Abstract
Background: In recent years, there have been dramatic increases in medical imaging use and increasing media attention to increased exposure to ionizing radiation in the United States. Patient perspectives on medical imaging radiation (MIR) use is understudied, but could guide primary care discussions. This study examines prevalence of worry about the health harms from MIR in the US general population. Methods: This cross-sectional study used the 2012-2013 Health Information National Trends Survey conducted by the National Cancer Institute. A nationally representative sample (N = 3532) was drawn from the US general population to observe prevalence of worry about MIR as well as potential covariates, including demographic, medical, and psychological factors, health information-seeking, physician trust in providing cancer information, and cancer fatalism. Results: About 65% of the sample population reported experiencing at least some worry about MIR. Univariable and multivariable logistic regressions indicate higher rates of MIR worry among women, racial/ethnic minorities, those with lower educational attainment, foreign-born Americans, those who self-report poorer health, and those with a personal history of cancer. Lower trust in cancer information from physicians and greater attention to cancer information from popular media were each associated with higher rates of worry about health harms of MIR. Conclusions: An accurate assessment of public worry about MIR will aid primary care providers’ efforts to understand patient responses to medical imaging and identify addressable knowledge gaps regarding benefits and risks of medical imaging. These data may improve risk communication regarding medical imaging among referring primary care physicians, radiologists, and patients.
Keywords: medical imaging, radiation, worry, attitudes, general population
Introduction
Over the past few decades, the dramatic increase in the use of medical imaging tests that employ ionizing radiation in the United States has led to growing sensitization to patient safety, which has resulted in efforts to reduce radiation exposure during these tests, and consideration of alternatives to their use whenever possible.1 There is substantial uncertainty concerning the actual risks associated with medical imaging radiation (MIR).2-8 In this context, the mass media has devoted increasing coverage to patient safety in the context of tests that use MIR. For example, in January 2014, the Op-Ed section of The New York Times9 featured an essay written by a cardiologist and a radiologist that was headlined, “We are Giving Ourselves Cancer” and dramatically described perceived population harms of MIR.
While the media focus on MIR has been predominantly negative,10 it is not clear how this dialogue has affected the general population. Patients’ concerns about the health risks of MIR could increase patient anxiety and impede quality of life, and could impede imaging adherence, given that high cancer worries are related to general distress and can lead to avoidance of imaging, such as cancer screening.11 An accurate assessment of population worry about the harms of MIR will assist in efforts to anticipate and understand patients’ attitudes toward medical imaging, and improve risk communication and shared decision making regarding medical imaging among referring primary care physicians, radiologists as well as patients. Furthermore, understanding patient characteristics associated with high levels of worry about MIR will help referring physicians anticipate and address such concerns in specific patient subpopulations.
Accordingly, Aim I is to determine rates of worry about MIR in the US general population and to compare these with rates of worry about other common environmental hazards. Aim II is to determine significant correlates of MIR worry, including demographics, medical and psychological factors, health information-seeking and physician trust, as well as cancer fatalism—the belief that cancer is inevitable.
Methods
Study Design and Participants
The Health Information National Trends Survey12 (HINTS, 2013) version 4, cycle 2 is a nationally representative survey that was conducted by the National Cancer Institute (NCI) via mail between October 2012 and January 2013. Of 12 057 invitees, 3630 participants returned completed surveys. The total sample consisted of 3532 individuals for whom complete data on the outcome of interest (worry about MIR) was available.
Measures
Worry About MIR
The study dependent variable was a self-report item measuring the amount of worry about the health harms of MIR. Other items assessed worry regarding the health harms of chemicals in water, chemicals in food, outdoor air pollution, chemicals in household products, indoor air contaminants, chemicals in personal products, and radiation from cell phones.
Demographic Factors
Gender, age, race/ethnicity, educational attainment, annual income, whether the participant was born in the United States, subjective health status, health insurance status, as well as personal cancer history, and general anxiety13 were assessed.
Health Information-Seeking and Physician Trust
Participants were asked whether they sought health information, how much trust they would have in cancer information from a doctor, and finally, the level of attention paid to information about cancer from 7 different media sources (eg, print newspapers, the Internet, radio, and local television news; all 7 combined into a summary score, 0-100 range).
Cancer Fatalism
Consistent with prior work, 3 questions (eg, “There’s not much you can do to lower your chances of getting cancer”) were combined to create a continuous summary score (0-100) measure of cancer fatalism.14
The specific wording of all measures reported in this study appears at: http://hints.cancer.gov/docs/HINTS_4_Cycle_2_English.pdf.
