Abstract
Scientific advances, open information access, and evolving health-care economics are disrupting extant models of health-care delivery. Physicians increasingly practice as team members, accountable to payers and patients, with improved efficiency, value, and quality. This change along with a greater focus on population health affects how systems of care are structured and delivered. Pathologists are not immune to these disruptors and, in fact, may be one of the most affected medical specialties. In the coming decades, it is likely that the number of practicing pathologists will decline, requiring each pathologist to serve more and often sicker patients. The demand for increasingly sophisticated yet broader diagnostic skills will continue to grow. This will require pathologists to acquire appropriate professional training and interpersonal skills. Today’s pathology training programs are ill designed to prepare such practitioners. The time to practice for most pathology trainees is typically 5 to 6 years. Yet, trainees often lack sufficient experience to practice independently and effectively. Many studies have recognized these challenges suggesting that more effective training for this new century can be implemented. Building on the strengths of existing programs, we propose a redesign of pathology residency training that will meet (and encourage) a continuing evolution of American Board of Pathology and Accreditation Council for Graduate Medical Education requirements, reduce the time to readiness for practice, and produce more effective, interactive, and adaptable pathologists. The essence of this new model is clear definition and acquisition of core knowledge and practice skills that span the anatomic and clinical pathology continuum during the first 2 years, assessed by competency-based metrics with emphasis on critical thinking and skill acquisition, followed by individualized modular training with intensively progressive responsibility during the final years of training. We anticipate that implementing some or all aspects of this model will enable residents to attain a higher level of competency within the current time-based constraints of residency training.
Keywords: competency, progressive responsibility, residency training
Introduction
The practice of medicine is undergoing its most rapid period of change since the Flexner era of the early 1900s. The triple aim of improving the patient experience, improving the health of populations, and reducing the per capita cost of health care is driving health-care delivery systems to thrive under prospective budget-based payment models and/or alternative payment models involving pay-for-performance and provider financial risk.1,2 Beyond these economic imperatives, the following are 3 fundamental forces driving the 21st century medicine: (1) patient-centric care, (2) democratization of the “information gap,” and (3) accountability for safety and quality.3 These forces will profoundly affect the role of the 21st century pathologists and challenge the programs responsible for training them.
Twenty-First Century Medicine Is Patient Centric
Aging populations experience more illness. Advancing scientific and medical knowledge expands the repertoire of diagnostic tests and treatment options. Economics requires these to be used appropriately and effectively on a patient-by-patient basis. Coupled with widespread adoption of electronic medical records, this drives medicine toward standardized, evidence-driven practice in large systems, by health-care teams including generalists managing health maintenance and routine care, specialists managing disease or organ system–specific care, and other specialists (including pathologists and radiologists) providing diagnostic expertise. Patients are followed longitudinally as they receive preventive care and wellness management, interspersed with episodic care for acute illness and management of chronic disease, disability, and comorbidity. Patients fall into cohorts allowing well-designed health-care systems to tailor patient-specific and condition-specific diagnostic and treatment plans based on accurate diagnosis and data analytics. Outcomes improve through more effective care management with reduction in the costs3 of ineffective care (Figure 1 shows 1 example).
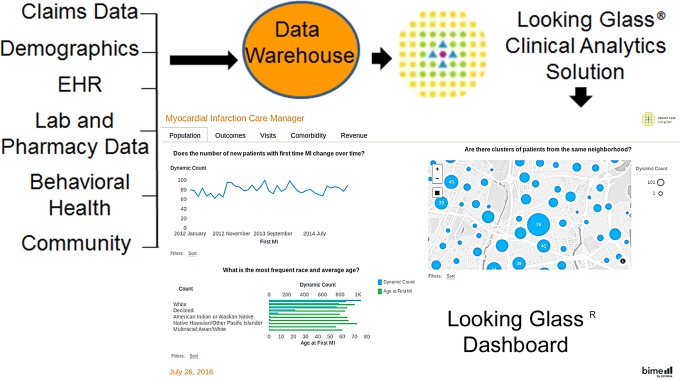
Figure 1.
Predictive analytics and intelligence.4,5 Looking Glass Clinical Analytics (formerly Clinical Looking Glass [CLG]) is designed to capture and transform masses of data in order to improve patient care and care coordination, enable medical centers to improve performance, and expose opportunities for achieving breakthroughs in clinical practice. Pathologists working in health-care teams can use existing data to drive continuous quality improvement. Looking Glass Clinical Analytics will help determine and align clinical best practice, proactively identify readmission risk across populations, and conduct comparative effectiveness research. Reprinted from Streamline Health with permission.
Twenty-First Century Medicine—Democratization of the Information Gap
Patients and physicians alike have instant access to the world’s information. No longer is access to the “facts” the privileged resource of the trained professional. This reality is already transforming pedagogy in our universities and medical schools, where the emphasis of education has shifted from assimilating facts to an emphasis on critical thinking and effective and appropriate use of the vast information resources instantly available. It is also rapidly transforming the patient–physician relationship. Patients now expect to be fully informed of their conditions, are increasingly aware of health risks and treatment options, and are better equipped to shop for “optimal” treatment. The individual patient acquires “agency,”6 with more control over care than in times past. Health-care services provided for the benefit of the patient must thus be aligned with the patient’s expectations and consent. Health-care providers must learn to communicate, both with each other in a health-care team across the electronic interface and with patients.7 The role of physicians, and particularly pathologists, in this new environment will increasingly center on their success as “critical thinkers” who apply wisdom and skill in optimally guiding diagnostic and treatment decisions and as communicators to clinical colleagues and patients. Thus, the pathologist’s primary obligation will be as an expert consultant to the patient, directly and/or as a member of the patient’s health-care team (Figure 2). Currently, residents interact directly with the patient and health-care team in a variety of areas including the following: cytopathology (fine needle aspiration), transfusion medicine (apheresis and donor services), microbiology, hematology/coagulation, genetics, and tumor board.
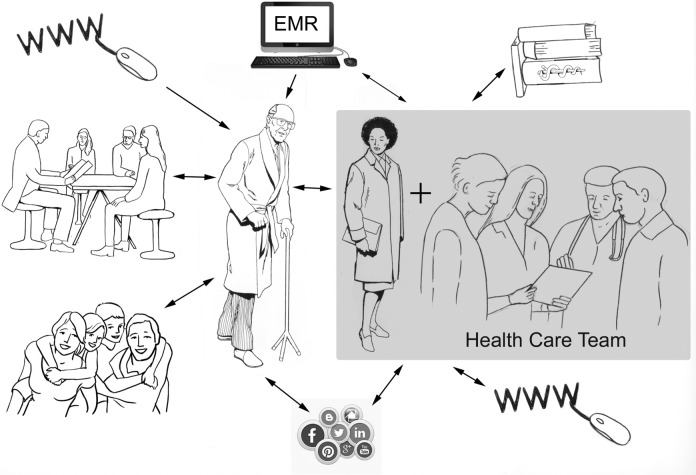
Figure 2.
Bridging the information gap.7 Patients have access to information from the Internet, social media, friends, and family as well as their health-care team. This information shapes the communication with their team, which can be face-to-face, or via the electronic medical record, which patients can access via a “patient portal.” Because patients have access to so much information and relatively limited ability to evaluate it, the challenge for the team is to explain medical information to the patient efficiently and effectively to achieve an optimal course of care for the patient. The health-care team consists of the primary care clinician, treating and diagnostic specialists, and other health-care workers. The pathologist, a member of the team, advises on diagnostic test selection, ensures test accuracy, and communicates the results to the treating professionals; at times, the pathologist explains the test results directly to the patient. The pathologist contributes to the medical literature through investigation and communication that advance evidence-based medicine. In addition, the pathologist educates the health-care team and disseminates information through the Internet and social media.
Twenty-First Century Medicine—Accountability for Quality and Safety
Accountability in medical practice was a central theme of the 1999 Institute of Medicine (IOM) report, To Err is Human 8,9; the 2015 IOM report, Improving Diagnosis in Healthcare,10 highlighted the problem of diagnostic error. Diagnostic error is defined as “the failure to (a) establish an accurate and timely explanation of the patient’s health problem(s) or (b) communicate that explanation to the patient.” The mitigation of diagnostic error presents an enormous challenge in health care and also an immense opportunity for pathologists.11 As integral members of the health-care team, pathologists are optimally situated and oriented to mitigate errors at all phases of the diagnostic process. Pathologists own the analytic process and are skilled at using quality measures to detect and minimize error. Their activities thus undergird many aspects of diagnostic medicine. However, because many errors originate in the preanalytic and postanalytic phases, pathologists need to engage health-care teams throughout the health-care process, not just at the point of diagnostic interpretation (Figure 3).
