Abstract
The cancer stem cell (CSC) hypothesis has captured the attention of many scientists. It is believed that elimination of CSCs could possibly eradicate the whole cancer. CSC surface markers provide molecular targeted therapies for various cancers, using therapeutic antibodies specific for the CSC surface markers. Various CSC surface markers have been identified and published. Interestingly, most of the markers used to identify CSCs are derived from surface markers present on human embryonic stem cells (hESCs) or adult stem cells. In this review, we classify the currently known 40 CSC surface markers into 3 different categories, in terms of their expression in hESCs, adult stem cells, and normal tissue cells. Approximately 73% of current CSC surface markers appear to be present on embryonic or adult stem cells, and they are rarely expressed on normal tissue cells. The remaining CSC surface markers are considerably expressed even in normal tissue cells, and some of them have been extensively validated as CSC surface markers by various research groups. We discuss the significance of the categorized CSC surface markers, and provide insight into why surface markers on hESCs are an attractive source to find novel surface markers on CSCs.
Keywords: Adult stem cells, Cancer stem cells, Human embryonic stem cells, Normal tissue cells, Surface marker
INTRODUCTION
Scientific knowledge about cancer formation and progression has explosively expanded over the past two decades. Cancers are regarded as aberrant and heterogeneous tissues containing a variety of cells that originate from a unique and rare subset of cancer cells having a self-renewal capacity and potential to differentiate into multiple cell lineages (1). Rare subsets of cancer cells with stem-like properties, referred to as cancer stem cells (CSCs) or tumor initiating cells (TICs), are responsible for cancer initiation, progression, and dissemination to distant organs (1, 2). The first prospective identification of CSCs was carried out with acute myeloid leukemia (AML), in which the surface markers of leukemic stem cells were defined as CD34+CD38− phenotype (3). When transplanted into non-obese diabetic/severe combined immunodeficiency (NOD/SCID) mice, the small immature subset of CD34+CD38− cells was able to reinitiate the same leukemia, whereas the major abundant subset of CD34+CD38+ cells was ineffective (3). The results demonstrates for the first time the existence of CSCs in liquid tumors, and encouraged many researchers to use various cell surface markers to isolate CSCs from heterogeneous cell populations of solid tumor tissues. Since then, CSCs have been isolated from various solid tumors, including breast (4), brain (5), prostate (6), pancreas (7), colon (8), lung (9), stomach (10), ovary (11), liver (12), and skin (13). After the identification of various CSCs, many researchers believe that the specific elimination of these cells will lead to the disappearance of entire tumors, based on the concept that the sole source of tumor self-renewal is the CSC. Since CSCs were identified on the basis of their cell surface molecules, specific antibodies/immunotoxins against the surface molecules have also been successfully developed to selectively eradicate CSCs (14–17). Although there are still some doubts about the therapeutic strategies targeting CSCs, the approaches are expected to lead to better clinical outcomes in cancer patients, by halting the tumor progression (15, 18).
The development of therapeutic strategies targeting CSCs mainly relies on the use of cell surface markers to identify, enrich, and/or isolate CSCs. Many CSC surface markers have been identified, although some surface markers are controversial and need further investigation (1, 2, 19). Interestingly, most of the current CSC surface markers are derived from known normal embryonic or adult stem cell surface markers (1, 2, 19–21). The similarity of cell surface markers suggests that CSCs predominantly originate from normal stem cells via the accumulation of epigenetic and genetic alterations (20). In this review, the currently published 40 CSC surface markers are classified into 3 different categories, depending on their expression on hESCs, adult stem cells, and normal tissue cells. The first group of CSC surface markers are expressed on hESCs, but are weakly or rarely expressed on normal tissue cells (Table 1). The second group of CSC surface markers are expressed on adult stem cells, but are weakly or rarely expressed on normal tissue cells (Table 2). The third group of CSC surface markers are expressed on hESCs and/or adult stem cells, and are also considerably expressed on various normal tissue cells (Table 3). In the tables, the histological data of some CSC surface markers not been published before, originates from the human protein atlas (http://www.proteinatlas.org/). CD133 is the most frequently studied CSC surface marker in various cancers, and specific antibodies/immunotoxins against CD133 have been successfully developed for their selective eradication (14, 17). CD133 expression is detected in 22 of 82 cell types from 44 normal human tissues (approximately 27%) (http://www.proteinatlas.org/). Based on the rate of CD133 expression, a CSC surface marker is classified as rare expression in normal tissue cells, if the marker is detected less than 27% (< 22 out of 82 normal tissue cells).
Table 1.
CSC surface markers expressed on hESCs, but rarely expressed in normal tissue cells
| CSC surface marker | Origin and function | Expression in hESC/hPSC | Expression in adult stem cell | Expression in normal tissues/cells | Expression in CSCs | Ref. |
|---|---|---|---|---|---|---|
| SSEA3 | hESC marker | Yes | Mesenchymal | Rare | Teratocarcinoma, breast | (22, 23, 26) |
| SSEA4 | hESC marker | Yes | Mesenchymal, cardiac | Rare | Teratocarcinoma, breast | (24–26) |
| TRA-1-60 | hESC marker | Yes | NA* | Rare | Teratocarcinoma, breast, prostate | (28, 29) |
| TRA-1-81 | hESC marker | Yes | NA | Rare | Teratocarcinoma, breast | (28) |
| SSEA1 | Mouse ESC marker | Yes (mouse) | Cardiac | Rare | Teratocarcinoma, renal, lung | (30–32) |
| CD133 (AC133) | Marker for hematopoietic stem cells. | Yes | Hematopoietic Neural Prostate | Rare (proliferative cell) | Breast, prostate, colon, glioma, liver, lung, ovary | (33–38) |
| CD90 (Thy-1) | Signal transduction/cell adhesion | Yes | Mesenchymal, cardiac | Rare (T-cell, neuron) | Brain, liver | (39–43) |
| CD326 (EpCAM) | Cell adhesion, signal transduction | Yes | No | Rare (epithelial cell) | Colon, pancreas, liver | (7, 44–46) |
| Cripto-1 (TDGF1) | Self-renewal/survival in esc | Yes | NA | Rare (pancreas, hippocampus) | Breast, colon, lung | (47, 48) |
| PODXL-1 (Podocalyxin-like protein 1) | Ligand for L-selectin | Yes | Mesenchymal Hematopoietic | Rare (podocyte) | Leukemia, breast, pancreas, lung | (49–51) |
| ABCG2 | ATP-binding cassette transporter | Yes | Hematopoietic Muscle Neural | Rare (myogenic) | Lung, breast, brain | (53–55) |
| CD24 | B cell proliferation | Yes | Intestinal | Rare (B lymphoid, neural) | Breast, gastric, pancreas | (4, 36, 57) |
| CD49f (Integrin α6) | Cell adhesion | Yes | Hematopoietic | Rare (rectum, urinary bladder) | Glioma | (58–60) |
| Notch2 | Signal transduction | Yes | Neural | Rare (subset in large intestine) | Pancreas, lung | (61–63) |
| CD146 (MCAM) | Melanoma cell adhesion molecule | Yes | Mesenchymal | Rare (endothelial, ganglion cell) | Rhabdoid tumor, sarcoma | (36, 64, 65) |
| CD10 (Neprilysin) | Metallo-endopeptidase, FDA-approved target | Yes | Mesenchymal | Rare (glandular cells in some tissues) | Breast, head and neck | (36, 66–69) |
| CD117 (c-KIT) | Receptor for stem cell factor, FDA-approved target | Yes | Mesenchymal Cardiac | Rare (myeloid) | Ovary | (36, 70–72) |
| CD26 (DPP-4) | Dipeptidyl peptidase iv, FDA-approved target | Yes | Hematopoietic | Rare (intestine, kidney, male, female tissues, activated T, B, NK cells) | Colorectal, leukemia | (73–75) |
Not available.
Table 2.
CSC surface markers expressed on adult stem cells, but rarely expressed on normal tissue cells
| CSC surface marker | Origin and function | Expression in hESC/hPSC | Expression in adult stem cell | Expression in normal tissue/cells | Expression in CSCs | Ref. |
|---|---|---|---|---|---|---|
| CXCR4 | Receptor for chemokine, FDA-approved target | No | Neural | Rare (lymphoid) | Breast, brain, pancreas | (76–79) |
| CD34 | Cell adhesion | No | Hematopoietic | Rare (lymphoid) | Leukemia, squamous cell carcinoma | (3, 80–82) |
| CD271 | Nerve growth factor receptor | No | Mesenchymal | Rare (neural crest) | Melanoma, head and neck | (13, 83, 84) |
| CD13 (Alanine aminopeptidase) | Marker for kidney disease | No | Mesenchymal | Rare (myeloid) | Liver | (85–87) |
| CD56 (NCAM) | Cell adhesion | No | Mesenchymal | Rare (lymphoid) | Lung | (88, 89) |
| CD105 (Endoglin) | Coreceptor for TGF-β | No | Mesenchymal | Rare (endothelial) | Renal | (90–92) |
| LGR5 | Cell adhesion | No | Intestinal, kidney, stomach, hair follicle | Rare (brain, intestine, female tissues) | Intestinal, colorectal | (93–98) |
| CD114 (CSF3R) | Colony stimulating factor 3 receptor, FDA-approved target | No | Neural crest, BM-derived precursors | Rare (placenta, BM, brain, heart muscle, skin) | Neuroblastoma | (99–101) |
| CD54 (ICAM-1) | Cell adhesion, FDA-approved target | No | Mesenchymal | Rare (endothelial cell) | Gastric | (102–104) |
| CXCR1, 2 | Receptor for chemokine | NA* | Mesenchymal | Rare (spleen, leucocyte subset) | Breast, pancreas | (105–108) |
| TIM-3 (HAVCR2) | Immune checkpoint receptor | NA | NA | Rare (lymphoid) | Leukemia | (109) |
| CD55 (DAF) | Inhibitor of complement | NA | NA | Rare (lymphoid) | Breast | (110, 163) |
| DLL4 (Delta-like ligand 4) | Notch ligand | NA | Intestinal | Rare (intestine, liver, gall bladder and renal tubuli, Purkinje and glandular cells) | Colorectal, ovarian | (111–113) |
| CD20 (MS4A1) | B cell lineage, FDA-approved target | No | No | Rare (lymphoid) | Melanoma | (114–116, 164, 165) |
| CD96 | T cell-specific receptor | NA | No | Rare (weak in lymphoid) | Leukemia | (117–120, 166) |
Not available.
Table 3.
