Abstract
Background
There is limited information on the prevalence of posttraumatic stress disorder (PTSD) across primary care settings.
Objective
Determine the prevalence of clinician-diagnosed PTSD and questionnaire-ascertained PTSD symptoms in primary care patients.
Methods
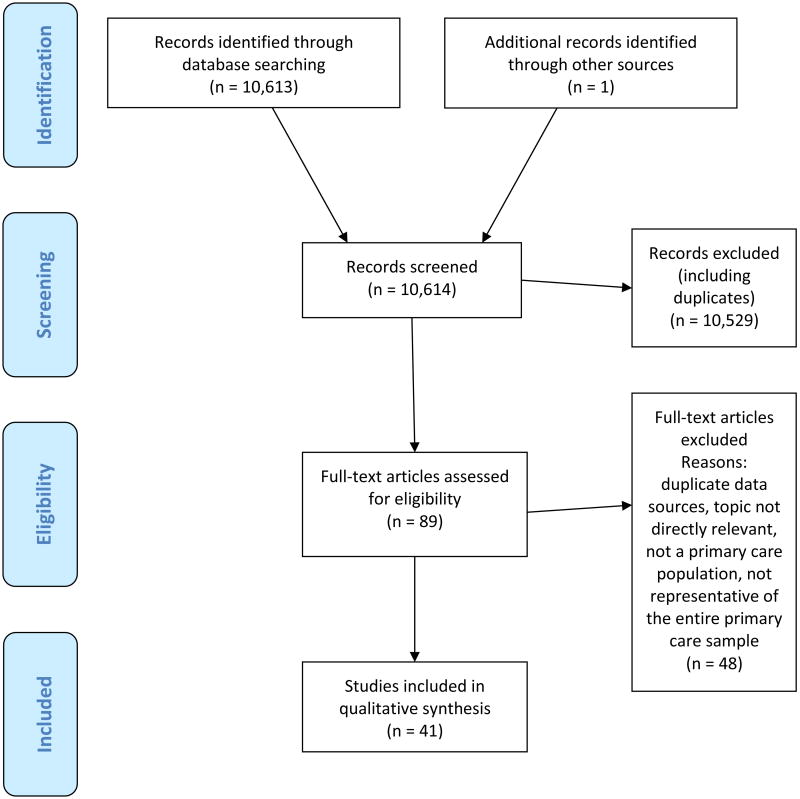
A systematic review of the literature using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method, searching MEDLINE, CINAHL, Cochrane Database, PsychINFO, EMBASE, Google Scholar, and relevant book chapter bibliographies. Studies that reported on the prevalence, including point and/or lifetime prevalence, of PTSD ascertained using diagnostic interviews, self-report questionnaires, or from administrative data, among patients seen in primary care were deemed eligible for inclusion. We abstracted data on the PTSD assessment tool, the mean questionnaire scores/cutoff scores, the time period of PTSD symptoms, and PTSD prevalence reported.
Results
Of 10,613 titles screened, 41 studies were eligible for inclusion. The included studies assessed PTSD in a total of 7,256,826 primary care patients. The median point prevalence of PTSD across studies was 12.5%. The point prevalence of the civilian population median was 11.1%, the special risk population median was 12.5%, and the veteran median was 24.5%. The point prevalence of diagnostic interview-ascertained PTSD ranged from 2% to 32.5%, the point prevalence of questionnaire-based substantial PTSD symptoms ranged from 2.9% to 39.1%. Lifetime prevalence of diagnostic interview ascertained-PTSD ranged from 14.5% to 44.3%. The prevalence of PTSD in administrative data-based studies ranged from 3.5% to 48.8%.
Conclusions
PTSD is common in primary care settings. Additional research on effective and generalizable interventions for PTSD in primary care is needed.
Keywords: Health Services Needs and Demand, Prevalence, Primary Health Care, Stress Disorders, Post-Traumatic
Introduction
Posttraumatic stress disorder (PTSD) is a psychiatric illness first recognized in war veterans and later more widely recognized in those who experience other traumas, including abuse or assault, traumatic injuries and life-threatening illnesses.1-3 Individuals with PTSD actively suffer from severe psychiatric symptoms which impair functioning such as panic attacks when confronted with reminders of the trauma.4 Diagnostic criteria for PTSD include an exposure to an actual or threatened death, serious injury, or sexual violence in the following ways: direct experience, witnessing, learning about traumatic events that occurred to close family or friends, or experiencing repeated or extreme exposure to aversive details of the traumatic events. Over a period of 4 weeks they experience a constellation of symptoms including intrusive symptoms (including flashbacks, nightmares and intrusive thoughts of the incident), avoidant behavior (avoiding situations, people, stimuli that remind them of the traumatic event), negative mood (which can include self-blame for the traumatic incident, isolation and detachment), and alterations in arousal (including hypervigilence, exaggerated startle response, poor sleep and concentration).”4
According to the National Comorbidity Survey Replication (NCS-R), one of the largest epidemiological studies of mental disorders performed in the United States general population, the lifetime prevalence of PTSD in adults is 6.8% and the annual prevalence is 3.5%.5, 6 Adverse experiences in childhood are one example of events that can result in later symptoms of PTSD. Primary care patients have a high prevalence of adverse childhood experiences (ACEs), leading to increased physical illness burden.7 About 25-30% of those who experience traumatic events such as those measured by the ACEs study develop PTSD.8
Although there is a high prevalence of traumatic event exposure among primary care patients and collaborative care interventions have been developed for the successful treatment of common mental disorders in primary care settings,9, 10 there remains a need for information on the overall prevalence of PTSD across primary care settings. Understanding the rates of PTSD in primary care settings can facilitate the selection and use of a standard screening tool (such as the PC-PTSD-5)11 and clinically useful algorithms for patients with PTSD served in primary care clinics. Effective screening tools and treatment protocols for stepped care12 models are especially important in light of increased behavioral health integration efforts in primary care settings across the U.S.