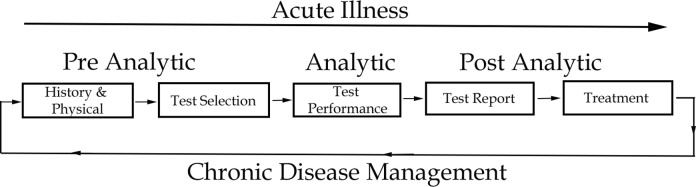
Figure 3.
Pathologist role in the diagnostic process. Pathologists must actively engage as part of the health-care team. Working within the health-care team in preanalytics, the pathologist facilitates optimal test selection, ensures accuracy in the analytic phase, and synthesizes data in the postanalytic phase, minimizing time-to-diagnosis and reducing time-to-effective intervention. Active involvement by the pathologist yields health-care efficiencies and reduces diagnostic failures. Tracking longitudinal data and providing integrated reports enable the team to develop and maintain an optimal treatment plan for managing chronic disease.
Existing Training Programs Do Not Address the 21st Century Challenges
Although hard to generalize, 5 shortcomings of our existing training programs are commonly recognized: (1) they take too long, (2) their graduates are often not fully ready for independent practice, (3) their curriculum is fragmented into a series of narrow subspecialties, (4) they lack sufficient training in communication skills and teamwork reflective of how modern medicine is practiced, and (5) they need to provide more opportunity for residents to gain direct experience as a consultant.
The pathway to practice across all medical specialties has been a residency, typically followed by subspecialty fellowship. The American Board of Pathology (ABP) recognizes 4 primary certification tracks: dual certification in anatomic and clinical pathology (AP/CP) or AP and neuropathology or single certification in AP or CP. The dual certification tracks are both 4-year residencies; the single certification tracks are both 3-year residencies. Approximately, 85% of pathology residents pursue dual certification in AP/CP.
In 1985, the ABP adopted a requirement of an additional “credentialing” year for board certification, extending the duration of preparation for practice to 5 years for dual certificate tracks and 4 years for single certificate tracks. This requirement was eliminated in 2002, with the unintended consequence of a “double dose” of graduating board-eligible trainees in 2006.12 This sudden influx of trainees entering an already-tight job market accelerated the trend to pursue fellowship training, a trend reinforced by employer’s realization that a 3- to 4-year period of generic categorical training in pathology did not reliably qualify graduates for successful independent practice.13 This trend toward supernumerary years of pathology training continues. In the 2015 American Society for Clinical Pathology Resident In-Service Examination survey, only 4% of residents did not expect to take a fellowship, 52% of residents expected to take 1 fellowship, 43% expected to take 2 fellowships, and 1% expected to take more than 2 fellowships (Figure 4). The average number of fellowships per pathology trainee was ∼1.4. With 85% of trainees in 4-year residency tracks and 15% in 3-year tracks, this amounts to an average of ∼5.3 years of cumulative residency and fellowship training.14,15 Unless staunched, the trajectory of this trend toward longer cumulative training is likely to continue, exacerbating the declining number of pathologists available to address increasing demands of their expanded roles in the health-care team (Figure 5).16,17
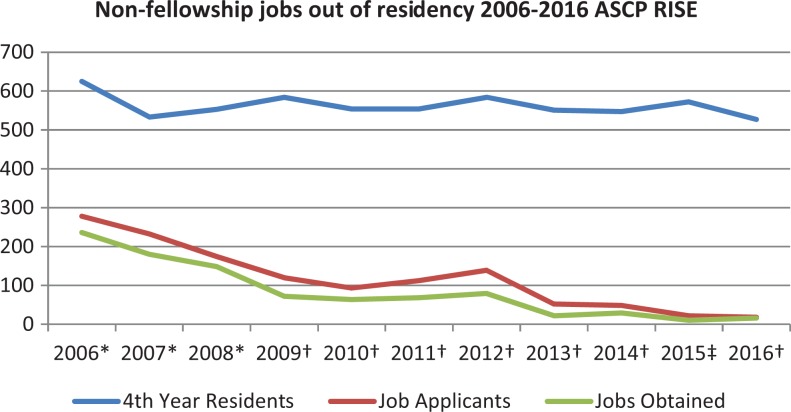
Figure 4.
Pathology trainee fellowship trends.14,15 Although the yearly number of fourth-year pathology residents has varied only slightly over the past decade, the fraction of graduates applying for or obtaining jobs without first taking fellowship training has decreased from about 40% at the beginning of the decade to less than 4% by its end. This change reflects the perception by both trainees and their prospective employers that the preparation provided by residency is insufficient for practice. *2006 to 2008 job applicants and jobs obtained reported among Resident In-Service Examination (RISE)-taking postgraduate year (PGY)-4 residents and fellows. †2009 to 2014 and 2016 job applicants and jobs obtained reported among RISE-taking PGY-3 and PGY-4 residents. ‡2015 job applicants reported among RISE-taking PGY-3 and PGY-4 residents; jobs obtained reported only among RISE-taking PGY-4 job applicants.
Figure 5.
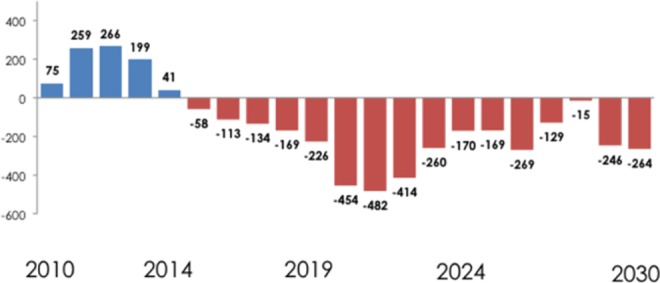
Predicted net loss of practicing pathologists from the workforce. Starting in 2014, the number of pathologists leaving practice is predicted to exceed the number of pathologists entering practice, resulting in a cumulative net decrease of approximately 3500 pathologists by 2030. Given continuing population growth, this will result in an even greater decrease in the number of pathologists per patient, with people living longer and the aging population also experiencing more chronic illness. Reprinted from Archives of Pathology and Laboratory Medicine with permission.17
Existing training is also commonly fragmented across both the AP/CP divide and narrow, typically AP, subspecialties. Although 4-year AP/CP training programs nominally offer 18 (4-week) months of focused AP and 18 months of CP training and 1 “flexible” year of electives for development as a practitioner, the modal program in 2013 was actually 27 months of AP and 18 of CP, with only 3 for flexible electives. This training is then most often followed by fellowship in a subspecialty of AP, yielding a higher level of diagnostic skill in a narrower area and extending the time in training (Figure 6). This type of training also results in segmented exposure to most areas of pathology practice and hinders holistic disease-based learning, that is, there is no systematic integration of AP-based disease and organ system diagnosis with clinical laboratory findings. That such a divide continues to persist is remarkable, given the advent of computational and molecular advances that blur the distinctions between AP and CP. With so much effort and attention given to the development of focused diagnostic skills, there is less focus on the communication and interpersonal skills required for team practice.18,19 One area of training that may be an exception and thus serve as a useful paradigm for the way forward is hematopathology. Practice in this specialty comes the closest to integrating all aspects of pathology to yield optimally actionable patient information and maximal value to the health-care team; the close interaction of hematopathologists and hematologist/oncologists demonstrates the value of this paradigm. Thus, hematopathology can serve as an example of how our residents should approach every diagnostic area. This integrated and team-oriented approach will enable trainees to attain a higher level of competency within the 4-year training period and become adaptable practitioners in their future career (Table 1 lists a representative series of milestones, with their corresponding competencies, and potential measures).
Figure 6.
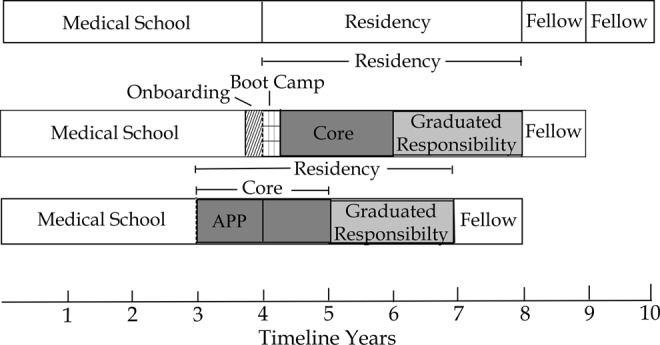
Time to competency for practicing pathology. The current training model for anatomic and clinical pathology with 1 or 2 fellowships is typically 9 to 10 years including medical school. Even so, community pathologists express opinions that many of our trainees lack specific practice skills. Altering our training process can reduce the time to competency by introducing practice skills earlier in training and accelerating graduated responsibility. In addition, an advanced pathology practice pathway (APP) providing a continuum from medical school through residency could reduce the time to practice by another year.