Analytic Strategy
All analyses were conducted in R version 3.1.015 using the “survey” package,16,17 version 3.29-5 to account for the HINTS complex sampling design. The HINTS full-sample weight was applied to all analyses to yield nationally representative point estimates. Standard errors were calculated using jackknife repeated replications with the set of replicate weights included with the HINTS data.
First, covariates of interest were examined using descriptive statistics (unweighted frequencies, weighted percentages, means with 95% confidence intervals [CIs]). Next, logistic regression analysis was conducted and presented as unadjusted (univariable) and adjusted (multivariable) odds ratios with 95% CIs. For the logistic regression analysis, the dependent variable (MIR worry) was dichotomized (not at all/a little vs some/a lot) and elevated MIR worry was modeled. Omnibus F tests were calculated to assess the overall statistical significance of variables entered into the models. Three multivariable logistic regression models were fit to the data. The first model included only the associations between the demographic variables and MIR worry. The second model included health information-seeking and physician trust variables in addition to demographics. The third model added cancer fatalism to the demographic model.
Results
Characteristics of the Sample
Table 1 reports the descriptive characteristics of the analyzed HINTS sample. The sample was balanced in terms of gender, predominantly aged 18 to 64 years, 33% non-white, and highly diverse in educational attainment and income. Most were US born (86%), had health insurance (82%), and reported subjective health that was good or better than good (84%).
Table 1.
Descriptive Characteristics of the Sample (N = 3532).a
| Variables and Level Categories | n (%) |
|---|---|
| Gender | |
| Male | 1376 (48.9) |
| Female | 2144 (51.1) |
| Age, years | |
| 18-34 | 527 (30.9) |
| 35-49 | 838 (26.6) |
| 50-64 | 1144 (25.5) |
| 65-74 | 538 (9.4) |
| 75+ | 391 (7.6) |
| Race/Ethnicity | |
| White | 2156 (67.1) |
| Asian | 106 (4.8) |
| Black | 576 (12.0) |
| Hispanic | 486 (13.7) |
| Other | 121 (2.4) |
| Education | |
| Less than high school | 296 (13.0) |
| High school graduate | 751 (20.1) |
| Some college | 1047 (37.9) |
| College graduate | 838 (18.6) |
| Postgraduate degree | 531 (10.4) |
| Annual income, $ | |
| 0-9999 | 346 (10.5) |
| 10 000-14 999 | 239 (6.0) |
| 15 000-19 999 | 210 (5.2) |
| 20 000-34 999 | 535 (14.7) |
| 35 000-49 999 | 503 (15.6) |
| 50 000-74 999 | 565 (16.7) |
| 75 000-99 999 | 423 (12.7) |
| 100 000–199 999 | 476 (14.9) |
| ≥200 000 | 135 (3.8) |
| Born in the United States | |
| Yes | 3007 (85.6) |
| No | 482 (14.4) |
| General health self-assessment | |
| Poor | 116 (3.0) |
| Fair | 478 (12.9) |
| Good | 1253 (35.1) |
| Very good | 1212 (37.3) |
| Excellent | 377 (11.7) |
| Health insurance | |
| Yes | 2928 (82.3) |
| No | 566 (17.7) |
| Personal cancer history | |
| Yes | 452 (8.2) |
| No | 3062 (91.8) |
| Physician’s Health Questionnaire–4 Anxiety | |
| Higher anxiety ≥3 | 536 (15.6) |
| Lower anxiety <3 | 2863 (84.4) |
Unweighted frequencies (n) and weighted percentages are presented. Percentages reflect valid response set.
Aim I: Rates and Levels of Worry About MIR in the General Population
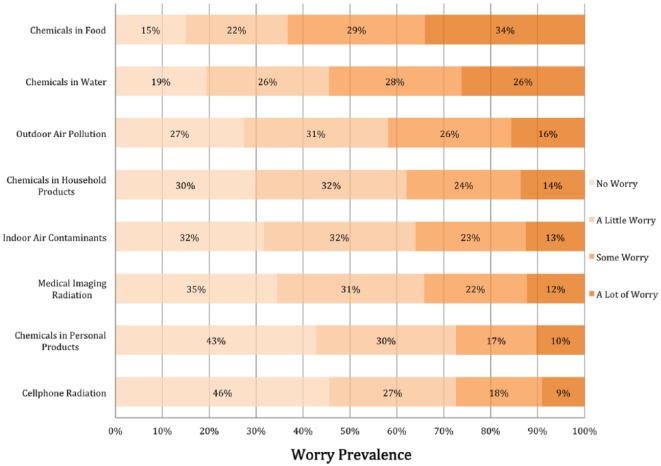
About two-thirds of the sample (65.5%, 95% CI = 62.9% to 68.1%) reported worry regarding the health effects of radiation from medical imaging. Specifically, 31.1% (95% CI = 28.6% to 34.0%) reported a little worry, 21.9% (95% CI = 19.1% to 24.7%) reported some worry, and 12.3% (95% CI = 10.6% to 14.0%) reported a lot of worry (see Figure 1). Rates of worry about the health effects for other hazards were higher than for MIR.
