, can lead to transformed life perspectives.33
Thus, prior research supports expectations that transformations would be associated with survivors’ demographic background, their level of stress exposure, and their cognitive appraisals of cancer-related stressors. Our study sought to describe the range and extent of self-reported transformation among long-term elderly cancer survivors. Furthermore, we examined the roles of demographic characteristics, cumulative stress exposure, and appraisals of cancer-related stress in contributing to PTT (Figure).
Methods
Participants
Using a cross-sectional survey design, interviews were conducted with 288 survivors of breast, colorectal, and prostate cancer. The current study is part of a larger investigation of older-adult long-term cancer survivors.29 The sample (Table 1) was obtained from the tumor registry of a large Midwestern university-based hospital center. We selected older long-term survivors from the cancer registry (aged ≥60 years and 5+ years after diagnosis). The sample had a mean age of 72.5 (SD, 7.6) years and was, on average, 10.4 (SD, 5.5) years past diagnosis. Age 60 years was chosen as it is the decade of life in which the incidence of cancer doubles.35 Based on traditions of the gerontological cancer literature, we refer to this age group as older adults (as distinguished from children or young or middle-aged adults).1,36
Table 1.
Mean, SD, and Coding for Variables in the Conceptual Model
| Variable | Coding | % | Mean | SDa |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, y | Range, 60–95 | 72.5 | 7.6 | |
| Sex | — | |||
| Male | 42.0 | |||
| Female | 58.0 | |||
| Race | — | |||
| White | 33.0 | |||
| African American | 67.0 | |||
| Years of education | Range 3–30 | 14.1 | 3.5 | |
| Cumulative stress exposure | ||||
| Type of cancer | ||||
| Breast | 40.3 | — | ||
| Prostate | 29.5 | — | ||
| Colorectal | 30.2 | — | ||
| Years of survivorship | Range, 3–24 | 10.4 | 5.5 | |
| Stage of cancer | 1 = In situ, 2 = local, 3 = regional, 4 = distal | 2.3 | 0.6 | |
| No. of treatment types | Possible range, 0–5; actual range, 0–4 | 1.6 | 0.8 | |
| No. of current illness symptoms | Possible range, 0–22; actual range, 0–14 | 3.4 | 3.0 | |
| Functional limitations (Nagi34) | Possible range, 0–33; actual range, 0–25 | 5.1 | 5.3 | |
| Recent life events | Possible range, 0–11; actual range, 0–8 | 2.1 | 1.4 | |
| Stress appraisal | ||||
| Cancer was a traumatic experience | 0 = Not at all; 3 = very much | 1.7 | 1.0 | |
| Cancer was a stressful event | 0 = Not at all; 3 = very much | 1.5 | 1.1 | |
| Worry about recurrence | Possible range, 4–20; actual range, 4–20; α reliability = .839 | 11.2 | 3.4 | |
| Concern regarding stigma (others’ perception) | 1 = Strongly disagree; 5 = strongly agree | 2.1 | 0.8 | |
| Self-perception of stigma | 1 = Strongly disagree; 5 = strongly agree | 2.2 | 0.7 | |
| Posttraumatic outcomes | ||||
| General transformation | ||||
| Life change | 1 = Strongly disagree; 5 = strongly agree | 2.4 | 0.9 | |
| Survivor identity adopted | 1 = Strongly disagree; 5 = strongly agree | 3.5 | 1.0 | |
| Decisions altered | 1 = Strongly disagree; 5 = strongly agree | 2.8 | 1.0 | |
| Problems minimized | 1 = Strongly disagree; 5 = strongly agree | 3.3 | 1.0 | |
| Domain-specific transformation | ||||
| Changes in religiosity | 1 = Less religious; 4 = much more religious | 2.4 | 0.6 | |
| Changes in closeness to family | 0 = Not at all; 3 = very much | 1.4 | 1.0 |
SDs not reported for categorical variables.
We sampled survivors of breast (40%), colorectal (30%), and prostate cancer (30%), the 3 most common survivable cancers among older adults.37 We oversampled African Americans, who constitute 33% of the sample. This was done to provide sufficient statistical power to evaluate the influence of being African American on outcomes in this study.
Participants were randomly selected from more than 6000 individuals in the tumor registry. From among these, 2129 survivors were identified who met the age, race, and cancer-type criteria for the study (≥60 years or older; treated for breast, colorectal, or prostate cancer; ≥5 years after diagnosis; and African American or white). The study randomly selected 635 of these individuals to fill the study cells related to race and cancer type, as discussed above. We were able to contact 517 individuals, of whom 321 agreed to participate and signed the institutional review board–approved consent form (62% agreement rate). For this analysis, 33 cases were excluded because of missing data on key study outcomes. The final sample included 121 men and 167 women.