Table 1.
The Pathology Milestone Project.*
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 |
|---|---|---|---|---|
| PC1: Consultation: Analyzes, Appraises, Formulates, Generates, and Effectively Reports Consultation (AP and CP). Evaluation Methods: Direct Observation, Retrospective Peer Review, Portfolio, Feedback From Clinical Colleagues (360 Evaluations), Peer Review, and HIPAA Training Documentation Provided | ||||
| Understands the implications of and the need for a consultation | Prepares a draft consultative report (verbal or written) | Prepares a full consultative report with a written opinion for common diseases | Independently prepares a full consultative written report with comprehensive review of medical records on common and uncommon diseases | Proficient in pathology consultations with comprehensive review of medical records |
| Understands the concept of a critical value and the read-back procedure | Knows the critical value list and participates in the critical value callback of results | Applies the escalation procedure for failed critical value callbacks | Recommends new or alternate escalation procedures for failed critical value callbacks as needed | Participates in intuitional processes of generating the critical value list |
| Understands that advanced precision diagnostics, personalized medicine (eg, molecular diagnostic testing), may be applied to patient care for genetic, neoplastic, and infectious disorders and population health | Understands the role of specific advanced precision diagnostics and personalized medicine assays, and how results affect patient diagnosis and prognosis, and overall | Understands preanalytic issues and quality control for advanced precision diagnostics and personalized medicine | Provides consultation, as needed, to clinicians about utilization and interpretation of advanced precision diagnostics and personalized medicine | Is proficient in consultation regarding test utilization and treatment decisions based on advanced precision diagnostics and personalized medicine |
| PC2: Interpretation and Reporting: Analyzes Data, Appraises, Formulates, and Generates Effective and Timely Reports (CP). Evaluation Methods: Direct Observation, Simulation, Feedback From Clinical Colleagues (360 Evaluations), Retrospective Peer Review, and Quality Management Results | ||||
| Identifies key elements in the health-care record | Uses clinical correlation to interpret and report test results | Limits and focuses a differential diagnosis | Able to lead discussion on developing a differential diagnosis based upon clinical information | Proficient in using health-care records and clinical information to develop a limited and focused differential diagnosis |
| Observes and assists in the interpretation and reporting of the diagnostic test | Accurately interprets and reports the results | Prepares a differential diagnosis for abnormal results | Knows potential confounding factors that may contribute to erroneous results | Proficient in the interpretation and reporting of clinical pathology test results in the context of the patient’s medical condition |
| Understands indications for common tests | Understands and applies algorithms in the work-up for common diagnoses | Understands and applies algorithms in the work-up for common and uncommon diagnoses | Understands and prudently applies justification for approval of costly testing | Writes policies on algorithms for testing |
| PC3: Interpretation and Diagnosis: Demonstrates Knowledge and Practices Interpretation and Analysis to Formulate Diagnoses (AP). Evaluation Methods: Direct Observation, Simulation, Feedback From Clinical Colleagues (360 Evaluations), and Examination | ||||
| Distinguishes normal from abnormal histology and recognizes confounding factors | Consistently recognizes, correctly identifies common histopathologic findings (develops a “good eye”) and able to troubleshoot (eg, tissue artifacts, processing, and sampling issues) | Makes accurate diagnoses reliably, appreciates the nuances of diseases, and is able to independently troubleshoot confounding factors | Assesses, analyzes, and is able to distinguish subtle differences in difficult cases | |
| Recognizes the importance of a complete pathology report for patient care | Begins to make connections between clinical differential diagnosis, gross, and microscopic pathologic findings | Correlates the clinical differential diagnosis with gross and microscopic pathologic findings | Analyzes complex cases, integrates literature, and prepares a full consultative written report with comprehensive review of medical records. Interprets ancillary testing results in clinical context | Proficient in interpretation with comprehensive review of medical records |
| PC4: Reporting: Analyzes Data, Appraises, Formulates, and Generates Effective and Timely Reports (AP). Evaluation Methods: Direct Observation, Narrative, Feedback From Clinical Colleagues (360 Evaluations), and Retrospective Peer Review | ||||
| Applies prior knowledge and draws on resources to learn normal gross anatomy, histology, and special techniques | Attends and contributes to gross and microscopic conferences | Reliably applies knowledge of gross and histologic features in formulating a diagnosis for common entities and able to present at gross conference | Reliably applies knowledge of gross and histologic features in formulating a diagnosis for common and uncommon entities | Produces timely reports with complete accurate gross and histopathologic findings, including ancillary studies, and integrates evidence-based medicine/current literature and knowledge |
| Recognizes the role of the surgical pathologist in the management of patients, including the utilization of cancer staging | Brings clinical/ancillary information to sign out (eg, radiology, prior cases, and reading about case) | Selects, orders, and interprets clinical/ancillary information to refine a differential diagnosis | Integrates clinical/ancillary information into report | Manages ambiguity and uncertainty in result interpretation and ancillary testing |
| PC5: Procedure: Surgical Pathology Grossing: Demonstrates Attitudes, Knowledge, and Practices That Enable Proficient Performance of Gross Examination (Analysis and Appraisal of Findings, Synthesis and Assembly, and Reporting; AP). Evaluation Methods: Direct Observation, 360 Evaluations, Periodic Self-Assessment, Narrative, Portfolio, and Quality Management | ||||
| Recognizes the importance of grossing for the interpretation of histology and management of patients | Correctly describes and appropriately samples common surgical specimens, including necessary tissues for ancillary studies in correct media/fixative | Applies principles of grossing to newly encountered specimen types | Correctly describes and appropriately samples all specimen types | Proficient in the performance of surgical pathology gross examination |
| Applies prior knowledge and draws on resources to learn normal gross anatomy | Understands the components of an appropriate and complete report | Produces reports that contain all the necessary information for patient management; edits transcribed reports effectively | Dictates complete, logical, and succinct descriptions | Proficient in the production of complete, logical, and succinct descriptions |
| PC6: Procedure: Intraoperative Consultation/Frozen Sections: Demonstrates Attitudes, Knowledge, and Practices That Enable Proficient Performance of Gross Examination, Frozen Section (Analysis and Appraisal of Findings, Synthesis And Assembly, and Reporting; AP). Evaluation Methods: Direct Observation, Narrative, Feedback From Clinical Colleagues (360 Evaluations), Retrospective Peer Review, Portfolio, and Quality Management | ||||
| Understands common surgical procedures and the resultant specimens and potential intraoperative consultation/frozen section/intraoperative cytology (IOC/FS) | Procures tissue for diagnosis under supervision | Correctly selects tissue for frozen section diagnosis independently | Responds appropriately to the concerns of the surgeon | Proficient in the performance of IOC/FS |
| PC7: Procedures: If Program Teaches Other Procedures (eg, Bone Marrow Aspiration, Apheresis, Fine-Needle Aspiration Biopsy, Ultrasound-Guided FNA, etc; AP/CP). Evaluation Methods: Direct Observation and Simulation | ||||
| Recognizes the role of the procedure | Observes and assists on the procedure | Obtains informed consent | Able to perform the procedure with minimal supervision | Proficient in the performance of the procedure |
| MK1: Diagnostic Knowledge: Demonstrates Attitudes, Knowledge, and Practices That Incorporate Evidence-Based Medicine and Promote Life-Long Learning (AP/CP). Evaluation Methods: Direct Observation, Pretest and Posttest, Rotation Exams, Narrative, 360 Evaluations, Board Examination, Maintenance of Certification/SAMs, RISE, and PRISE | ||||
| Identifies the resources for learning in pathology | Assimilates medical knowledge in pathology from various learning sources | Performs scientific literature review and investigation of clinical cases to inform patient care (evidence-based medicine) and improve diagnostic knowledge of pathology | Applies and synthesizes medical knowledge from scientific literature review and investigation to inform patient care (evidence-based medicine) | Contributes to medical knowledge of others and participates in life-long learning through literature review, CME, and SAMs |
| MK2: Teaching: Demonstrates Ability to Interpret, Synthesize, and Summarize Knowledge and Teaches Others (AP/CP). Evaluation Methods: Direct Observation, 360 Evaluations, Teaching Evaluations, Student Performance on Exams, Simulations, and Conference Presentation Evaluation Portfolio | ||||
| Participates in active learning | Understands and begins to acquire the skills needed for effective teaching | Teaches peers as needed | Teaches across departments and at all levels, including to clinicians, patients, and families | Models teaching across departments and at all levels, including for clinicians, patients, and families |
| MK3: Procedure: Autopsy: Demonstrates Knowledge and Practices That Enable Proficient Performance of a Complete Autopsy (Analysis and Appraisal of Findings, Synthesis and Assembly, and Reporting; AP). Evaluation Methods: Direct Observation, Feedback From Clinical Colleagues (360 Evaluations), Narrative, Portfolio Review, Quality Management, and Peer Evaluation | ||||
