Abstract
Intestinal stomas are necessary for several colon and rectal conditions and represent a major change in the new ostomate's daily life. Though dehydration is the most frequent etiology requiring readmission, irritant contact dermatitis and a host of other peristomal skin conditions are more common complications for ostomates. Wound, ostomy, and continence nurses are invaluable resources to both ostomy patients and providers. A few simple interventions can prevent or resolve most common peristomal complications. Good stoma care is possible in a resource-poor environment.
Keywords: ileostomy, colostomy, peristomal skin complications, enterostomal therapy, ostomy
Intestinal diversion is necessary for several colorectal conditions, including inflammatory bowel disease, trauma, diverticular disease, and malignancy. Whether temporary or permanent, proper perioperative care and education is essential for acclimation to life with a stoma. Enhanced stoma education involving wound, ostomy, and continence (WOC) nurses, as well as postdischarge telephone calls can minimize stoma complications and readmission and maximize patient satisfaction. 1 Unfortunately, these intensive pathways are not always feasible ubiquitously, particularly in limited-resource settings. Providers must be equipped with a knowledge foundation regarding common postoperative peristomal complications to act as the first responder to ostomates in crisis.
Basic Tenets of Postoperative Stoma Care
In the early postoperative period, three stages of ileostomy adaptation have been described. Initial function, with production of thin bilious effluent, occurs within the first two postoperative days. Output then peaks, stabilizes, and steadily declines as effluent becomes more formed when solid food is introduced. 2 3 The final stage lasts over several weeks. Metabolic adaptations promote renal sodium conservation, leading to decreased urine output total and decreased body water. 4 The ideal mature ileostomy produces 500 to 1,200 mL of oatmeal-like effluent daily. Unlike small bowel stomas, colostomies tend to produce semisolid fecal effluent shortly after the resumption of oral intake, although colostomy adaptation also occurs to a small degree.
Prior to inpatient discharge, new small bowel ostomates require specific diet instructions intended to maintain salt and water balance and to slow progression of food boluses through the intestinal track. Ideally, food is well salted and thoroughly chewed, and divided into five to six small portions daily with deliberate rest for 15 to 30 minutes after meals. Patients are advised to avoid simple carbohydrates. Fluid and solid intake should be separated. Several over-the-counter oral hydration solutions (Ceralyte, Cera Products, Columbus, GA; DripDrop ORS, DripDrop Inc., San Francisco, CA) are available for patients who have persistently high ileostomy output. In limited-access areas, low calorie electrolyte drinks (G2, PepsiCo; Pedialyte, Abbott Nutrition) or homemade World Health Organization oral rehydration salts ( http://apps.who.int/medicinedocs/en/d/Js4950e/2.4.html#Js4950e.2.4 ) can be effectively substituted to sustain electrolyte balance and hydration.
Upon discharge, the ileostomate must be competent in emptying his/her appliance and recording ileostomy output during the adaptation phase. In the era of accelerated care paths, the new ostomate is often ready for discharge during the period of peak effluent volume. Readmission rates following ileostomy formation can approach 17% for dehydration alone. 5 6 Patients require dehydration-specific counseling to minimize this sequela. Patients must vigilantly monitor for signs and symptoms of dehydration, including nausea, oliguria, concentrated urine, dry mouth, thirst, and lightheadedness. Ostomates should be provided a contact number to alert providers of dehydration symptoms or if ileostomy outputs exceed 1,200 mL daily. 7 It is not unusual for patients to learn that decreased ostomy output can be a pleasant side effect of anorexia, and patients must not limit oral intake as a long-term fecal management strategy as this will exacerbate dehydration.
Basic Stoma Care
An ostomy pouching system consists of the odor proof pouch, the skin barrier, and water resistant tape. The pouch is available in several lengths and materials. A pouch with an integrated closure (built onto the bottom of the pouch) prevents issues such as loss of the closure piece. The skin barrier is a flexible hydrocolloid adhesive that is either precut or cut-to-fit at the skin stoma junction. A snug fit prevents the stoma effluent from making contact with the skin. The hydrocolloid adhesive erodes with moisture; pouch wear time is generally 4 days to prevent chemical irritation from leakage. The cut-to-fit skin barrier allows precise adjustments as postoperative edema recedes and the required aperture size evolves. In some settings accessory products, such as skin barrier paste or skin barrier rings, to enhance the seal are applied around the stoma.
Patient Perspective: Goals of Stoma Self-Care
A new ostomate initially needs to acquire the basic skills of emptying and changing the pouching system. Caregivers and loved ones are also encouraged to apprentice during teaching sessions. The technique initially taught to the patient should closely replicate how the patient will eventually empty the pouch following hospital discharge. The end of the pouch is held cephalad to the stoma, and opened and directed into the toilet between the patient's legs to allow stool drainage. Once the pouch is emptied, the end is cleansed with toilet paper and resealed. Since water and detergents soften pouch adhesive and shorten wear time, washing the pouch is not advised. Since a heavy, over-filled pouch can pull away from the skin, the pouch may need to be emptied six or more times daily. Therefore, emptying the pouch is a critical skill to learn before discharge. Ideally, an initial demonstration of changing and applying the pouching system is provided the first day after surgery. Pain, apprehension, and preoccupation with viewing the stoma at first may limit knowledge recall after the first lesson, but by the second lesson, the patient ideally participates in and can demonstrate all steps.
At home, the newly discharged ostomate applies stoma care techniques learned during inpatient teaching sessions. Home care nursing should coincide with pouch changes to help bridge toward independent self-care. The patient should be discharged with extra pouching systems with complete specific manufacturer ordering information including product numbers, web site URLs, and telephone numbers. Advise the patient to check with his/her insurance provider about reimbursement criteria. For example, home care provided through Medicare Part B currently includes ostomy supplies as part of the service, but regional and payer, variations may exist.
Wound, Ostomy, and Continence Nurse Perspective
Resources
Guidelines from the American Society of Colon and Rectal Surgeons recommend that ostomy education has pre- and postoperative components involving a specialized provider such as a WOC nurse, when possible. 8 Several studies have shown that WOC nurse education is highly valued by patients and improves postoperative psychosocial adjustment to the stoma. 9 10 Frequently occurring early postoperative complications such as pouch leakage and skin excoriation can be successfully treated with early WOC nurse care. 11 12 To this end, the Wound, Ostomy and Continence Nurses Society maintains an online search tool to pair patients and providers with a local WOC nurse. 13
The American College of Surgeons (ACS) has developed the Ostomy Home Skills Program that includes an educational digital video disc and booklet, sample pouches, a measurement guide, and a practice model to promote problem solving and self-care. 14 These kits are used as pre- and postoperative adjuncts to increase patient comprehension and skill acquisition. The kits are currently free for ACS members. Videos and print materials from the kits are available through the ACS and YouTube web sites.