After obtaining informed consent and institutional review board approval, interviewers who were experienced in working with older adults conducted individual face-to-face interviews, which lasted approximately 1½ hours per respondent. Data were available on all study questions for 288 individuals from among a total of 321 study participants. Respondents and nonrespondents were similar on all variables, with the exception of significantly higher response rates among white patients.
Measures
The measures that operationalize key constructs in our model are described in the following sections, with further descriptive information provided in Table 1.
CUMULATIVE STRESS EXPOSURE
Cancer Severity
This construct includes cancer stage at diagnosis and range of treatment types. Cancer stage and treatment types are widely used indicators that serve as surrogate measures of severity of illness and complexity of treatment.38 Stage at diagnosis was derived from information in the tumor registry. Range of treatment types was based on respondents’ self-reports of having received any or all of the following treatments: surgery, radiation, chemotherapy, hormone therapy, and/or another treatment type (possible range, 0–5). Thus, a patient who received surgery and radiation treatments was recorded as having received 2 different types of treatment. A patient who received surgery, chemotherapy, and radiation was recorded to have received 3 different types of treatment.
Current Illness Symptoms (Cancer Related)
A list of 22 possible illness symptoms was constructed, based on focus groups conducted with older-adult, long-term cancer survivors. Respondents were asked which of these symptoms they are currently experiencing. This index is similar to measures used in prior cancer research39 and has been used in prior publications by the authors.40 Examples of symptoms include nausea, weakness, pain, and swelling. Each of the 22 items was coded with 1 = “have symptom now” or 0 = “do not have the symptom now.”
Functional Limitations
This index, developed by Nagi,34 assesses the problems respondents had with 11 specific motor tasks, such as standing, lifting or carrying objects, moving limbs, stooping/bending, or kneeling. Each response was scored on a 4-point continuum from 0 = “no difficulty” to 3 = “unable to perform” (possible range, 0–33). This is a widely used scale with an α reliability of .89 in our research. Based on prior research with older adults, functional limitations often reflect multiple comorbidities.30
Recent Life Events
The Life Events Index, developed by Kahana et al,41 inquires about 11 events commonly experienced by older adults, during the past year. Events range from death of a close family member, to divorce of a child or grandchild, to financial difficulties. The total number of events that survivors experienced during the past year is the summary score.41
STRESS APPRAISAL
Appraisals of Cancer-Related Trauma and Stress
Two single-item indicators of perceived stressfulness of the cancer experience were included. These items were conceptualized as meaningful but relatively independent self-perceptions, because they did not have a high-enough correlation to constitute a scale. These 2 separate questions assess (1) the extent to which cancer was perceived as a traumatic experience and (2) whether cancer was perceived as a stressful experience. Answer categories for each item range from 0 = “not at all” to 3 = “very much.”
Worry About Recurrence of Cancer
This was measured based on the work of Gotay and colleagues.42 Four items were used to assess this domain, as exemplified by “I worry about my cancer coming back” and “I worry about future diagnostic tests.” Responses were scored on a 5-point continuum from 1 = “strongly disagree” to 5 = “strongly agree.” The scores on individual items were totaled to create a total index score. The mean score of this indicator was 11.2 (SD, 3.4), with a potential range of 4 to 20. The α reliability was .84. Results of factor analysis indicated that the cancer-related worry items do not cross-load significantly with anxiety or depression.43
Appraisal of Cancer-Related Stigma
Feeling stigmatized by cancer was assessed using 2 single-item indicators: (1) “I am concerned about how others view me since I have had cancer,” and (2) “Others view me as being changed by my experience with cancer.” Both items are scored on a Likert scale ranging from 1 = strongly disagree to 5 = strongly agree. These 2 items did not have sufficiently high correlations (r = 0.22) to constitute a unidimensional scale, so they are used in this research as single-item indicators.
POSTTRAUMATIC TRANSFORMATION OUTCOMES ATTRIBUTED TO CANCER
Six single-item indicators were included to assess diverse changes in life outlook attributed to the cancer experience. Respondents were asked, using a 5-item Likert scale, to what extent they agreed with each statement. Items are life change (PTT 1), that is, “life has changed a great deal since having cancer”; survivor identity adopted (PTT 2), that is, “being a cancer survivor is an important part of who I am”; decisions altered (PTT 3), that is, “cancer affected various decisions I made in life”; problems minimized (PTT 4), that is, “other problems appeared less important after I had cancer”; domain-specific transformations related to religiosity (PTT 5), and closeness to family (PTT 6). Using Likert scales, respondents were asked to report (1) whether they consider themselves more or less religious and (2) whether they feel closer or less close to their family since having had cancer. The 6 dimensions of transformation correspond to experiences of transformation that have been identified by cancer survivors in qualitative research, based on content analysis of shared narratives.27 However, based on our factor analysis, these items appear to reflect conceptually distinct dimensions, as they did not load on a single factor, nor did they yield a sufficiently high α reliability coefficient when combined. As a result, these are incorporated into the analysis as single-item indicators.
