Abstract
Purpose
The decline in U.S. adolescent fertility has accelerated since 2007. Modeling fertility change using behavioral data can inform adolescent pregnancy prevention efforts.
Methods
We used data on sexual activity and contraceptive use from National Surveys of Family Growth for young women 15–19 years of age, and contraceptive failure rates, to estimate a Pregnancy Risk Index (PRI) for the periods 2007, 2009, and 2012. Logistic regression was used to test for change over time in sexual activity, contraceptive use, and PRI. Statistical decomposition was used to calculate attribution of change in the PRI to changes in sexual activity or contraceptive method use.
Results
Sexual activity in the last 3 months did not change significantly from 2007 to 2012. Pregnancy risk declined among sexually active adolescent women (p = .046), with significant increases in the use of any method (78%–86%, p = .046) and multiple methods (26%–37%, p = .046). Use of highly effective methods increased significantly from 2007 to 2009 (38%–51%, p = .010). Overall, the PRI declined at an annual rate of 5.6% (p = .071) from 2007 to 2012 and correlated with birth and pregnancy rate declines. Decomposition estimated that this decline was entirely attributable to improvements in contraceptive use.
Conclusions
Improvements in contraceptive use appear to be the primary proximal determinants of declines in adolescent pregnancy and birth rates in the United States from 2007 to 2012. Efforts to further improve access to and use of contraception among adolescents are necessary to ensure they have the means to prevent pregnancy.
Keywords: Abstinence, Contraception, Sexual behaviors, Teen pregnancy
After substantial declines in the 1990s and early 2000s and a stall from 2005 to 2007, the U.S. adolescent birth rate declined rapidly between 2007 and 2013—dropping 36%, among 15- to 19-year olds [1]. There has also been a 25% decline in the adolescent pregnancy rate over a shorter period, falling from 70 pregnancies per 1,000 women in 2007 to 52 pregnancies per 1,000 women in 2011 [2]. The declines in adolescent pregnancy and birth rates since 2007 have occurred in all 50 states, across racial and ethnic groups, and among both younger and older teens, although differentials across subgroups and geographic locations remain [2,3]. Increasing use of abortion has not contributed to these declines, and abortion ratios (the ratio of abortions to live births) have declined very slowly over this period [2].
Despite these substantial declines, the United States continues to have adolescent birth and pregnancy rates that are higher than rates of other developed countries. Comparing rates of adolescent pregnancy in 2011, the U.S. rate (52 per 1,000 females, 15–19) is more than six times as high as Switzerland (8 per 1,000), more than twice as high as France (25 per 1,000) and slightly higher than England and Wales (47 per 1,000) [4]. Most adolescent pregnancies in the United States are unintended [5], and the majority of sexually active adolescent women report that they would be upset if they became pregnant [6].
To date, there has been limited research focused on identifying the causes of these rapid and large declines in the United States since 2007. Adolescent fertility is influenced by both distal and proximate factors. Distal factors may occur at many levels, including individual, household, community, and other structural contexts [7]. Given the broad scope of the declines, research has generally focused on macro-level social and economic factors such as the economy, media, and public policies [8–11]. These distal factors may influence fertility via proximate determinants, including sexual activity and use of contraception; changes in these behaviors and outcomes are national goals for Healthy People 2020 [12].
A focus on adolescent sexual activity and contraceptive use can improve our knowledge of the direct mechanisms driving the observed declines in adolescent pregnancy and childbearing. Understanding these two proximate factors can prime further research to examine distal determinants of adolescent fertility trends and inform policy development and implementation.
We have examined declines in adolescent pregnancy risk across the period from 1991 to 2007 in multiple analyses, using data from the National Survey of Family Growth (NSFG) as well as from high school students in the Youth Risk Behavior Surveillance (YRBS) [13–15]. Using NSFG data for 1995–2002, we found that 86% of the reduction in pregnancy risk among young women aged 15–19 (including both those in and out of school), was due to contraception, with the remainder due to declines in sexual activity (concentrated entirely among younger teens) [14]. Similarly, using YRBS data on high school students—a systematically younger group—we found that the substantial declines in adolescent pregnancy rates in the United States from 1991 to 2007 could be primarily attributed to improved contraceptive use [15].