Figure 1.
Self-reported worry about harm to health from medical imaging radiation compared with other hazards (N = 3532). Participants’ estimates of worry for a series of hazards. Responses represent portion of sample who reported no worry or any other degree of worry (a little worry, some worry, or a lot of worry).
Aim II: Correlates of MIR Worry
Univariable and multivariable logistic regressions examining associations between elevated MIR worry and demographics, health information-seeking, and cancer fatalism variables are presented in Table 2. At the univariable level, higher worry about MIR was significantly associated with female gender, racial/ethnic minority status, having an annual income <$50 000, lower education, and being foreign born. Additionally, higher worry about MIR was significantly associated with poorer subjective health, having a personal history of cancer, and elevated general anxiety. Worry about MIR was not associated with age or health insurance status. In terms of health information-seeking, MIR worry was not associated with seeking health information in the past year but was significantly associated with being less trusting of cancer information communicated by doctors, and with paying more attention to cancer information from popular media. The univariable relation between MIR worry and cancer fatalism was not statistically significant.
Table 2.
Univariable and Multivariable Logistic Regressions Examining Correlates of Worrya About Harm From MIR (N = 3532).
| Variables and Level Categories | Unadjusted OR (95% CI) | Omnibus F P-Value | Adjusted OR (95% CI) | Omnibus F P-Value |
|---|---|---|---|---|
| Demographics b | ||||
| Gender | ||||
| Male | 1.00 Referent | .012* | 1.00 Referent | .017* |
| Female | 1.39 (1.08-1.78)* | 1.44 (1.08-1.92)* | ||
| Age | ||||
| [10 unit increase] | 1.06 (0.98-1.14) | .157 | 1.06 (0.96-1.17) | .282 |
| Race/Ethnicity | ||||
| White | 1.00 Referent | <.001*** | 1.00 Referent | .016* |
| Asian | 4.30 (2.05-9.01)*** | 2.86 (1.07-7.65)* | ||
| Black | 1.70 (1.29-2.26)*** | 1.49 (1.11-2.00)* | ||
| Hispanic | 2.39 (1.65-3.46)*** | 1.76 (1.13-2.73)* | ||
| Other | 1.97 (0.87-4.45) | 2.04 (0.86-4.89) | ||
| Education | ||||
| Less than high school | 3.20 (2.32-4.41)*** | <.001*** | 2.06 (1.33-3.20)** | .014* |
| High school graduate | 1.33 (0.94-1.88) | 1.18 (0.71-1.95) | ||
| Any college | 1.41 (1.11-1.80)** | 1.30 (0.96-1.77) | ||
| Postgraduate degree | 1.00 Referent | 1.00 Referent | ||
| Annual income, $ | ||||
| <50 000 | 1.84 (1.4-2.42)*** | <.001*** | 1.21 (0.86-1.69) | .280 |
| ≥50 000 | 1.00 Referent | 1.00 Referent | ||
| Born in the USA | ||||
| Yes | 1.00 Referent | <.001*** | 1.00 Referent | .020* |
| No | 2.98 (2.21-4.01)*** | 1.84 (1.13-3.01)* | ||
| General health self-assessment | ||||
| Poor-Fair | 2.62 (1.83-3.77)*** | <.001*** | 1.92 (1.30-2.84)** | .002** |
| Good-Excellent | 1.00 Referent | 1.00 Referent | ||
| Health insurance | ||||
| Yes | 1.00 Referent | .066† | 1.00 Referent | .563 |
| No | 1.40 (0.99-1.99)† | 1.11 (0.79-1.56) | ||
| Personal cancer history | ||||
| Yes | 1.48 (1.09-1.99)* | .014* | 1.53 (1.12-2.10)* | .011* |
| No | 1.00 Referent | 1.00 Referent | ||
| PHQ-4 Anxiety | ||||
| Higher anxiety ≥3 | 1.54 (1.14-2.10)** | .007** | 1.18 (0.84-1.67) | .341 |
| Lower anxiety <3 | 1.00 Referent | 1.00 Referent | ||
| Information-seeking behaviors c | ||||
| Ever sought health info | ||||
| Yes | 0.97 (0.69-1.36) | .857 | 1.12 (0.71-1.78) | .619 |
| No | 1.00 Referent | 1.00 Referent | ||
| Trusts in cancer info from doctor | ||||
| A lot | 1.00 Referent | .005** | 1.00 Referent | .008** |
| <A lot | 1.38 (1.11-1.71)** | 1.52 (1.14 - 2.04)** | ||
| Attention to cancer info | ||||
| [10 unit increase] | 1.17 (1.1-1.25)*** | <.001*** | 1.12 (1.04-1.20)** | .003** |
| Cancer fatalism d | ||||
| Cancer Fatalism | ||||
| [10 unit increase] | 0.98 (0.93-1.03) | .436 | 0.96 (0.90-1.03) | .285 |
Abbreviations: MIR, medical imaging radiation; OR, odds ratio; CI, confidence interval; PHQ, Physician’s Health Questionnaire.