Analysis
Descriptive data on demographic characteristics, cumulative stress exposure, stress appraisal, and PTT outcomes are presented (Table 1) as a prelude to linear regression analyses (Table 2). Correlations among PTT items were obtained, and external correlates of each construct were explored (they are reported in the text and are not shown in the tables, but are available on request). Next, regression equations were estimated to examine the relative impact of demographic characteristics, cumulative stress exposure, and stress appraisal on indices of PTT, controlling for other predictors (Table 2). Standardized regression coefficient (β) and the unstandardized regression coefficient (B) are provided to identify the net effects of each predictor on the respective outcome. The regression analysis also provides basic goodness-of-fit information (R2, F, and P values) for the respective equations.
Table 2.
Linear Regression: Factors Associated With Posttraumatic Transcendence (N = 288)a
| Intercept | General Transformations
|
Domain-Specific Transformations
|
||||
|---|---|---|---|---|---|---|
| (1) Life Change | (2) Survivor Identity Adopted | (3) Decisions Altered | (4) Problems Minimized | (5) Changes in Religiosity | (6) Changes in Closeness to Family | |
|
|
|
|||||
| 3.12b β (B) |
2.03c β (B) |
1.59c β (B) |
4.02b β (B) |
2.26b β (B) |
0.43 β (B) |
|
| Demographic characteristics | ||||||
| Age | −.14 (−0.02)c | .01 (0.00) | −.13 (−0.02)c | −.12 (−0.02)c | −.12 (−0.01)c | −.07 (−0.01) |
| Sex (F)d | −.05 (−0.10) | .06 (0.11) | .16 (0.32)e | .05 (0.09) | .02 (0.02) | .08 (0.16) |
| Race (AA)d | .01 (0.02) | .07 (0.14) | −.03 (−0.06) | −.02 (−0.04) | .19 (0.25)e | .18 (0.36)e |
| Years of education | −.01 (0.00) | −.13 (−0.04)c | .13 (0.04)c | −.11 (−0.03) | −.04 (−0.01) | −.12 (−0.03)c |
| Cumulative stress exposure | ||||||
| Cancer stage | −.07 (−0.11) | .03 (0.06) | −.04 (−0.07) | −.07 (−0.11) | .06 (0.06) | .11 (0.18)c |
| No. of treatment types | .15 (0.18)c | .00 (0.00) | −.04 (−0.06) | .04 (0.05) | −.02 (−0.01) | −.09 (−0.11) |
| Functional limitations | .13 (0.02) | −.03 (−0.01) | −.05 (−0.01) | .05 (0.01) | .00 (−0.01) | .00 (0.00) |
| Total no. of current illness symptoms | .06 (0.02) | .08 (0.03) | .08 (0.03) | −.06 (−0.02) | .04 (0.01) | .15 (0.05)c |
| Recent life events | .09 (0.05) | .07 (0.05) | −.07 (−0.06) | −.01 (−0.01) | .06 (0.03) | .07 (0.05) |
| Stress appraisal | ||||||
| Cancer was traumatic | −.04 (−0.04) | .00 (0.00) | .00 (0.00) | .00 (0.00) | .05 (0.03) | .06 (0.05) |
| Cancer was stressful | .06 (0.05) | .08 (0.07) | .19 (0.17)e | .10 (0.09) | .08 (0.04) | .12 (0.10) |
| Worry about recurrence | −.03 (−0.01) | .06 (0.02) | .21 (0.06)b | .13 (0.04)c | .01 (0.00) | .06 (0.02) |
| Concern over stigma | .11 (0.12) | .14 (0.17)c | .14 (0.17)c | .17 (0.21)e | .09 (0.07) | .11 (0.13)c |
| Feel stigmatized | .16 (0.19)e | .19 (0.25)e | .15 (0.19)e | −.01 (−0.02) | .09 (0.08) | .03 (0.04) |
| R | 0.39 | 0.40 | 0.52 | 0.35 | 0.36 | 0.45 |
| R2 | 0.15 | 0.16 | 0.27 | 0.12 | 0.13 | 0.20 |
| Adj R2 | 0.11 | 0.12 | 0.23 | 0.08 | 0.09 | 0.16 |
| F | 3.86 | 4.23 | 7.94 | 3.09 | 3.35 | 5.42 |
| P | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
Significant values appear in bold; P values 2-tailed.
P ≤ .001.
P ≤ .05.
Binary variables were coded 0, 1. For sex, female = 1; for race, African American = 1.
P ≤ .01.
Results
We first present descriptive findings regarding key constructs of the model. The information provided supplements data provided in Table 1 and offers useful insights into the appraisal of the illness experience and of survivorship in later life.