CSC surface markers expressed on both stem cells and normal tissue cells
| CSC surface marker | Origin and function | Expression in hESC/hPSC | Expression in adult stem cell | Expression in normal tissue cells | Expression in CSCs | Ref. |
|---|---|---|---|---|---|---|
| CD29 (Integrin β1) | Cell adhesion, FDA-approved target | Yes | Mesenchymal | Ubiquitously | Breast, colon | (36, 121–123) |
| CD9 | Cell adhesion | Yes | Adipose-derived mesenchymal | Many tissues (except gall bladder, liver, lymphoid tissues) | Leukemia | (70, 124–126) |
| CD166 (ALCAM) | Cell-cell/cell-matrix interaction | Yes (weak) | Adipose, intestine | Many epithelial cells | Colorectal, lung | (9, 36, 127–130) |
| CD44 variants | Hyaluronic acid receptor, FDA-approved target | No | Hematopoietic Adipose Mesenchymal | Most epithelial and lymphatic tissues | HNSCC, breast, colon, liver, ovarian, pancreas, gastric | (91, 131–140) |
| ABCB5 | ABC transporter | NA* | Limbal | Majority of normal tissues (weak, moderate) | Melanoma | (141, 142) |
| Notch3 | Signal transduction | NA | Neural | Many tissues | Pancreas, lung | (61, 63) |
| CD123 (IL-3R) | Receptor for IL-3 | NA | No | Majority of normal tissues | Leukemia | (143, 144) |
Not available.
CSC SURFACE MARKERS EXPRESSED ON hESCs, BUT RARELY EXPRESSED IN NORMAL TISSUE CELLS
CSC surface markers expressed on hESCs, but rarely expressed in normal tissue cells, are summarized in Table 1. Stage-specific embryonic antigen 3 (SSEA-3) and SSEA-4 are epitopes on related glycosphingolipids, and play a key role in identifying hESCs (22). SSEA-3 is expressed on adult human mesenchymal stem cells (MSCs) (23), while SSEA-4 is expressed on mesenchymal and cardiac stem cells (24, 25). SSEA-3 and SSEA-4 are expressed on breast cancer cells and breast CSCs (26). TRA-1-60 and TRA-1-81 antigens, expressed on podocalyxin in human pluripotent stem cells (hPSCs) (27), are associated to breast cancer (28). TRA-1-60 is also expressed on a minor subset of stem-like human prostate TICs (29). SSEA-1 is a surface marker for neural stem cells (NSCs), and SSEA-1+ cells from brain tumors show properties of brain tumor stem cells (30). SSEA-1 is also related to lung and renal tumors (31, 32). SSEA-3, SSEA-4, TRA-1-60, TRA-1-81, and SSEA-1 are all carbohydrate epitopes and well-characterized oncofetal antigens, which are rarely expressed in adult normal differentiated tissues and cells. They are all hESC surface markers, except for SSEA-1.
CD133 (Prominin-1) is a glycosylated, 115–120-kDa protein with five transmembrane domains and two large extracellular loops (33). The exact function of CD133 still remains unknown, but it seems to organize cell membrane topology (34). CD133 was initially discovered as a target of AC133 monoclonal antibody (MAb), specific for the CD34+ population of hematopoietic stem cells (HSCs) (35). CD133 is expressed on the surface of hESCs (36) and NSCs (37), and is downregulated upon the differentiation of hESCs, suggesting that CD133 expression is restricted to undifferentiated hESCs (36). CD133 is one of the most frequently studied surface markers in solid cancers (33). The CD133 marker has identified CSC populations in the breast, brain, lung, pancreas, liver, prostate, ovary, colon, and head and neck cancers, and CD133+ populations clearly generate tumors in immunocompromised mice more efficiently than CD133− populations (33). Although CD133 is mainly expressed on the surface of proliferating cells, it has also been detected on the surface of differentiated epithelial cells in a variety of tissues (http://www.proteinatlas.org/). It appears that CD133 protein expression does not change upon differentiation; however, tertiary conformational changes in differentiated colon cancer cells block the binding of AC133 antibody, suggesting that the expression of the AC133 epitope is restricted to undifferentiated stem cells (33, 38). Targeting CD133+ cells with AC133-derivatives in the human body also shows minimal side effects, suggesting that CD133 expression may be quite low in normal stem cells, and the plasticity of human HSCs may select a normal stem cells with a CD133− phenotype during the targeted therapies (17).
CD90 (Thy-1) is expressed on bone marrow (BM)-derived MSCs (39) and undifferentiated hESCs, whereas it is rarely expressed in normal tissue cells (40). Since CD90+ cells from hepatocellular carcinoma cell lines are capable of generating tumor nodules in immunodeficient mice, CD90 is also considered a marker for brain and insulinoma CSCs (41–43). EpCAM (epithelial cell adhesion molecule, CD326) is a transmembrane glycoprotein mediating Ca2+-independent homotypic cell-cell adhesion in epithelial cells. Although EpCAM is expressed on some normal epithelial tissues and cells, it has been used as an undifferentiated hESC marker (44). EpCAM is also found in most adenocarcinomas, and is involved in tumor metastases and CSCs (45). EpCAM+ hepatocellular carcinoma and pancreatic carcinoma cells have been suggested to function as TICs with stem/progenitor cell features (7, 46). Cripto-1 (Teratocarcinoma-derived growth factor 1) is one of many common genes shared by both embryonic cells and cancer cells, and it contributes to early embryogenesis and cancer progression. Cripto-1 is associated with undifferentiated hESCs, but is hardly detected in normal human cells (47). Cripto-1 also has important functions in many human tumors, promoting cancer cell migration, proliferation, epithelial-mesenchymal transition (EMT), and angiogenesis. Cripto-1 expression is increased several-fold in human colon, gastric, pancreatic, lung, and breast carcinomas, and can be enriched from a subpopulation of cancer cells with stem-like characteristics, indicating that Cripto-1 is a CSC marker (48).
PODXL-1 (Podocalyxin-like protein 1) is rarely expressed in normal tissue cells (http://www.proteinatlas.org/), but is highly expressed on the surface of undifferentiated hESCs (49). PODXL-1 is also expressed in hematopoietic precursor cells and leukemia (50). PODXL-1 and BMI-1 are ubiquitously expressed in small cell lung carcinoma (SCLC) due to aberrant epigenetic changes, supporting the role of PODXL-1 as a potential CSC surface marker in SCLC (51). The ATP-binding cassette sub-family G member 2 (ABCG2/ABCP/MXR/BCRP) functions as a multidrug transporter in cancer drug resistance phenotypes. Although functional ABCG2 is highly expressed in undifferentiated hESCs (52, 53), some controversial data are also present (54). ABCG2 protein is rarely expressed in normal tissue cells, but some amount is detected in the intestine, seminal vesicle, and endothelial cells (http://www.proteinatlas.org/). Side population in human lung cancer cell lines and tumors displays elevated expression of ABCG2, and is enriched with stem-like cancer cells (55). CD24 is a heavily and variably glycosylated 35–60 kDa glycosyl phosphatidylinositol (GPI)-linked sialoprotein, rarely expressed in normal tissues except B cell precursors, neutrophils, neuronal cells, and certain epithelial cells (56). Although CD24 is expressed in human neuronal lineages, it is highly expressed in undifferentiated hESCs (36). Since CD24 is detected in a wide variety of cancers, it is proposed as a marker for CSCs (4, 20, 57). The combination of CD24 and CD44 is used to identify breast CSCs, since CD44+/CD24low cells exclusively retain tumorigenic activity and display stem cell-like properties (4). CD49f (integrin α6) is highly expressed in hESCs, and significantly decreases upon embryoid body formation (58). CD49f is weakly expressed in normal tissues, except in the rectum and urinary bladder (http://www.proteinatlas.org/). Knockdown of CD49f in hESCs downregulates PI3K/AKT signaling and upregulates the level of p53, inducing differentiation into three germ layers (58). CD49f+ cells are suggested as a HSC population because they are highly efficient in generating long-term multilineage grafts (59). Targeting CD49f in glioblastoma stem cells (GSCs) suppresses self-renewal, proliferation, and tumor formation capacity, providing evidence that GSCs express high levels of CD49f, which serve not only as an isolation marker, but also as an anti-glioblastoma target (60). Notch 2 plays important roles in various developmental processes via binding with their ligand, such as Jagged (61). Notch 2 is expressed on undifferentiated hESCs and upregulated during neural differentiation of hESCs (62). It is rarely expressed in normal tissues, except in subsets of cells in the large intestine and potential endocrine cells (http://www.proteinatlas.org/). The Notch family is important in maintaining human NSCs via control of proliferation (63). Notch 2 is used as a CSC marker in pancreas and lung (61). CD146 is one of the most well-known surface markers for human MSCs, and is also intermediately expressed on hESCs (36). Recent studies reveal that CD146 is a novel marker for highly tumorigenic cells, and is a potential therapeutic target in malignant rhabdoid tumor and primary sarcoma (64, 65).
CD10, CD117 and CD26 are drug target molecules approved by the Federal Food and Drug Administration (FDA). CD10 (membrane metallo-endopeptidase) is a membrane-bound metallopeptidase that inactivates various peptide hormones, including glucagon, substance P, oxytocin, and bradykinin (66). CD10+ hematopoietic progenitors are “common lymphoid progenitors”, which can differentiate into T, B, or natural killer cells (66). CD10 is intermediately expressed in undifferentiated hESCs, and is downregulated during neural differentiation of hESCs (36). CD10 is detected in human BM- and placenta-derived MSCs (67), but is rarely detected in normal tissue cells. However, it shows positivity in the luminal membrane in the small intestine, kidney, epididymis and prostate, and is also expressed in hepatocytes (http://www.proteinatlas.org/). Recent studies have shown that in head and neck squamous cell (HNSCC) and breast carcinomas, CD10 is a novel marker for therapeutic resistance and CSCs (68, 69). CD117 (c-Kit) is a receptor for stem cell factor, having very low expression in normal tissue cells (http://www.proteinatlas.org/). Subpopulations of hESCs (approximately 24%) are CD117-positive (36, 70). CD117 is involved in signal transduction of survival and self-renewal in various cells (71). Human epithelial ovarian cancer CD44+CD117+ cells possess properties of CSCs, exhibiting increased chemoresistance (72). CD26 (dipeptidyl peptidase-4, DPP4) is a surface serine DPP4 expressed on different cell types, and is involved in cleaving the amino-terminal dipeptide from some chemokines, including C-X-C motif chemokine ligand 12/stromal cell-derived factor-1 (CXCL12/SDF-1), which has important roles in HSC engraftment, mobilization and homing. CD26 is expressed in hPSCs and HSCs (73), is rarely expressed in various normal tissue cells, but it is highly expressed in kidney, small intestine, and male and female tissue cells (http://www.proteinatlas.org/). Studies have shown that CD26 is a CSC marker for leukemic stem cells and colorectal CSCs (74, 75).