Worry item was dichotomized as none/a little worry versus some/a lot of worry.
In the first multivariable model, the adjusted odds ratios for each demographic variable are adjusted for all of the other demographic variables.
In the second multivariable model, the adjusted odds ratios for each information-seeking behavior variable are adjusted for all of the demographic variables and for the other information-seeking behavior variables.
In the third multivariable model, the adjusted odds ratio for the cancer fatalism variable is adjusted for all of the demographic variables.
Near-significance at P < .10; *significance at P < .05; **significance at P < .01; ***significance at P < .001.
The multivariable analyses yielded similar findings with a few exceptions. The first model, demographics, indicated higher rates of MIR worry among females, racial/ethnic minorities, less educated individuals, foreign-born Americans, those who self-report poorer health, and those with a personal history of cancer. In the second model, information-seeking controlling for demographics, MIR worry was significantly associated with being less trusting of cancer information communicated by doctors and with paying more attention to cancer information from various forms of popular media. Cancer fatalism was still not statistically significant after controlling for demographics (third model).
Discussion
An accurate assessment of public concerns about the harms of MIR will aid referring physicians’ efforts to anticipate and understand patient responses to medical imaging. These data suggest that a large proportion of individuals (65%) in the United States have salient concerns about exposure to radiation from medical tests, a fact that mirrors an expanding dialogue about the delivery of radiation via medical imaging in the medical community and the news media.10,18-20 We found higher levels of MIR worry in this large, nationally representative US sample than in research on smaller samples, which found 12% in those about to undergo imaging in 2011,18 and 37% in a shopping mall in 2000, were concerned about MIR.19
Significant correlates of MIR worry indicate 4 population subgroups where MIR worry is most prevalent. These groups include the underserved, those with health challenges, those who are less trusting of cancer information from their physicians, and those more attentive to cancer topics in the media. First, worry about MIR was found to be higher in non-whites, those with lower educational attainment, and Americans who were born outside the United States. Health literacy is lower in underserved populations,21 and new health innovations are absorbed more slowly in underserved populations.22 Lower health literacy and poorer access to health innovations could dictate that underserved populations have less access to high-quality information about the benefits as well as the potential harms of medical imaging. Furthermore, lower income was associated with significantly higher MIR worry in the univariable model only, likely due to a high degree of overlap with lower education, which remained significantly linked to MIR worry in both analyses. The analysis also suggests that women endorse higher levels of worry than men.
A second important study finding is that higher MIR worry is associated with both a personal history of cancer and poorer self-reported health. Indeed, those who have serious health issues such as cancer20 may be imaged more frequently and be aware of potential risks associated with repeated imaging. As such, it is possible that 2 separate subgroups exist—where low socioeconomic status and low knowledge dictate higher MIR worry, and also where those with health concerns (and potentially higher knowledge) may also have higher MIR worry. Additionally, individuals who have been previously diagnosed with cancer may be more likely to worry about cancer in general. In a study examining cancer patient perspectives on MIR, patients felt the need for more information about the rationales for the recommendation of one test over another and for test intervals, and more explicit information about communication between the radiologist and the provider who ordered the test.20 Primary care patients with poorer health may also be more frequently imaged, and worry more about health, in general. General anxiety was not related to MIR worry in the multivariable analyses, indicating that specific concerns about MIR were distinct from general anxiety. However, worry about MIR would be expected to be high in those with anxious symptoms.