Cumulative Stress Exposure
Most survivors had localized forms of cancer (61.3%), whereas almost a third had regional cancer involvement (29.7%). It is notable that about half of the sample received only surgery (47.2%), followed by a combination of surgery and radiation (13%), or surgery and chemotherapy (10.4%). Common cancer-related symptoms reported included pain (37%) and general weakness (32%). The most common functional limitations were problems standing for long periods (58%) and problems in stooping/bending or kneeling (32%). The most frequent life event experienced was the death of a close friend or neighbor (42%) followed by the death of a close family member, experienced by 42% of respondents.
Stress Appraisals (Trauma, Stress, Worry, and Stigma)
About half of the respondents considered their cancer to be a traumatic experience, and a similar proportion considered their cancer to be a “stressful event.” Regarding worry of recurrence, 43% of the respondents scored in the upper half of the Worry Scale, with more than one-third expressing concern about possible recurrence of their cancer. Few respondents reported experiencing feelings of stigma as a result of cancer. Thus, only about 9% either agreed or strongly agreed with the statement, “I am concerned about how others view me since I have had cancer,” and only 8% either agreed or strongly agreed that “Others view me as being changed by my experience with cancer.”
Posttraumatic Transformation
Many respondents considered being a cancer survivor as an important part of their identity. Specifically, about two-thirds of respondents “agree” or “strongly agree” that being a cancer survivor is an important part of who they are. Furthermore, more than three-fourths of respondents agree or strongly agree that since their cancer diagnosis, their lives have changed a great deal. Having cancer has changed respondents’ perspectives on how they make decisions (decisions altered). About one-third of respondents (32.3%) agree or strongly agree that cancer has affected the decisions they make. With regard to domain-specific transformations of changes in religiosity and in closeness with family, almost one-third of respondents reported having become more religious, and more than one-third reported enhanced family closeness subsequent to cancer.
Multivariate Analysis
We conducted linear regression analyses of demographic characteristics, cumulative stress exposure, and stress appraisal on the PTT outcomes (Table 2). As part of our analyses, we examined colinearity for the 2 variables; “cancer was traumatic” and “cancer was stressful.” These had a tolerance level greater than 0.5, indicating that colinearity is not a problem. Furthermore, including each variable separately in the regression analysis did not alter results. The same is true when testing for colinearity among the 2 stigma items.
As we consider the 3 major sets of predictors in our model (demographic characteristics, cumulative stress exposure, and stress appraisals) across PTT outcomes, demographic characteristics and stress appraisals, as a group, have a stronger impact than do the cumulative stress exposure variables. One fairly consistent trend across most outcomes is that, even in this group of older adults, the younger respondents report more transformation as a result of their cancer. We also find significant effects of “concern over stigma” and “feeling stigmatized” across the transformation outcomes.
The individual models for all 6 outcomes achieved statistical significance, suggesting that our broader conceptual model has explanatory value across diverse transformation outcomes. The model for “altered decisions” (PTT 3) had the best fit, with an adjusted R2 of 0.23. Several important findings emerged when examining specific predictors of each of the PTT indicators.
For life change (PTT 1), 11% of the variance is explained by the predictors. Being younger (β = −.14), having more types of treatment (β = .15), and feeling more stigmatized (β = .16) were uniquely and significantly associated with this outcome.
For survivor identity adopted (PTT 2), the predictors together explain 12% of the variance. However, none of the cumulative stress exposure variables have a statistically significant impact on this outcome. The variables that have significant net effects on this outcome include having fewer years of education (β = −.13), greater concern over stigma (β = .14), and feeling more stigmatized (β = .19).
For decisions altered (PTT 3), together the predictors explain 23% of the total variance. Statistically significant individual predictors include demographic characteristics and indicators of stress appraisal. Demographic predictors include being younger (β = −.13), being a woman (β = .16), and having more years of education (β = .13). Indicators of stress appraisal showed significant independent effects on whether cancer altered life decisions. These include appraising cancer as more stressful (β = .19), having more cancer worry (β = .21), having more concern over sigma (β = .14), and reporting being stigmatized (β = .15).
Regarding problems minimized (PTT 4), the predictors explained only 8% of the variance. Younger age had a significant effect (β = −.12). None of the stress exposure variables were significant predictors. Among stress appraisals, worry about recurrence of illness (β = .13) and concerns over stigma (β = .17) proved to be significant.
For changes in religiosity (PTT 5), predictors explain 9% of the variance. Only 2 predictors are statistically significant and predictive of reporting enhanced religiosity. They are being younger (β = −.12) and being African American (β = .19).