CSC SURFACE MARKERS EXPRESSED ON ADULT STEM CELLS, BUT RARELY EXPRESSED ON NORMAL TISSUE CELLS
CSC surface markers expressed on adult stem cells but rarely expressed on normal human cells, are summarized in Table 2. CXCR4 (CXC chemokine receptor) was originally discovered as a coreceptor for the human immunodeficiency virus. CXCR4 is a potential cell surface marker for early embryonic NSCs, and is highly upregulated during the differentiation of hESCs to NSCs in vitro (76, 77). Extensive immunostaining of CXCR4 expression in normal human tissues is unavailable, but RNA expression analysis reveals that CXCR4 expression is rarely expressed in many normal tissue cells, except in lymphatic organs including BM (http://www.proteinatlas.org/). CXCR4 maintains a stem cell population in tamoxifen-resistant breast cancer cells, and has a critical role in the metastasis of breast cancer (78, 79). CD34, first detected on the cell surface of hematopoietic progenitor cells (80), is rarely expressed in normal tissue, except in hematopoietic progenitor/stem cells (81). The first evidence of CSC came from studies on human AML, in which leukemic stem cells were identified as a CD34+CD38− cell subpopulation (3). CD34 is also required for the isolation of TICs of squamous cell carcinomas (82).
CD271 (low-affinity nerve growth factor receptor) is specifically expressed in MSCs, and is rarely expressed in normal tissues, except in neural crest (83). CD271 has been suggested as a CSC surface marker in melanoma (13). However, it is not clear whether CD271 alone is sufficient to isolate melanoma CSCs, because some melanomas metastasize in NOD/SCID IL2Rγnull mice, irrespective of whether they arise from CD271− or CD271+ populations (84). CD13 (alanine aminopeptidase) may regulate the angiogenic signal, which is related to cell morphogenesis (85). CD13 is rarely expressed in normal tissues, but highly detected in renal tubules, intestine, exocrine pancreas, prostate, liver and gall bladder (http://www.proteinatlas.org/). It is a marker for MSCs isolated from various tissues (86), and is a suggested putative marker for liver CSCs (87). CD56 (neural cell adhesion molecule) is a membrane glycoprotein expressed on the surface of neurons, skeletal muscle and natural killer (NK) cells, and is a marker for MSCs and small-cell lung CSCs (88). CD56 is rarely expressed in normal tissue cells, except in the central and peripheral nerves (89). CD105 (endoglin) is a member of the transforming growth factor β (TGF) receptor family that binds TGF-β1 and -β3 on human endothelial cells (90). Known as a cell surface marker for MSCs (91), tumoral CD105 has been described as a new CSC marker of renal cell carcinomas (92). LGR5 (leucine-rich repeat-containing G-protein coupled receptor 5) is a member of G protein-coupled receptor, and is not expressed on hESCs (93). Discovered as an adult stem cell marker in the small intestine (94), LGR5 is considered as a biomarker of adult stem cells in multiple epithelia (95). It is rarely expressed in various normal tissue cells, although it is detected in the brain, gastrointestinal and female tissues (http://www.proteinatlas.org/). LGR5 is a CSC marker in mouse intestinal cancers (96), and has also been suggested as a CSC maker for human colon and colorectal cancers (97, 98).
CD114 (colony stimulating factor 3 receptor) is a cytokine receptor, and plays an important role in granulopoiesis during the inflammatory process. It is present on precursor cells in the BM, and initiates cell proliferation and differentiation into mature granulocytes and macrophages in response to stimulation by G-CSF (99). CD114 is rarely expressed in normal tissue cells, except in the brain, placenta, heart muscle, testis and skin (http://www.proteinatlas.org/). CD114 has been identified as a potential marker for CSCs in neural crest-derived tumors (100, 101). CD54 (intercellular adhesion molecule 1) is related to cell-cell interaction (102); it is not expressed in hESCs, but is weakly expressed in MSCs (103). Although rarely expressed in many normal tissue cells, CD54 is highly detected in the lung, kidney and lymphoid organs (http://www.proteinatlas.org/). CD54 is also used in the isolation of gastric CSCs (104). CXCR1 (chemokine receptor 1) and CXCR2 (chemokine receptor 2) are integral membrane proteins, which specifically bind and respond to cytokines of the CXC chemokine family. These receptors have a high binding affinity to IL8, and transduce signaling through a G-protein activated second messenger system (105). CXCR1 shows moderate membranous positivity in a subset of cells in the blood vessels (http://www.proteinatlas.org/). CXCR1 and CXCR2 are not only expressed on the surface of MSCs (106), but are also expressed on breast and pancreas CSCs (107, 108). TIM-3 (T-cell immunoglobulin domain and mucin domain-3) is an activation-induced inhibitory molecule involved in immune tolerance. TIM-3 is only expressed in a subset of lymphoid cells in normal tissues (http://www.proteinatlas.org/). TIM-3 is not expressed on the surface of normal HSCs, but is highly expressed on leukemic stem cells in most types of AML (109). CD55 (decay-accelerating factor) is not detected in normal tissues, except in the ovary, lung, placenta, adrenal gland and salivary gland (http://www.proteinatlas.org/). CD55 may be a novel surface marker for breast CSCs, since a small population of cells with CD55 expression is correlated to poor prognosis in breast cancer patients (110). DLL4 (delta-like ligand 4) serves as a ligand for Notch signaling and promotes stem cell self-renewal and vascular development. Notch signaling is necessary for maintaining intestinal progenitor and stem cells (111). Inhibiting human DLL4 in the tumors reduces the CSC frequency because of the inhibition of TIC frequency by the DLL4 blockade (112, 113).
CD20 and CD96 are expressed in B and T lineage cells, respectively, rather than in stem cells. The function of CD20 is not clear during B-cell development (114). CD20 is not expressed in normal tissues except in the lymphoid organs and skin (http://www.proteinatlas.org/). Even though CD20 expression is not distinguished between normal B-lymphocytes and malignant melanoma, CD20 is used as a marker for melanoma (115). Melanomas contain a CD20+ subpopulation of melanoma cells that contributes to melanoma heterogeneity and tumorigenesis (116). CD96 functions as a T cell-specific receptor (117); it is a transmembrane glycoprotein on human and mouse T and NK cells (118). CD96 is not expressed by a majority of cells in normal HSCs, but it is frequently expressed on leukemic stem cells (119, 120).
CSC SURFACE MARKERS EXPRESSED ON BOTH STEM CELLS AND NORMAL TISSUE CELLS
CSC surface markers that are expressed on both hESCs and normal tissue cells are summarized in Table 3. CD29 (integrin β1) is a cell adhesion molecule that mediates the interactions between adhesion molecules on adjacent cells and/or the extracellular matrix (121). It is highly expressed in both hESCs and MSCs, and is also ubiquitously expressed in various normal tissues (http://www.proteinatlas.org/) (36, 122). CD29 has been suggested as a cell surface marker for breast CSCs, because the CD29+CD49f+ cell population displays CSC activity in allograft-nude mice (123). CD9 (MRP-1) is a tetraspan family glycoprotein which modulates cellular adhesion, migration, and proliferation (124). CD9 is a cell surface marker of undifferentiated hESCs (70) and adipose-derived MSCs (125). CD9 protein expression is detected in a majority of normal tissues, but its expression is negative or weak in the gall bladder, liver, and lymphoid tissues (http://www.proteinatlas.org/). However, it is a useful marker to identify CSCs in human B-acute lymphoblastic leukemia cells (B-ALL), and is linked to several signaling pathways involved in regulating the CSC properties of B-ALL (126). CD166 (activated leukocyte cell adhesion molecule) is a type I membrane glycoprotein, which is a member of the immunoglobulin superfamily. Its expression is detected in many epithelial cells (http://www.proteinatlas.org/). CD166 is weakly expressed in undifferentiated hESCs (36), and is a marker for multipotential human adipose-derived stromal stem cells and intestinal stem cells (127, 128). Although CD166 is a marker of colorectal CSCs (129), and has also been identified as an “inert” CSC surface marker for non-small cell lung cancer (NSCLC), some controversial studies are also present (9, 130).
CSC surface markers expressed on both adult stem cells and normal tissues are summarized in Table 3. CD44, a hyaluronic acid receptor, is one of the most frequently studied markers in various cancer cells. CD44 is a multi-structural and multi-functional cell surface molecule, whose role is primarily governed by various post-translational modifications (131). The CD44 family has many isoforms that are expressed by alternative splicing of the pre-mRNA (131). CD44 standard (CD44s) is an 85–90-kDa transmembrane glycoprotein with basic 10 standard exons, whereas tissue-specific splice variants (CD44v1–10) consist of the standard set and combinations of the 10 variable exons. Its function is implicated in cell adhesion and migration, but a prominent role of CD44 is to bind to hyaluronic acid in the extracellular matrices. CD44 has been detected in human HSCs (132), MSCs (91), and adipose-derived stem cells (133), and has been extensively used in combination or with other putative markers, to isolate CSCs from various solid tumors (131, 134). CD44s is ubiquitously expressed in many normal cell types; however, its significance as a CSC marker may be limited (135). Recent studies suggest that conflicting results may be attributed to the expression of alternatively spliced variants. In this regard, CD44 variant 9 (CD44v9) has emerged as a novel marker of cancer stemness in a variety of solid tumors (136–139). Another variant, CD44v8–10, whose expression is low in normal tissues, also appears to be a cancer-specific marker for gastric CSCs (140). Other variants of CD44 have also been suggested as CSC markers in various cancers (131).
ABCB5 is an ATP-binding cassette transporter and a P-glycoprotein family member, principally expressed in physiological skins and human malignant melanomas. Expressed on normal liver and limbal stem cells (141), ABCB5 shows weak and moderate cytoplasmic staining in a majority of normal tissues (http://www.proteinatlas.org/). Because ABCB5+ subpopulations show self-renewal and differentiation capacity, ABCB5+ tumor cells have been suggested as melanoma-initiating cells (142). Notch 3 is important for maintaining human NSCs by controlling cell proliferation (63). Notch 3 protein is ubiquitously expressed in many normal tissue cells, including appendix, gallbladder and urinary bladder (http://www.proteinatlas.org/). However, Notch 3 is suggested as a CSC marker in pancreas and lung cancers (61). CD123 is an interleukin 3 specific subunit of a heterodimeric cytokine receptor, which is highly expressed in AML. IL-3 treatment increases the proliferation of AML (143). CD123 is ubiquitously expressed in normal human tissues (http://www.proteinatlas.org/). CD123 is a well-known target for the therapy of leukemia, since it is not expressed on normal HSCs but is highly expressed on leukemic stem cells (144).