| Understands the value of an autopsy | Able to perform all 7 aspects of a routine autopsy | Able to plan and perform complex/difficult cases | Performs uncomplicated gross dissection within 4 hours | Proficient in the performance of a complete autopsy and in reporting the results in a timely manner |
| Understands the principles of confidentiality, universal precautions, chemical hazards, and personal protective equipment | Is aware of reporting regulations, such as legal jurisdiction, statutes regarding authorization to perform autopsy (medical examiner), device reporting, and communicable diseases | Understands chain of custody, the elements of scene investigation, trace evidence, and court testimony | Assesses and applies chain of custody, interprets the elements of scene investigation, trace evidence, and court testimony | Proficient in the discussion of the chain of custody and interpretation and assessment of the elements of scene investigation, trace evidence, and giving court testimony |
| SBP1: Patient Safety: Demonstrates Attitudes, Knowledge, and Practices That Contribute to Patient Safety (AP/CP). Evaluation Methods: Direct Observation, Narrative, QA Reports (Misidentification Rates and Amended Report Rates), Transfusion Committee Results/Work-Ups, and Documentation Provided | ||||
| Understands the importance of identity and integrity of the specimen and requisition form and verifies the identity | Consistently checks identity and integrity of specimen | Troubleshoots preanalytic problems, as needed, with minimal supervision, including deviations from policies (waivers) | Troubleshoots patient safety issues (including preanalytic, analytic, and postanalytic), as needed, without supervision | Writes and implements policies on patient safety, as needed |
| SBP2: Lab Management: Regulatory and Compliance: Explains, Recognizes, Summarizes, and Is Able to Apply Regulatory and Compliance Issues (AP/CP). Evaluation Methods: Direct Observation, Portfolio, Simulation, Examination, Team Leader Performance Evaluation, Portfolio Review, Quality Management, and Peer Evaluation | ||||
| Knows that laboratories must be accredited | Knows accrediting agencies of the laboratory | Completes laboratory inspector training | Participates in an internal or external laboratory inspection | Participates in or leads internal or external laboratory inspections |
| Can define appropriate disclosure of PHI as defined by the HIPAA | Understands and applies policies and procedures in PHI as defined by HIPAA | Confirms IRB approval prior to biospecimen procurement | Assists colleagues as needed with policies and procedures of PHI as defined by HIPAA | Participates in institutional review process, as needed |
| SBP3: Lab Management: Resource Utilization (Personnel and Finance): Explains, Recognizes, Summarizes, and Is Able to Apply Resource Utilization (AP/CP). Evaluation Methods: Direct Observation, Portfolio, Simulation, 360 Evaluations, and Analysis of Resident Evaluations (Meeting, Employee Interview, and Difficult Conversations) | ||||
| Interprets an organizational chart and is aware of employment contracts and benefits | Knows the personnel and lines of reporting in the laboratory | Understands and describes the process of personnel management and employment laws (eg, interview questions, Family and Medical Leave Act, and termination policies) | Creates a basic job description and participates in employee interviews/performance evaluation (real or simulated experiences) | Manages personnel effectively |
| Describes a budget | Recognizes different budget types (ie, capital vs operating budget) | Understands key elements of hospital and laboratory budgets | Participates in a budget cycle exercise (draft, defend, and propose logical cuts and/or additions) | Develops and manages a laboratory budget |
| SBP4: Lab Management: Quality, Risk Management, and Laboratory Safety: Explains, Recognizes, Summarizes, and Is Able to Apply Quality Improvement, Risk Management, and Safety Issues (AP/CP). Evaluation Methods: Direct Observation, Portfolio, Simulation, Narrative, Examination, and 360 Evaluations | ||||
| Understands the concept of a laboratory quality management plan | Demonstrates a knowledge of proficiency testing and its consequences | Reviews and analyzes proficiency testing results | Manages laboratory quality assurance and safety | |
| Understands when and how to file an incident or safety report | Understands continuous improvement tools, such as Lean and Six Sigma | Participates in department and hospital-wide quality, risk management, and safety initiatives | Utilizes continuous improvement tools, such as Lean and Six Sigma | |
| SBP5: Lab Management: Test Utilization: Explains, Recognizes, Summarizes, and Is Able to Apply Test Utilization (AP/CP). Evaluation Methods: Direct Observation, Portfolio, 360 Analyses, and Simulation | ||||
| Is aware of the test menu and rationale for ordering | Able to understand appropriate ordering or inappropriate ordering and overutilization | Able to interpret charts and graphs that demonstrate utilization patterns | Able to create charts and graphs that demonstrate utilization patterns (simulated or real experiences) | Demonstrates a broad portfolio of analyses for utilization reviews in complex scenarios and team management to drive change in areas both within and outside the department |
| SBP6: Lab Management: Technology Assessment: Explains, Recognizes, Summarizes, and Is Able to Apply Technology Assessment (AP/CP). Evaluation Methods: Direct Observation, Portfolio, and Simulation | ||||
| Understands the value of new technology | Aware of cost–benefit analysis for new technology | Able to perform a cost–benefit analysis | Participates in new instrument and test selection, verification, implementation, and validation (including reference range analysis) and maintains a portfolio of participation in these experiences | Acts as primary assessor for new technology and is able to lead efforts to optimize test utilization and resource management |
| SBP7: Informatics: Explains, Discusses, Classifies, and Applies Clinical Informatics (AP/CP). Evaluation Methods: Direct Observation, 360 Evaluations, and Portfolio Data | ||||
| Demonstrates familiarity with basic technical concepts of hardware, operating systems, and software for general purpose applications | Understands lab-specific software, key technical concepts and subsystems on interfaces, workflow, barcode application, and automation systems (enterprise systems architecture) | Applies informatics skills as needed in project management (data management, computational statistics) | Participates in operational and strategy meetings, apprentices troubleshooting with information technology staff, applies informatics skills in laboratory management and integrative bioinformatics (able to aggregate multiple data sources and often multiple data analysis services) | Able to utilize medical informatics in the direction and operation of the laboratory |
| PBLI1: Recognition of Errors and Discrepancies: Displays Attitudes, Knowledge, and Practices That Permit Improvement of Patient Care From Study of Errors and Discrepancies (AP/CP). Evaluation Methods: Self-Assessment (Written and Verbal), Direct Observation, and Narrative | ||||
| Acknowledges and takes responsibility for errors when recognized | Recognizes limits of own knowledge | Reflects upon errors in a group setting (such as M&M type conference setting) | Demonstrates significant awareness of own blind spots | Provides immediate communication of error/discrepancies to clinicians |
| PBLI2: Scholarly Activity: Analyzes and Appraises Pertinent Literature, Applies Scientific Method to Identify and Interpret Evidence-Based Medicine, and Applies it Clinically (AP/CP). Evaluation Methods: Direct Observation and Evaluation of Presentations By Participants, Portfolio, and Examination | ||||
| Demonstrates working knowledge of basic statistical analysis | Develops knowledge of the basic principles of research (demographics, IRB, and human subjects), including how research is conducted, evaluated, explained to patients, and applied to patient care | Critically reads and incorporates the medical literature into presentations and lectures | Critically examines literature for study design and use in evidence-based clinical care | Proficient in critical evaluation of the literature and participates in life-long learning |
| PROF1: Licensing, Certification, Examinations, Credentialing: Demonstrates Attitudes and Practices That Ensure Timely Completion of Required Examinations and Licensure (AP/CP). Evaluation Methods: Documentation Provided | ||||
| Completes and passes step 2CK and 2CS of USMLE | Completes and passes step 3 of USMLE | Performs at expected level on objective examinations | Applies for full and unrestricted medical license | Board eligible/board certified and begins to participate in maintenance of certification (SAMs, etc) |
| PROF2: Professionalism: Demonstrates Honesty, Integrity, and Ethical Behavior (AP/CP). Evaluation Methods: Direct Observation and 360 Evaluations | ||||
| Behaves truthfully and understands the concepts of ethical behavior, occasionally requiring guidance, and seeks counsel when ethical questions arise | Is truthful, acknowledges personal near misses and errors, and puts the needs of patients first | Identifies, communicates, and corrects errors | Serves as a role model for members of the health-care team in accepting personal responsibility | Models truthfulness to all members of the health-care team, is viewed as a role model in accepting personal responsibility by members of the health-care team, and always puts the needs of each patient above his or her own interests |
| PROF3: Professionalism: Demonstrates Responsibility and Follow-Through on Tasks (AP/CP). Evaluation Methods: Direct Observation, 360 Evaluations, and Portfolio Data (eg, autopsy TAT) | ||||
| Completes assigned tasks on time | Assists team members when requested | Anticipates team needs and assists as needed | Anticipates team needs and takes leadership role to independently implement solutions | Is a source of support/guidance to other members of health-care team |