Most ostomy product manufacturers provide patient educational materials online and offer preoperative stoma site marking kits, hands-on skill kits, product samples, and complementary support services. In addition to online educational materials, the United Ostomy Associations of America hosts a moderated discussion board and publishes a quarterly publication that includes articles on living with a stoma and keeps patients up to date on new products. Most regions have one or more stoma support groups that conduct monthly educational meetings; contact information for new attendees should be kept on hand in every provider's office. 15
Stoma Site Selection
Stoma site selection and marking performed by a WOC nurse, whenever feasible, and meticulous construction of a protruding stoma are two controllable factors both known to decrease the development of problematic stomas and peristomal skin complications. 8 16 Principles of stoma site selection and creation are covered in depth elsewhere in this volume, but the authors stress their key importance in allowing for stoma self-care and preventing skin sequela.
Stoma Care in a Limited-Resource Setting
A variety of specialized stoma supplies are available, but all may not be necessary. In facilities where stomas are infrequently created, a “universal” cut-to-fit extended wear drainable clear pouching system with integrated closure accommodating stomas 22 to 64 mm in diameter can accommodate most ostomates while minimizing stocking costs and confusion. An essential accessory item to stock is a skin barrier ring that can be stretched and molded. This ring can be custom fit around the stoma or cut into small pieces to fill in irregular contours. Two may be stacked together to create a convex surface if the skin around the stoma is retracted or if the stoma lumen is not centrally located. These two items will allow for successful pouching in a large majority of patients with fecal stomas.
Incidence, Risk Factors, and Management of Common Peristomal Skin Conditions
Up to 20 to 70% of ostomates will experience stoma-related complications, and perhaps even higher rates are possible when skin complications are considered. 17 18 19 20 Peristomal skin complications occur in 25 to 43% of patients with ileostomies and 7 to 20% of those with colostomies, and are the focus of this article. 11 18 21 22 23 Parastomal hernia, necrosis, retraction, stenosis, prolapse, peristomal abscess, varices, pyoderma gangrenosum, high-output enterostomy, and fistula will be discussed elsewhere in this issue of Clinics in Colon and Rectal Surgery .