A previous analysis estimated borderline increases in the pregnancy risk between 2003 and 2007 that paralleled a small increase in the actual adolescent birth and pregnancy rates from 2005 to 2007 [15]. This study and others validate our approach to measuring pregnancy risk, which accounts for sexual activity, contraceptive use, and contraceptive failure [16,17].
Building directly on these previous studies, this article uses NSFG data to examine how changes in adolescent sexual activity and contraceptive use influence adolescent fertility risk in the United States from 2007 to 2013. This analysis utilizes newly estimated method-specific contraceptive failure rates for the United States [18]. We estimate trends in sexual activity and contraceptive use patterns and use statistical decomposition to attribute declines in pregnancy risk to these two behavioral components.
Methods
Data
The NSFG is a periodic national probability household survey of women and men aged 15–44 years in the United States [19]. The NSFG used a multistage, stratified-clustered sampling frame; interviews were conducted continuously from June 2006 to December 2010 and again from June 2011 to June 2013. Sampling weights provided by the National Center for Health Statistics allow division of the data into three nationally representative and nonoverlapping periods: June 2006–June 2008, July 2008–December 2010, and June 2011–June 2013, which we refer to as 2007, 2009, and 2012, respectively. Our analyses were limited to women aged 15–19 at the time of the interview (2007 n = 1,085, 2009 n = 1,199, and 2012 n = 1,037). Methods of data collection and dissemination of the public use data set were reviewed by National Center for Health Statistics’ institutional review board protections of human subjects.
Measures
Following the methodology we developed and refined in prior work [13–16], we calculated the Pregnancy Risk Index (PRI) for each period estimating the annual risk of becoming pregnant among adolescent women based upon recent sexual activity (vaginal-penile sex in the last 3 months), contraceptive method(s) used at last sexual intercourse, and method-specific contraceptive failure rates (CFRs); nonuse of contraception was assigned a specific risk of pregnancy as well. Thus, the PRI score represents each woman’s risk of pregnancy in 1 year, given her sexual activity and contraceptive use. The overall PRI summarizes, at the population-level, the risk of pregnancy among all adolescents, incorporating information about both the level of recent sexual activity and the level of contraceptive risk.
For each individual i, we calculated a PRI score with the following formula:
The mean of these individual scores is the overall PRI of the entire population. As indicated by the formula, the PRI score for a woman who was not sexually active in the past 3 months (or had never had sexual intercourse) was set to zero, as she did not face a current risk of pregnancy. The PRI for each sexually active woman was estimated as the CFR of the methods used at last intercourse. We used new typical-use 1-year CFRs estimated from the 2006 to 2010 NSFG pregnancy and contraceptive calendars and adjusted for abortion underreporting [18]. A “typical-use” CFR is the number of pregnancies occurring among 100 women using a specific contraceptive method over a 12-month period; typical use refers to the way a method is actually used by women and their partners, including inconsistent or incorrect use [20]. Recent research has found significant variation in CFRs by race/ethnicity but not age [18]. Thus, for the most common methods (pill, patch, condom, and withdrawal), we used race/ethnicity-specific CFRs for 15- to 44-year olds (Failure rates stratified by race/ethnicity are available for women identified as Hispanic, non-Hispanic white, and non-Hispanic black. For the 6% of respondents identified as “other”, we applied the CFR for non-Hispanic white women.). For less common methods, only overall CFRs were available. To represent the reduced pregnancy risk associated with the use of two methods at most recent intercourse, we followed the practice of earlier research and multiplied the method-specific CFRs [15,16]. (Although women could report simultaneous use of up to four contraceptive methods, we limited our failure rate calculations to the two most effective methods.)
Sexually active women using no method at last intercourse were assigned a PRI score of 85, based on widely accepted estimates of the risk of pregnancy over a 12-month period [21]. Finally, following the approach of earlier research, women who were pregnant at the time of interview (n = 30 cases in 2007, 28 in 2009, and 27 in 2011) were assigned the contraceptive method that they reported using at the time they became pregnant [14]; (90.5% reported using no method at the time they got pregnant).
Analysis
For each of the three time periods (2007, 2009, and 2012), we estimated the percentages of sexually active female adolescents (sex in the last 3 months), the contraceptive methods used at most recent intercourse (or when pregnancy occurred), and the number of methods used, testing for significant changes over time between adjacent periods (2007 vs. 2009 and 2009 vs. 2012) and across the whole time period (2007 vs. 2012) using logistic regression. As a sensitivity analysis, we also examined changes over time in alternate measures of adolescent sexual activity (sex in the last 12 months, sex in the last 4 weeks, and ever had vaginal intercourse). Contraceptive method use was estimated for individual methods, as well as the overall use of highly effective methods (including intrauterine device, implant, injectable, pill, patch, and ring).