Finally, physician trust and cancer information-seeking patterns were also associated with MIR worry. Those with lower trust in cancer information provided by their doctors reported higher MIR worry. Additionally, participants who reported paying a lot of attention to a variety of common sources of cancer information reported higher levels of MIR worry, suggesting that individuals who are likely to worry about MIR are also likely to be receptive to mass media coverage of cancer issues.23 There are substantial opportunities for medical imaging experts such as radiologists and medical physics professionals to better communicate with the news media23-25 regarding the actual risks associated with MIR, as well as the social factors that may amplify or minimize perceived risks associated with MIR.23 Future research should examine whether improved primary care communication about these topics may both increase physician trust and reduce MIR worry.
Study limitations include the modest study response rate, as well as cross-sectional nature of the data, which does not allow for examination of cause and effect relationships between the covariates and worry about MIR. Additionally, our assessment of MIR worry was based on one item, and with this dataset we could not examine specific health concerns such as cancer worry, which is common in the population.11,26,27 Full consideration of myriad public concerns about medical imaging, including both shorter and longer term effects, and other environmental exposures is necessary to fully address their health and policy implications.28-30
Key points and study contributions are as follows. Worry about MIR is relatively high in the US population, and highest in the underserved, those with health challenges, those who are less trusting of cancer information from their physicians, and those more attentive to cancer topics in the media. This study contributes to the literature in that it documents prevalence and patterns of MIR in a large, nationally representative population. Public perspectives regarding the risks and benefits of imaging tests that deliver ionizing radiation can help shape the dialogue regarding shared decision making about recommended tests,31,32 ultimately enhancing patient engagement, and shared decision making, regarding medical imaging among referring physicians and their patients.
Author Biographies
Jennifer L. Hay is Associate Attending Psychologist in the Department of Psychiatry and Behavioral Sciences at Memorial Sloan Kettering Cancer Center. Her work focuses on understanding how cognitive and emotional factors influence cancer prevention and control behaviors.
Geoffrey S. Gold is a doctoral candidate in clinical psychology at Hofstra University. He earned his master’s degree in clinical psychology from Hofstra University in 2015 and his bachelor’s degree in psychology from Binghamton University in 2013.
Raymond E. Baser is a biostatistician in the Department of Epidemiology & Biostatistics at Memorial Sloan Kettering Cancer Center and Co-Chair of the MSKCC Biostatistics Protocol Review Committee. He has particular expertise in the measurement and analysis of patient-reported outcome data.
Hedvig Hricak is Chair of the Department of Radiology, Memorial Sloan Kettering Cancer Center. The hallmark of her research career has been the validation of new diagnostic imaging technologies with a special emphasis on oncology. She is a member of the National Academy of Medicine (formerly the Institute of Medicine) of the National Academy of Sciences (NAS) and has served as Vice Chair of the NAS Committee on Tracking Radiation Doses from Medical Diagnostic Procedures, and as chair of the IOM/NAS Committee on Research Directions in Human Biological Effects of Low Level Ionizing Radiation.
Lawrence T. Dauer is a medical health physicist specializing in radiation protection at Memorial Sloan Kettering Cancer Center. He holds associate attending physicist appointments in both the Department of Radiology and Department of Medical Physics, and serves as the Radiation Safety Manager and Chair of the Emergency Management Committee. He has spent 30 years in the field of radiation protection and medical health physics.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hricak H, Brenner DJ, Adelstein SJ, et al. Managing radiation use in medical imaging: a multifaceted challenge. Radiology. 2011;258:889-905. [DOI] [PubMed] [Google Scholar]
- 2. International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007;37(2-4):1-332. [DOI] [PubMed] [Google Scholar]