SIMILARITIES BETWEEN CSC SURFACE MARKERS AND STEM CELL SURFACE MARKERS
Most of the 40 CSC surface markers described above are expressed on both CSCs and normal stem cells, suggesting that there is a high level of similarity between CSC surface markers and stem cell surface markers. The idea that cancers arise from residual embryonic tissues appeared in the early 19th century, and was formally published by Durante and Conheim as the “embryonic rest hypothesis of cancer development” (145, 146). This hypothesis states that remnants of embryonic tissue remain in adult organism, and cancers arise from these remaining embryonic cells (145, 146). Based on the hypothesis, adult stem cells would be leftover ESCs in adult tissues after birth. Interestingly, cancer and embryonic cells show similar histological morphologies and have many common features, such as reduced contact inhibition, high proliferation rate, tissue invasion ability, anaerobic metabolism, dedifferentiation status, evasion of immune destruction, secretion of angiogenic factors, and expression of embryonic genes. In the 1970s, researchers found that rabbits immunized with mouse embryos create antibodies that cross-reacted with 72 different mouse tumors (147). Antibodies produced against human embryos also recognize a variety of human tumors, including lung, skin, bronchial, renal, colonic, hepatic and breast (148). Immunization with embryonic cells shows similar results; immunized mice make antibodies that recognize both tumors and embryos (149, 150). These findings led to the idea that animals or humans vaccinated with embryonic tissues, might trigger an immune response against cancer and prevent cancer progression. Interestingly, vaccination with embryonic cells does not show cross-reactivity with various adult tissues, except skin (145). These and subsequent studies provide the concept about “oncofetal antigens” that are typically present only during embryonic and fetal development, but are found in cancerous tissues in adults (150).
The relationship between cancer and embryonic tissues/cells has attracted a lot of attention after the development of hESCs and CSCs. Li et al. (2009) reported that vaccination of mice with hESCs results in strong immune responses against colon carcinoma cells without autoimmune responses (151). Mice vaccinated with mouse ESCs induce obvious anti-tumor immunity, which protects them from the formation and development of lung cancer (152). Mice vaccinated with mouse ESC, cocultured with STO fibroblasts expressing granulocyte macrophage-CSF, also suppress lung cancer development induced by carcinogen administration and chronic pulmonary inflammation (153). These findings suggest the concept that ESCs have oncofetal antigens, which are also present on cancer cells. The concept about oncofetal antigens being expended to adult stem cells is because adult stem cells are considered as leftover ESCs in adult tissues. Global analysis of gene expression networks further suggest that core pluripotency genes, such as NANOG, OCT4, SOX2, and MYC, are primary gene sets shared by both ESCs and cancers (154, 155). Almost half of the genes that are upregulated as a result of genomic alterations in hESCs, are also closely linked to the expression of cancer genes (156, 157).
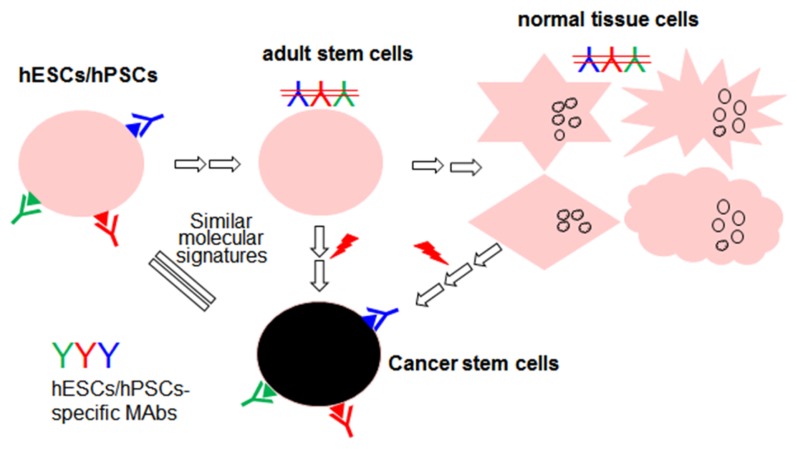
The basic similarities between hESCs and CSCs are that both have pluripotency or multipotency, and express the same oncofetal antigens, such as SSEA-3, SSEA-4, TRA-1-60, TRA-1-81, EpCAM, and Cripto. When injected into immunodeficient mice, both are capable of generating teratoma tumors. Both ESCs and CSCs also have other common characteristics, such as high proliferation potential, indefinite self-renewal, high nuclear to cytoplasmic ratio, and increased expression of anti-apoptotic genes (158). The activation of ESC-like gene expression in adult cells is considered to endow self-renewal to CSCs (159). Analysis of signaling molecules in CSCs reveals that CSCs also contain common signaling, such as Wnt-, Notch-, Sonic hedgehog- and Fibroblast growth factor-2-signaling that regulate the hESCs as well (158, 159). Thus, hESCs and CSC have high potential to have the same cell surface markers (Fig. 1). Until now, approximately 40 CSC surface markers have been identified (Table 1–3), of which 35 markers (approximately 88%) are also expressed on normal embryonic or adult stem cells, thus demonstrating the basic similarities between CSCs and normal stem cells.
Fig. 1.
Proposed strategy for the identification of novel CSC surface markers by using hESCs/hPSCs-specific MAbs. Shown is an overall scheme showing a normal cellular hierarchy of embryonic stem cells (hESCs/hPSCs), adult stem cells, and differentaited normal tissue cells. Cancer stem cells can be derived from hESCs/hPSCs, adult stem cells and normal tissues cells. MAbs specific to undifferentiated hESCs/hPSCs, but not to adult stem cells and normal tissue cells, will be attractive tools to discover novel CSC surface markers, since the antigens recognized by the MAbs is highly likely to be present on CSCs, but not on normal tissue cells, in adults.
CONCLUSION AND FUTURE PERSPECTIVES
We summarize 40 CSC surface markers in this review, although some known surface markers are not accurate and need further studies. To better isolate specific CSCs from various heterogeneous tumors, more functional markers are needed. To isolate functional CSCs, there is a need to search for more specific surface markers, or use multiple surface markers in combination. We classify the currently known 40 CSC surface markers into 3 different categories, depending on their expression on hESCs, adult stem cells, and normal tissue cells. Of the 40 CSC markers, approximately 83% (33 out of 40 CSC markers) are rarely expressed on normal tissue cells (Table 1–3). We believe that the CSC surface markers have potential usefulness as therapeutic targets against CSCs due to their low cross reactivity to normal tissue cells. As expected, 9 of these are already approved as drug target molecules by FDA. Seven CSC surface markers are ubiquitously expressed on normal tissue cells (Table 3), which may lead to side effects when they are targeted for elimination. For example, CD44s is ubiquitously expressed in many normal cell types, which may cause side effects in CD44s-targeted therapies. According to recent studies, however, the variant CD44v8–10 is a bona fide CSC-specific marker (136–140). Interestingly, the variant CD44v8–10 is weakly expressed in normal tissues, suggesting that the ambiguity regarding functional aspects of CD44 in CSC identity largely attributes to the expression of alternatively spliced variants. In this regard, functional epitopes on some CSC surface markers should be extensively defined for specific detection of CSCs in future studies. Most of CSCs were isolated by using monoclonal or polyclonal antibodies. Recent studies reveal that examination of the general protein expression is not sufficient to distinguish specific CSCs from heterogeneous populations (38, 136–140). In the case of CD133, the expression of AC133 epitope on CD133 protein is only restricted to undifferentiated stem cells (38), suggesting that CSC-specific epitopes are necessary to analyze functional CSC activity. CSC-specific epitopes may also be present or absent, depending on the CD44 splice variant, which may generate some conflicting data in CD44-expressed cancers. Many commercially available antibodies are generated against synthetic peptides from target proteins instead of real tertiary and native forms of target proteins, and the use of the antibodies may lead to misinterpretation about the functional CSCs. Therefore, the development of many antibodies recognizing CSC-specific functional epitopes is necessary to overcome the current ambiguity of some CSC surface markers.
Identification of a novel CSC marker is challenging, since CSCs are generally rare in tumor tissues (1). Therefore, identifying novel surface markers on normal stem cells will be an alternative approach to find novel surface markers on CSCs. However, since adult stem cells are very rare in mature tissues, isolating these cells from an adult tissue is challenging, and culture methods to expand up to their required numbers is another task. Furthermore, when surface markers on adult stem cells are utilized as therapeutic targets against CSCs, there may be a possibility to eliminate normal adult stem cells and impair the normal process of tissue regeneration. Contrary to adult stem cells, hESCs or hPSCs are relatively easy to grow in culture. Among the 40 CSC markers, 21 CSC surface markers (approximately 53%) are expressed on hESCs as well. Many of these surface markers originate from surface markers on undifferentiated hESCs. These surface markers may be potential candidates as CSC markers, since surface markers of undifferentiated hESCs have oncofetal characteristics and are rarely expressed on normal tissue cells (Table 1 and Fig. 1). By using a modified decoy immunization strategy, we generated 37 MAbs which bind to undifferentiated hESCs, but weakly or not at all to differentiated hESCs or differentiated primary cells (160). By using the MAbs, we found that cell surface-expressed E1B-AP5 and BAP31 are novel surface markers on undifferentiated hESCs (161, 162). Interestingly, cell surface E1B-AP5 and BAP31 are also expressed on some cancer cell lines, while they are not expressed on normal differentiated cells (161, 162), suggesting that these types of hESC surface markers deserve to be studied as potential CSC surface markers. Thus, finding novel surface markers on undifferentiated hESCs is an attractive alternative to screen novel CSC surface markers. A proposed strategy for the identification of novel CSC surface markers by using hESC/hPSC-specific MAbs is presented in Fig. 1.
ACKNOWLEDGEMENTS
We thank Profs Yonghyun Kim and Hee Chul Lee for their comments and careful proofreading. This study was supported by the National Research Foundation of Korea (2016-903249 and 2016-008610).
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicting financial interests.