Next, we estimated the mean PRI among sexually active adolescents, and all adolescent women, for each period. We used paired t tests for the difference in means to test for significant changes over time. All analyses accounted for the complex survey design of the NSFG data using the svy commands in Stata 14 [22].
To compare the PRI estimated from the NSFG to actual pregnancy rates and birth rates for 15- to 19-year olds, we calculated Pearson correlation coefficients and compared the annualized rate of change in each measure. Pregnancy rates were available through 2011, while we examined birth rates through 2013 to align with the behavioral data from the NSFG (sexual and contraceptive behaviors in 2012 would result in births in 2013). Birth rates are a good proxy for pregnancy rates in assessing trends over time, as the ratio of abortions to live births has changed little from year to year among adolescents since 2007 [2].
Finally, to assess the extent to which the decline in the PRI from 2007 to 2012 was due to changes in sexual activity or changes in contraceptive use, we statistically decomposed the PRI into these two component parts. In the standard demographic decomposition formula described by Das Gupta [23] for decomposing change over two time periods, the first component of the PRI (sexual activity, in this case) is held constant in order to calculate a standardized rate: the amount we would expect the PRI to change if only the second component (contraceptive use) had changed. To extend this methodology to address change over three time periods, we instead calculated standardized changes in the rate between the first and second periods as well as between the first and third periods; we then averaged the two to arrive at the standardized change in the rate over the full period 2007–2012. This standardized change is divided by the observed change in the rate from 2007 to 2012 to give us the estimated proportion due to contraceptive use over the three time periods; the expected proportion due to sexual activity is calculated as its complement.
Results
Sexual activity in the last 3 months among all females ages 15–19 did not change significantly between 2007, 2009, and 2012 (31% 2007, 33% 2009, and 30% 2012), Table 1. Similarly, none of the alternate measures of sexual activity (sex in the last 12 months, sex in the last 4 weeks, and ever had vaginal intercourse) changed significantly between periods either.
Table 1.
Percentage of young women aged 15–19 by sexual activity and NSFG survey year, 2007–2012
| 2007 (N = 1,085) |
Survey year 2009 (N = 1,199) |
2012 (N = 1,037) |
2007 versus 2009
|
2009 versus 2012
|
2007 versus 2012
|
||||
|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | p value | p value | p value | |
| Measures of sexual activity | |||||||||
| Sexually active in last 3 months | 31 | 27.2–35.1 | 33 | 29.6–37.2 | 30 | 25.3–35.1 | .399 | .279 | .740 |
| Sexually active in last 12 months | 39 | 34.3–44.3 | 42 | 37.8–46.3 | 40 | 34.4–45.7 | .700 | .140 | .330 |
| Sexually active in the last 4 weeks | 25 | 21.9–28.8 | 28 | 24.6–31.4 | 25 | 20.1–29.8 | .290 | .280 | .852 |
| Ever had sex | 43 | 37.9–47.9 | 45 | 41.1–49.7 | 45 | 39.3–50.4 | .460 | .871 | .603 |
All measures refer to vaginal-penile intercourse.
CI = confidence interval.
Overall, contraceptive use patterns indicate increases in the use of methods by adolescent females during the examined period (Table 2). There was a statistically significant decline from 2007 to 2012 in the share of adolescents reporting no method use at last sex (22%–14%, p = .046). Conversely, the share of teens reporting one or more methods used at last sex increased significantly from 2007 to 2012, rising from 78% to 86%. There also was a statistically significant increase in the share of adolescent females reporting multiple method use (two or more methods) at last sex, increasing from 26% in 2007 to 37% in 2012 (p = .046); pill and condom were the most common combination across the period. Few young women reported use of three or more contraceptive methods at last sex. Overall, the use of all highly effective methods (IUD, implant, injectable, pill, patch, and ring) increased from 2007 to 2009 (from 38% to 51%, p = .01) but then did not change significantly from 2009 to 2012.
Table 2.