The present systematic review quantifies what is known about the prevalence of PTSD in primary care settings to help clinicians and researchers have a benchmark with which to compare the prevalence of the populations that they are working (both for screening and treatment purposes). While a recent review article addressed this topic,13 to our knowledge this is the first systematic review article with the scope and breadth to capture relevant studies for inclusion. The present report documents the results of a systematic review of studies examining PTSD in primary care settings. Our objective was to obtain an accurate estimate of PTSD in various adult primary care populations in the existing literature. We sought to review both the prevalence of administrative data documented PTSD and questionnaire-ascertained clinically meaningful PTSD symptoms in primary care patients.
Methods
Approach
A systematic review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method.14
Search Strategy
Databases searched included MEDLINE (using MeSH terms and a general search), CINAHL, Cochrane Library, PsychINFO, EMBASE, Google Scholar, and relevant book chapter bibliographies. The following search terms and strategy was used: (“Traumatic stress” or PTSD or posttraumatic or “posttraumatic stress disorder” or trauma or “post traumatic” or “post-traumatic”) AND (“primary care” or PCP or “patient centered medical home” or “internal medicine” or “family medicine” or “general practice” or “obstetrics and gynecology” or “ob/gyn” or “primary health care” or “primary healthcare”) AND (prevalence). This search included MeSH terms PTSD, Primary Healthcare, Patient Centered Medical Home, Internal Medicine, Family Medicine, and Obstetrics and Gynecology, each of which map onto similar terms to expand the search in the MEDLINE database.
The databases were searched from January 1980 when the diagnosis of PTSD was first included in the Diagnostic and Statistical Manual of Mental Disorders-III (DSM-III), to January 2016 (date last searched). Authors MS and HH screened titles and abstracts as well as reviewed the full text of eligible articles. If data within the articles were unclear original study authors were contacted for clarification.
Eligibility Criteria
Inclusion criteria comprised original articles in English reporting the prevalence, including point and/or lifetime prevalence, of PTSD among patients seen in a primary care setting. Primary care was defined as first contact medical care (family practice, internal medicine, obstetrics-gynecology clinics). We included articles in which PTSD was ascertained using diagnostic interviews, self-report questionnaires, or from medical record diagnoses.
Articles were excluded if they contained duplicate data sources with other articles (so as not to over-represent one primary care sampled population), if the topic was found not to be directly relevant, if the study was not primary care-based, or if the population studied was not representative of the entire primary care population at the study site(s). We also excluded abstracts, case reports/case series and review articles.
Study records
Initial titles were screened by one author (MS) and selected abstracts were screened by two independent reviewers/authors (MS and HH). Studies were selected for inclusion if two authors agreed that they clearly met eligibility criteria. The prevalence of PTSD was the main outcome of interest and was examined based on different sub-groups including general primary care, veterans in primary care, and special risk populations in primary care (e.g. refugees and immigrants). Additional outcomes of interest included type of diagnostic or screening tool used and sample characteristics. The diagnostic or screening tools were important to better understand potential differences in PTSD prevalence and the sample characteristics were important to examine potential trends in various prevalence levels (e.g. elevated rates of PTSD in primary care veteran populations).
The abstracted data from each study was collected into a data collection spreadsheet accessible to both authors involved in this process (MS and HH). Abstracted data included primary care population sample characteristics (location, clinic site, urban/rural, mean age, population type, gender, race, study design, and number of participants in the sample), and results (PTSD prevalence, PTSD ascertainment tool, mean questionnaire scores and cutoff scores [if relevant], time period of symptoms measured, and number of participants that completed PTSD assessment).
Risk of bias
Articles were assessed for risk of bias using an adapted risk of bias screen developed by Hoy et al.,15 which has been used in other systematic review articles.16 The Hoy bias tool was modified to screen for bias based on the studies representation of a primary care sample rather than a national population. Articles were ranked for risk of bias by two authors (MS and HH) independently. Articles were assigned a low, medium, or high risk of bias with 9 representing little bias and 0 representing a high risk of bias. Low risk of bias was assigned if the article contained 7-9 items on the risk of bias screen, moderate risk if the article contained 3-6 items, and high risk if the article contained 0-2 items. The risk of bias information was provided in the results section with authors noting any trends in bias score and prevalence rates.
Because of the diversity in primary care, quantitative synthesis was not appropriate for this systematic review. Median PTSD prevalence was calculated using a median calculator in order to summarize the data.
Results
Of 10,613 titles screened, 89 full-text articles were assessed for eligibility. Forty-one studies were included in the qualitative synthesis (see Figure 1). General sample characteristics are described in Table 1 while results are found in Table 2. Studies were conducted in the following countries: Canada (1), Italy (1), Israel (2), Lithuania (1), Puerto Rico (1), Qatar (1), South Africa (2), Spain (1), Sweden (1), Switzerland (1), and the United States (29).
Figure 1.
PRISMA13 flow diagram of article selection
Table 1. Sample characteristics of PTSD in primary care reviewed studies.