REFERENCES
- 1.Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8:755–768. doi: 10.1038/nrc2499. [DOI] [PubMed] [Google Scholar]
- 2.Tirino V, Desiderio V, Paino F, et al. Cancer stem cells in solid tumors: an overview and new approaches for their isolation and characterization. FASEB J. 2013;27:13–24. doi: 10.1096/fj.12-218222. [DOI] [PubMed] [Google Scholar]
- 3.Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3:730–737. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 4.Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A. 2003;100:3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh SK, Hawkins C, Clarke ID, et al. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 6.Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ. Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res. 2005;65:10946–10951. doi: 10.1158/0008-5472.CAN-05-2018. [DOI] [PubMed] [Google Scholar]
- 7.Li C, Heidt DG, Dalerba P, et al. Identification of pancreatic cancer stem cells. Cancer Res. 2007;67:1030–1037. doi: 10.1158/0008-5472.CAN-06-2030. [DOI] [PubMed] [Google Scholar]
- 8.O’Brien CA, Pollett A, Gallinger S, Dick JE. A human colon cancer cell capable of initiating tumour growth in immunodeficient mice. Nature. 2007;445:106–110. doi: 10.1038/nature05372. [DOI] [PubMed] [Google Scholar]
- 9.Zhang WC, Shyh-Chang N, Yang H, et al. Glycine decarboxylase activity drives non-small cell lung cancer tumor-initiating cells and tumorigenesis. Cell. 2012;148:259–272. doi: 10.1016/j.cell.2011.11.050. [DOI] [PubMed] [Google Scholar]
- 10.Takaishi S, Okumura T, Tu S, et al. Identification of gastric cancer stem cells using the cell surface marker CD44. Stem Cells. 2009;27:1006–1020. doi: 10.1002/stem.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curley MD, Therrien VA, Cummings CL, et al. CD133 expression defines a tumor initiating cell population in primary human ovarian cancer. Stem Cells. 2009;27:2875–2883. doi: 10.1002/stem.236. [DOI] [PubMed] [Google Scholar]
- 12.Terris B, Cavard C, Perret C. EpCAM, a new marker for cancer stem cells in hepatocellular carcinoma. J Hepatol. 2010;52:280–281. doi: 10.1016/j.jhep.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 13.Boiko AD, Razorenova OV, van de Rijn M, et al. Human melanoma-initiating cells express neural crest nerve growth factor receptor CD271. Nature. 2010;466:133–137. doi: 10.1038/nature09161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bach P, Abel T, Hoffmann C, et al. Specific elimination of CD133+ tumor cells with targeted oncolytic measles virus. Cancer Res. 2013;73:865–874. doi: 10.1158/0008-5472.CAN-12-2221. [DOI] [PubMed] [Google Scholar]
- 15.Kaiser J. The cancer stem cell gamble. Science. 2015;347:226–229. doi: 10.1126/science.347.6219.226. [DOI] [PubMed] [Google Scholar]
- 16.Waldron NN, Barsky SH, Dougherty PR, Vallera DA. A bispecific EpCAM/CD133-targeted toxin is effective against carcinoma. Target Oncol. 2014;9:239–249. doi: 10.1007/s11523-013-0290-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmohl JU, Vallera DA. CD133, Selectively Targeting the Root of Cancer. Toxins (Basel) 2016;8:165. doi: 10.3390/toxins8060165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou BB, Zhang H, Damelin M, Geles KG, Grindley JC, Dirks PB. Tumour-initiating cells: challenges and opportunities for anticancer drug discovery. Nat Rev Drug Discov. 2009;8:806–823. doi: 10.1038/nrd2137. [DOI] [PubMed] [Google Scholar]
- 19.Xia P. Surface markers of cancer stem cells in solid tumors. Curr Stem Cell Res Ther. 2014;9:102–111. doi: 10.2174/1574888X09666131217003709. [DOI] [PubMed] [Google Scholar]
- 20.Islam F, Gopalan V, Smith RA, Lam AK. Translational potential of cancer stem cells: A review of the detection of cancer stem cells and their roles in cancer recurrence and cancer treatment. Exp Cell Res. 2015;335:135–147. doi: 10.1016/j.yexcr.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 21.Zhao W, Ji X, Zhang F, Li L, Ma L. Embryonic stem cell markers. Molecules. 2012;17:6196–6236. doi: 10.3390/molecules17066196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomson JA, Itskovitz-Eldor J, Shapiro SS, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–1147. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 23.Kuroda Y, Kitada M, Wakao S, et al. Unique multipotent cells in adult human mesenchymal cell populations. Proc Natl Acad Sci U S A. 2010;107:8639–8643. doi: 10.1073/pnas.0911647107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gang EJ, Bosnakovski D, Figueiredo CA, Visser JW, Perlingeiro RC. SSEA-4 identifies mesenchymal stem cells from bone marrow. Blood. 2007;109:1743–1751. doi: 10.1182/blood-2005-11-010504. [DOI] [PubMed] [Google Scholar]
- 25.Sandstedt J, Jonsson M, Vukusic K, et al. SSEA-4+ CD34− cells in the adult human heart show the molecular characteristics of a novel cardiomyocyte progenitor population. Cells Tissues Organs. 2014;199:103–116. doi: 10.1159/000363225. [DOI] [PubMed] [Google Scholar]
- 26.Chang WW, Lee CH, Lee P, et al. Expression of Globo H and SSEA3 in breast cancer stem cells and the involvement of fucosyl transferases 1 and 2 in Globo H synthesis. Proc Natl Acad Sci U S A. 2008;105:11667–11672. doi: 10.1073/pnas.0804979105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schopperle WM, DeWolf WC. The TRA-1-60 and TRA-181 human pluripotent stem cell markers are expressed on podocalyxin in embryonal carcinoma. Stem Cells. 2007;25:723–730. doi: 10.1634/stemcells.2005-0597. [DOI] [PubMed] [Google Scholar]
- 28.Corominas-Faja B, Cufi S, Oliveras-Ferraros C, et al. Nuclear reprogramming of luminal-like breast cancer cells generates Sox2-overexpressing cancer stem-like cellular states harboring transcriptional activation of the mTOR pathway. Cell Cycle. 2013;12:3109–3124. doi: 10.4161/cc.26173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rajasekhar VK, Studer L, Gerald W, Socci ND, Scher HI. Tumour-initiating stem-like cells in human prostate cancer exhibit increased NF-kappaB signalling. Nat Commun. 2011;2:162. doi: 10.1038/ncomms1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mao XG, Zhang X, Xue XY, et al. Brain Tumor Stem-Like Cells Identified by Neural Stem Cell Marker CD15. Transl Oncol. 2009;2:247–257. doi: 10.1593/tlo.09136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liebert M, Jaffe R, Taylor RJ, Ballou BT, Solter D, Hakala TR. Detection of SSEA-1 on human renal tumors. Cancer. 1987;59:1404–1408. doi: 10.1002/1097-0142(19870415)59:8<1404::AID-CNCR2820590804>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 32.Miyake M, Zenita K, Tanaka O, Okada Y, Kannagi R. Stage-specific expression of SSEA-1-related antigens in the developing lung of human embryos and its relation to the distribution of these antigens in lung cancers. Cancer Res. 1988;48:7150–7158. [PubMed] [Google Scholar]
- 33.Grosse-Gehling P, Fargeas CA, Dittfeld C, et al. CD133 as a biomarker for putative cancer stem cells in solid tumours: limitations, problems and challenges. J Pathol. 2013;229:355–378. doi: 10.1002/path.4086. [DOI] [PubMed] [Google Scholar]
- 34.Irollo E, Pirozzi G. CD133: to be or not to be, is this the real question? Am J Transl Res. 2013;5:563–581. [PMC free article] [PubMed] [Google Scholar]
- 35.Yin AH, Miraglia S, Zanjani ED, et al. AC133, a novel marker for human hematopoietic stem and progenitor cells. Blood. 1997;90:5002–5012. [PubMed] [Google Scholar]
- 36.Sundberg M, Jansson L, Ketolainen J, et al. CD marker expression profiles of human embryonic stem cells and their neural derivatives, determined using flow-cytometric analysis, reveal a novel CD marker for exclusion of pluripotent stem cells. Stem Cell Res. 2009;2:113–124. doi: 10.1016/j.scr.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 37.Uchida N, Buck DW, He D, et al. Direct isolation of human central nervous system stem cells. Proc Natl Acad Sci U S A. 2000;97:14720–14725. doi: 10.1073/pnas.97.26.14720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kemper K, Sprick MR, de Bree M, et al. The AC133 epitope, but not the CD133 protein, is lost upon cancer stem cell differentiation. Cancer Res. 2010;70:719–729. doi: 10.1158/0008-5472.CAN-09-1820. [DOI] [PubMed] [Google Scholar]
- 39.Dennis JE, Esterly K, Awadallah A, Parrish CR, Poynter GM, Goltry KL. Clinical-scale expansion of a mixed population of bone-marrow-derived stem and progenitor cells for potential use in bone-tissue regeneration. Stem Cells. 2007;25:2575–2582. doi: 10.1634/stemcells.2007-0204. [DOI] [PubMed] [Google Scholar]
- 40.International Stem Cell I. Adewumi O, Aflatoonian B, et al. Characterization of human embryonic stem cell lines by the International Stem Cell Initiative. Nat Biotechnol. 2007;25:803–816. doi: 10.1038/nbt1318. [DOI] [PubMed] [Google Scholar]
- 41.Buishand FO, Arkesteijn GJ, Feenstra LR, et al. Identification of CD90 as Putative Cancer Stem Cell Marker and Therapeutic Target in Insulinomas. Stem Cells Dev. 2016;25:826–835. doi: 10.1089/scd.2016.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.He J, Liu Y, Zhu T, et al. CD90 is identified as a candidate marker for cancer stem cells in primary high-grade gliomas using tissue microarrays. Mol Cell Proteomics. 2012;11 doi: 10.1074/mcp.M111.010744. M111 010744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang ZF, Ho DW, Ng MN, et al. Significance of CD90+ cancer stem cells in human liver cancer. Cancer Cell. 2008;13:153–166. doi: 10.1016/j.ccr.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 44.Ng VY, Ang SN, Chan JX, Choo AB. Characterization of epithelial cell adhesion molecule as a surface marker on undifferentiated human embryonic stem cells. Stem Cells. 2010;28:29–35. doi: 10.1002/stem.221. [DOI] [PubMed] [Google Scholar]