Selected contraceptive method use among adolescent women (15–19 years) who have engaged in recenta sexual intercourse by NSFG survey year, 2007–2012
| 2007
|
2009
|
2012
|
2007 versus 2009
|
2009 versus 2012
|
2007 versus 2012
|
||||
|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | p value | p value | p value | |
| Sexually active in last 3 months | 31 | 27.2–35.1 | 33 | 29.6–37.2 | 30 | 25.3–35.1 | .399 | .279 | .740 |
| Number of methods used at last sex | |||||||||
| No method | 22 | 16.8–27.7 | 13 | 9.1–19.3 | 14 | 9.1–20.3 | .025 | .921 | .046 |
| One or more methods | 78 | 72.3–83.2 | 87 | 80.7–90.9 | 86 | 79.7–90.9 | .025 | .921 | .046 |
| Two or more methods | 26 | 18.4–30.3 | 34 | 23.2–37.7 | 37 | 25.9–43.2 | .198 | .466 | .046 |
| Three or more methods | 2 | .6–5.5 | 4 | 2.0–8.9 | 3 | 1.3–6.2 | .218 | .464 | .505 |
| Method type | |||||||||
| Highly effective methodsb | 38 | 32.4–44.2 | 51 | 43.0–59.3 | 46 | 37.5–53.7 | .010 | .324 | .133 |
| IUD and implant | 1 | .5–3.8 | 4 | 2.0–8.9 | 3 | 1.2–9.1 | .072 | .704 | .194 |
| Injectable | 6 | 3.8–10.0 | 10 | 6.6–14.3 | 7 | 4.1–10.8 | .133 | .220 | .809 |
| Pill | 26 | 20.6–32.0 | 33 | 27.1–40.1 | 35 | 27.0–43.3 | .084 | .780 | .068 |
| Patch and ring | 5 | 2.5–8.6 | 4 | 2.0–7.1 | 1 | .2–2.5 | .694 | .024 | .007 |
| Condom | 49 | 42.3–56.1 | 50 | 42.8–57.8 | 55 | 47.5–63.1 | .817 | .336 | .224 |
| Withdrawal | 15 | 10.3–21.7 | 18 | 13.4–24.8 | 20 | 13.5–27.8 | .412 | .771 | .306 |
| Rhythm | 1 | .3–4.5 | 0 | .0–1.1 | 2 | .8–3.7 | .087 | .017 | .619 |
Bold indicates statistically significant findings.
Defined as within the last 3 months.
Includes IUD, implant, injectable, pill, patch, and ring.
Despite these increases in use of any method and multiple methods, we found few significant increases in use of any specific methods at last intercourse. Use of IUD or implant had a marginally significant increase from 2007 to 2009 (from 1% to 4%, p = .072) but was unchanged in the later period, while use of injectables did not change significantly over time. From 2007 to 2012, there was a marginally significant increase in use of the pill (26%–35%, p = .068) but a significant decline in use of the patch or ring (5%–1%, p = .007). There were also nonsignificant increases in condom use (49%–55%) and withdrawal (15%–20), while use of the rhythm method did not change and remained at or less than 2%.
Together, these shifts in contraceptive use resulted in a significant decline in the PRI (Table 3). Among adolescents sexually active in the last 3 months, the PRI declined 26% from 2007 to 2012 (annual rate of 5%), p = .046. Among all adolescent women, the PRI declined 28% from 2007 to 2012 (annual rate of 6%), p = .071. Our decomposition analysis estimated that 106% of the change in the overall PRI from 2007 to 2012 was attributable to improvements in contraceptive method use, and −6% was attributable to changes in the percentage of sexually active young women. The negative attribution to sexual activity indicates that if only the observed changes in sexual activity had occurred (specifically the nonsignificant increase from 31% to 33% from 2007 to 2009), this would have resulted in an increase in the PRI. Instead, the entire decline in the PRI is attributed to improvements in contraceptive use, which compensated for the increase in sexual activity.
Table 3.