| PROF4: Professionalism: Gives and Receives Feedback (AP/CP). Evaluation Methods: Direct Observation, 360 Evaluations, Role-Play or Simulation, and Resident Experience Narrative | ||||
| Receives feedback constructively | Accepts feedback constructively and modifies practice in response to feedback | Able to provide constructive feedback | Exemplifies giving and receiving constructive feedback | Encourages and actively seeks feedback to improve performance |
| PROF5: Professionalism: Demonstrates Responsiveness to Each Patient’s Unique Characteristics and Needs (AP/CP). Evaluation Methods: Direct observation, 360 Evaluations, Role-Play or Simulation, and Resident Experience Narrative | ||||
| Respects diversity, vulnerable populations, and patient autonomy | Is aware of potential for bias or cultural differences to affect clinical care | Demonstrates cultural competency | Identifies and avoids biases and recognizes cultural differences that may affect clinical care | Works with peers to avoid biases |
| PROF6: Professionalism: Demonstrates Personal Responsibility to Maintain Emotional, Physical, and Mental Health (AP/CP). Evaluation Methods: Direct Observation, 360 Evaluations, Role-Play or Simulation, and Resident Experience Narrative | ||||
| Exhibits basic professional responsibilities, such as timely reporting for duty rested, readiness to work, and being appropriately dressed | Manages emotional, physical, and mental health and issues related to fatigue/sleep deprivation | Manages emotional, physical, and mental health and issues related to fatigue/sleep deprivation, especially in stressful conditions | Recognizes signs of impairment in self and others and facilitates seeking appropriate help when needed | Accesses institutional resources to address impairment and initiates seeking appropriate help when needed |
| ICS1: Intradepartmental Interactions and Development of Leadership Skills: Displays Attitudes, Knowledge, and Practices that Promote Safe Patient Care Through Team Interactions and Leadership Skills Within the Laboratory (AP/CP). Evaluation Methods: Direct Observation, 360 Evaluations, and Narrative | ||||
| Demonstrates respect for and willingness to learn from all members of the pathology team | Works effectively with all members of the pathology team | Understands own role on the pathology team and flexibly contributes to team success through a willingness to assume appropriate roles as needed | Helps to organize the pathology team to facilitate optimal communication and coeducation among members | Leads the pathology team effectively |
| Is aware of the significance of conflict in patient care | Aware of the mechanisms for conflict resolution | Utilizes mechanisms for conflict resolution and helps to defuse and ameliorate conflict | Participates effectively in conflict resolution | Models effective conflict prevention and resolution skills |
| ICS2: Interdepartmental and Health-Care Clinical Team Interactions: Displays Attitudes, Knowledge, and Practices That Promote Safe Patient Care Through Interdisciplinary Team and Leadership Skills Within the Laboratory (AP/CP). Evaluation Methods: Direct Observation, 360 Evaluations, and Narrative | ||||
| Recognizes the importance of clinical input in formulating a differential diagnosis and composing a final diagnosis | Participates through observation and active interaction with clinicians to obtain relevant clinical and/or radiologic data | Assesses, analyzes, and interprets pathology reports and is able to discuss findings in consultation with clinical colleagues | Knows how subtleties may impact or alter patient care and recognizes and uses nuances in the proper wording in the discussion of pathology findings | Fully participates as a member of the health-care team and is recognized as proficient by peers and clinical colleagues |
| Is aware that multidisciplinary conferences are used to further appropriate patient care | Attends multidisciplinary conferences | Prepares and presents cases at multidisciplinary conferences | Can lead multidisciplinary conferences | Organizes and is responsible for multidisciplinary conferences |
| Understands utility of communication with other members of the clinical team | Appropriately triages requests for information from the clinical team | Effectively communicates clinically significant or unexpected values, including critical values | Participates in or leads communication with the clinical team to contribute to patient care | Serves as a consultant to the health-care team |
Abbreviations: ABP, American Board of Pathology; ACGME, Accreditation Council for Graduate Medical Education; AP, anatomic pathology; CME, continuing medical education; CP, clinical pathology; HIPAA, Health Insurance Portability and Accountability Act; IOC/FS, intraoperative consultation/frozen section; IRB, institutional review board; PHI, protected health information; PRISE, Pathologist Recertification Individualized Self-Assessment Exam; RISE, Resident In-Service Examination; SAMs, self-assessment modules; USMLE, United States Medical Licensing Examination; FNA, fine needle aspiration; ICS, interpersonal and communication skills; MK, medical knowledge; PBL, practice-based learning and improvement; PC, patient care; PROF, professionalism; SBP, systems-based practice; QA, quality assurance; M&M, morbidity and mortality; 2CK and 2 CS, United States Medical Licensing Examination (USMLE) step 2 clinical knowledge and step 2 clinical skills; TAT, turn-around-time.
*“The Milestones are designed only for use in evaluation of resident physicians in the context of their participation in ACGME-accredited residency or fellowship programs. The Milestones provide a framework for the assessment of the development of the resident physician in key dimensions of the elements of physician competency in a specialty or subspecialty. They neither represent the entirety of the dimensions of the six domains of physician competency nor are they designed to be relevant in any other context” (ACGME and ABP, July, 2015).
Influence of Accreditation and Certification on Training Program Structure
The Accreditation Council for Graduate Medical Education (ACGME) defines structural, resource, and personnel requirements for residency training and review programs to assess compliance. Successful review results in accreditation of a residency program. The ABP provides institutions moderate flexibility in the way they design their curriculum. The ABP certifies pathologists via a board examination and measures continued competency through a periodic maintenance of certification program. The ABP’s mandate is tightly defined by the American Board of Medical Specialties; it is ultimately answerable to the public and, if it were to lose the public trust, to government regulators. Hence, the ACGME and ABP exist in distinct spaces, largely limiting them to examining uncontestable evidence for accreditation and certification, respectively. In summary, program accreditation focuses on structure, resources, and personnel, whereas the certifying exams test what trainees can do objectively, with subjective and qualitative aspects of performance left to the programs to assess and certify.
It is promising that the ABP has expressed interest in novel ways to more fully assess trainees. Examples could include a portfolio of case narratives/work-ups that a resident has carried out individually or as a team member, a simulation examination such as the United States Medical Licensing Examination Clinical Skills Assessment, or oral exercises conducted during residency as surgical trainees now do. A combination of achievement metrics and a skills portfolio could assess trainees more comprehensively than the present nearly exclusive focus on high-risk multiple-choice examinations. The ACGME in conjunction with the ABP has also implemented training milestones in pathology. The milestone framework lends itself well to smoothly incorporating the assessment of additional skills as training programs evolve, such as interpersonal and communication abilities, and their benchmarking against national indicators of achievement.20 Aggregation of milestone assessments at the program level can also be used inter alia to inform accreditation assessment of the programs themselves. Collectively, the continued development of effective milestones and competency-based metrics as exemplified above will be critical to the success of the 21st century training in pathology.
The Way Forward—Crafting a Better Pathology Graduate Medical Education Program
Current training programs have evolved to reflect the needs of their era. As we enter a new era, we face new challenges and need programs that meet seemingly conflicting goals: train better, train more broadly, and train more efficiently. Several authors have previously addressed one or the other of these challenges, offering thoughtful appraisals of the problem.21-27 Often, these suggestions reflect the perspective of the author’s own orientation, be it academic specialty practice versus community generalist practice, AP versus CP. Suggestions include earlier and more focused specialization,28-30 better clinical knowledge and communication skills,30,31 a common educational core with transition to advanced modules as a means to competency,32 and a comprehensive training program in CP only.21
Realistic improvement in pathology graduate medical education (GME) programs must address all 3 of the goals above. The program must effectively support the career aspirations of those seeking specialty practice careers that demand focused expertise, as well as those aiming for community practice settings where broader practice skills are required. It must also make room for emerging disciplines and new practice paradigms, such as pathology informatics, genomic medicine, population health, and team practice, without sacrificing the deep expertise and experience needed to practice competently in particular areas of pathology. A plan is proposed below to achieve these aims efficiently, drawing on improved pedagogy, a more flexible and balanced curriculum, earlier engagement of trainees during their terminal year in medical school, competency-based metrics, and elective tracks providing graduated responsibility appropriate to each candidate’s career goals.