Finally, we consider the predictors of the outcome changes in closeness to family (PTT 6), which explain 16% of the variance. Statistically significant demographic predictors include being African American (β = .18) and having less education (β = −.12). Regarding cumulative stress exposure predictors, statistically significant variables include having a more advanced stage of cancer (β = .11) and experiencing more health-related symptoms (β = .15). Regarding stress appraisal, experiencing greater concern regarding stigma was predictive of feeling closer to family (β = .11).
Discussion
Our descriptive findings reveal that, among older adults, being a long-term cancer survivor is viewed as a transformative experience and as an important part of respondents’ identities. Cancer survivorship remains a salient identity for the majority of this group long after the treatment phase of their illness. Our findings also indicate that transformations reported by survivors are complex. Although they may reflect aspects of PTG, they also incorporate recognition of changes in one’s assumptive world, which reflect vulnerability.44 Embracing a survivor identity may be viewed as a reassertion of one’s self-worth. At the same time, the belief that one has become a changed person who has altered the decisions about what is important in life incorporates both a sense of loss and enhanced maturity, after surviving cancer.12,44 Transformations may evolve over long periods, as part of meaning making, which helps individuals assimilate the trauma into their new identity.
Our multivariate analyses reveal some shared, as well as some distinctive, correlates of different aspects of transformations, reflecting altered life perspectives. Feeling stigmatized was associated with all 3 of 4 dimensions of general transformations, but appeared unrelated to domain specific transformations. It is noteworthy that although feelings of stigmatization are not common in our sample, they play an important role in impacting multiple domains of transformation.45
Our finding that younger age in our sample is significantly associated with 4 of the 6 PTT outcomes is consistent with prior research.46 Developing cancer at a relatively younger age, even in an older population, poses a greater threat to life expectancy and to identity and could consequently result in greater transformation.27 Being female was positively associated with reporting decision-altering transformations subsequent to cancer. Although race was not associated with any of the general transformation outcomes, African American respondents reported greater increases in religiosity and in family closeness subsequent to cancer than did their white counterparts. These results may be interpreted as reflecting culturally salient dimensions of coping with trauma, such as finding meaning in religious expression among African American older adults.47,48 Indeed, prior research shows greater evidence of PTG among African Americans who had experienced life-threatening illness than among other racial groups.47
It is notable that cumulative stress exposure was not associated with most of the transformation outcomes. These findings are consistent with the growing recognition that stress exposure may impact individuals very differently49 and confirm the significant role played by personal appraisals of stress exposure.50 The importance of processing memories of the traumatic experience51 and searching for meaning22 is that they can promote transformative views of the self. The survivor may never fully recapture the self-image of good health and invulnerability.51 Also, feeling even slightly stigmatized could serve as a significant impetus for transformation, given that individuals perceive themselves through the perceptions of others.
Limitations of the Study
Before discussing practice implications of our study, several limitations must be noted The sample was obtained from an urban, university-based cancer center in a Midwestern city, and thus, findings may not be generalizable to rural populations or other regions of the United States. Limitations of our study also include the use of cross-sectional data, which does not allow for definitive establishment of causal sequencing among the variables. Nevertheless, we note that theory and logic are consistent with the causal ordering suggested in our study. Prior studies have documented different concerns and sequelae among survivors during different phases of survivorship.52 Because all of our respondents are older and are long-term cancer survivors, our data cannot be generalized to young cancer survivors or to patients who are in the early phases of survivorship.19 We acknowledge that there may be recall bias in reports of cancer survivors about the trauma or stress posed by their cancer, as respondents had the diagnosis of cancer, on average, 10 years before their study participation. The multivariate analyses presented explained a statistically significant but relatively modest proportion of the total variance in 4 of the 6 PTTs considered. Personality variables and coping dispositions may be profitably considered in future studies, in an effort to increase the explanatory value of the model. Thus, individuals with an early life history of openness to experience53 and those who may engage in positive coping may be more likely to process traumatic experiences in a way that creates meaning and positive reappraisals of stressful circumstances.
Conclusions and Implications for Practice
As we consider implications of our findings for cancer survivors, several useful observations emerge from our study. In our earlier research on this sample,43 survivors demonstrated an absence of major clinical psychopathology, such as PTSD. Nevertheless, survivors did evidence somewhat higher levels of depression than the general population. Findings of the present study regarding increased closeness of survivors to their family reflect resilience among survivors.49 Respondents were cognizant of the multiple ways that cancer survivorship has altered their life perspectives.54 Our study also contributes to the growing recognition within the field of psycho-oncology that living with cancer is a transformative experience that results in both positive and negative outcomes.7 Our findings support the view that unidimensional focus on PTG and benefit finding in the aftermath of cancer represent an oversimplification of the complex transformations in identity that result from the pervasive threat of this illness.54
As cancer survivors, including the elderly, can expect to live for longer periods following cancer diagnosis, practicing nurses can benefit from better understanding the diversity in survivor quality-of-life outcomes, including altered life perspectives.36 Recognition that survivors may live with dual outcomes of benefit finding and distress about altered identity allows nurse practitioners to be more sensitive to both survivor strengths and concerns. Awareness of such long-term prospects can help reinforce hope during earlier treatment phases, although it can also direct attention to psychological needs of long-term survivors.49 Our findings also raise awareness about the role of lingering worry about the future and concern about the stigma of cancer as issues impacting cancer survivor outcomes. Because older patients may be reticent to share such concerns, clinicians may find it useful to elicit discussion about these problems. Our findings also call for clinical attention being directed at women and relatively younger cancer survivors who are more likely to report major transformations in the aftermath of their cancer.