| Study | Location | Site affiliation |
Urban/Rural | Mean age (SD) |
Population type |
Gender | Race | Risk of bias* |
Study design | N of enrolled sample (as reported) |
|---|---|---|---|---|---|---|---|---|---|---|
| General Primary Care | ||||||||||
| Stein et al. (2000)17 | San Diego, California, USA | Academic primary care | Urban | 36.9 (SD not provided) | Civilian | 56.5% female | 61.1% Caucasian; 12.5% Filipino; 8.2% Latino/Hispanic; 7.6% Asian American; 4.1% African American | M | Cross-sectional | 762 eligible |
| Applegate (2001)18 | Louisiana, USA | Academic primary care | Urban | 46.4 (SD 13.8) | Low-income | 81% female | 74.2% African American; 25% Caucasian; 1% other | M | Cross-sectional | 433 enrolled |
| Taubman-Ben-Ari et al. (2001)19 | Israel | Non-academic primary care | Not reported - Israel is 91% urban | 51.4 (SD 17.8) | Israelis | 60% female | Israeli | L | Retrospective review of medical records | 2975 enrolled |
| Carey et al. (2003)20 | South African township | Non-academic primary care | Urban | 31.1 (SD 10.77) | “Poor urban community” | 61.2% female | Xhosa township historically segregated for black Africans only | M | Retrospective review of medical records | 220 enrolled |
| Thulesius et al. (2004)21 | Sweden | Non-academic primary care | Both | 46.6 (SD 15.2) | Civilians in Sweden | 60% female | Not reported | L | Cross-sectional | 1378 enrolled |
| Gillock et al. (2005)22 | New Hampshire, USA | Academic primary care | Rural | 41.91 (SD 10.45) | Civilian | 69% female | 95% Caucasian | M | Cross-sectional | 627 approached |
| Gomez-Benevto et al. (2006)23 | Valencia, Spain | Non-academic primary care | Urban | 44 (SD 17) | Civilian | 66% female | Not reported | L | Cross-sectional | 331 enrolled |
| Kroenke et al. (2007)24 | 12 states, USA | Non-academic primary care | Not reported | 47.1 (SD 15.5; range 18-87 years) | Civilian | 69% female | 81% non-Hispanic White; 7% Black; 9% Hispanic; 3% other | L | Cross-sectional | 2982 invited |
| Liebschutz et al. (2007)25 | Boston, Massachusetts, USA | Academic primary care | Urban | 42 (SD 11.3) | Civilian | 51% female | 59% Black/African American; 19% White; 8% Hispanic/Latino; 14% other | M | Cross-sectional | 621 enrolled |
| Peltzer et al. (2007)26 | South Africa | Non-academic primary care | Rural | 31.1 (SD 11.8) | Population in a developing setting | 76% female | 100% Black African | L | Cross-sectional | 250 enrolled |
| Cwikel et al. (2008)27 | Israel | Non-academic primary care | Not reported - Isreal is 91% urban | 30.6% age 25-44; 42.8% age 45-64; 26.5% age 65-75 | Civilian | 65.2% female | Not reported | L | Cross-sectional | 77% of those eligible included |
| Fedovskiy et al. (2008)28 | Atlanta, Georgia, USA | Academic primary care | Urban | 38.5 (SD 11.4) | Women who are low income, uninsured, relatively low level of education | 100% female | 100% Latina | M | Cross-sectional | Not reported |
| Fogarty et al. (2008)29 | Boston, Massachusetts, USA | Academic primary care | Urban | 68.8% age 18-44 | Civilian | 61.1% female | 46.8% Black | L | Cross-sectional | 72% response rate |
| Duran et al. (2009)30 | Albuquerque, New Mexico, USA | Non-academic primary care | Urban and 5 tribes | 18-45 years of age | American Indian women | 100% female | 100% American Indian | M | Cross-sectional | 396 enrolled |
| Freedy et al. (2010)31 | Southeastern USA | Academic primary care | Both | Men 45.1% age 18-44, women 55.3% age 18-44 | Civilian | 82.5% female | 65% White, 35% African American or other | M | Cross-sectional | 519 enrolled |
| Gaynes et al. (2010)32 | Chapel Hill, North Carolina, USA | Academic primary care | Urban | 45.2 (SD 15.4) | Civilian | 70.9% female | 66.9% White, 28.4% African American, 4.6% other | L | Cross-sectional | 723 enrolled |
| Wrenn et al. (2011)33 | Atlanta, Georgia, USA | Non-academic primary care | Urban | 37 (range 18-74) | Inner city | 67% female | 94% African American | M | Cross-sectional | 58% of those approached included |
| Vera et al. (2012)34 | San Juan, Puerto Rico | Non-academic primary care | Urban | 42.9 mean; 33.1% 18-35; 32.7% 36-50; 34.2% 51-65 | Civilian | 79.4% female | Puerto Rican and Dominican | L | Cross-sectional | 93% of those approached agreed to participate |
| Bunevicius et al. (2014)35 | Lithuania | Non-academic primary care | Urban | 50 (SD 19) | Civilian | 68% female | Lithuanian | L | Cross-sectional | 1170 approached |
| Preville et al. (2014)36 | Quebec, Canada | Non-academic primary care | Both | 73.2 (SD 6.1) | Civilian | 57.3% female | Quebecois | L | Cross-sectional | 1811 agreed |
| Bener et al. (2015)37 | Qatar | Non-academic primary care | Urban | 37.8% aged 35-49 | Civilian | 56.3% female | Qatari nationals | L | Cross-sectional | 2000 approached |
| Special Risk (Refugee/Immigrant) | ||||||||||
| Eisenman et al. (2003)38 | Los Angeles, California, USA | Non-academic primary care | Urban | 46.1 (SD 24.7) | Primarily uninsured Latino population | 75.3% female | 100% Latino: 41.5% from Mexico; 32.5% from El Salvador; 17.7% from Guatemala; 8.3% from “other” (Honduras, Nicaragua, Cuba, and South America) | M | Cross-sectional | 1287 approached |