Obesity and emergency surgery are frequently cited risk factors for complicated enterostomy. Patients with a high body mass index are at risk for stoma retraction and necrosis, parastomal hernia, and a poorly sited stoma. 19 20 Surgeon experience and specialization are also implicating factors for stoma-related complications, particularly in the emergent setting. 24 25 American Society of Anesthesiologists (ASA) grade is a risk factor for stoma-related morbidity; however, it is also suggested that higher ASA grade may influence the surgeon to create a stoma. 24 Diabetes, smoking, and age are also associated with postoperative stoma complications. 19 Enterostomy type (i.e., ileostomy vs. colostomy) influences type of complication, with colostomies having higher rates of parastomal hernia and ileostomies having higher rates of peristomal skin irritation. 18 High rates of stoma complications are noted in inflammatory bowel disease, particularly in Crohn's disease, where patients may ultimately require surgical stoma revision as definitive treatment. 26 27
Peristomal Skin Complications
The overarching treatment strategy for most peristomal skin complications following correct diagnosis is to adjust the pouching system and add topical therapy to promote healing. To protect the skin and facilitate healing, the patient must be able to maintain a proper seal between the pouch appliance and skin. Undoubtedly, sustaining an adequate pouch seal can be one of the most difficult and frustrating aspects for new ostomates when managing skin complications. Frequent and conscientious follow-up and multidisciplinary care is required between the patient, surgeon, home health, and stoma care professional. Peristomal skin complications arising from poor siting or improperly constructed stomas that prove refractory to expert stoma care may rarely require surgical revision or resiting.
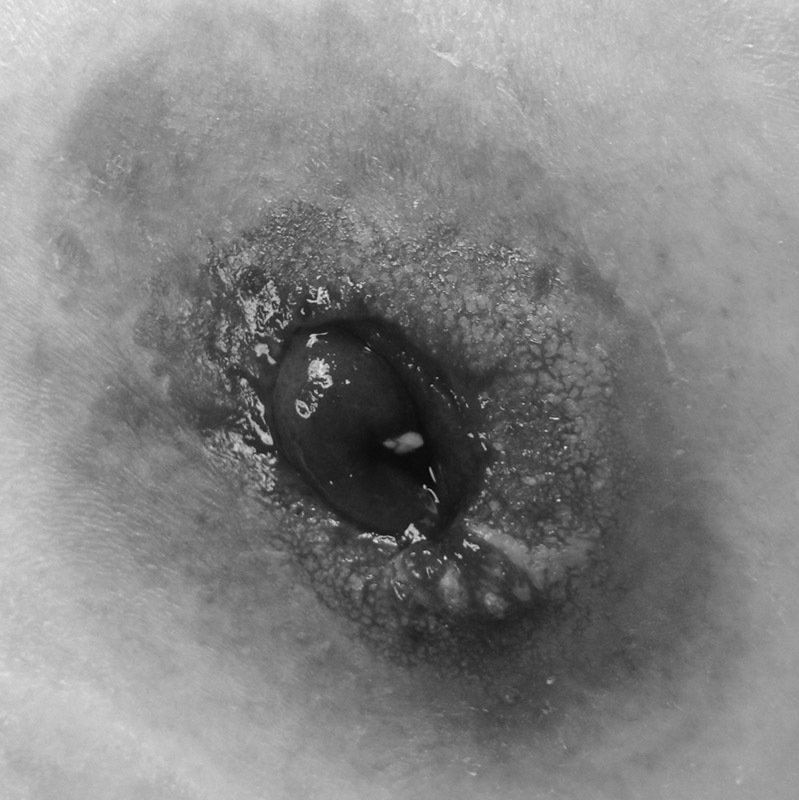
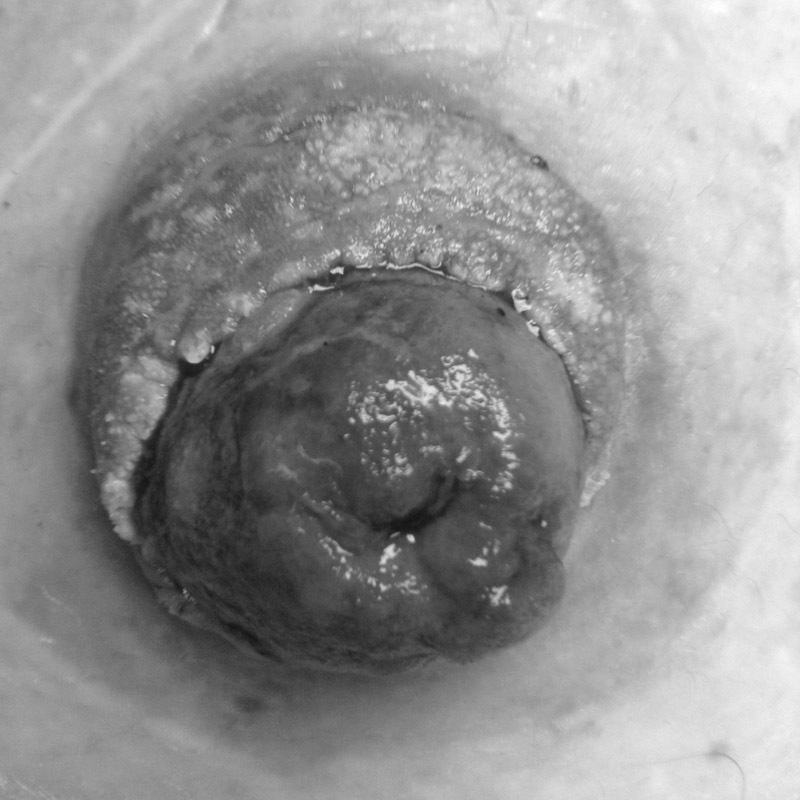
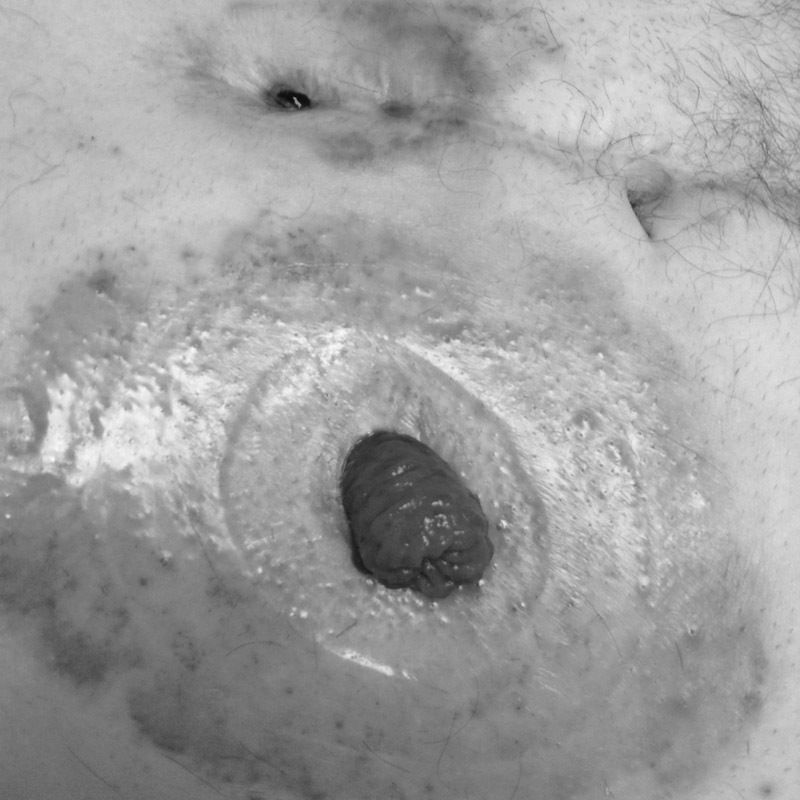
Mucocutaneous Separation
Mucocutaneous separation (MCS) is a common early complication after stoma formation, and the incidence is likely underreported in the literature. Mucocutaneous suture disruption can trigger wound breakdown and appliance leakage in the early postoperative period ( Figs. 1 and 2 ). MCS may arise from a combination of excessive stoma tension, infection, or impaired wound healing. MCS can intimidate patients and nonstoma care providers and can delay patient pouching proficiency. Local wound care measures coupled with fastidious pouching can lead to complete healing in most cases of MCS. The mucocutaneous cleft is irrigated of any fibrinous slough with warm saline. Skin barrier powder is then used to fill in the MCS defect before applying the pouching system. The aforementioned steps will prevent fecal contamination of the wound base prior to applying pouching system adhesive. 28 With early detection and appropriate wound care, most MCS cases will heal. Circumferential MCS is treated in a similar fashion, but presents special challenges and may predispose to eventual retraction and stenosis.
Fig. 1.
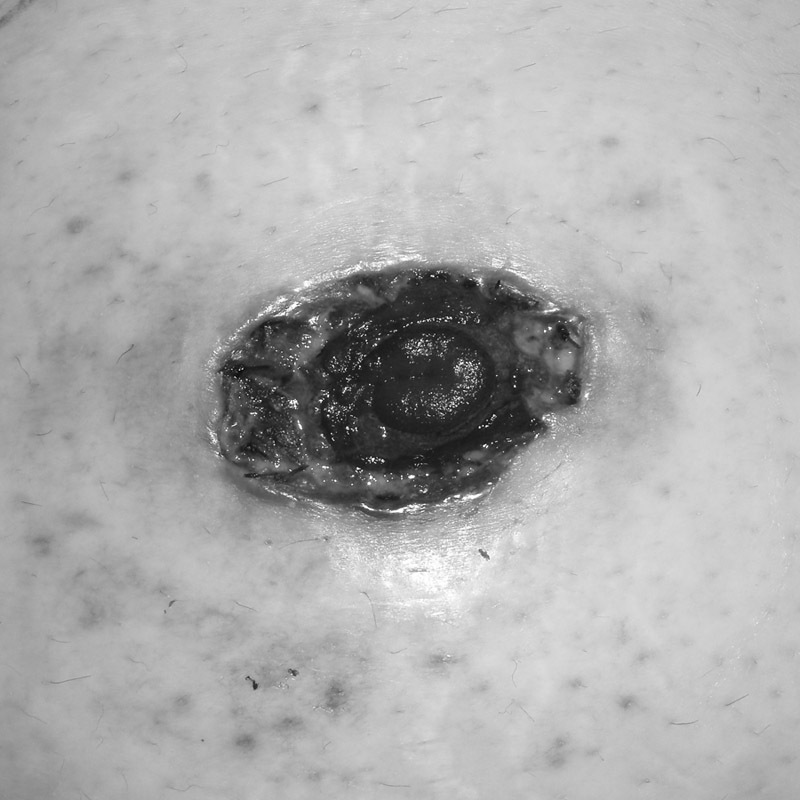
Clean mucocutaneous separation.