Early Engagement of Medical Students
The journey from first-year medical student to competent practitioner requires acquisition of many skills and much knowledge.33-35 Increasingly, medical school training must include much of what is also needed by the modern pathologist: medical and scientific knowledge,36 critical “Bayesian” thinking (statistics, informatics, handling “big data”),37-39 understanding cognitive bias,40-43 knowledge of health-care systems and patient behavior,44 empathy45-47 and wellness,48 and group dynamics.6,49-51 Reinforcing medical school training and relating it to the context of how pathology is practiced at the very onset of GME training would offer many advantages. Pathology GME should ideally begin in the terminal year of medical school. This would be a time not only to inculcate basic practice skills required for all medical practice but also to begin the onboarding process52 and contextualize the skills most pertinent to pathology. A possible way this could be accomplished would be through a national online tutorial. All trainees accepted to accredited programs would be expected to complete this tutorial before matriculating. One example is the online site being used by Montefiore for medical students entering pathology training (Figure 7).53 Effort invested in an effective onboarding process is returned manifold in trainees’ greater success and productivity throughout the program.
Figure 7.
Combined student tutorial and pathology-specific onboarding program. The figure is the home page for the Montefiore Einstein onboarding program for its pathology residency. The incoming residents are given access to the program approximately 6 weeks before beginning the residency program as a self-study to prepare for residency and as information about the program, institution, and city. The self-study includes a review of normal histology and case-based teaching of basic principles in diagnostic medicine.53 Reprinted from Academic Pathology with permission.
Advanced Credit Pathway
In addition to a tutorial for entering trainees, it would be advantageous to develop an advanced pathology practice pathway (APP) in medical school where the post-match portion of the last year of medical school or the entire last year could serve as segue to the first year of pathology residency training (Figure 6), similar to the program for family medicine54,55 and the pilot program for pediatrics.56,57 This could shorten the time to competency and/or allow trainees to master additional practice skills. The GME credit for such an APP would no doubt require ABP approval and need to be under the purview of a residency program director. However, it should be noted that advanced GME credit to medical students is not a new idea; prior to 2002, when the credentialing year requirement was dropped, advanced credit was routinely offered to medical students who had completed a postsophomore fellowship in pathology.
Finally, a process for recognizing advanced pathology practice skills acquired abroad should also be considered. Many foreign medical graduates matriculating to pathology GME programs have already completed extensive training in pathology abroad. Some have even practiced pathology for years. It would be advantageous if these skills could be recognized, perhaps not necessarily by shortening the training period but by allowing trainees with demonstrated competence to advance their training in new areas, rather than repeat what they already know. As the ABP moves to develop greater reliance on competency-based metrics, the opportunity more constructively to engage such trainees should not be overlooked.
Onboarding
As noted above, the onboarding process should naturally follow the engagement of the entering trainee while he or she is in the final semester of medical school (Figure 7). The goals of an effective onboarding process go beyond simple formalities and avoidance of problems; rather, onboarding should be the first step in preparing a trainee to achieve excellence. These attributes of an effective onboarding have been extensively discussed.53
The onboarding process should focus on universal (AP/CP) themes that a resident should know on day 1, with teaching that uses a case-based approach. Team-building skills are introduced and practiced. The importance of critical or Bayesian thinking related to preanalytic, analytic, and postanalytic variables is emphasized. There is group discussion of the ethical and legal issues surrounding autopsy, patient consent and patient rights, responsibilities under Health Insurance Portability and Accountability Act, the pathologist as a health-care team member, the ethics and procedures of research tissue use, and so on. The fundamental elements of the diagnostic process could also begin in an onboarding program, including a refresher in histology and case-based teaching to introduce methods (statistics and data analytics) for evaluating test utilization and quality management for evaluating test results.
A Uniform “Core” Curriculum Providing Basic Training Across the Anatomic Pathology/Clinical Pathology Continuum
Following onboarding, the trainee moves to a core curriculum (Figure 8). The first month or 2 of the residency core curriculum (boot camp58) focuses on basic skills and foundational knowledge; the resident will be able to apply to future learning throughout residency training. Residents work in teams in boot camp, and the schedule is designed to provide a careful balance between lecture, hands-on skills, and presentation skills. The design is to optimize learning of basic pathology knowledge, the acquisition of pathology skills, and the ability to communicate with clinical colleagues, all of which are required for team practice. Formal training and exercises in team dynamics should also be part of the core. The next 10 four-week modules of the first year focus on expanding basic knowledge and skills in both AP and CP. Included are the major clinical laboratories (chemistry, hematology, microbiology, and transfusion medicine) and anatomic services (autopsy, surgical, and cytopathology). There is no distinction between AP and CP trainees; this is a core required of all entering pathologists. The rationale is that regardless of the sphere of practice, fundamental principles of critical thinking, data analytics, and the integration of diverse data modalities are critical to all modern pathologists.
Figure 8.
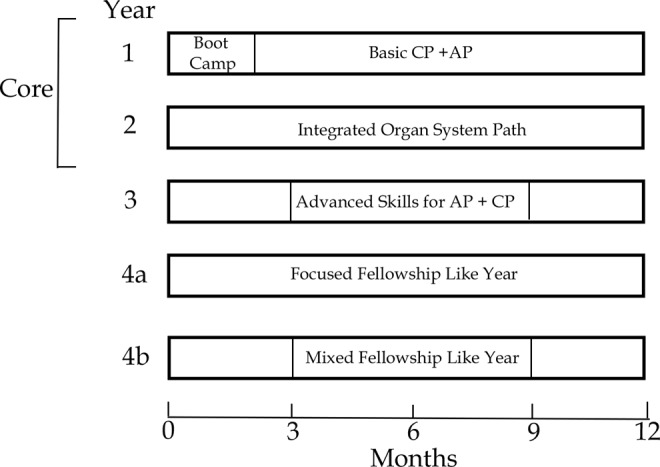
Flexible curriculum. Boot camp (2 months) serves as a continuation of the onboarding process to provide the new resident with fundamental knowledge and skills they will continue to develop during their training. This is a process-driven training that will enable the resident to develop a systematic approach to making and communicating a diagnosis. Residents will learn grossing and histopathologic techniques, quality control and quality assurance, concepts in test utilization, presentation skills, and methods for analyzing longitudinal data. The first year resident will work in a team with senior residents and faculty as mentors. The remaining core training in the first year will focus on fundamental knowledge and skills in the major clinical laboratories (chemistry, hematology, microbiology, and transfusion medicine) and anatomic services (autopsy, surgical, and cytopathology). The second year will begin to integrate AP/CP training by focusing on organ systems; although training in hematopathology naturally enables integration, other systems will require effort. The third year will continue to emphasize disease-based diagnoses with large 3-month blocks advancing skills in particular areas of anatomic and clinical pathology. The fourth year will serve as a focused fellowship like year in a single discipline or can be divided into mini fellowship like rotations to suit the resident’s career trajectory. Both the third and fourth years will escalate independent practice experience. AP indicates anatomic pathology; CP, clinical pathology.
Contrary to recent trends, autopsy training should have a prominent place in the core curriculum. Autopsy segues from the clinical mode of practice in which the new resident has most recently been immersed into the diagnostic process. It requires the resident to integrate the clinical history with developing skills in gross examination, tissue handling, and histopathology. The autopsy experience allows the trainees a rare opportunity to synthesize and issue a timely and meaningful report that integrates clinical history, imaging, laboratory and anatomic findings, and a quality of care assessment. The autopsy experience should also engage the resident with numerous hospital and health-care workers, introducing them as a key professional and consultant to the health-care team. Timely completion of an autopsy requires the full diagnostic process, including organizational and communication skills to report the findings both in writing and in a conference setting. Competency in all these elements of a postmortem examination should emerge as the metric used for certification, rather than the number of autopsies completed by the trainee.
The autopsy is also one of the few circumstances in which the pathology resident functions in a way similar to residents in other specialties tasked with patient care. Residents in other specialties are typically presented with a clinical problem to assess but always in context of the patient before them. Conversely, pathology residents are most often merely presented with a specimen, relying on the requesting physician to (occasionally) provide the clinical context. Yet, as part of a health-care team, pathologists must not be isolated if they are to contribute as true consultants to both test selection and diagnosis (and thereby to treatment).
The remaining months of core program should be diagnosis focused. For example, diagnostic skills in hematopathology require both morphologic and laboratory data interpretive skills. Learning which tests are required to make a diagnosis, interpreting test results, and synthesizing a diagnosis from the cumulative data reinforce a pathophysiology-based diagnostic process. This method of training, together with exposure to quality management59 projects, longitudinal data analysis, and presentations at clinical conferences, provides residents a strong diagnostic base on which to develop advanced diagnostic skills in subsequent years of training.60 For pathology services that do not require integration of morphologic diagnosis with laboratory findings, such as transfusion medicine, the resident should be actively engaged in health-care teams as part of the learning experience. Thus, we expect the resident to acquire basic knowledge of pathology diagnostics in the context of team-based practice during the 22 four-week months of core learning experience. This new paradigm would require programs to allocate time credit for integrated diagnostic training to either AP or CP training for purposes of board eligibility as is done now for hematopathology or require the ABP to acknowledge the eligibility of integrated diagnostic training per se.