Pregnancy risk index and overall changes attributable to sexual activity and contraceptive use, by NSFG survey year, 2007–2012
| Survey year
|
2007 versus 2009
|
2009 versus 2012
|
2007 versus 2012
|
Annual change(2007–2012)
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2007
|
2009
|
2012
|
||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | p value | p value | p value | % | |
| Pregnancy Risk Index (PRI) | ||||||||||
| Sexually active adolescents | 24 | 19.6–27.5 | 17 | 12.7–20.9 | 18 | 13.1–21.9 | .019 | .804 | .046 | −5.1 |
| All adolescents | 7 | 5.7–8.9 | 6 | 4.1–7.0 | 5 | 3.7–6.7 | .128 | .754 | .071 | −5.6 |
| Overall Change in PRI | ||||||||||
| Percent attributable to sexual activity | −6% | |||||||||
| Percent attributable to contraceptive use | 106% | |||||||||
Figure 1 shows the trends in the PRI, pregnancy rate, and birth rate. The pregnancy risks estimated from behavioral data were highly correlated with actual changes in adolescent pregnancy and birth rates (Pearson correlations of .88 and .84, respectively). The 5.6% annual rate of decline in the overall PRI from 2007 to 2012 compares similarly to the 6.3% annual rate of decline in the adolescent pregnancy rate from 2007 to 2011 and the annual rate of decline in the adolescent birth rate (declining 5.8% from 2007 to 2012 and 6.0% from 2007 to 2013).
Figure 1.
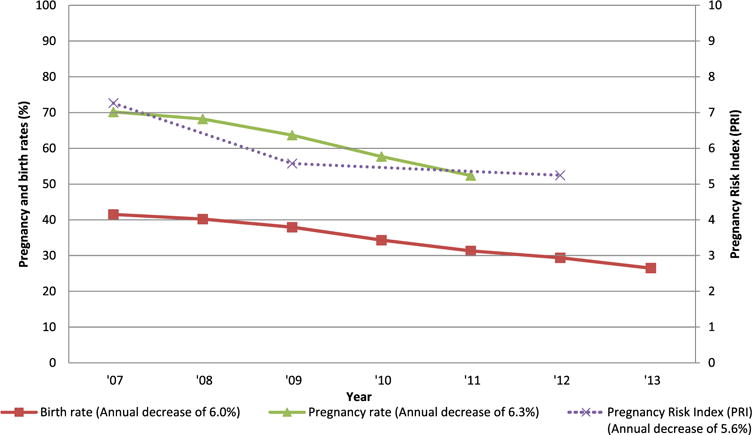
Birth rate, pregnancy rate, and pregnancy risk among women aged 15–19 years, 2007–2013.
Discussion
Substantial declines in adolescent pregnancy and birth rates in the United States occurred between 2007 and 2012. During this period, we estimated significant declines in the PRI—a behavioral indicator determined by sexual activity, contraceptive use, and contraceptive efficacy—correlated to the declines in the pregnancy and birth rates.
Our analysis indicates that improvement in contraceptive use accounted for all the decline in the PRI from 2007 to 2012. Statistically significant improvements in contraceptive use included increases in the share of adolescent girls using any contraceptive method at last sex (and thus an equal decline in use of no method) and increases in multiple method use. Both of these trends were influenced by an increase in highly effective methods, particularly the pill. These findings extend and parallel the conclusions of our previous research analyses that found that improvements in contraceptive use drove much of the decline in teen pregnancy rates from 1991 to 2007. However, during this earlier period, some of the PRI decline also was attributed to declining sexual activity. Here, the NSFG shows no decline in adolescent sexual activity from 2007 to 2012 (and a nonsignificant increase from 2007 to 2009), suggesting that this behavioral factor did not play a role in the recent PRI declines. Most recently (since this article was initially peer reviewed), data from the national YRBS shows sharp declines in sexual activity among high school students from 2013 to 2015—after a long plateau from 2001 to 2013 [24]. At this point, it is unclear whether these new data represent a new trend or are the result of other factors.
The PRI methodology, which creates a composite measure, identified reductions in overall risk not apparent in the individual contraceptive method use measures. Although overall contraceptive use increased, changes over time in specific methods generally were not statistically significant at conventional levels. However, with less than one-third of adolescent women sexually active, our statistical testing for changes in contraceptive use was underpowered. Although we found small (and not statistically significant) changes in some contraceptive methods, it was in combination that, these changes resulted in significant reductions in the PRI.
Although some studies have descriptively linked increased access to LARC (long-acting reversible contraceptive) methods to localized declines in adolescent birth rates [25,26], our analysis indicates that LARC use has played a modest role at the national-level through 2012. While the share of adolescents using LARC at last sex did not change significantly during the period under study, this may change moving forward with newer clinical guidelines supporting LARC methods as first-line contraceptive choices for adolescents [27,28]. Recent data collected from high school students in the YRBS survey documents an increase in IUD and implant use from 2013 to 2015 for female students [24]. Given its relatively low failure rates, even with typical use, future increases in LARC use would reduce pregnancy risk. But any efforts to promote LARC use should be guided by individuals’ method preferences and reproductive autonomy, recognizing that contraception is a personal decision and not “one size fits all” [29].