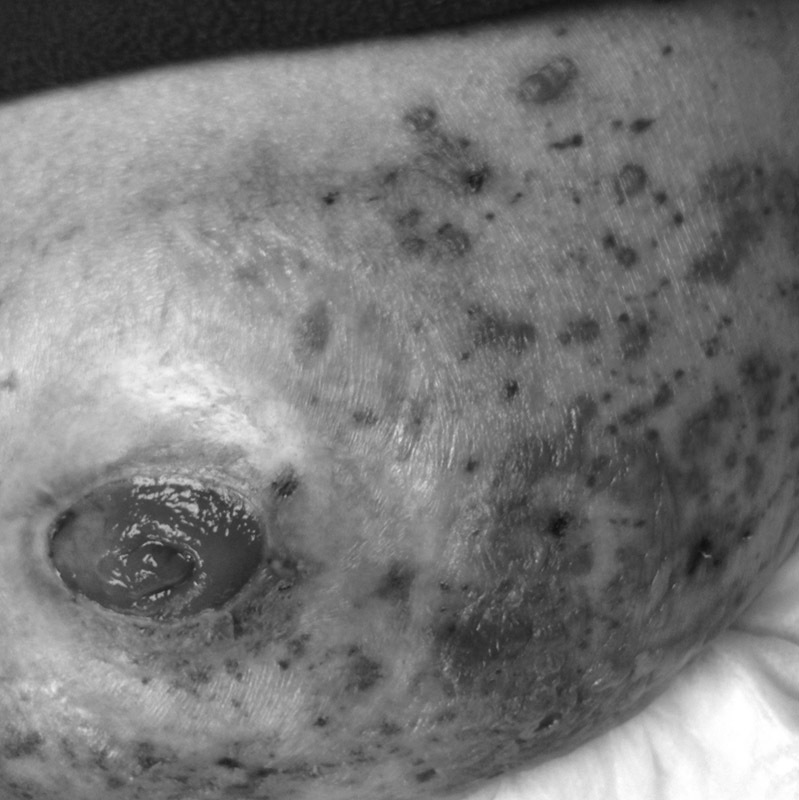
Fig. 2.

Mucocutaneous separation in a retracted stoma leading to leaking and irritant contact dermatitis.
Suture Sinus and Granulation Tissue
Granulomas are red, moist, lesions at the mucocutaneous junction representing an immunological response to retained suture material ( Fig. 3 ). 29 Granulomas are typically tender, friable, and weep serous fluid, which may impair complete pouch sealing due to moisture at the pouch–skin interface. Granulomas may also cause chronic moisture changes of the epidermis (see the Pseudoverrucous Epitheliomatous Hyperplasia section). If present, each granuloma is probed and all residual suture material is removed. Reactive hypertrophic granulation tissue typically responds well to topical silver nitrate. Surgical suture removal is necessary when office-based treatment is not tolerated or successful.
Fig. 3.

Suture granuloma.
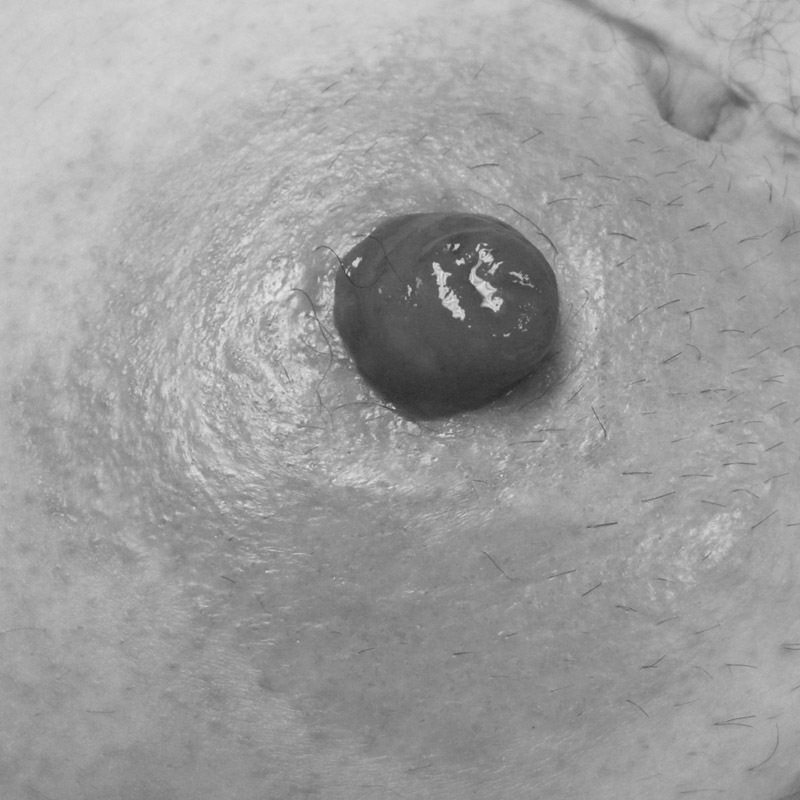
Leakage/Chemical Irritation
Chemical dermatitis is a common problem that affects up to 34% of ileostomy patients. 21 The slightly acidic nature of skin (pH: 4.0–5.9) contributes to its normal barrier function. 30 Ileostomies continually produce watery, alkaline, effluent rich in proteolytic enzymes that irritate exposed peristomal skin. Chronic leakage leads to loss of skin integrity and maceration ( Fig. 4 ), which can quickly progress to painful peristomal ulceration ( Figs. 5 and 6 ). The distribution of chemical dermatitis corresponds to the topography of leakage. Poor stoma siting, inadequate stoma protrusion, and improperly sized pouching systems all can lead to leakage-associated dermatitis. Moreover, pouch appliances worn in excess of 5 days can lead to disintegration of the protective hydrocolloid adhesive wafer leading to “silent leakage.” Leakage can quickly trigger chemical irritation within of hours of exposure. Leakage-associated dermatitis is best prevented by creating a properly protruding stoma (1–2 cm for colostomy, 2–3 cm for ileostomy) located on a flat area of the abdomen with a properly fit pouching system. After identifying and correcting the leakage (typically with filler pastes and/or application of a convex pouching system), affected skin tends to heal rapidly. Topical hydrocolloid powder will help prevent peristomal skin loss. 31 32 33 34 Rarely, operative resiting may be indicated for cases of recalcitrant leakage dermatitis that prove refractory to pouching system modifications.
Fig. 4.

Early moisture change.
Fig. 5.
Denuded skin from irritant contact dermatitis.
Fig. 6.
Irritant contact dermatitis resulting from leakage.