Our study also offers some useful guidelines for nurses for initiating discussions with patients who are long-term cancer survivors about their appraisals of their cancer experience. Eliciting the patient’s perspectives has therapeutic value as it affirms both respect and empathy.3 It also opens the door for patients to articulate how the illness experience has transformed their life outlook and identities even long after the treatment phase.4 Nurses and other clinical staff working with cancer survivors can benefit from recognizing the life-changing nature of the cancer experience. Indeed, nurse professionals are at the forefront of planning for care of cancer survivors.5,55 Discussion of specific changes in life outlook and specific transformations experienced by survivors can open the dialogue to meaning making and acceptance of a changed self. Nurses, oncologists, and primary care physicians, as well as mental health professionals, can benefit from communicating about patients’ appraisals of their illness, issues of stigma, and the life-changing nature of the cancer experience.45,56 Recognition that changes may incorporate elements of suffering as well as positive transcendence can also help patients accept the complex emotions and cognitive reorganization that they may be experiencing. Such therapeutic interactions can provide cancer patients with the tools to deal with both the promise and the challenges of long-term survivorship.36
Acknowledgments
The authors thank Jane A. Brown, PhD, and Melinda Loroco, MA, for their contributions to earlier drafts of this article.
This research was supported by grant RO1-CA78975 from the National Cancer Institute, National Institutes of Health.
References
- 1.Avis E, Deimling G. Cancer survivorship and aging. Cancer. 2008;113(S12):3519–3529. doi: 10.1002/cncr.23941. [DOI] [PubMed] [Google Scholar]
- 2.Wyatt G, Friedman L. Long-term female cancer survivors: quality of life issues and clinical implications. Cancer Nurs. 1996;19(1):1–7. doi: 10.1097/00002820-199602000-00001. [DOI] [PubMed] [Google Scholar]
- 3.King C, Hines P, editors. Quality of Life: From Nursing & Patient Perspectives. Sudbury, MA: Jones & Bartlett; 2003. [Google Scholar]
- 4.Jacobsen P. Clinical practice guidelines for the psychosocial care of cancer survivors. Cancer. 2009;115(S18):4419–4429. doi: 10.1002/cncr.24589. [DOI] [PubMed] [Google Scholar]
- 5.Haylock P, Mitchell S, Cox T, Temple S, Curtiss C. The cancer survivor’s prescription for living. Am J Nurs. 2007;107(4):58–70. doi: 10.1097/01.NAJ.0000265276.92317.b2. [DOI] [PubMed] [Google Scholar]
- 6.Smyth J. Disclosing gaps between supportive and palliative care- the past 20 years. Support Care Cancer. 2008;16(2):109–111. doi: 10.1007/s00520-007-0354-4. [DOI] [PubMed] [Google Scholar]
- 7.Doyle N. Cancer survivorship: evolutionary concept analysis. J Adv Nurs. 2008;62(4):499–509. doi: 10.1111/j.1365-2648.2008.04617.x. [DOI] [PubMed] [Google Scholar]
- 8.Smith M, Redd W, Peyser C, Vogl D. Post-traumatic stress disorder in cancer: a review. Psychooncology. 1999;8(6):521–537. doi: 10.1002/(sici)1099-1611(199911/12)8:6<521::aid-pon423>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 9.Zoellner T, Maercker A. Posttraumatic growth in clinical psychology- a critical review and introduction of a two component model. Clin Psychol Rev. 2006;26(5):626–653. doi: 10.1016/j.cpr.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Deimling GT, Bowman KF, Wagner LJ. Cancer survivorshipand identity among long-term survivors. Cancer Invest. 2007;25:758–765. doi: 10.1080/07357900600896323. [DOI] [PubMed] [Google Scholar]
- 11.Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Calhoun LG, Tedeschi RG, editors. Handbook of Posttraumatic Growth: Research and Practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2006. pp. 138–175. [Google Scholar]
- 12.McCorkle R, Hughes L, Robinson L, Levine B, Nuamah I. Nursing interventions for newly diagnosed older cancer patients facing terminal illness. J Palliat Care. 1998;14(3):39–45. [PubMed] [Google Scholar]