| Eytan et al. (2007)39 | Geneva, Switzerland | Academic primary care | Urban | 30 (SD 11) | Asylum seekers in Switzerland | 26% female | 58% African; 37% European; 5% Asian | L | Cross-sectional | 107 enrolled |
| Aragona et al. (2013)40 | Rome, Italy | Non-academic primary care | Urban | 37.58 (SD 11.45) | New Immigrants to Italy | 39.65% female | 100% first generation immigrants from: Asia (22.1%); Africa (28.2%); Latin America (6.7%); Eastern Europe (43.1%); Romania (30.9%); China (7.4%); Bangladesh (6.1%) | L | Cross-sectional | 412 enrolled |
| Veteran | ||||||||||
| Dobie et al. (2002)41 | Puget Sound, Washington, USA | VA system | Urban | 48 (SD 13.7) | Veteran | 100% female | 74.5% White; 9.2% Black; 14.9% other | L | Cross-sectional | 1794 invited |
| Mori et al. (2003)42 | Boston, Massachusetts, USA | VA primary care | Urban | 64 | Veteran | 2.2% female | 77% Caucasian | M | Cross-sectional | 313 enrolled |
| Prins et al. (2003)43 | Palo Alto and Menlo Park, California, USA | VA primary care and women's health | Urban | 52.1 (SD 15.8) | Veteran | 66% female | 68.6% Caucasian; 17.8% African American; 4.3% Hispanic; 4.9% Asian/Pacific American; 1.1% Native American; 3.2% Other | M | Cross-sectional | 335 enrolled |
| Escalona et al. (2004)44 | New Mexico, USA | VA primary care | Urban | 23-85 years | Women veterans, with non-veteran spouses as controls | 100% female | 46% White; 30% Hispanic; 3% American Indian or Alaskan Native; 3% Black; 2% Asian or Pacific Islander; 1% Hispanic Black; 15% not reported | M | Retrospective | 601 approached, 334 enrolled |
| Magruder et al. (2005)45 | Charleston and Columbia, South Carolina; Tuscaloosa and Birmingham, Alabama, USA | VA primary care | Urban clinics covering populations of several southern states | 60.9 (SD 12.1) | Veteran | 7.9% female | 61% White | L | Cross-sectional | 1198 enrolled |
| Spiro et al. (2006)46 | Boston, Massachusetts, USA | VA system | Urban | Not reported | Veteran | 0% female | Not reported | L | Cross-sectional | 6829 patients approached 2425 enrolled |
| Seal et al. (2007)47 | USA | VA system | Not reported | 26% age 18-24; 28% age 25-29; 22% 30-39; 24% ≥40 | Veteran | 13% female | 69% White; 18% Black; 11% Hispanic; 2% other | M | Retrospective review of medical records | 165,351 screened |
| Funderburk et al. (2008)48, 49 | USA | VA primary care | Both | 62 (SD 16) | Veteran | 4% female | 93% White | M | Retrospective review of medical records | 86,326 screened |
| Kinder et al. (2008)50 | White River Junction, VT; Richmond, VA; Birmingham, AL; Little Rock, AK; Los Angeles and San Francisco CA; and Seattle, WA, USA | VA primary care | Both | 64 (SD 12) | Veteran | ∼4% female | ∼73% White | M | Retrospective review of medical records and self-report | 35,715 screened |
| Andersen et al. (2010)51 | Upstate New York, USA | VA primary care | Both | 68% ages 20-29 | Veteran | 11% female | 85% White; 8% Black; 3% Hispanic; 2% other; 1% unknown | L | Retrospective review of medical records | 4416 screened |
| Haskell et al. (2010)52 | Connecticut, USA | VA primary care and women's health | Both | 32 (SD not reported) | Veteran | 19% female | 11% Black; 64% White; 25% other | M | Retrospective review of medical records | 1129 screened |
| McDevitt-Murphy et al. (2010)53 | Memphis, Tennessee, USA | VA primary care | Urban | 34.5 (SD 9.4) | Veteran | 9.9% female | 62.3% White; 35.1% Black/African American | M | Cross-sectional | 74% response rate |
| Zivin et al. (2010)54 | USA | VA primary care | Both | 63.8 (SD not reported) | Veteran | 5% female | 58% White; 12% “nonwhite”; 30% unknown | M | Retrospective review of medical records | 2,536,727 screened |
| Mitchell et al. (2014)55 | Boston, MA, USA | VA primary care | Urban | 52.12 (SD 17.12) | Veteran | 100% female | 54.5% Cauc; 18.7% Af. Am; 1.4% Hisp/Lat; 1.8% Asian; 1.0% Native American/Pac. Islander; 22.5% unknown | M | Retrospective review of medical records | 492 screened |
| Mohanty et al. (2015)56 | USA | VA primary care | Both | Age at first VA visit 18.6-61.3yo | Veteran | 100% female | ∼40% Cauc; 19% Af. Am; 10% Hisp/Lat; 6.6% unknown | M | Retrospective review of medical records | 78,435 screened |
| Trivedi et al. (2015)57 | USA | VA primary care | Both | 57.3 (SD 13.8) if any mental illness | Veteran | 8.5% female if any mental illness | 72.3% Cauc; 19.7% Af. Am; 1.0% Hisp/Lat; 2.9% other; 4.2% unknown if any mental illness | M | Cross-sectional | 4,461,208 assessed |
| Wingenfeld et al. (2015)58 | San Francisco and Palo Alto, CA, USA | VA primary care | Urban | 58 (SD 11) | Veteran | 6.4% female | 57.2% Cauc | L | Cross-sectional | 1,020 assessed |
Risk of bias calculated using adapted Hoy et al.'s Risk of Bias Tool.15 Authors adapted ranges out of 9: score 7-9 low, 3-6 medium, and 0-2 high risk of bias.
Abbreviations: L: low risk of bias; M: medium risk of bias; N: number of subjects; USA: United States of America; VA: Veterans Affairs
Table 2. PTSD prevalence in primary care populations.