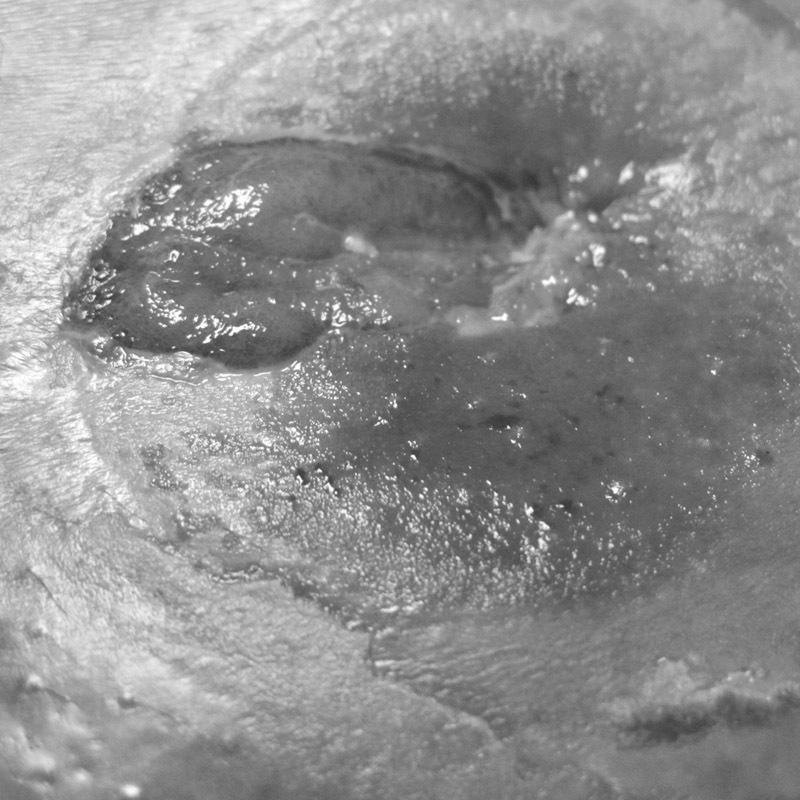
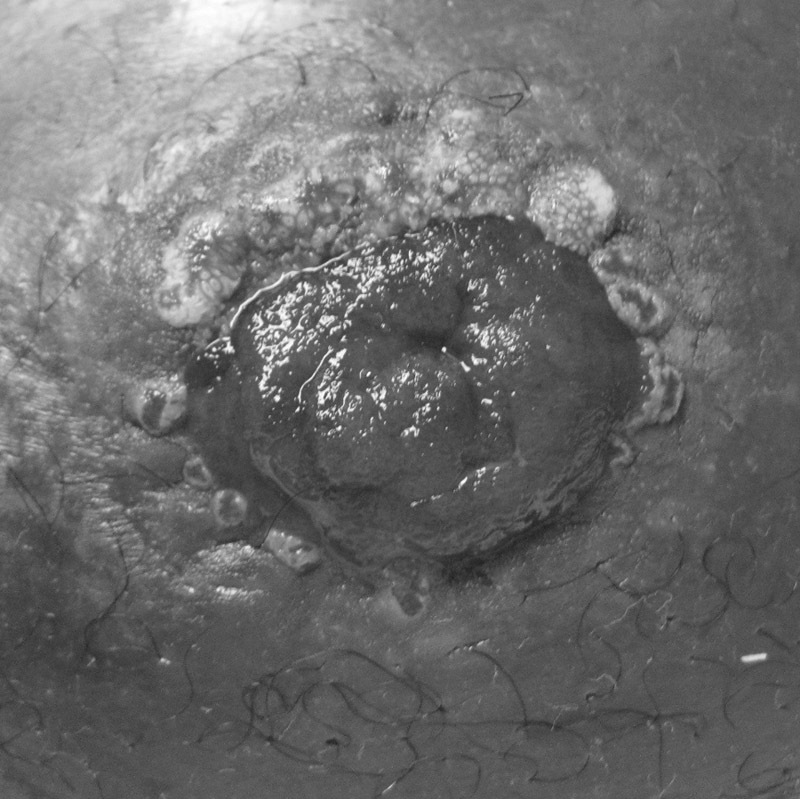
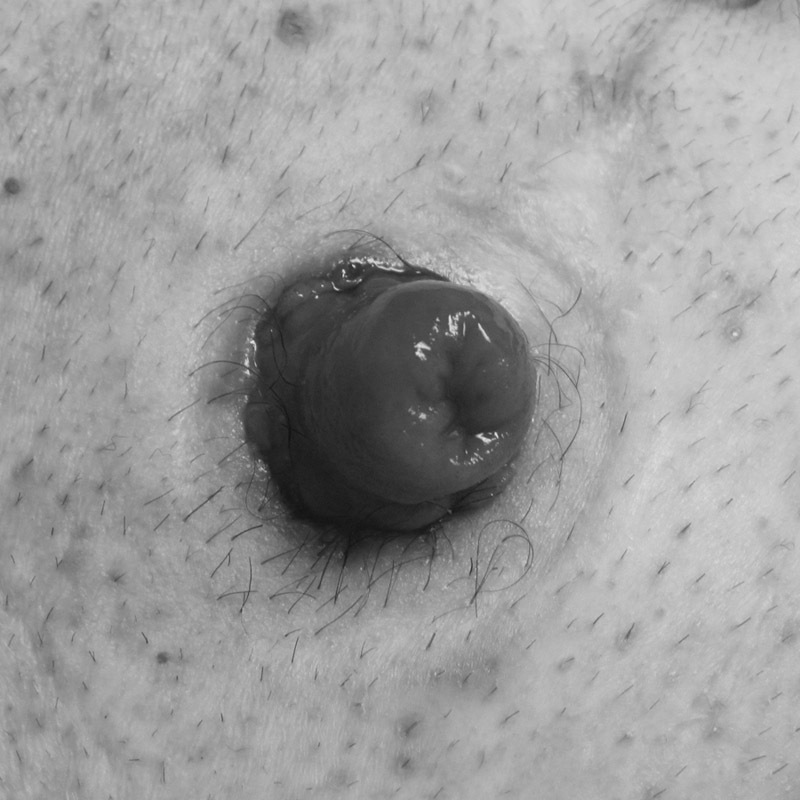
Pseudoverrucous Epitheliomatous Hyperplasia
Pseudoverrucous epitheliomatous hyperplasia (PEH) is an uncommon sequela from chronic irritant contact dermatitis hypothesized to arise from prolonged moisture exposure. 35 Chronic peristomal moisture leads to benign pseudoverrucous changes around the stoma that appear as raised, thickened, and bumpy skin with variable color changes ( Figs. 7 and 8 ). Patients may report peristomal itching and bleeding, whereas dermal biopsies may demonstrate acanthosis, elongated rete ridges, hyperkeratosis, and dermal inflammation. 11 The differential diagnosis for PEH includes condyloma, neoplasm, bacterial infection, and candidiasis. PEH treatment typically involves reassessing the skin barrier aperture size, although the raised, irregular area may still prevent adequate sealing ( Fig. 9 ). Topical silver nitrate may resolve raised skin lesions. Intralesional corticosteroid injection may be required, and severe lesions can require surgical excision.
Fig. 7.
Chronic moisture change.
Fig. 8.

Pseudoverrucous epitheliomatous hyperplasia.
Fig. 9.
Pseudoverrucous epitheliomatous hyperplasia that will interfere with pouching system application.