These analyses rely on new typical-use CFRs estimated from the 2006–2010 NSFG [18]. These new failure rates have decreased as compared to estimates derived from earlier rounds of the NSFG, indicating improvements in how couples use contraception. (These improvements contrast with little change in CFRs between 1988 and 2002.) [30–32]) Estimates for all methods from the 2006–2010 survey are more than one-third lower than those from the 1995 survey. Studies that do not incorporate these improvements in CFRs may miss an important influence on adolescent pregnancy and birth rates [8,33].
The recent declines in adolescent pregnancy and birth rates in the United States have not occurred in isolation but are part of nearly universal reductions in adolescent fertility during the second half of the 20th century. Since the 1950s in both the United States and Western Europe, declining adolescent fertility has been influenced by widespread social forces such as rising educational opportunities for young women, the invention of modern methods of contraception, rising age at marriage, and legalization of abortion [34]. Prior research found that much of the difference in adolescent pregnancy rates between the United States and European countries resulted from lower rates of contraceptive use among U.S. adolescents [35]; the increasing rates documented here may reduce these differences.
Limitations
This analysis had several limitations. Although the overall NSFG sample size is adequate, small sample sizes in key subgroups, particularly sexually active adolescents, constrained our ability to examine differential patterns by racial/ethnic or age groups within the adolescent population. Estimates of method-specific contraceptive use among sexually active adolescents were underpowered, reducing the likelihood of estimating statistically significant changes.
We applied CFRs estimated from the 2006–2010 NSFG; any potential changes within this period, or since 2010, cannot be identified. We also assumed that there was no change in adolescents’ biological fecundity during the relatively short study period. The analysis relies on self-reports which may reflect social desirability bias or other reporting errors. Our analysis did not consider changes in the composition of which adolescents use which contraceptive methods, and further attention should be given to heterogeneity among adolescents by their method of contraception.
We recognize that by focusing on changes in the proximate determinants of adolescent pregnancy—sexual activity and contraceptive use—this analysis does not measure how upstream social or ecological influences impact these behaviors. Future research should continue to investigate the distal influences of the recent declines in adolescent pregnancy. The findings of this analysis also argue for a focus on mechanisms that influence contraceptive use patterns instead of influences on sexual activity, which has contributed little to the ongoing declines in adolescent pregnancy risk.
Public health implications
The rapid declines in adolescent pregnancy and births from 2007 to 2012 occurred despite stagnant rates of sexual activity. Instead, we find that the contraceptive behaviors of sexually active adolescents have driven the recent shifts in fertility outcomes. The increases in overall contraceptive use at last sex from 2007 to 2012 are part of a longer trend. Between 1995 and 2012, any method use at last sex among adolescent women increased from 66% to 86%, while use of multiple methods increased from 11% to 37% [14]. Taken together, evidence from this study and our previous studies indicates that the substantial long-term decline of 57% in adolescent birth rates from 1991 to 2013 [1] can be primarily attributed to increases in overall contraceptive use. With the risk of pregnancy associated with no method use at 85%, adolescents’ uptake of any method, regardless of its failure rate, markedly reduces this risk. Policy discussions should focus on supporting adolescent contraceptive use generally, including access to the full range of methods.
Public policy and programs can play a critical role in supporting adolescent contraceptive use. Since contraceptive use is the critical driver of adolescent fertility, it is important to ensure adolescents’ access to comprehensive sexuality education that provides medically accurate information about contraception. A recent meta-analysis of comprehensive sexuality education and abstinence-only programs evaluation data indicates that comprehensive sexuality education can increase condom and contraceptive use; however, abstinence-only programs have not demonstrated effectiveness in changing adolescent sexual behavior or in reducing teen pregnancy or sexually transmitted infections [36]. Despite recent declines in adolescent pregnancy, the percentage of adolescents who report receiving formal instruction about birth control has declined, while the share receiving only abstinence instruction has increased [37]. The increased availability of the Internet to adolescents and the anonymity it provides for searching sensitive topics, offers new opportunities to meet the sexual health needs of adolescents [38]. Further research should examine adolescents’ use of online sexual and reproductive health information online, as well as the quality of this information.