| Study | N of completed PTSD assessment | PTSD ascertainment tool | Mean questionnaire scores (SD) | Cutoff scores | Time period of PTSD symptoms measured | PTSD Prevalence | ||
|---|---|---|---|---|---|---|---|---|
| Point | Lifetime | Medical records/claims | ||||||
| Stein et al. (2000)17 | 368 | PCL-C | 29.7 (12.5) | 4 or 5 on at least 1 “B” criteria, at least 2 “C” criteria, and at least 1 “D” criteria | Past month | 9% | ||
| Applegate (2001)18 | 431 | DIS-IV | N/A | N/A | Past month | 10% | 21.6% | |
| Taubman-Ben-Ari et al. (2001)19 | 2,975 | PTSD Inventory from Soloman et al. 1987 59 | Not reported | Not reported | Past month | 23% | ||
| Carey et al. (2003)20 | 220 | Adapted CIDI | N/A | N/A | Past month | 19.9% (16.7% male, 21.9% female) | 44.3% (42.3% male; 45.5% female) | |
| Thulesius et al. (2004)21 | 1,113 | PTSS-10 and IES and 7 additional items re: hyperarousal symptoms | Not reported | >35 for IES and >5 for PTSS-10 | Past few days | 6.5% | ||
| Gillock et al. (2005)22 | 232 | PCL-C plus additional items to assess DSM-IV criteria E and F “Life Events Checklist” | Not reported | If met criteria A through F | Past month | 9% full PTSD/25% partial PTSD | ||
| Gomez-Benevto et al. (2006)23 | 295 | CIDI | N/A | N/A | Past month and lifetime | 9% | 14.5% | |
| Kroenke et al. (2007)24 | 965 | SCID | N/A | N/A | Past month | 8.6% | ||
| Liebschutz et al. (2007)25 | 509 | CIDI | N/A | N/A | “[C]urrent past 12 mo and lifetime PTSD documented from CIDI” | 23% (95% CI,19-26%) | 34% | 11% |
| Peltzer et al. (2007)26 | 250 | PCL-C, interview administered; Trauma History Questionnaire | M 3.5 (SD not provided) | 3+ (“cluster scoring”) | Past month | 12.4% | ||
| Cwikel et al. (2008)27 | 976 | “PTSD Checklist--21 items” | Not reported | Not reported | Not reported | 2.9% | ||
| Fedovskiy et al. (2008)28 | 105 | Posttraumatic Stress Diagnostic Scale “structured interview” | Not reported | ≥28 out of 49 | Past month | 19% | ||
| Fogarty et al. (2008)29 | 367 | Short screen from Breslau et al.60 | Not reported | 4+ | Past month | 14.6% | ||
| Duran et al. (2009)30 | 234 | CIDI | N/A | N/A | Past year | 14.5% | ||
| Freedy et al. (2010)31 | 411 | CAPS (modified for telephone interview rather than face-to-face) | N/A | N/A | Past month | 32.1% (19.4% male; 34.8% female) | ||
| Gaynes et al. (2010)32 | 647 | MINI | Not reported | ≥ 2 | Past month | 6.3% | ||
| Wrenn et al. (2011)33 | 767 | PSS | Not reported | “A categorical variable that serves as a proxy for PTSD was created based on DSM-IV A-E criterion responses to the PSS questionnaire (A, presence of trauma; B, presence of at least 1 intrusive symptoms; C, presence of at lease 3 avoidance/numbing symptoms; and D, presence of at least 2 hyperarousal symptoms; and E, present for at least 1 month).” | Past month | 30% | ||
| Vera et al. (2012)34 | 3,568 | PC-PTSD | Not reported | 3+ | Past month | 14% | ||
| Bunevicius et al. (2014)35 | 988 | MINI | Not reported | Not reported | Past two weeks | 2% | ||
| Preville et al. (2014)36 | 1,765 | PTSS Scale | 7.5 (9.6) | 10 | 6-months | 11.1% | ||
| Bener et al. (2015)37 | 1475 | Arabic WMH-CIDI-10 (verson 3.0) | N/A | N/A | Past month | 10.5% | ||
| Special Risk Populations (Refugee/Immigrant) | ||||||||
| Eisenman et al. (2003)38 | 512 | PCL-C | Not reported | Not reported | Past month | 12.5% (18% if exposed to violence, 8% if not exposed) | ||
| Eytan et al. (2007)39 | 101 | Adapted MINI | 1st criteria 83%, 2nd criteria 59%, 3rd avoidance 28%, 4th criteria 24%, 5th criteria 24% | Not reported | Past month | 23.8% | ||
| Aragona et al. (2013)40 | 391 | Harvard Trauma Questionnaire | Not reported | 2.5 | Past month | 10.2% | ||
| Veterans | ||||||||
| Dobie et al. (2002)41 | 282 | CAPS | N/A | N/A | Past month | 36% | ||
| Mori et al. (2003)42 | 309 | BAI-PC | BAI-PC mean 4.27 range 0-21 | BAI-PC cutoff 5 and above; PCL ≥50 | “Current PTSD” | 12% | ||
| Prins et al. (2003)43 | 167 | CAPS | N/A | N/A | Past month | 24.5% | ||
| Escalona et al. (2004)44 | 264 (134 veterans and 130 non-veteran controls) | CIDI | N/A | N/A | Lifetime | 27% | ||
| Magruder et al. (2005)45 | 746 | CAPS | N/A | N/A | Past month | 11.5% | ||
| Spiro et al. (2006)46 | 2,262 | PCL-M | PTSD+ M=56.1, SD=12.3, range 31-85 (does not list these measures for the group as a whole) | Not reported | Past month | 20% | ||
| Seal et al. (2007)47 | 103,788 | Medical record review, ICD-9 code | N/A | N/A | Diagnosis present in the medical record | 13% | ||
| Funderburk et al. (2008)48 | 10,043 | PC-PTSD | Not reported | ≥3 means “at risk” | Past month | 3.5% | ||
| Kinder et al. (2008)50 | 35,715 | ICD-9 or self-report | N/A | N/A | Lifetime | 12.1% | ||
| Andersen et al. (2010)51 | 4,416 | Medical record review, ICD-9 dx by primary care provider | N/A | N/A | Past month symptoms, screen given yearly, diagnosed within 6 years of the study | 14.5% | ||
| Haskell et al. (2010)52 | 1,129 | PC-PTSD | Not reported | ≥3 means “at risk” | Past month | 31.1% (33% male; 21% female) | ||
| McDevitt-Murphy et al. (2010)53 | 151 | PCL-M | Not reported | 50 | Past month | 39.1% | ||
| Zivin et al. (2010)54 | 2,536,727 | Medical record review, dx method not reported | N/A | N/A | Diagnosis present in the medical record | 4.2% | ||
| Mitchell et al. (2014)55 | 492 | Medical record review, ICD-9 code | N/A | N/A | Diagnosis present in the medical record | 26.8% | ||
| Mohanty et al. (2015)56 | 78,435 | Medical record review, ICD-9 code | N/A | N/A | Diagnosis present in the medical record | 29.2% | ||
| Trivedi et al. (2015)57 | 4,461,208 | Medical record review, ICD-9 code | N/A | N/A | Diagnosis present in the medical record | 9% | ||
| Wingenfeld et al. (2015)58 | 613 | CAPS | N/A | N/A | Past month and lifetime | 32.5% | 48.8% | |
Abbreviations: BAI-PC: Beck Anxiety Inventory-Primary Care; BPHQ: Brief Patient Health Questionnaire; CAPS: Clinician-Administered PTSD Scale; CIDI: Composite International Diagnostic Interview; DIS-IV: diagnostic interview schedule for DSM-IV; DSM-IV: Diagnostic and Statistical Manual, fourth edition; Dx: diagnosis; ICD-9: International Classification of Diseases, Ninth Revision; IES: Impact of Event Scale; MINI: Mini-international Neuropsychological Interview; PC-PTSD: Primary Care PTSD Screen; PCL-C: PTSD checklist-civilian; PCL-M: PTSD checklist-military; PTSS: Post Traumatic Stress Syndrome; PCL: PTSD checklist; PTSD: Posttraumatic stress disorder; PTSS-10: Posttraumatic Stress Syndrome-10; SCID: Structured Clinical Interview; VA: Veterans Affairs; WMH: World Mental Health
Study designs included 30 cross-sectional studies and 11 retrospective reviews of the medical records.