- 45.Patriarca C, Macchi RM, Marschner AK, Mellstedt H. Epithelial cell adhesion molecule expression (CD326) in cancer: a short review. Cancer Treat Rev. 2012;38:68–75. doi: 10.1016/j.ctrv.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 46.Yamashita T, Ji J, Budhu A, et al. EpCAM-positive hepatocellular carcinoma cells are tumor-initiating cells with stem/progenitor cell features. Gastroenterology. 2009;136:1012–1024. doi: 10.1053/j.gastro.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bianco C, Rangel MC, Castro NP, et al. Role of Cripto-1 in stem cell maintenance and malignant progression. Am J Pathol. 2010;177:532–540. doi: 10.2353/ajpath.2010.100102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bianco C, Salomon DS. Targeting the embryonic gene Cripto-1 in cancer and beyond. Expert Opin Ther Pat. 2010;20:1739–1749. doi: 10.1517/13543776.2010.530659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choo AB, Tan HL, Ang SN, et al. Selection against undifferentiated human embryonic stem cells by a cytotoxic antibody recognizing podocalyxin-like protein-1. Stem Cells. 2008;26:1454–1463. doi: 10.1634/stemcells.2007-0576. [DOI] [PubMed] [Google Scholar]
- 50.Kelley TW, Huntsman D, McNagny KM, Roskelley CD, Hsi ED. Podocalyxin: a marker of blasts in acute leukemia. Am J Clin Pathol. 2005;124:134–142. doi: 10.1309/7BHLAHHU0N4MHT7Q. [DOI] [PubMed] [Google Scholar]
- 51.Koch LK, Zhou H, Ellinger J, et al. Stem cell marker expression in small cell lung carcinoma and developing lung tissue. Hum Pathol. 2008;39:1597–1605. doi: 10.1016/j.humpath.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 52.Padmanabhan R, Chen KG, Gottesman MM. Lost in Translation: Regulation of ABCG2 Expression in Human Embryonic Stem Cells. J Stem Cell Res Ther. 2014;4:24230. doi: 10.4172/2157-7633.1000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Apati A, Orban TI, Varga N, et al. High level functional expression of the ABCG2 multidrug transporter in undifferentiated human embryonic stem cells. Biochim Biophys Acta. 2008;1778:2700–2709. doi: 10.1016/j.bbamem.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 54.Sarkadi B, Orban TI, Szakacs G, et al. Evaluation of ABCG2 expression in human embryonic stem cells: crossing the same river twice? Stem Cells. 2010;28:174–176. doi: 10.1002/stem.262. [DOI] [PubMed] [Google Scholar]
- 55.Ho MM, Ng AV, Lam S, Hung JY. Side population in human lung cancer cell lines and tumors is enriched with stem-like cancer cells. Cancer Res. 2007;67:4827–4833. doi: 10.1158/0008-5472.CAN-06-3557. [DOI] [PubMed] [Google Scholar]
- 56.Kristiansen G, Sammar M, Altevogt P. Tumour biological aspects of CD24, a mucin-like adhesion molecule. J Mol Histol. 2004;35:255–262. doi: 10.1023/B:HIJO.0000032357.16261.c5. [DOI] [PubMed] [Google Scholar]
- 57.Zhang C, Li C, He F, Cai Y, Yang H. Identification of CD44+CD24+ gastric cancer stem cells. J Cancer Res Clin Oncol. 2011;137:1679–1686. doi: 10.1007/s00432-011-1038-5. [DOI] [PubMed] [Google Scholar]
- 58.Yu KR, Yang SR, Jung JW, et al. CD49f enhances multipotency and maintains stemness through the direct regulation of OCT4 and SOX2. Stem Cells. 2012;30:876–887. doi: 10.1002/stem.1052. [DOI] [PubMed] [Google Scholar]
- 59.Notta F, Doulatov S, Laurenti E, Poeppl A, Jurisica I, Dick JE. Isolation of single human hematopoietic stem cells capable of long-term multilineage engraftment. Science. 2011;333:218–221. doi: 10.1126/science.1201219. [DOI] [PubMed] [Google Scholar]
- 60.Lathia JD, Gallagher J, Heddleston JM, et al. Integrin alpha 6 regulates glioblastoma stem cells. Cell Stem Cell. 2010;6:421–432. doi: 10.1016/j.stem.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yen WC, Fischer MM, Axelrod F, et al. Targeting notch signaling with a notch2/notch3 antagonist (tarextumab) inhibits tumor growth and decreases tumor-initiating cell frequency. Clin Cancer Res. 2015;21:2084–2095. doi: 10.1158/1078-0432.CCR-14-2808. [DOI] [PubMed] [Google Scholar]
- 62.Fox V, Gokhale PJ, Walsh JR, Matin M, Jones M, Andrews PW. Cell-cell signaling through NOTCH regulates human embryonic stem cell proliferation. Stem Cells. 2008;26:715–723. doi: 10.1634/stemcells.2007-0368. [DOI] [PubMed] [Google Scholar]
- 63.Imayoshi I, Sakamoto M, Yamaguchi M, Mori K, Kageyama R. Essential Roles of Notch Signaling in Maintenance of Neural Stem Cells in Developing and Adult Brains. J Neurosci. 2010;30:3489–3498. doi: 10.1523/JNEUROSCI.4987-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nodomi S, Umeda K, Saida S, et al. CD146 is a novel marker for highly tumorigenic cells and a potential therapeutic target in malignant rhabdoid tumor. Oncogene. 2016;35:5317–5327. doi: 10.1038/onc.2016.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wei Q, Tang YJ, Voisin V, et al. Identification of CD146 as a marker enriched for tumor-propagating capacity reveals targetable pathways in primary human sarcoma. Oncotarget. 2015;6:40283–40294. doi: 10.18632/oncotarget.5375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Galy A, Travis M, Cen D, Chen B. Human T, B, natural killer, and dendritic cells arise from a common bone marrow progenitor cell subset. Immunity. 1995;3:459–473. doi: 10.1016/1074-7613(95)90175-2. [DOI] [PubMed] [Google Scholar]
- 67.Mariotti E, Mirabelli P, Abate G, et al. Comparative characteristics of mesenchymal stem cells from human bone marrow and placenta: CD10, CD49d, and CD56 make a difference. Stem Cells Dev. 2008;17:1039–1041. doi: 10.1089/scd.2008.0212. [DOI] [PubMed] [Google Scholar]
- 68.Fukusumi T, Ishii H, Konno M, et al. CD10 as a novel marker of therapeutic resistance and cancer stem cells in head and neck squamous cell carcinoma. Br J Cancer. 2014;111:506–514. doi: 10.1038/bjc.2014.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Maguer-Satta V, Chapellier M, Delay E, Bachelard-Cascales E. CD10: a tool to crack the role of stem cells in breast cancer. Proc Natl Acad Sci U S A. 2011;108:E1264. doi: 10.1073/pnas.1116567108. author reply E1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carpenter MK, Rosler ES, Fisk GJ, et al. Properties of four human embryonic stem cell lines maintained in a feeder-free culture system. Dev Dyn. 2004;229:243–258. doi: 10.1002/dvdy.10431. [DOI] [PubMed] [Google Scholar]
- 71.Miettinen M, Lasota J. KIT (CD117): a review on expression in normal and neoplastic tissues, and mutations and their clinicopathologic correlation. Appl Immunohistochem Mol Morphol. 2005;13:205–220. doi: 10.1097/01.pai.0000173054.83414.22. [DOI] [PubMed] [Google Scholar]
- 72.Chen J, Wang J, Chen D, et al. Evaluation of characteristics of CD44+CD117+ ovarian cancer stem cells in three dimensional basement membrane extract scaffold versus two dimensional monocultures. BMC Cell Biol. 2013;14:7. doi: 10.1186/1471-2121-14-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ou X, O’Leary HA, Broxmeyer HE. Implications of DPP4 modification of proteins that regulate stem/progenitor and more mature cell types. Blood. 2013;122:161–169. doi: 10.1182/blood-2013-02-487470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Herrmann H, Sadovnik I, Cerny-Reiterer S, et al. Dipeptidylpeptidase IV (CD26) defines leukemic stem cells (LSC) in chronic myeloid leukemia. Blood. 2014;123:3951–3962. doi: 10.1182/blood-2013-10-536078. [DOI] [PubMed] [Google Scholar]
- 75.Pang R, Law WL, Chu AC, et al. A subpopulation of CD26+ cancer stem cells with metastatic capacity in human colorectal cancer. Cell Stem Cell. 2010;6:603–615. doi: 10.1016/j.stem.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 76.Zhang L, Hua Q, Tang K, Shi C, Xie X, Zhang R. CXCR4 activation promotes differentiation of human embryonic stem cells to neural stem cells. Neuroscience. 2016;337:88–97. doi: 10.1016/j.neuroscience.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 77.Li M, Chang CJ, Lathia JD, et al. Chemokine receptor CXCR4 signaling modulates the growth factor-induced cell cycle of self-renewing and multipotent neural progenitor cells. Glia. 2011;59:108–118. doi: 10.1002/glia.21080. [DOI] [PubMed] [Google Scholar]
- 78.Mukherjee D, Zhao J. The Role of chemokine receptor CXCR4 in breast cancer metastasis. Am J Cancer Res. 2013;3:46–57. [PMC free article] [PubMed] [Google Scholar]
- 79.Dubrovska A, Hartung A, Bouchez LC, et al. CXCR4 activation maintains a stem cell population in tamoxifen-resistant breast cancer cells through AhR signalling. Br J Cancer. 2012;107:43–52. doi: 10.1038/bjc.2012.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Civin CI, Strauss LC, Brovall C, Fackler MJ, Schwartz JF, Shaper JH. Antigenic analysis of hematopoiesis. III. A hematopoietic progenitor cell surface antigen defined by a monoclonal antibody raised against KG-1a cells. J Immunol. 1984;133:157–165. [PubMed] [Google Scholar]
- 81.Sutherland HJ, Lansdorp PM, Henkelman DH, Eaves AC, Eaves CJ. Functional characterization of individual human hematopoietic stem cells cultured at limiting dilution on supportive marrow stromal layers. Proc Natl Acad Sci U S A. 1990;87:3584–3588. doi: 10.1073/pnas.87.9.3584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schober M, Fuchs E. Tumor-initiating stem cells of squamous cell carcinomas and their control by TGF-beta and integrin/focal adhesion kinase (FAK) signaling. Proc Natl Acad Sci U S A. 2011;108:10544–10549. doi: 10.1073/pnas.1107807108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Buhring HJ, Battula VL, Treml S, Schewe B, Kanz L, Vogel W. Novel markers for the prospective isolation of human MSC. Ann NY Acad Sci. 2007;1106:262–271. doi: 10.1196/annals.1392.000. [DOI] [PubMed] [Google Scholar]