An effective core will produce an adaptable, resilient61 pathologist with well-developed fundamental diagnostic skills in broad areas of pathology. This will lay the groundwork for the acquisition of advanced diagnostic skills during the remainder of the residency, reducing the need for multiple fellowships. However, new metrics will be needed to assess the effectiveness of the core training program; if such programs become prevalent, the ABP may wish to adapt their requirements for certification as described above.
Advanced Training Tailored to the Trainee’s Career Goals
Following the core, trainees will embark on advanced training that addresses their career goals and remaining ABP requirements. During this period, trainees will work increasingly independent and be expected to achieve a significant level of competence in major areas of surgical and CP. Required rotations will be interspersed with electives. The time available for electives and advanced training will be augmented by time liberated by advanced placement credit earned during the onboarding and core curriculum. Electives in genomic pathology, informatics, research, public health, medical economics, and team dynamics, and other emerging areas of importance to the future practice of pathology may be used to augment the advanced training experience.
Transition to Practice
The final year of the training program should prepare the trainee for practice. This requires that trainees be fully accountable for their diagnoses and their participation in the health-care team. Along the way, steps preparing the trainee for this point will have been in place, such as “hot-seat” rotations and presentations at tumor boards. However, until the trainee gains confidence in their fund of knowledge and knows that their medical decisions will actually impact patient care, they are not ready to practice. To achieve this transition, the training program must be ready to allow the trainee to make increasingly independent clinical decisions, providing backup but not usurping their front-line responsibility (“oversight” in the ACGME taxonomy of supervision). Currently, many programs do this with fellows by credentialing them for clinical practice; however, there is no reason that suitably qualified senior trainees could not also be licensed as physicians and so credentialed. Ideally, this practice could be incorporated as a routine part of a forward-looking training program.
Summary: A Pathology Graduate Medical Education Program for the 21st Century
If pathologists are to have an impact on improving health care (both for individual patients and for populations) and in reducing diagnostic errors, we must ensure that our residency programs produce skilled diagnosticians with solid interpersonal and communication skills that enable them to be effective members of health-care teams.62 There must be a core training that provides foundational pathology skills and knowledge (AP and CP) and teaches critical thinking/clinical reasoning,63,64 quality management, and communication skills, all in the context of a team environment of care. The model program we envision is the one that accomplishes these goals while allowing flexibility to accommodate differing career aspirations and does it all in a maximum of 4 years. A fifth year would be reserved for advanced training and development as a subspecialist practitioner. Five structural elements underlie this model: (1) an advanced credit pathway, with engagement of trainees while in medical school; (2) an “onboarding” process at the onset of training; (3) a boot camp transitioning to a core curriculum that provides basic training across the AP/CP continuum; (4) advanced training modules tailored to the trainee’s career goals; and (5) a period of intensive and progressive responsibility leading to independent practice experience. Each of these elements is of independent utility. Combined, they have the potential to radically advance the present pathology GME training paradigm. Such a program would restore a rational approach to our existing training that has evolved in a chaotic way over the last decade through de facto obligate incorporation of subspecialty fellowships into general training, driven by the unintended consequences of changes in certification requirements superimposed on fluctuations in the employment market. A broad outline of this training model is summarized in Figure 9. One can envision a modern training program with a core lasting 24 months intended to give an individual a strong grounding in these elements of pathology, the basics of which can then be used over an additional 24 months of training to develop greater expertise in particular areas of pathology while experiencing progressively increasing responsibility. At a minimum, by the fourth year, a trainee should be practicing as a fellow does today and possibly as an attending in their first month of practice. Thus, in the current 4-year time frame, residents will attain a higher level of competency if some or all of the elements of our model are implemented. This will also reduce the total training time, even for those residents desiring a 1-year fellowship for subspecialty practice.
Figure 9.
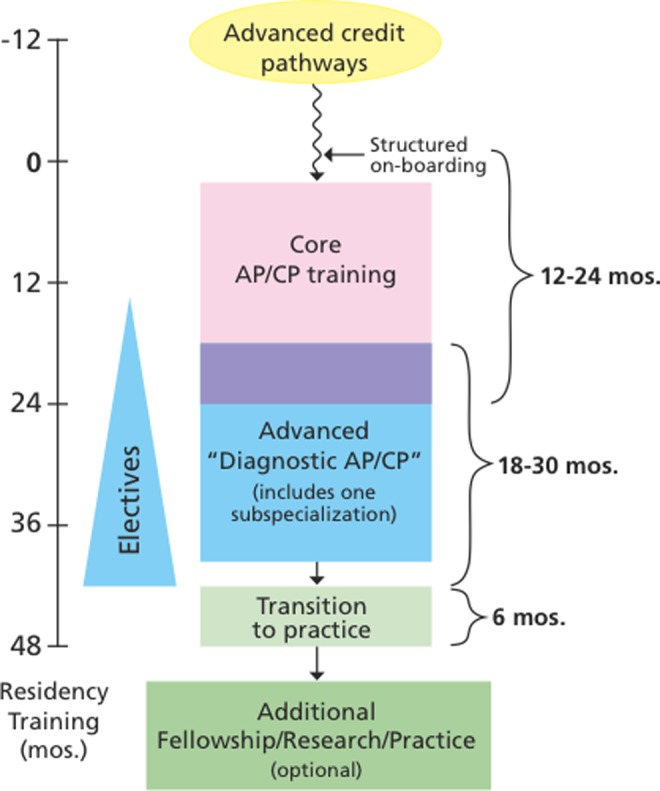
Outlines of a model pathology residency. This composite figure reflects the elements of our current proposal including advanced credit, core training, advanced training, transition to practice within the residency, and additional fellowship training. Implementation of some or all of the elements should improve our current training programs, reducing the time to competency for practicing pathology.
Footnotes
Authors’ Note: All authors contributed equally to this study and are listed in alphabetical order.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Sussman I, Prystowsky MB. Pathology service line: a model for accountable care organizations at an academic medical center. Hum Pathol. 2012;43:629–631. [DOI] [PubMed] [Google Scholar]
- 2. Sutton M, Nikolova S, Boaden R, Lester H, McDonald R, Roland M. Reduced mortality with hospital pay for performance in England. New Engl J Med. 2012;367:1821–1828. [DOI] [PubMed] [Google Scholar]
- 3. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27:759–769. [DOI] [PubMed] [Google Scholar]
- 4. Berwick DM. Making good on ACOs’ promise—the final rule for the Medicare shared savings program. New Engl J Med. 2011;365:1753–1756. [DOI] [PubMed] [Google Scholar]
- 5. Bellin E. Riddles in Accountable Healthcare: A Primer to Develop Analytic Intuition for Medical Homes and Population Health. North Charleston, SC: CreateSpace Independent Publishing Platform; 2015. [Google Scholar]
- 6. Schein EH. Humble Inquiry: The Gentle Art of Asking Instead of Telling. Oakland, CA: Berrett-Koehler Publishers; 2013. [Google Scholar]
- 7. Tang PC, Lansky D. The missing link: bridging the patient–provider health information gap. Health Aff. 2005;24:1290–1295. [DOI] [PubMed] [Google Scholar]
- 8. Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Vol 6: Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 9. Leape LL, Berwick DM. Five years after to err is human: what have we learned? JAMA. 2005;293:2384–2390. [DOI] [PubMed] [Google Scholar]
- 10. Balogh EP, Miller BT, Ball JR. Improving Diagnosis in Health Care. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 11. Institute of Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 12. Black-Schaffer WS, Crawford JM. The evolving landscape for pathology subspecialty fellowship applications. Am J Clin Pathol. 2012;137:513–515. [DOI] [PubMed] [Google Scholar]
- 13. Domen RE, Talbert ML, Johnson K, et al. Assessment and management of professionalism issues in pathology residency training results from surveys and a workshop by the graduate medical education committee of the college of american pathologists. Acad Pathol. 2015;2:1–9. doi:10.1177/2374289515592887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rinder H, Frank K, Wagner J. ASCP fellowship & job market surveys. A report on the 2013 RISE, FISE, FISHE, NPISE, PISE, and TMISE surveys 2015.