Allergic Contact Dermatitis
Allergies can arise from any ostomy product including the skin barrier, powders, pastes, belts, cleansing products, and adhesives. Allergic reactions are rare but can produce geographic erythema, blisters, pruritus, and pain ( Fig. 10 ). Allergic dermatitis should be suspected following changes in pouching products and routines. An easy way to empirically diagnose allergic dermatitis is to place a small amount of the suspected product elsewhere on the patient's skin for 24 to 48 hours. If no allergic reaction develops, formal allergy testing is performed. Treatment of allergic dermatitis begins by substituting the offending product with a nonallergenic alternative. Allergic skin may be further treated with topical aerosolized corticosteroids, and rarely systemic steroids are required. 33
Fig. 10.
Mild allergic contact dermatitis.
Folliculitis
Folliculitis is inflammation of the hair follicles thought to arise from trauma at the hair-bearing areas underlying the stoma pouch system. Vigorous appliance removal can traumatize peristomal skin follicles, leading to infection with gram-positive bacteria (e.g., Staphylococcus aureus) . 29 Folliculitis is characterized by erythematous pustules noted at individual hair follicles ( Fig. 11 ). Folliculitis is avoided by instructing the patient to clip, but not shave, hair under the appliance using a clipper or scissors. Additionally, gentle use of an adhesive remover when removing the pouching system may prevent follicular trauma. Topical treatment may also entail cleansing the peristomal skin with an antibacterial soap at pouch change or use of an antibacterial powder. 34
Fig. 11.
Peristomal folliculitis.
Pressure Wounds and Mechanical Trauma
Peristomal pressure wounds may develop from pouching apparatus, typically due to use of a convex appliance or stoma belt ( Fig. 12 ). Pressure wounds are commonly associated with parastomal hernias, particularly when a hard convex ring is used to pouch. Full- or partial-thickness skin wounds may develop where the firm portions of the appliance contacts the apex of the hernia bulge. If a convex appliance is required to sustain an adequate seal, a soft or flexible convex pouching system may be used. The authors recommend treating full-thickness pressure wounds first with an alginate dressing covered with a nonadherent foam or hydrocolloid dressing. Partial-thickness pressure wounds can be treated with skin barrier powder, and thin foam or hydrocolloid dressings. As with most peristomal skin conditions, close follow-up and meticulous care is required to prevent progression.
Fig. 12.
Peristomal pressure ulcer due to convex pouching system.
Epidermal stripping and mechanical skin trauma can occur from repeated applications of the appliance and from overzealous removal of old paste or tape residue. 36 Mechanical trauma is best treated with reinforcing WOC nurse education sessions focusing on careful observation of pouching technique and wear-time counseling.
Psoriasis
Peristomal psoriasis presents similarly to psoriasis on other skin areas. Psoriatic lesions are characteristically well-demarcated, erythematous plaques with flaky, shiny scales. Psoriasis tends to follow one of the following four characteristic patterns: psoriatic plaques in the area around the skin barrier but not extending beneath it, plaques both beneath and beyond the wafer, glazed erythematous psoriasis with similar lesions in a more typical flexor distribution, and generalized pustular psoriasis. 32 Distribution of psoriatic lesions tend to follow the Koebner phenomenon, with lesions appearing in areas of dermal trauma. Treatment of peristomal psoriasis is based on reducing inflammation with topical or intralesional steroid preparations. Betamethasone aqueous lotion is helpful since it does not interfere with the pouching system seal. Prevention of peristomal trauma may reduce psoriasis recurrence. 11
Bacterial and Fungal Infection
Peristomal cellulitis is somewhat uncommon compared with other peristomal skin complications. Cellulitis tends to arise from typical skin flora bacteria, most commonly Staphylococcus aureus . 34 Cellulitis can present as an erythematous peristomal plaque ( Fig. 13 ). Peristomal cellulitis is initially treated with oral antibiotics, but severe soft tissue infection may require parenteral antibiotics or rarely debridement. When bacterial skin infections are present, it is critical to rule out a deeper peristomal abscess. In addition to causing overlying cellulitis, abscesses will be painful and fluctuant and may spontaneously drain. Peristomal abscesses are more commonly seen in ostomates with Crohn's disease and may represent a peristomal fistula. Unlike isolated peristomal cellulitis, peristomal abscesses tend to be caused by enteric organisms rather than skin flora. If a peristomal abscess is confirmed, drainage should be performed either through an incision at the mucocutaneous junction or > 4 cm away from the mucocutaneous junction to avoid interference with the stoma pouch.
Fig. 13.
Peristomal bacterial infection Staphylococcus aureus.
The warm, dark, moist environment under the pouch adhesive is particularly hospitable to fungal infection with Candida albicans . Exposure to stool due to too large a skin-barrier aperture may further exacerbate peristomal fungal infections. Fungal infection is more common in ileostomy patients, particularly those with debilitated or immunocompromised states. Fungal lesions are bright red and moist and can be papules, vesicles, pustules, or erosions. Satellite lesions are often seen in fungal infections, which help to distinguish candidiasis from dermatitis. 37 Patients will report severe itching and burning. Diagnosis is generally based on appearance, but, if needed, potassium hydroxide testing of rash scrapings can be performed. A properly fitted skin barrier and topical antifungal powder will generally result in successful treatment. Oral antifungal agents are required only for recalcitrant infection.
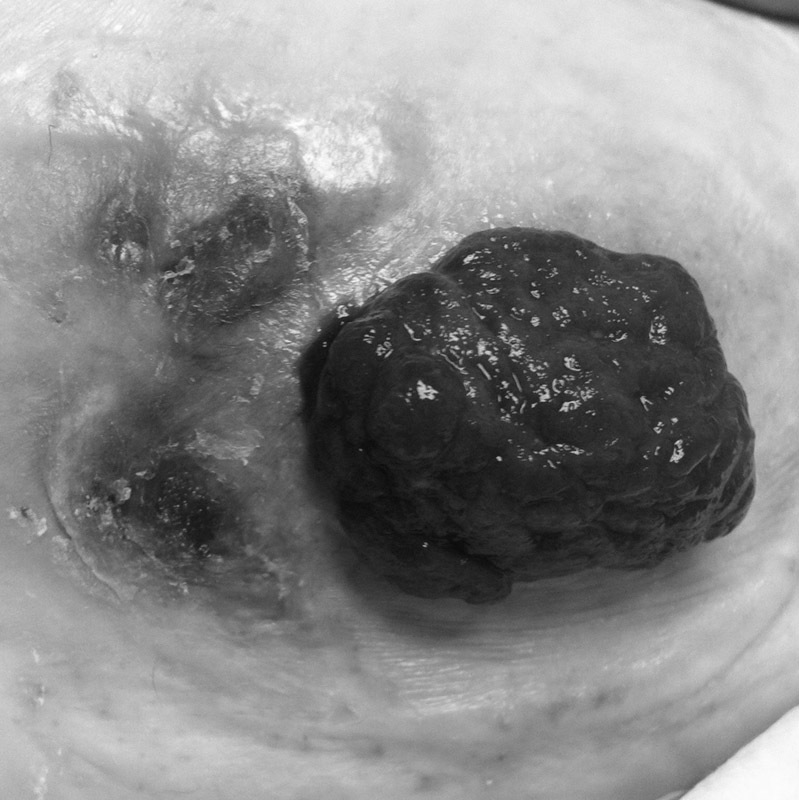
Neoplasia
Stomal malignancy has rarely been described in case reports. 38 Stomal malignancy may arise as metachronous colorectal cancer, sequela of inflammatory bowel disease, or spontaneous de novo cancer, or can represent locoregional spread from cutaneous malignancy. Stomal metastasis arising from other carcinomas including colorectal, gastric, and lung neoplasms have been reported. 39 40 41 Stomal malignancies typically present as a mass lesion ( Fig. 14 ), but stricture, rash, and ulceration may be the presenting symptoms requiring a high index of suspicion for diagnosis. Metachronous peristomal colorectal cancer has been described anywhere from 4 to 30 years after initial diagnosis. 42 When stomal malignancies occur, the typical treatment is wide local excision and stoma resiting, when feasible.