- 84.Quintana E, Shackleton M, Foster HR, et al. Phenotypic heterogeneity among tumorigenic melanoma cells from patients that is reversible and not hierarchically organized. Cancer Cell. 2010;18:510–523. doi: 10.1016/j.ccr.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bhagwat SV, Lahdenranta J, Giordano R, Arap W, Pasqualini R, Shapiro LH. CD13/APN is activated by angiogenic signals and is essential for capillary tube formation. Blood. 2001;97:652–659. doi: 10.1182/blood.V97.3.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rahman MM, Subramani J, Ghosh M, et al. CD13 promotes mesenchymal stem cell-mediated regeneration of ischemic muscle. Front Physiol. 2014;4:402. doi: 10.3389/fphys.2013.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Haraguchi N, Ishii H, Mimori K, et al. CD13 is a therapeutic target in human liver cancer stem cells. J Clin Invest. 2010;120:3326–3339. doi: 10.1172/JCI42550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Salcido CD, Larochelle A, Taylor BJ, Dunbar CE, Varticovski L. Molecular characterisation of side population cells with cancer stem cell-like characteristics in small-cell lung cancer. Br J Cancer. 2010;102:1636–1644. doi: 10.1038/sj.bjc.6605668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shimojima M, Nishimura Y, Miyazawa T, Kato K, Tohya Y, Akashi H. CD56 expression in feline lymphoid cells. J Vet Med Sci. 2003;65:769–773. doi: 10.1292/jvms.65.769. [DOI] [PubMed] [Google Scholar]
- 90.Altomonte M, Montagner R, Fonsatti E, et al. Expression and structural features of endoglin (CD105), a transforming growth factor beta1 and beta3 binding protein, in human melanoma. Br J Cancer. 1996;74:1586–1591. doi: 10.1038/bjc.1996.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Maleki M, Ghanbarvand F, Reza Behvarz M, Ejtemaei M, Ghadirkhomi E. Comparison of mesenchymal stem cell markers in multiple human adult stem cells. Int J Stem Cells. 2014;7:118–126. doi: 10.15283/ijsc.2014.7.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Saroufim A, Messai Y, Hasmim M, et al. Tumoral CD105 is a novel independent prognostic marker for prognosis in clear-cell renal cell carcinoma. Br J Cancer. 2014;110:1778–1784. doi: 10.1038/bjc.2014.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Forster R, Chiba K, Schaeffer L, et al. Human intestinal tissue with adult stem cell properties derived from pluripotent stem cells. Stem Cell Rep. 2014;2:838–852. doi: 10.1016/j.stemcr.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Barker N, van Es JH, Kuipers J, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–1007. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 95.Barker N, Tan S, Clevers H. Lgr proteins in epithelial stem cell biology. Development. 2013;140:2484–2494. doi: 10.1242/dev.083113. [DOI] [PubMed] [Google Scholar]
- 96.Barker N, Ridgway RA, van Es JH, et al. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457:608–611. doi: 10.1038/nature07602. [DOI] [PubMed] [Google Scholar]
- 97.Kemper K, Prasetyanti PR, De Lau W, Rodermond H, Clevers H, Medema JP. Monoclonal antibodies against Lgr5 identify human colorectal cancer stem cells. Stem Cells. 2012;30:2378–2386. doi: 10.1002/stem.1233. [DOI] [PubMed] [Google Scholar]
- 98.Hirsch D, Barker N, McNeil N, et al. LGR5 positivity defines stem-like cells in colorectal cancer. Carcinogenesis. 2014;35:849–858. doi: 10.1093/carcin/bgt377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ward AC. The role of the granulocyte colony-stimulating factor receptor (G-CSF-R) in disease. Front Biosci. 2007;12:608–618. doi: 10.2741/2086. [DOI] [PubMed] [Google Scholar]
- 100.Zage PE, Whittle SB, Shohet JM. CD114: A New Member of the Neural Crest-Derived Cancer Stem Cell Marker Family. J Cell Biochem. 2017;118:221–231. doi: 10.1002/jcb.25656. [DOI] [PubMed] [Google Scholar]
- 101.Hsu DM, Agarwal S, Benham A, et al. G-CSF receptor positive neuroblastoma subpopulations are enriched in chemotherapy-resistant or relapsed tumors and are highly tumorigenic. Cancer Res. 2013;73:4134–4146. doi: 10.1158/0008-5472.CAN-12-4056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tohma S, Ramberg JE, Lipsky PE. Expression and distribution of CD11a/CD18 and CD54 during human T cell-B cell interactions. J Leukoc Biol. 1992;52:97–103. doi: 10.1002/jlb.52.1.97. [DOI] [PubMed] [Google Scholar]
- 103.Amaral AT, Manara MC, Berghuis D, et al. Characterization of human mesenchymal stem cells from ewing sarcoma patients. Pathogenetic implications. PLoS One. 2014;9:e85814. doi: 10.1371/journal.pone.0085814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen T, Yang K, Yu J, et al. Identification and expansion of cancer stem cells in tumor tissues and peripheral blood derived from gastric adenocarcinoma patients. Cell Res. 2012;22:248–258. doi: 10.1038/cr.2011.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wilson S, Wilkinson G, Milligan G. The CXCR1 and CXCR2 receptors form constitutive homo- and heterodimers selectively and with equal apparent affinities. J Biol Chem. 2005;280:28663–28674. doi: 10.1074/jbc.M413475200. [DOI] [PubMed] [Google Scholar]
- 106.Ringe J, Strassburg S, Neumann K, et al. Towards in situ tissue repair: human mesenchymal stem cells express chemokine receptors CXCR1, CXCR2 and CCR2, and migrate upon stimulation with CXCL8 but not CCL2. J Cell Biochem. 2007;101:135–146. doi: 10.1002/jcb.21172. [DOI] [PubMed] [Google Scholar]
- 107.Singh JK, Farnie G, Bundred NJ, et al. Targeting CXCR1/2 significantly reduces breast cancer stem cell activity and increases the efficacy of inhibiting HER2 via HER2-dependent and -independent mechanisms. Clin Cancer Res. 2013;19:643–656. doi: 10.1158/1078-0432.CCR-12-1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chen L, Fan J, Chen H, et al. The IL-8/CXCR1 axis is associated with cancer stem cell-like properties and correlates with clinical prognosis in human pancreatic cancer cases. Sci Rep. 2014;4:5911. doi: 10.1038/srep05911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kikushige Y, Shima T, Takayanagi S, et al. TIM-3 is a promising target to selectively kill acute myeloid leukemia stem cells. Cell Stem Cell. 2010;7:708–717. doi: 10.1016/j.stem.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 110.Ikeda J, Morii E, Liu Y, et al. Prognostic significance of CD55 expression in breast cancer. Clin Cancer Res. 2008;14:4780–4786. doi: 10.1158/1078-0432.CCR-07-1844. [DOI] [PubMed] [Google Scholar]
- 111.Pellegrinet L, Rodilla V, Liu Z, et al. Dll1- and dll4-mediated notch signaling are required for homeostasis of intestinal stem cells. Gastroenterology. 2011;140:1230–1240. e1231–1237. doi: 10.1053/j.gastro.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hoey T, Yen WC, Axelrod F, et al. DLL4 blockade inhibits tumor growth and reduces tumor-initiating cell frequency. Cell Stem Cell. 2009;5:168–177. doi: 10.1016/j.stem.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 113.Fischer M, Yen WC, Kapoun AM, et al. Anti-DLL4 inhibits growth and reduces tumor-initiating cell frequency in colorectal tumors with oncogenic KRAS mutations. Cancer Res. 2011;71:1520–1525. doi: 10.1158/0008-5472.CAN-10-2817. [DOI] [PubMed] [Google Scholar]
- 114.O’Keefe TL, Williams GT, Davies SL, Neuberger MS. Mice carrying a CD20 gene disruption. Immunogenetics. 1998;48:125–132. doi: 10.1007/s002510050412. [DOI] [PubMed] [Google Scholar]
- 115.Smith MR. Rituximab (monoclonal anti-CD20 antibody): mechanisms of action and resistance. Oncogene. 2003;22:7359–7368. doi: 10.1038/sj.onc.1206939. [DOI] [PubMed] [Google Scholar]
- 116.Fang D, Nguyen TK, Leishear K, et al. A tumorigenic subpopulation with stem cell properties in melanomas. Cancer Res. 2005;65:9328–9337. doi: 10.1158/0008-5472.CAN-05-1343. [DOI] [PubMed] [Google Scholar]
- 117.Wang PL, O’Farrell S, Clayberger C, Krensky AM. Identification and molecular cloning of tactile. A novel human T cell activation antigen that is a member of the Ig gene superfamily. J Immunol. 1992;148:2600–2608. [PubMed] [Google Scholar]
- 118.Martinet L, Smyth MJ. Balancing natural killer cell activation through paired receptors. Nat Rev Immunol. 2015;15:243–254. doi: 10.1038/nri3799. [DOI] [PubMed] [Google Scholar]
- 119.Garg S, Madkaikar M, Ghosh K. Investigating cell surface markers on normal hematopoietic stem cells in three different niche conditions. Int J Stem Cells. 2013;6:129–133. doi: 10.15283/ijsc.2013.6.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hosen N, Park CY, Tatsumi N, et al. CD96 is a leukemic stem cell-specific marker in human acute myeloid leukemia. Proc Natl Acad Sci U S A. 2007;104:11008–11013. doi: 10.1073/pnas.0704271104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Goodfellow PJ, Nevanlinna HA, Gorman P, Sheer D, Lam G, Goodfellow PN. Assignment of the gene encoding the beta-subunit of the human fibronectin receptor (beta-FNR) to chromosome 10p11.2. Ann Hum Genet. 1989;53:15–22. doi: 10.1111/j.1469-1809.1989.tb01118.x. [DOI] [PubMed] [Google Scholar]
- 122.Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 123.Vassilopoulos A, Chisholm C, Lahusen T, Zheng H, Deng CX. A critical role of CD29 and CD49f in mediating metastasis for cancer-initiating cells isolated from a Brca1-associated mouse model of breast cancer. Oncogene. 2014;33:5477–5482. doi: 10.1038/onc.2013.516. [DOI] [PubMed] [Google Scholar]
- 124.Zoller M. Tetraspanins: push and pull in suppressing and promoting metastasis. Nat Rev Cancer. 2009;9:40–55. doi: 10.1038/nrc2543. [DOI] [PubMed] [Google Scholar]