The point prevalence of PTSD diagnosis ascertained by diagnostic interviews (e.g., Structured Clinical Interview [SCID], Diagnostic Interview Schedule [DIS], Composite International Diagnostic Interview [CIDI], Mini-international Neuropsychological Interview [MINI], Clinician-Administered PTSD Scale [CAPS]) ranged from 2% to 32.5% (17 studies18, 20, 23-25, 28, 30-32, 35, 37, 39, 41, 43-45, 58). The point prevalence of substantial PTSD/clinically important PTSD symptoms based on questionnaire thresholds ranged from 2.9% to 39.1% (15 studies17, 19, 21, 22, 26, 27, 33, 38, 40, 42, 46, 53,29, 34, 36). The median point prevalence of PTSD in all primary care samples was 12.5% (civilian population median [N = 21]: 11.1%, special risk population median [N = 3]: 12.5%, and veteran median [N = 7]: 24.5%).
The prevalence of PTSD in administrative data-based studies ranged from 3.5% to 48.8% (11 studies25, 47, 48, 51, 52, 54, 25, 50, 55-57). Finally, the lifetime prevalence of PTSD diagnosis based on diagnostic interviews ranged from 14.5% to 48.7% (6 studies18, 20, 23, 25, 44, 58).
Several potential risk factors for PTSD in primary care populations were identified. In studies reporting separate results for PTSD point prevalence for men and women, women were more likely to have PTSD in civilian populations,20, 31 while men were more likely to have lifetime PTSD in one veteran population.52 Populations with known prior exposure to violence generally had higher rates of PTSD than those without prior exposure to violence.38
The PTSD Checklist (PCL) (6 studies)17, 22, 26, 38, 46, 53 and the Composite International Diagnostic Interview (CIDI) (6 studies)20, 23, 25, 30, 37, 44 were the diagnostic tools most often used. The PCL is a screening measure while CIDI is a structured clinical diagnostic interview. Risk of bias in all studies remained medium to low (reported individually in Table 2) and trends in a relationship between bias score and prevalence rate were not apparent.
Discussion
This systematic review highlights several key features of PTSD in primary care settings. First, the point prevalence of PTSD was much higher than the one-year general population prevalence of PTSD found by the NCS-R6 indicating that primary care is an especially important setting in which to identify and manage PTSD.
Additionally, there was a very wide range in the prevalence of PTSD found in the included studies, similar to the wide range found by Greene et al.13 Greene et al. note that the significant heterogeneity apparent in their findings was a result of “samples with different levels of trauma exposure.”13 Another reason for this heterogeneity may be that populations could have trauma exposure but have sufficient protective factors (e.g. secure attachment relationships to process the traumatic experiences)61-63 mitigating the risk for development of PTSD symptoms. Additionally, many people who experience trauma and suffer from mental health effects of trauma do not fit the criteria for PTSD (e.g. chronic childhood abuse experiences, ongoing domestic violence experiences).1 Our findings suggest that level of trauma exposure specific to the diagnosis of PTSD is likely one factor contributing to this heterogeneity as studies of veterans generally had higher PTSD reported (median 24.5%) than those of civilians (median 11.1%) or special risk (refugee/immigrant) primary care samples (median 12.5%). We additionally identified several reasons that may account for this range, including varying methods of case ascertainment (various scales with different cut off scores, structured interviews, and chart reviews) or unmeasured differences between study populations (e.g. location, age, other untracked demographic factors, or selection factors [patient refusal rates, random versus consecutive sampling]).
Specific risk factors identified for various populations include women being more likely to have PTSD in civilian populations. This finding might suggest that women experience more trauma than men in civilian populations (e.g. are more often subject to domestic violence), or have less access to protective factors. Men were found to have more lifetime PTSD in one large veteran population study; the timeframe of PTSD symptoms might be important to consider (e.g. veterans may return from combat without expressing PTSD symptoms which may develop later in life). It makes intuitive sense that populations with known prior exposure to violence were generally found to have higher PTSD prevalence.
We assessed for meaningful differences of methodology and found that diagnostic interview and questionnaire threshold PTSD diagnosis studies exhibited very similar ranges, suggesting that questionnaires might be similarly effective in identifying PTSD when compared to diagnostic interviews. Median PTSD prevalence was calculated to summarize the data with the caveat that individual primary care clinics may be best served to find studies examining populations with characteristics similar to themselves in order to estimate their PTSD prevalence.
The findings reveal that although primary care PTSD prevalence reports vary greatly, PTSD in this setting is common (regardless of the type of population [i.e., civilians versus veterans]) with the median prevalence approximating that of depression.64, 65 Given the growing understanding of mental and physical adverse effects of traumatic stress,7, 66, 67 it is important to use a standard screening tool, and then develop clear and feasible clinical guidelines based on the available evidence, with regards to the management of PTSD in the primary care setting. A systematic review of PTSD interventions in medical settings is needed to help further our understanding of evidence-based PTSD management.
Although guidelines for depression treatment in primary care settings have been developed, relatively few guidelines have been designed to address the management of PTSD in primary care. In the U.S., a pragmatic treatment algorithm exists with guidelines for mental health prescribers for treating PTSD and is based on a literature review and the experience within one practice setting;68 however, this is not a primary care-based program nor has it been tested in primary care or for use by non-mental health specialists.