- 15. Rinder HM. ASCP fellowship & job market survey. Am Soc Clin Pathol. 2012. pp. 1–40. [Google Scholar]
- 16. Robboy SJ, Gupta S, Crawford JM, et al. The pathologist workforce in the united states: ii. An interactive modeling tool for analyzing future qualitative and quantitative staffing demands for services. Arch Pathol Lab Med. 2015;139:1413–1430. [DOI] [PubMed] [Google Scholar]
- 17. Robboy SJ, Weintraub S, Horvath AE, et al. Pathologist workforce in the United States: I. Development of a predictive model to examine factors influencing supply. Arch Pathol Lab Med. 2013;137:1723–1732. [DOI] [PubMed] [Google Scholar]
- 18. Mitchell RJ, Parker V, Giles M. When do interprofessional teams succeed? Investigating the moderating roles of team and professional identity in interprofessional effectiveness. Hum Relat. 2011;64:1321–1343. [Google Scholar]
- 19. Steinberg JJ, Prystowsky MB. Team-based health care in pathology training programs. Arch Pathol Lab Med. 2014;138:724. [DOI] [PubMed] [Google Scholar]
- 20. Nasca TJ, Weiss KB, Bagian JP. Improving clinical learning environments for tomorrow’s physicians. New Engl J Med. 2014;370:991–993. [DOI] [PubMed] [Google Scholar]
- 21. Smith BR, Wells A, Alexander CB, et al. Curriculum content and evaluation of resident competency in clinical pathology (laboratory medicine): a proposal. Hum Pathol. 2006;37:934–968. [DOI] [PubMed] [Google Scholar]
- 22. Association of Directors of Anatomic and Surgical Pathology. Curriculum content and evaluation of resident competency in anatomic pathology: a proposal. Hum Pathol. 2003;34:1083–1090. [DOI] [PubMed] [Google Scholar]
- 23. Weiss RL, McKenna BJ, Lord-Toof M, Thompson NN. A consensus curriculum for laboratory management training for pathology residents. Am J Clin Pathol. 2011;136:671–678. [DOI] [PubMed] [Google Scholar]
- 24. Wells A, Smith B. Counterpoint: developing a clinical pathology curriculum to meet current and future needs. Clin Chem. 2006;52:971–972. [DOI] [PubMed] [Google Scholar]
- 25. Folberg R, Antonioli DA, Alexander CB. Competency-based residency training in pathology: challenges and opportunities. Hum Pathol. 2002;33:3–6. [DOI] [PubMed] [Google Scholar]
- 26. Kass ME, Crawford JM, Bennett B, et al. Adequacy of pathology resident training for employment: a survey report from the future of pathology task group. Arch Pathol Lab Med. 2007;131:545–555. [DOI] [PubMed] [Google Scholar]
- 27. Alexander CB. Pathology graduate medical education (overview from 1926 to 2005). Hum Pathol. 2006;37:923–928. [DOI] [PubMed] [Google Scholar]
- 28. Domen RE, Baccon J. Pathology Residency training: time for a new paradigm. Hum Pathol. 2014;45:1125–1129. [DOI] [PubMed] [Google Scholar]
- 29. Otis CN. Residency training in anatomic pathology: looking forward in the 21st century. Hum Pathol. 2006;37:929–931. [DOI] [PubMed] [Google Scholar]
- 30. Talbert ML, Ashwood ER, Brownlee NA, et al. Resident preparation for practice: a white paper from the College of American Pathologists and Association of Pathology Chairs. Arch Pathol Lab Med. 2009;133:1139–1147. [DOI] [PubMed] [Google Scholar]
- 31. Horowitz RE. The successful community hospital pathologist—what it takes. Hum Pathol. 1998;29:211–214. [DOI] [PubMed] [Google Scholar]
- 32. Naritoku WY, Alexander CB, Bennett BD, et al. The pathology milestones and the next accreditation system. Arch Pathol Lab Med. 2014;138:307–315. [DOI] [PubMed] [Google Scholar]
- 33. Batalden P, Leach D, Swing S, Dreyfus H, Dreyfus S. General competencies and accreditation in graduate medical education. Health Aff. 2002;21:103–111. [DOI] [PubMed] [Google Scholar]
- 34. Carraccio CL, Benson BJ, Nixon LJ, Derstine PL. From the educational bench to the clinical bedside: translating the dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83:761–767. [DOI] [PubMed] [Google Scholar]
- 35. Leach DC. Competence is a habit. JAMA. 2002;287:243–244. [DOI] [PubMed] [Google Scholar]
- 36. Nagy W, Townsend D. Words as tools: learning academic vocabulary as language acquisition. Read Res Q. 2012;47:91–108. [Google Scholar]
- 37. Ashby D. Bayesian statistics in medicine: a 25 year review. Stat Med. 2006;25:3589–3631. [DOI] [PubMed] [Google Scholar]
- 38. Spiegelhalter D, Myles JP, Jones DR, Abrams KR. An introduction to Bayesian methods in health technology assessment. Br Med J. 1999;319(7208):508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ashby D, Smith AF. Evidence-based medicine as Bayesian decision-making. Stat Med. 2000;19:3291–3305. [DOI] [PubMed] [Google Scholar]
- 40. Croskerry P. From mindless to mindful practice—cognitive bias and clinical decision making. N Engl J Med. 2013;368:2445–2448. [DOI] [PubMed] [Google Scholar]
- 41. Croskerry P. When I say… cognitive debiasing. Med Educ. 2015;49:656–657. [DOI] [PubMed] [Google Scholar]
- 42. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf. 2013;22(suppl 2):ii58–ii64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: impediments to and strategies for change. BMJ Qual Saf. 2013;22(suppl 2):ii65–ii72. doi:10.1136/bmjqs-2012-001713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jacobsen PB, Holland JC, Steensma DP. Caring for the whole patient: the science of psychosocial care. J Clin Oncol. 2012;30:1151–1153. [DOI] [PubMed] [Google Scholar]
- 45. Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatr;159(9):1563–9; 2002. [DOI] [PubMed] [Google Scholar]
- 46. Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38:934–941. [DOI] [PubMed] [Google Scholar]
- 47. Hojat M, Vergare MJ, Maxwell K. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–1191. [DOI] [PubMed] [Google Scholar]
- 48. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. The Lancet. 2009;374(9702):1714–1721. [DOI] [PubMed] [Google Scholar]
- 49. Schein EH. Organizational Culture and Leadership. Vol 2 Hoboken, NJ: John Wiley & Sons; 2010. [Google Scholar]
- 50. Schein EH. Organizational Psychology. Englewood Cliffs, NJ: Prentice-Hall; 1970. [Google Scholar]
- 51. Nelson EC, Batalden PB, Godfrey MM. Quality by Design: A Clinical Microsystems Approach. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 52. Hébert TM, Maleki S, Vasovic LV, Arnold JL, Steinberg JJ, Prystowsky MB. A team-based approach to autopsy education: integrating anatomic and clinical pathology at the rotation level. Arch Pathol Lab Med. 2014;138:322–327. [DOI] [PubMed] [Google Scholar]
- 53. Hébert TM, Szymanski J, Mantilla J, et al. Onboarding for pathology residency programs—The Montefiore Experience. Acad Pathol. 2016;3:1–4. doi:10.1177/2374289516639979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. McDermott J. Harnessing our opportunity to make primary care sustainable. New Engl J Med. 2011;364:395–397. [DOI] [PubMed] [Google Scholar]
- 55. Jones BG, Berk SL. The family medicine accelerated track model: producing more family doctors faster. Virtual Mentor. 2012;14:845–853. [DOI] [PubMed] [Google Scholar]
- 56. Roberts KB. Pediatric education across the continuum: what continuum? Acad Pediatr. 2014;14:325–329. [DOI] [PubMed] [Google Scholar]
- 57. Powell D, Carraccio C, Aschenbrener C, Englander R. Education in Pediatrics Across the Continuum (The EPAC Project) AAMC “White Paper” Committee Report. Web site https://www.aamc.org/download/347738/data/epaccharter.pdf.
- 58. Naritoku WY, Vasovic L, Steinberg JJ, Prystowsky MB, Powell SZ. Anatomic and clinical pathology boot camps: filling pathology-specific gaps in undergraduate medical education. Arch Pathol Lab Med. 2014;138:316. [DOI] [PubMed] [Google Scholar]
- 59. Rishi A, Hoda ST, Crawford JM. A required rotation in clinical laboratory management for pathology residents five-year experience at Hofstra Northwell School of Medicine. Acad Pathol. 2016;3:1–13. doi:10.1177/2374289516644621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tufte ER, Graves-Morris P. The Visual Display of Quantitative Information. Vol 2 Cheshire, CT: Graphics press; 1983. [Google Scholar]
- 61. Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88:301–303. [DOI] [PubMed] [Google Scholar]
- 62. Burt RS. Brokerage and Closure: An Introduction to Social Capital. Oxford: OUP; 2005. [Google Scholar]
- 63. Tversky A, Kahneman D. Rational choice and the framing of decisions. J Bus. 1986;59:S251–S278. [Google Scholar]
- 64. Kahneman D. Thinking, Fast and Slow. New York, NY: Macmillan; 2011. [Google Scholar]