- 125.Kim YJ, Yu JM, Joo HJ, et al. Role of CD9 in proliferation and proangiogenic action of human adipose-derived mesenchymal stem cells. Pflugers Arch. 2007;455:283–296. doi: 10.1007/s00424-007-0285-4. [DOI] [PubMed] [Google Scholar]
- 126.Yamazaki H, Xu CW, Naito M, et al. Regulation of cancer stem cell properties by CD9 in human B-acute lymphoblastic leukemia. Biochem Biophys Res Commun. 2011;409:14–21. doi: 10.1016/j.bbrc.2011.04.098. [DOI] [PubMed] [Google Scholar]
- 127.Zannettino AC, Paton S, Arthur A, et al. Multipotential human adipose-derived stromal stem cells exhibit a perivascular phenotype in vitro and in vivo. J Cell Physiol. 2008;214:413–421. doi: 10.1002/jcp.21210. [DOI] [PubMed] [Google Scholar]
- 128.Wang F, Scoville D, He XC, et al. Isolation and characterization of intestinal stem cells based on surface marker combinations and colony-formation assay. Gastroenterology. 2013;145:383–395. e381–321. doi: 10.1053/j.gastro.2013.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Levin TG, Powell AE, Davies PS, et al. Characterization of the intestinal cancer stem cell marker CD166 in the human and mouse gastrointestinal tract. Gastroenterology. 2010;139:2072–2082 e2075. doi: 10.1053/j.gastro.2010.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tachezy M, Zander H, Wolters-Eisfeld G, et al. Activated leukocyte cell adhesion molecule (CD166): an “inert” cancer stem cell marker for non-small cell lung cancer? Stem Cells. 2014;32:1429–1436. doi: 10.1002/stem.1665. [DOI] [PubMed] [Google Scholar]
- 131.Thapa R, Wilson GD. The Importance of CD44 as a Stem Cell Biomarker and Therapeutic Target in Cancer. Stem Cells Int. 2016;2016;2087204 doi: 10.1155/2016/2087204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lapidot T, Dar A, Kollet O. How do stem cells find their way home? Blood. 2005;106:1901–1910. doi: 10.1182/blood-2005-04-1417. [DOI] [PubMed] [Google Scholar]
- 133.Zuk PA, Zhu M, Ashjian P, et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13:4279–4295. doi: 10.1091/mbc.E02-02-0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zoller M. CD44: can a cancer-initiating cell profit from an abundantly expressed molecule? Nat Rev Cancer. 2011;11:254–267. doi: 10.1038/nrc3023. [DOI] [PubMed] [Google Scholar]
- 135.Jaggupilli A, Elkord E. Significance of CD44 and CD24 as cancer stem cell markers: an enduring ambiguity. Clin Dev Immunol. 2012;2012;708036 doi: 10.1155/2012/708036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nagano O, Okazaki S, Saya H. Redox regulation in stem-like cancer cells by CD44 variant isoforms. Oncogene. 2013;32:5191–5198. doi: 10.1038/onc.2012.638. [DOI] [PubMed] [Google Scholar]
- 137.Hirata K, Suzuki H, Imaeda H, et al. CD44 variant 9 expression in primary early gastric cancer as a predictive marker for recurrence. Br J Cancer. 2013;109:379–386. doi: 10.1038/bjc.2013.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yoshikawa M, Tsuchihashi K, Ishimoto T, et al. xCT inhibition depletes CD44v-expressing tumor cells that are resistant to EGFR-targeted therapy in head and neck squamous cell carcinoma. Cancer Res. 2013;73:1855–1866. doi: 10.1158/0008-5472.CAN-12-3609-T. [DOI] [PubMed] [Google Scholar]
- 139.Ishimoto T, Nagano O, Yae T, et al. CD44 variant regulates redox status in cancer cells by stabilizing the xCT subunit of system xc(−) and thereby promotes tumor growth. Cancer Cell. 2011;19:387–400. doi: 10.1016/j.ccr.2011.01.038. [DOI] [PubMed] [Google Scholar]
- 140.Lau WM, Teng E, Chong HS, et al. CD44v8-10 is a cancer-specific marker for gastric cancer stem cells. Cancer Res. 2014;74:2630–2641. doi: 10.1158/0008-5472.CAN-13-2309. [DOI] [PubMed] [Google Scholar]
- 141.Ksander BR, Kolovou PE, Wilson BJ, et al. ABCB5 is a limbal stem cell gene required for corneal development and repair. Nature. 2014;511:353–357. doi: 10.1038/nature13426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Schatton T, Murphy GF, Frank NY, et al. Identification of cells initiating human melanomas. Nature. 2008;451:345–349. doi: 10.1038/nature06489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Miyauchi J, Kelleher CA, Yang YC, et al. The effects of three recombinant growth factors, IL-3, GM-CSF, and G-CSF, on the blast cells of acute myeloblastic leukemia maintained in short-term suspension culture. Blood. 1987;70:657–663. [PubMed] [Google Scholar]
- 144.Sadras T, Perugini M, Kok CH, et al. Interleukin-3-mediated regulation of beta-catenin in myeloid transformation and acute myeloid leukemia. J Leukoc Biol. 2014;96:83–91. doi: 10.1189/jlb.2AB1013-559R. [DOI] [PubMed] [Google Scholar]
- 145.Brewer BG, Mitchell RA, Harandi A, Eaton JW. Embryonic vaccines against cancer: an early history. Exp Mol Pathol. 2009;86:192–197. doi: 10.1016/j.yexmp.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 146.Sell S. On the stem cell origin of cancer. Am J Pathol. 2010;176:2584–2494. doi: 10.2353/ajpath.2010.091064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Stonehill EH, Bendich A. Retrogenetic expression: the reappearance of embryonal antigens in cancer cells. Nature. 1970;228:370–372. doi: 10.1038/228370a0. [DOI] [PubMed] [Google Scholar]
- 148.Klavins JV, Mesa-Tejada R, Weiss M. Human carcinoma antigens cross reacting with anti-embryonic antibodies. Nat New Biol. 1971;234:153–154. doi: 10.1038/newbio234153a0. [DOI] [PubMed] [Google Scholar]
- 149.Bendich A, Borenfreund E, Stonehill EH. Protection of adult mice against tumor challenge by immunization with irradiated adult skin or embryo cells. J Immunol. 1973;111:284–285. [PubMed] [Google Scholar]
- 150.Adinolfi M, Lessof MH. Cancer, oncogenes and oncofetal antigens. Q J Med. 1985;54:193–204. [PubMed] [Google Scholar]
- 151.Li Y, Zeng H, Xu RH, Liu B, Li Z. Vaccination with human pluripotent stem cells generates a broad spectrum of immunological and clinical responses against colon cancer. Stem Cells. 2009;27:3103–3111. doi: 10.1002/stem.234. [DOI] [PubMed] [Google Scholar]
- 152.Dong W, Du J, Shen H, et al. Administration of embryonic stem cells generates effective antitumor immunity in mice with minor and heavy tumor load. Cancer Immunol Immunother. 2010;59:1697–1705. doi: 10.1007/s00262-010-0899-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Yaddanapudi K, Mitchell RA, Putty K, et al. Vaccination with embryonic stem cells protects against lung cancer: is a broad-spectrum prophylactic vaccine against cancer possible? PLoS One. 2012;7:e42289. doi: 10.1371/journal.pone.0042289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kim J, Woo AJ, Chu J, et al. A Myc network accounts for similarities between embryonic stem and cancer cell transcription programs. Cell. 2010;143:313–324. doi: 10.1016/j.cell.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ben-Porath I, Thomson MW, Carey VJ, et al. An embryonic stem cell-like gene expression signature in poorly differentiated aggressive human tumors. Nat Genet. 2008;40:499–507. doi: 10.1038/ng.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Narva E, Autio R, Rahkonen N, et al. High-resolution DNA analysis of human embryonic stem cell lines reveals culture-induced copy number changes and loss of heterozygosity. Nat Biotechnol. 2010;28:371–377. doi: 10.1038/nbt.1615. [DOI] [PubMed] [Google Scholar]
- 157.Lee AS, Tang C, Rao MS, Weissman IL, Wu JC. Tumorigenicity as a clinical hurdle for pluripotent stem cell therapies. Nat Med. 2013;19:998–1004. doi: 10.1038/nm.3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Dvorak P, Dvorakova D, Hampl A. Fibroblast growth factor signaling in embryonic and cancer stem cells. FEBS Lett. 2006;580:2869–2874. doi: 10.1016/j.febslet.2006.01.095. [DOI] [PubMed] [Google Scholar]
- 159.Clarke MF, Fuller M. Stem cells and cancer: two faces of eve. Cell. 2006;124:1111–1115. doi: 10.1016/j.cell.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 160.Choi HS, Kim H, Won A, et al. Development of a decoy immunization strategy to identify cell-surface molecules expressed on undifferentiated human embryonic stem cells. Cell Tissue Res. 2008;333:197–206. doi: 10.1007/s00441-008-0632-6. [DOI] [PubMed] [Google Scholar]
- 161.Choi HS, Kim WT, Kim H, et al. Identification and characterization of adenovirus early region 1B-associated protein 5 as a surface marker on undifferentiated human embryonic stem cells. Stem Cells Dev. 2011;20:609–620. doi: 10.1089/scd.2010.0265. [DOI] [PubMed] [Google Scholar]
- 162.Kim WT, Seo Choi H, Min Lee H, Jang YJ, Ryu CJ. B-cell receptor-associated protein 31 regulates human embryonic stem cell adhesion, stemness, and survival via control of epithelial cell adhesion molecule. Stem Cells. 2014;32:2626–2641. doi: 10.1002/stem.1765. [DOI] [PubMed] [Google Scholar]
- 163.Medof ME, Lublin DM, Holers VM, et al. Cloning and characterization of cDNAs encoding the complete sequence of decay-accelerating factor of human complement. Proc Natl Acad Sci U S A. 1987;84:2007–2011. doi: 10.1073/pnas.84.7.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Stashenko P, Nadler LM, Hardy R, Schlossman SF. Characterization of a human B lymphocyte-specific antigen. J Immunol. 1980;125:1678–1685. [PubMed] [Google Scholar]
- 165.Reff ME, Carner K, Chambers KS, et al. Depletion of B cells in vivo by a chimeric mouse human monoclonal antibody to CD20. Blood. 1994;83:435–445. [PubMed] [Google Scholar]
- 166.Gramatzki M, Ludwig WD, Burger R, et al. Antibodies TC-12 (“unique”) and TH-111 (CD96) characterize T-cell acute lymphoblastic leukemia and a subgroup of acute myeloid leukemia. Exp Hematol. 1998;26:1209–1214. [PubMed] [Google Scholar]