The collaborative care model or other primary care interventions may have the potential of addressing the treatment needs of those with PTSD in primary care settings. The effectiveness of collaborative care treatment for depression in primary care is well established.69, 70 There is some preliminary evidence including three randomized controlled trials indicating that collaborative care may be an effective intervention for PTSD in primary care;10, 71-74 and some evidence that other interventions in primary care may be equally or more effective than collaborative care.75, 76 One randomized controlled trial found that patients who attended eight cognitive processing therapy (CPT) sessions in addition to usual care by a primary care clinician had equal improvement to patients who received extensive telemedicine collaborative care interventions.71 This finding might reflect that patients who are able to tolerate eight therapy sessions are a self-selecting population who is more able to engage in treatment, or it might indicate that therapy is the mainstay of treatment for PTSD. Another randomized controlled trial found that patients receiving a “minimally enhanced usual care intervention” consisting of primary care clinician education about “trauma, PTSD, and evidence-based psychopharmacology” resulted in improvement greater than those receiving a more traditional and resource intensive collaborative care intervention.76 This surprising finding may indicate that treatment with a provider whom the patient is comfortable and has an already-established relationship is more successful than more intensive treatment with a new team, and suggests that psychoeducation and medication education for primary care physicians may be a cost effective method of treating patients with PTSD. However, decreased PTSD symptoms were noted for all groups in the study, and improvements in the “minimally enhanced usual care” group were not overwhelmingly different than the collaborative care group.76 It seems that attention to this diagnosis is likely helpful, and that researchers have yet to determine the specific clinical treatment that works best. Given the high prevalence of PTSD in primary care and the lack of specialty mental health providers to adequately manage PTSD, more studies of types of collaborative care or other interventions for this condition in primary care settings are needed to better understand how to optimally meet the needs of this population. Trauma expert Judy Herman offers the following general guideline “[t]he core experiences of psychological trauma are disempowerment and disconnection. Recovery, therefore, is based upon the empowerment of the survivor and the creation of new connections. Recovery can take place only within the context of relationships; it cannot occur in isolation.”1 Researchers and clinicians may need to shift from focusing on individual patient treatment to facilitating greater psychological connections for these patients.
Neglecting mental health treatment for this population may make common medical conditions more difficult to manage. For instance, the original ACEs study showed a direct relationship between high numbers of adverse childhood experiences and increased risks for liver disease, ischemic heart disease, cancer, chronic lung disease, and skeletal fractures.7 While adverse events do not always result in PTSD this is an example of how emotional adversity correlates with long-term physical illness. A recent study showed that women with PTSD have nearly twice the likelihood of developing Type-2 diabetes.66 Furthermore, women with increased PTSD symptom severity were found to have a 104% increase in healthcare costs versus women with low severity of PTSD symptoms or those with no symptoms.67
While there are not yet studies of interventions for PTSD treatment that have shown a decrease in burden of physical disease, the collaborative care literature points to the benefit of addressing physical comorbidities with specific psychiatric diagnosis. The depression literature reveals that a collaborative care intervention targeting depression, glucose control in diabetes, hypertension and hyperlipidemia led to improvement in all outcomes.77 The Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) trial found that geriatric patients with depressive disorders receiving the collaborative care intervention had improved depression physical functioning78 and had reduced costs due to hospitalizations for medical illnesses.79 In a secondary analysis of the Communication and Low Mood (CALM) trial, the authors reported that treatment of anxiety improves self-reported physical functioning as measured by the twelve-item Short Form Survey (SF-12) (included here with the caveat that outcome assessment was manipulated in order to yield a significant finding).80
Primary care providers have the capacity to fill the gap between mental health need and mental health care availability.76 Primary care providers can use a screening tool such as the PTSD symptom checklist-civilian (PCL-C, 17 questions) or the PC-PTSD (4 questions) (both showed >80% sensitivity and specificity)31 to help identify possible PTSD in patients presenting with symptoms of anxiety or depression who have a history of trauma exposure. Following a positive PTSD screen and warranted diagnostic assessment to confirm a positive screen, primary care providers can prescribe prazosin for nightmares, serotonin reuptake inhibitors (paroxetine and sertraline are the only medications that are FDA approved for PTSD treatment) and/or venlafaxine as evidence-based options that have been shown to have efficacy for PTSD, and refer for appropriate therapy if the patient is agreeable to this intervention.68 Additionally, the United Kingdom National Institute for Health and Clinical Excellence (NICE) PTSD guidelines suggest trauma focused psychological therapy for all following a positive screen, prior to prescribing medications.8 Access to these therapies likely varies greatly between primary care clinical sites. Mental health providers are increasingly integrated into primary care sites and can be part of a “stepped care” model for patients who do not respond to initial interventions offered by primary care clinicians.81 Future studies should consider using a standardized screening tool, such as the PC-PTSD used in VA healthcare.
This review has several limitations. Despite efforts to comprehensively review multiple databases, relevant articles may have been missed due to inconsistent indexing in electronic databases. Articles not written in English were excluded due to difficulties accessing and/or translating findings, further increasing the risk of missing relevant articles and making this review more applicable to populations served by English speaking clinicians. Included studies had varying designs and therefore multiple methodological limitations. Ranges and medians of PTSD prevalence rather than means are reported due to the great variation in study designs, limiting generalizability of findings. Therefore, clinicians may be best served by reviewing the studies included that have similar demographics to those at their practice sites. The major strength of this study is the extensiveness of the search methodology. While the previously carried out Greene13 study had a similar focus to the present study, our study is significantly more systematic, including not just two databases but five; using MeSH terms to include more in the search results, and having a longer overall timeframe.
Conclusion
This systematic review identified that the prevalence of PTSD in primary care settings is varied greatly, ranging from 2% to 39.1%, but with a median point prevalence of 12.5%, similar to that of depression. Establishing a median prevalence is important for those working with primary care populations as they will be able to practically compare their clinic prevalence with one that might be expected, and target screening and/or treatment interventions accordingly. In light of the public health costs of PTSD, additional research is needed to examine and explore optimal management of PTSD in primary care settings, given the growing literature on this topic.