Fig. 14.

Adenocarcinoma arising from a stoma.
Herpes Zoster
Herpes zoster is caused by the reactivation of the varicella zoster virus. Zoster typically occurs in one or two adjacent dermatomes, most commonly on the trunk along a thoracic dermatome. The rash does not cross the sagittal midline. Stress and fatigue can trigger reactivation, and immunosuppressed or immunocompromised patients are at increased risk. The rash will begin as a cluster of clear vesicles forming over a 3- to 5-day period and progressing to dry, crusty areas ( Fig. 15 ). Pain in the area is frequently the presenting symptom. While rare, peristomal herpetic lesions are unroofed at the pouch change, and the resultant open moist areas can compromise the pouch seal, in addition to causing significant pain. A hydrocolloid dressing is placed over the involved area to provide a pouch seal; careful removal of the pouching system will decrease trauma to the area. Advise the patient on good hand washing techniques to avoid spread of the virus
Fig. 15.
Peristomal herpes zoster.
Conclusion
Excellent perioperative stoma care and education are essential for ostomates to feel confident in caring for and changing their pouching systems and to avoid dehydration. Many peristomal skin conditions are entirely preventable with meticulous skin and pouching system care. A variety of skin problems, some related to underlying disease and others related directly to issues with stoma care, require treatment either by a WOC nurse or an experienced physician. Those who create stomas should also be able to troubleshoot the issues their patients experience in the immediate postoperative period and beyond. Follow-up is critical for the patient with a new stoma both to educate the patient in correct stoma care and for early identification and treatment of peristomal skin conditions.
References
- 1.Hignett S, Parmar C D, Lewis W, Makin C A, Walsh C J. Ileostomy formation does not prolong hospital length of stay after open anterior resection when performed within an enhanced recovery programme. Colorectal Dis. 2011;13(10):1180–1183. doi: 10.1111/j.1463-1318.2010.02381.x. [DOI] [PubMed] [Google Scholar]
- 2.Tang C L, Yunos A, Leong A P, Seow-Choen F, Goh H S. Ileostomy output in the early postoperative period. Br J Surg. 1995;82(05):607. doi: 10.1002/bjs.1800820510. [DOI] [PubMed] [Google Scholar]
- 3.Taylor W E. St. Louis, MO: Quality Medical Publishing; 2004. PJH. Stoma physiology. [Google Scholar]
- 4.Hill G L, Goligher J C, Smith A H, Mair W S. Long term changes in total body water, total exchangable sodium and total body potassium before and after ileostomy. Br J Surg. 1975;62(07):524–527. doi: 10.1002/bjs.1800620706. [DOI] [PubMed] [Google Scholar]
- 5.Paquette I M, Solan P, Rafferty J F, Ferguson M A, Davis B R. Readmission for dehydration or renal failure after ileostomy creation. Dis Colon Rectum. 2013;56(08):974–979. doi: 10.1097/DCR.0b013e31828d02ba. [DOI] [PubMed] [Google Scholar]
- 6.Messaris E, Sehgal R, Deiling S et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum. 2012;55(02):175–180. doi: 10.1097/DCR.0b013e31823d0ec5. [DOI] [PubMed] [Google Scholar]
- 7.Prinz A, Colwell J C, Cross H H, Mantel J, Perkins J, Walker C A. Discharge planning for a patient with a new ostomy: best practice for clinicians. J Wound Ostomy Continence Nurs. 2015;42(01):79–82. doi: 10.1097/WON.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 8.Hendren S, Hammond K, Glasgow S C et al. Clinical practice guidelines for ostomy surgery. Dis Colon Rectum. 2015;58(04):375–387. doi: 10.1097/DCR.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 9.Nichols T R. Social connectivity in those 24 months or less postsurgery. J Wound Ostomy Continence Nurs. 2011;38(01):63–68. doi: 10.1097/won.0b013e318202a804. [DOI] [PubMed] [Google Scholar]
- 10.Coggrave M J, Ingram R M, Gardner B P, Norton C S. The impact of stoma for bowel management after spinal cord injury. Spinal Cord. 2012;50(11):848–852. doi: 10.1038/sc.2012.66. [DOI] [PubMed] [Google Scholar]
- 11.Salvadalena G.Incidence of complications of the stoma and peristomal skin among individuals with colostomy, ileostomy, and urostomy: a systematic review J Wound Ostomy Continence Nurs 20083506596–607., quiz 608–609 [DOI] [PubMed] [Google Scholar]
- 12.Erwin-Toth P, Thompson S J, Davis J S.Factors impacting the quality of life of people with an ostomy in North America: results from the Dialogue Study J Wound Ostomy Continence Nurs 20123904417–422., quiz 423–424 [DOI] [PubMed] [Google Scholar]
- 13.Wound, Ostomy and Continence Nurses SocietyAvailable athttp://www.wocn.org/default.asp?page=Nurse_Referral. Accessed November 11, 2015
- 14.American College of Surgeons. Available athttps://www.facs.org/education/patient-education/skills-programs/ostomy-program. Accessed November, 2015
- 15.Pittman J, Rawl S M, Schmidt C M et al. Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. J Wound Ostomy Continence Nurs. 2008;35(05):493–503. doi: 10.1097/01.WON.0000335961.68113.cb. [DOI] [PubMed] [Google Scholar]
- 16.Salvadalena G, Hendren S, McKenna L et al. WOCN Society and ASCRS Position Statement on preoperative stoma site marking for patients undergoing colostomy or ileostomy surgery. J Wound Ostomy Continence Nurs. 2015;42(03):249–252. doi: 10.1097/WON.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 17.Duchesne J C, Wang Y Z, Weintraub S L, Boyle M, Hunt J P.Stoma complications: a multivariate analysis Am Surg 20026811961–966., discussion 966 [PubMed] [Google Scholar]