- 13.Arman M, Rehnsfeldt A. The hidden suffering among breast cancer patients: a qualitative metasynthesis. Qual Health Res. 2003;13(4):510–527. doi: 10.1177/1049732302250721. [DOI] [PubMed] [Google Scholar]
- 14.Aldwin C. Stress, Coping, and Development: An Integrative Perspective. New York, NY: Guilford Press; 2000. [Google Scholar]
- 15.Janoff-Bulman R. Shattered Assumptions Towards a New Psychology of Trauma. New York: Free Press; 1992. [Google Scholar]
- 16.Carpenter J, Brockopp D, Andrykowski M. Self-transformation as a factor in the self-esteem and well-being of breast cancer survivors. J Adv Nurs. 1999;29(6):1402–1411. doi: 10.1046/j.1365-2648.1999.01027.x. [DOI] [PubMed] [Google Scholar]
- 17.Lauver DR, Connolly-Nelson K, Vang P. Stressors and coping strategies among female cancer survivors after treatments. Cancer Nurs. 2007;30(2):101–111. doi: 10.1097/01.NCC.0000265003.56817.2c. [DOI] [PubMed] [Google Scholar]
- 18.Frank A. The Wounded Storyteller: Body, Illness, and Ethics. Chicago, IL: University of Chicago Press; 1995. [Google Scholar]
- 19.Harpham W. A Guide to Your New Life. New York, NY: Harper Perennial; 1995. [Google Scholar]
- 20.Tedeschi RG, Park CL, Calhoun LG. Posttraumatic growth: conceptual issues. In: Tedeschi RG, Park CL, Calhoun LG, editors. Posttraumatic Growth: Positive Changes in the Aftermath of Crisis. Mahwah, NJ: Lawrence Erlbaum Associates; 1998. pp. 1–22. [Google Scholar]
- 21.Alferi S, Culver J, Carver C, Arena P, Antoni M. Religiosity, religious coping, and distress: a prospective study of catholic and evangelical Hispanic women in treatment for early-stage breast cancer. Health Psychol. 1999;4(3):343–356. doi: 10.1177/135910539900400304. [DOI] [PubMed] [Google Scholar]
- 22.Frankl V. Man’s Search for Meaning. New York, NY: Touchstone; 1984. [Google Scholar]
- 23.Kahana B, Kahana E. Toward a temporal-spatial model of cumulative life stress: placing late life stress effects in life course perspective. In: Lomranz J, editor. Handbook of Aging and Mental Health: An Integrative Approach. New York, NY: Plenum; 1998. pp. 153–178. [Google Scholar]
- 24.Lazarus R, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publishing Company; 1984. [Google Scholar]
- 25.Werner E, Smith R. Overcoming the Odds: High Risk Children From Birth to Adulthood. Ithaca, NY: Cornell University Press; 1992. [Google Scholar]
- 26.Lechner S, Zakowski S, Antoni M, et al. Do sociodemographic and disease-related variables influence benefit-finding in cancer patients? Psychooncology. 2003;12(5):491–499. doi: 10.1002/pon.671. [DOI] [PubMed] [Google Scholar]
- 27.Sammarco A. Quality of life of breast cancer survivors: a comparative study of age cohorts. Cancer Nurs. 2009;32(5):347–356. doi: 10.1097/NCC.0b013e31819e23b7. [DOI] [PubMed] [Google Scholar]
- 28.Russell K, Von AD, Giesler R, Storniolo A, Haase J. Quality of life of African-American breast cancer survivors: how much do we know? Cancer Nurs. 2008;32(6):E36–E45. doi: 10.1097/01.NCC.0000339254.68324.d7. [DOI] [PubMed] [Google Scholar]
- 29.Deimling G, Kahana B, Bowman K, Schaefer M. Cancer survivorship and psychological distress in later life. Psychooncology. 2002;11:479–494. doi: 10.1002/pon.614. [DOI] [PubMed] [Google Scholar]
- 30.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 31.Pelusi J, Krebs L. Understanding cancer-understanding the stories of life and living. J Cancer Educ. 2005;20(1):12–16. doi: 10.1207/s15430154jce2001s_04. [DOI] [PubMed] [Google Scholar]
- 32.Fife B, Wright E. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. 2000;41:50–67. [PubMed] [Google Scholar]
- 33.Herman J. Trauma and Recovery: The Aftermath of Violence From Domestic Abuse to Political Terror. New York, NY: Basic Books; 1992. [Google Scholar]
- 34.Nagi S. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q. 1976;92:101–103. [PubMed] [Google Scholar]
- 35.Greenlee RT, Hill-Harmon MB, Murray T, Thun M. Cancer statistics—2001. CA Cancer J Clin. 2001;51:15–38. doi: 10.3322/canjclin.51.1.15. [DOI] [PubMed] [Google Scholar]