The increase in adolescent contraceptive use may reflect recent efforts to increase adolescents’ access to reproductive health services, including expanding private and public insurance coverage through the Affordable Care Act and changing clinical guidelines [27,28,39]. Despite insurance expansion, publicly funded family planning centers remain an important source of contraceptive and reproductive health care, serving more than one million adolescents in 2013 [40]. Continued support of funding mechanisms that provide adolescents with confidential and comprehensive sexual and reproductive health care are necessary to maintain and expand the contraceptive use patterns observed in this study and to ensure access to supportive and essential adolescent health services.
IMPLICATIONS AND CONTRIBUTION.
Rapid declines in adolescent pregnancy and birth rates from 2007 to 2012 can be attributed to increases in contraceptive use, including use of any method, multiple methods, and of more effective methods. Based on this and previous research, adolescent fertility declines since 1991 can be primarily attributed to improved contraceptive use.
Acknowledgments
Funding Sources
This work was funded by a grant from the JPB Foundation (grant 386). Additional support was provided by the Guttmacher Center for Population Research Innovation and Dissemination (NIH grant 5 R24 HD074034).
References
- 1.Ventura SJ, Hamilton BE, Matthews TJ. National and state patterns of teen births in the United States, 1940–2013. Natl Vital Stat Rep. 2014;63:1–34. [PubMed] [Google Scholar]
- 2.Kost K, Maddow-Zimet I. National trends by age, race and ethnicity. New York, NY: Guttmacher Institute; 2016. U.S. teenage pregnancies, births and abortions, 2011. [Google Scholar]
- 3.Kost K, Maddow-Zimet I. State trends by age, race and ethnicity. New York, NY: Guttmacher Institute; 2016. U.S. teenage pregnancies, births and abortions, 2011. [Google Scholar]
- 4.Sedgh G, Finer LB, Bankole A, et al. Adolescent pregnancy, birth, and abortion rates across countries: Levels and recent trends. J Adolesc Health. 2015;56:223–30. doi: 10.1016/j.jadohealth.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374:843–52. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lau M, Lin H, Flores G. Pleased to be pregnant? Positive pregnancy attitudes among sexually active adolescent females in the United States. J Pediatr Adolesc Gynecol. 2014;27:210–5. doi: 10.1016/j.jpag.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Bongaarts J. A framework for analyzing the proximate determinants of fertility. Popul Dev Rev. 1978;4:105. [Google Scholar]
- 8.Kearney MS, Levine PB. Investigating recent trends in the US teen birth rate. J Health Econ. 2015;41:15–29. doi: 10.1016/j.jhealeco.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Kearney MS, Levine PB. Media influences on social outcomes: The impact of MTV’s 16 and Pregnant on teen childbearing. Am Econ Rev. 2015;105:3597–632. doi: 10.1257/aer.20140012. [DOI] [PubMed] [Google Scholar]
- 10.Boonstra HD. What is behind the declines in teen pregnancy rates? Guttmacher Policy Rev. 2014;17:15–21. [Google Scholar]
- 11.Ananat EO, Gassman-Pines A, Gibson-Davis C. Community-wide job loss and teenage fertility: Evidence from North Carolina. Demography. 2013;50:2151–71. doi: 10.1007/s13524-013-0231-3. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services. 2020 Topics & Objectives. Family Planning. Available at: http://www.healthypeople.gov/2020/topics-objectives/topic/family-planning/objectives. Accessed February 24, 2016.
- 13.Santelli JS, Abma J, Ventura S, et al. Can changes in sexual behaviors among high school students explain the decline in teen pregnancy rates in the 1990s? J Adolesc Health. 2004;35:80–90. doi: 10.1016/j.jadohealth.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Santelli JS, Lindberg LD, Finer LB, et al. Explaining recent declines in adolescent pregnancy in the United States: The contribution of abstinence and improved contraceptive use. Am J Public Health. 2007;97:150–6. doi: 10.2105/AJPH.2006.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santelli JS, Orr M, Lindberg LD, et al. Changing behavioral risk for pregnancy among high school students in the United States, 1991–2007. J Adolesc Health. 2009;45:25–32. doi: 10.1016/j.jadohealth.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 16.Santelli JS, Lindberg LD, Orr MG, et al. The pregnancy risk index: A useful method to estimate risk of pregnancy using existing behavioral data. New York, NY: Columbia University; 2009. [Google Scholar]
- 17.Waddell EN, Orr MG, Sackoff J, et al. Pregnancy risk among black, white, and Hispanic teen girls in New York City public schools. J Urban Health. 2010;87:426–39. doi: 10.1007/s11524-010-9454-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sundaram A, Vaughan B, Kost K. Contraceptive failure in the United States: Estimates from the 2006–2010 National Survey of Family Growth; paper presented at the annual meeting of the Population Association of America; Washington, DC. March 31–April 2, 2016. [Google Scholar]
- 19.Centers for Disease Control and Prevention, Division of Vital Statistics. National Survey of Family Growth. Available at: http://www.cdc.gov/nchs/nsfg.htm. Accessed February 22, 2016.