- 18.Robertson I, Leung E, Hughes D et al. Prospective analysis of stoma-related complications. Colorectal Dis. 2005;7(03):279–285. doi: 10.1111/j.1463-1318.2005.00785.x. [DOI] [PubMed] [Google Scholar]
- 19.Arumugam P J, Bevan L, Macdonald L et al. A prospective audit of stomas--analysis of risk factors and complications and their management. Colorectal Dis. 2003;5(01):49–52. doi: 10.1046/j.1463-1318.2003.00403.x. [DOI] [PubMed] [Google Scholar]
- 20.Chun L J, Haigh P I, Tam M S, Abbas M A. Defunctioning loop ileostomy for pelvic anastomoses: predictors of morbidity and nonclosure. Dis Colon Rectum. 2012;55(02):167–174. doi: 10.1097/DCR.0b013e31823a9761. [DOI] [PubMed] [Google Scholar]
- 21.Leong A P, Londono-Schimmer E E, Phillips R K. Life-table analysis of stomal complications following ileostomy. Br J Surg. 1994;81(05):727–729. doi: 10.1002/bjs.1800810536. [DOI] [PubMed] [Google Scholar]
- 22.Londono-Schimmer E E, Leong A P, Phillips R K. Life table analysis of stomal complications following colostomy. Dis Colon Rectum. 1994;37(09):916–920. doi: 10.1007/BF02052598. [DOI] [PubMed] [Google Scholar]
- 23.Caricato M, Ausania F, Ripetti V, Bartolozzi F, Campoli G, Coppola R. Retrospective analysis of long-term defunctioning stoma complications after colorectal surgery. Colorectal Dis. 2007;9(06):559–561. doi: 10.1111/j.1463-1318.2006.01187.x. [DOI] [PubMed] [Google Scholar]
- 24.Saghir J H, McKenzie F D, Leckie D M et al. Factors that predict complications after construction of a stoma: a retrospective study. Eur J Surg. 2001;167(07):531–534. doi: 10.1080/110241501316914911. [DOI] [PubMed] [Google Scholar]
- 25.Zorcolo L, Covotta L, Carlomagno N, Bartolo D C.Toward lowering morbidity, mortality, and stoma formation in emergency colorectal surgery: the role of specialization Dis Colon Rectum 200346111461–1467., discussion 1467–1468 [DOI] [PubMed] [Google Scholar]
- 26.Takahashi K, Funayama Y, Fukushima K et al. Stoma-related complications in inflammatory bowel disease. Dig Surg. 2008;25(01):16–20. doi: 10.1159/000117818. [DOI] [PubMed] [Google Scholar]
- 27.Carlstedt A, Fasth S, Hultén L, Nordgren S, Palselius I. Long-term ileostomy complications in patients with ulcerative colitis and Crohn's disease. Int J Colorectal Dis. 1987;2(01):22–25. doi: 10.1007/BF01648993. [DOI] [PubMed] [Google Scholar]
- 28.Boyd-Carson W, Thompson M J, Trainor B, Boyd K. Mucocutaneous separation. Nurs Stand. 2004;18(17):41–43. [PubMed] [Google Scholar]
- 29.Salvadalena G, Carmel J E, Colwell J C, Goldberg M T.Peri-stomal skin conditionsIn:, eds.WOCN Core Curriculum: Ostomy Management. Philadelphia, PA: Wolter Kluwer; 2015 [Google Scholar]
- 30.Agarwal S, Ehrlich A. Stoma dermatitis: prevalent but often overlooked. Dermatitis. 2010;21(03):138–147. [PubMed] [Google Scholar]
- 31.Nybaek H, Jemec G B. Skin problems in stoma patients. J Eur Acad Dermatol Venereol. 2010;24(03):249–257. doi: 10.1111/j.1468-3083.2010.03566.x. [DOI] [PubMed] [Google Scholar]
- 32.Lyon C C, Smith A J, Griffiths C E, Beck M H. The spectrum of skin disorders in abdominal stoma patients. Br J Dermatol. 2000;143(06):1248–1260. doi: 10.1046/j.1365-2133.2000.03896.x. [DOI] [PubMed] [Google Scholar]
- 33.Meisner S, Lehur P A, Moran B, Martins L, Jemec G B. Peristomal skin complications are common, expensive, and difficult to manage: a population based cost modeling study. PLoS One. 2012;7(05):e37813. doi: 10.1371/journal.pone.0037813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahmoud N NBB. St Louis, MO: Quality Medical Publishing; 2004. Diagnosis and treatment of peristomal skin conditions; pp. 39–55. [Google Scholar]
- 35.Douri T, Shawaf A Z. Letter: Pseudoverrucous papules and nodules: a case report. Dermatol Online J. 2012;18(04):14. [PubMed] [Google Scholar]
- 36.Hellman J, Lago C P. Dermatologic complications in colostomy and ileostomy patients. Int J Dermatol. 1990;29(02):129–133. doi: 10.1111/j.1365-4362.1990.tb04085.x. [DOI] [PubMed] [Google Scholar]
- 37.Morales-Mendoza Y, Fernández-Martínez R, Fabián-Victoriano M R et al. Candida species isolation in peristomal skin in patients with abdominal stomas and correlation to clinical signs: a descriptive pilot study. Adv Skin Wound Care. 2014;27(11):500–504. doi: 10.1097/01.ASW.0000455691.96993.ab. [DOI] [PubMed] [Google Scholar]
- 38.Maeda C, Hidaka E, Shimada M et al. Transverse colon cancer occurring at a colostomy site 35 years after colostomy: a case report. World J Surg Oncol. 2015;13:171. doi: 10.1186/s12957-015-0593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mourra N, Bataillon G, Lesurtel M. Fungating mass occurring at a colostomy site 50 years after colectomy for inflammatory condition. Gastroenterology. 2014;146(02):e1–e2. doi: 10.1053/j.gastro.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 40.Sabater-Marco V, García-García J A, Roig-Vila J V. Basaloid large cell lung carcinoma presenting as cutaneous metastasis at the colostomy site after abdominoperineal resection for rectal carcinoma. J Cutan Pathol. 2013;40(08):758–764. doi: 10.1111/cup.12145. [DOI] [PubMed] [Google Scholar]
- 41.Vijayasekar C, Noormohamed S, Cheetham M J. Late recurrence of large peri-stomal metastasis following abdomino-perineal resection of rectal cancer. World J Surg Oncol. 2008;6:96. doi: 10.1186/1477-7819-6-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shibuya T, Uchiyama K, Kokuma M et al. Metachronous adenocarcinoma occurring at a colostomy site after abdominoperineal resection for rectal carcinoma. J Gastroenterol. 2002;37(05):387–390. doi: 10.1007/s005350200054. [DOI] [PubMed] [Google Scholar]