- 3. National Research Council. Health Risks From Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 4. Semelka RC, Armao DM, Elias J, Jr, Picano E. The information imperative: is it time for an informed consent process explaining the risks of medical radiation? Radiology. 2012;262:15-18. [DOI] [PubMed] [Google Scholar]
- 5. Brenner DJ, Hricak H. Radiation exposure from medical imaging: time to regulate? JAMA. 2010;304:208-209. [DOI] [PubMed] [Google Scholar]
- 6. Tubiana M, Feinendegen LE, Yang C, Kaminski JM. The linear no-threshold relationship is inconsistent with radiation biologic and experimental data. Radiology. 2009;251:13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brink JA, Goske MJ, Patti JA. Informed decision making trumps informed consent for medical imaging with ionizing radiation. Radiology. 2012;262:11-14. [DOI] [PubMed] [Google Scholar]
- 8. Brink JA, Goske MJ, Patti JA. Informed consent for radiologic procedures. JAMA. 2011;305:888-889. [DOI] [PubMed] [Google Scholar]
- 9. Redberg RF, Smith-Bindman R. We are giving ourselves cancer. The New York Times. January 30, 2014. [Google Scholar]
- 10. Maloney E, Bylund C, Banerjee S. Newspaper coverage of the risks and benefits of medical radiation imaging. Paper presented at: The Annual Meeting of the Internation Communication Association; June 17-21, 2013; London, England. [Google Scholar]
- 11. Hay JL, Buckley TR, Ostroff JS. The role of cancer worry in cancer screening: a theoretical and empirical review of the literature. Psychooncology. 2005;14:517-534. [DOI] [PubMed] [Google Scholar]
- 12. Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9:443-460. [DOI] [PubMed] [Google Scholar]
- 13. Kroenke K, Spitzer RL, Williams JB, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613-621. [DOI] [PubMed] [Google Scholar]
- 14. Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol. Biomarkers Prev. 2007;16:998-1003. [DOI] [PubMed] [Google Scholar]
- 15. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. [Google Scholar]
- 16. Lumley T. Survey: analysis of complex survey samples. [R package version 3.28.2]. 2012. [Google Scholar]
- 17. Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9:1-19. [Google Scholar]
- 18. Busey JM, Soine LA, Yager JR, Choi E, Shuman WP. Patient knowledge and understanding of radiation from diagnostic imaging. JAMA Intern Med. 2013;173:239-241. [DOI] [PubMed] [Google Scholar]
- 19. Ludwig RL, Turner LW. Effective patient education in medical imaging: public perceptions of radiation exposure risk. J Allied Health. 2002;31:159-164. [PubMed] [Google Scholar]
- 20. Thornton RH, Dauer LT, Shuk E, et al. Patient perspectives and preferences for communication of medical imaging risks in a cancer care setting. Radiology. 2015;275:545-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006-483). U.S.Department of Education.Washington, DC: National Center for Education Statistics; 2006. [Google Scholar]
- 22. Viswanath K, Breen N, Meissner H, et al. Cancer knowledge and disparities in the information age. J Health Commun. 2006;11(suppl 1):1-17. [DOI] [PubMed] [Google Scholar]
- 23. Pidgeon N, Kasperson R, Slovic P. The Social Amplification of Risk. Cambridge, England: Cambridge University Press; 2003. [Google Scholar]
- 24. Aakhus M. Crafting interactivity for stakeholder engagement: transforming assumptions about communication in science and policy. Health Phys. 2011;101:531-535. [DOI] [PubMed] [Google Scholar]
- 25. Nelson DE, Hesse BW, Croyle RT. Making Data Talk: Communicating Public Health Data to the Public, Policy Makers, and the Press. New York, NY: Oxford University Press; 2009. [Google Scholar]
- 26. Consedine NS, Magai C, Krivoshekova YS, Ryzewicz L, Neugut AI. Fear, anxiety, worry, and breast cancer screening behavior: a critical review. Cancer Epidemiol Biomarkers Prev. 2004;13:501-510. [PubMed] [Google Scholar]
- 27. Hay JL, McCaul KD, Magnan RE. Does worry about breast cancer predict screening behaviors? A meta-analysis of the prospective evidence. Prev Med. 2006;42:401-408. [DOI] [PubMed] [Google Scholar]
- 28. Finkel AM. Perceiving others’ perceptions of risk: still a task for Sisyphus. Ann N Y Acad Sci. 2008;1128:121-137. [DOI] [PubMed] [Google Scholar]
- 29. Slovic P. Perception of risk. Science. 1987;236:280-285. [DOI] [PubMed] [Google Scholar]
- 30. Slovic P. Perception of risk from radiation. Radiat Protect Dosimetry. 1996;68:165-180. [Google Scholar]
- 31. Baerlocher MO, Detsky AS. Discussing radiation risks associated with CT scans with patients. JAMA. 2010;304:2170-2171. [DOI] [PubMed] [Google Scholar]
- 32. Dauer LT, Thornton RH, Hay JL, Balter R, Williamson MJ, St Germain J. Fears, feelings, and facts: interactively communicating benefits and risks of medical radiation with patients. AJR Am J Roentgenol. 2011;196:756-761. [DOI] [PMC free article] [PubMed] [Google Scholar]