- 20.Trussell J, Kost K. Contraceptive failure in the United States: A critical review of the literature. Stud Fam Plann. 1987;18:237. [PubMed] [Google Scholar]
- 21.Trussell J. Technol. 20th. Atlanta, GA: Bridgeing the Gap Communications; 2011. Efficacy: “Will it work?” Contracept. [Google Scholar]
- 22.StataCorp. Stata statistical software: Release 14. College Station, TX: StataCorp LP; 2014. [Google Scholar]
- 23.Das Gupta P. Standardization and decomposition of rates: A user’s manual. Washington, DC: US Department of Commerce, Economics and Statistics Administration, Bureau of the Census; 1993. [Google Scholar]
- 24.Kann L. Youth Risk Behavior Surveillance—United states, 2015. MMWR Surveill Summ. 2016;65:1–174. doi: 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 25.Secura GM, Madden T, McNicholas C, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med. 2014;371:1316–23. doi: 10.1056/NEJMoa1400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: Widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46:125–32. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 27.American College of Obstetricians and Gynecologists. Acog practice bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118:184–96. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 28.Committee on Adolescence. Contraception for adolescents. Pediatrics. 2014;134:e1244–56. doi: 10.1542/peds.2014-2299. [DOI] [PubMed] [Google Scholar]
- 29.Gubrium AC, Mann ES, Borrero S, et al. Realizing reproductive health equity needs more than long-acting reversible contraception (LARC) Am J Public Health. 2016;106:18–9. doi: 10.2105/AJPH.2015.302900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones EF, Forrest JD. Contraceptive failure rates based on the 1988 NSFG. Fam Plann Perspect. 1992;24:12–9. [PubMed] [Google Scholar]
- 31.Kost K, Singh S, Vaughan B, et al. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ranjit N, Bankole A, Darroch JE, et al. Contraceptive failure in the first two years of use: Differences across socioeconomic subgroups. Fam Plann Perspect. 2001;33:19–27. [PubMed] [Google Scholar]
- 33.Manlove J, Karpilow Q, Welti K, et al. Linking changes in contraceptive use to declines in teen pregnancy rates. Societies. 2015;6:1. [Google Scholar]
- 34.Lloyd CB, editor. Growing Up Global: The Changing Transitions to Adulthood in Developing Countries. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 35.Santelli JS, Sandfort T, Orr M. Transnational comparisons of adolescent contraceptive use: What can we learn from these comparisons? Arch Pediatr Adolesc Med. 2008;162:92–4. doi: 10.1001/archpediatrics.2007.28. [DOI] [PubMed] [Google Scholar]
- 36.Chin HB, Sipe TA, Elder R, et al. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: Two systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;42:272–94. doi: 10.1016/j.amepre.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 37.Lindberg L, Boonstra H, Maddow-Zimet I. Changes in adolescents’ receipt of sex education, 2006–2013. J Adolesc Health. 2016;58:621–7. doi: 10.1016/j.jadohealth.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simon L, Daneback K. Adolescents’ use of the internet for sex education: A thematic and critical review of the literature. Int J Sex Health. 2013;25:305–19. [Google Scholar]
- 39.English A. The patient protection and Affordable Care Act of 2010: How does it help adolescents and young adults? Cent Adolesc Health L Natl Adolesc Health Inf Innov Cent. 2010:1–9. [Google Scholar]
- 40.Frost JJ, Frohwirth L, Zolna MR. Contraceptive needs and services, 2013 update. New York, NY: Guttmacher Institute; 2015. [Google Scholar]