- 36.Rowland J, Aziz N, Tesauro G, Feuer E. The changing face of cancer survivorship. Semin Oncol Nurs. 2001;17(4):236–240. doi: 10.1053/sonu.2001.27912. [DOI] [PubMed] [Google Scholar]
- 37.Society AC. Cancer Facts and Figures. Atlanta, GA: American Cancer Society; 2006. [Google Scholar]
- 38.Earle CC. Quality of care. In: Feuerstein M, editor. Handbook of Cancer Survivorship. New York, NY: Springer Publishing Company; 2007. pp. 19–42. [Google Scholar]
- 39.Armer J, Radina M, Porock D, Culbertson S. Predicting breast cancer-related lymphedema using self-reported symptoms. Nurs Res. 2003;52(6):370–379. doi: 10.1097/00006199-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Deimling G, Sterns S, Bowman K, Kahana B. The health of older-adult, long-term cancer survivors. Cancer Nurs. 2005;28(6):415–424. doi: 10.1097/00002820-200511000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Kahana E, Fairchild T, Kahana B. Adaptation. In: Mangen DJ, Peterson W, editors. Research Instruments in Social Gerontology: Clinical and Social Psychology. Vol. 1. Minneapolis, MN: University of Minnesota Press; 1982. pp. 145–193. [Google Scholar]
- 42.Gotay CC, Shimizu H, Muraoka M, et al. Cancer-related attitudes: a comparative study in Japan and the US. Psychooncology. 2004;13:665–672. doi: 10.1002/pon.792. [DOI] [PubMed] [Google Scholar]
- 43.Deimling G, Bowman K, Sterns S, Wagner L, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15(4):306–320. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- 44.Collins R, Taylor S, Skokan L. A better world or a shattered vision? Soc Cogn. 1990;8(3):263–285. [Google Scholar]
- 45.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer. Br Med J. 2004;328(7454):1470–1473. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manne S, Ostroff J, Winkel G, et al. Posttraumatic growth after breast cancer: patient, partner, and couple perspectives. Psychosom Med. 2004;66(3):442–454. doi: 10.1097/01.psy.0000127689.38525.7d. [DOI] [PubMed] [Google Scholar]
- 47.Boswell GH, Kahana E, Dilworth-Anderson P. Spirituality and healthy lifestyle behaviors: stress counter-balancing effects on the well-being of older adults. J Relig Health. 2006;45(4):587–602. [Google Scholar]
- 48.Hamilton JB, Powe BD, Pollard AB, Lee KJ, Felton AM. Spirituality among African American cancer survivors: having a personal relationship with God. Cancer Nurs. 2007;30(4):309–316. doi: 10.1097/01.NCC.0000281730.17985.f5. [DOI] [PubMed] [Google Scholar]
- 49.Lent RW. Restoring emotional well-being: a model. In: Feuerstein M, editor. Handbook of Cancer Survivorship. New York, NY: Springer Publishing Company; 2007. pp. 231–248. [Google Scholar]
- 50.Thoits P. Personal agency in the stress process. J Health Soc Behav. 2006;47(4):309–323. doi: 10.1177/002214650604700401. [DOI] [PubMed] [Google Scholar]
- 51.Horowitz M. Stress-response syndromes: a review of posttraumatic and adjustment disorders. Hosp Community Psychol. 1986;37(3):241–249. doi: 10.1176/ps.37.3.241. [DOI] [PubMed] [Google Scholar]
- 52.Garofalo J, Choppala S, Hamann H, Gjerde J. Uncertainty during the transition from cancer patient to survivor. Cancer Nurs. 2009;32(4):E8–E14. doi: 10.1097/NCC.0b013e31819f1aab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Costa P, McCrae R. Trait theories of personality. In: Barone DF, Hersen M, Van Hasselt VB, editors. Advanced Personality. New York, NY: Plenum Press; 1998. pp. 103–121. [Google Scholar]
- 54.Sumalla E, Ochoa C, Blanco I. Posttraumatic growth in cancer: reality or illusion. Clin Psychol Rev. 2009;29(1):24–33. doi: 10.1016/j.cpr.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 55.Miller R. Implementing a survivorship care plan for patients with breast cancer. Clin J Oncol Nurs. 2008;12(3):479–487. doi: 10.1188/08.CJON.479-487. [DOI] [PubMed] [Google Scholar]
- 56.Heidrich S, Brown R, Egan J, et al. An individualized representational intervention to improve symptom management (IRIS) in older breast cancer survivors: three pilot studies. Oncol Nurs Forum. 2009;36(3):E133–E143. doi: 10.1188/09.ONF.E133-E143. [DOI] [PMC free article] [PubMed] [Google Scholar]