Acknowledgments
The authors would like to acknowledge Michelle Davids for her thoughtful review of the manuscript for which no compensation was received. The authors acknowledge the late Wayne Katon, MD, (1950-2015) for his support of this project.
Support: Margaret Spottswood has no funding to acknowledge. Hsiang Huang was supported by the Fulbright Scientific Mobility Program. Dimitry Davydow was supported by grant KL2 TR000421 from the National Institutes of Health. These funders were not involved in developing the protocol. The research was supported by the following grant from the Health Services Division of NIMH: T32 MH20021-14 (Dr. Katon).
Footnotes
Contributions: Dr. Spottswood performed the literature search and reviewed the studies and wrote the initial manuscript. Dr. Huang provided guidance during the initial review process, reviewed the studies and provided input on subsequent drafts of the manuscript. Dr. Davydow provided expertise in the area of PTSD and screening tools and input on subsequent drafts of the manuscript. Dr. Spottswood is the guarantor of the review.
Amendments: This protocol is the original protocol developed by the authors.
Prior presentations: A portion of this project (point prevalence only of preliminary data) was presented as a poster for the Academy of Psychosomatic Medicine Annual Meeting November 11-14, 2015.
Conflict of interest: Margaret Spottswood has no conflicts of interest to declare. Hsiang Huang has no conflicts of interest to declare. Dimitry Davydow has no conflicts of interest to declare.
References
- 1.Herman J. Trauma and Recovery: The aftermath of violence--from domestic abuse to political terror. 2nd. New York: Basic Books; 1997. [Google Scholar]
- 2.Zatzick DF, Rivera FP, Nathens AB, Jurkovich GJ, Wang J, Fan MY, Russo J, Salkever DS, Mackenzie EJ. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychol Med. 2007;37(10):1469–1480. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]
- 3.Davydow DS, Gifford EM, Desai SV, Needham DM, Bienvenu OJ. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry. 2008;30(5):421–434. doi: 10.1016/j.genhosppsych.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diagnostic and Statistical Manual of Mental Disorders. Vol. 5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 5.Kessler RC, Berglund P, Delmer O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 8.(NCCMH) TNCCfMH, editor. NICE clinical guideline. Vol. 26. Leicester and London, UK: The British Psychological Society and the Royal College of Psychiatrists; Mar, 2005. Post-traumatic Stress Disorder: the Management of PTSD in Adults and Children in Primary and Secondary Care. 2005. [PubMed] [Google Scholar]
- 9.Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C Investigators. I. Improving Mood-Promoting Access to Collaborative Treatment. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 10.Roy-Byrne PP, Craske MG, Sullivan G, Rose RD, Edlund MJ, Lang AJ, Bystritsky A, Welch SS, Chavira DA, Golinelli D, Campbell-Sills L, Sherbourne CD, Stein MB. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303(19):1921–1928. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prins A, Bovin M, Smolenski D, Marx B, Kimerling R, Jenkins-Guarnieri M, Kaloupek D, Schnurr PP, Kaiser A, Leyva Y, Tiet QQ. The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and Evaluation Within a Veteran Primary Care Sample. J Gen Intern Med. 2016 doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belsher B, J L, Freed MC, Evatt D, Liu X, Novak L, Zatzick DF, Bray RM, Engel C. Mental Health Utilization Patterns During a Stepped, Collaborative Care Effectiveness Trial for PTSD and Depression in the Military Health System. Medical Care. 2016;54(7):706–713. doi: 10.1097/MLR.0000000000000545. [DOI] [PubMed] [Google Scholar]
- 13.Greene T, Neria Y, Gross R. Prevalence, Detection and Correlates of PTSD in the Primary Care Setting: A Systematic Review. J Clin Psychol Med Settings. 2016;23:160–180. doi: 10.1007/s10880-016-9449-8. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 15.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Cerimele JM, Chwastiak LA, Dodson S, Katon WJ. The prevalence of bipolar disorder in primary care patients with depression or other psychiatric complaints: a systematic review. Psychosomatics. 2013;54(6):515–524. doi: 10.1016/j.psym.2013.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stein MB, McQuaid JR, Pedrelli P, Lenox R, McCahill ME. Posttraumatic Stress Disorder in the Primary Care Medical Setting. General Hospital Psychiatry. 2000;22(4):261–269. doi: 10.1016/s0163-8343(00)00080-3. [DOI] [PubMed] [Google Scholar]
- 18.Applegate BW. Traumatic Life Events, Posttraumatic Stress Disorder, and Health Outcomes in a Low-income, Primary Care Population. Dissertation Submitted to the Graduate Faculty of the Louisiana State University. 2000:1–92. [Google Scholar]
- 19.Taubman-Ben-Ari O, Rabinowitz J, Feldman D, Vaturi R. Post-traumatic stress disorder in primary-care settings: prevalence and physicians' detection. Psychological Medicine. 2001;31(3):555–560. doi: 10.1017/s0033291701003658. [DOI] [PubMed] [Google Scholar]
- 20.Carey P, Stein D, Zungu-Dirwayi N, Seedat S. Trauma and Posttraumatic Stress Disorder in an Urban Xhosa Primary Care Population: Prevalence, Comorbidity, and Service Use Patterns. The Journal of Nervous and Mental Disease. 2003;191(4):203–236. doi: 10.1097/01.NMD.0000061143.66146.A8. [DOI] [PubMed] [Google Scholar]
- 21.Thulesius H, Alveblom AK, Hakansson A. Post-traumatic stress associated with low self-rated well-being in primary care attenders. Nord J Psychiatry. 2004;58(4):261–266. doi: 10.1080/08039480410005765. [DOI] [PubMed] [Google Scholar]
- 22.Gillock KL, Zayfert C, Hegel MT, Ferguson RJ. Posttraumatic stress disorder in primary care: prevalence and relationships with physical symptoms and medical utilization. Gen Hosp Psychiatry. 2005;27(6):392–399. doi: 10.1016/j.genhosppsych.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Gomez-Beneyto M, Salazar-Fraile J, Marti-Sanjuan V, Gonzalez-Lujan L. Posttraumatic stress disorder in primary care with special reference to personality disorder comorbidity. British Journal of General Practice. 2006;56(526):349–354. [PMC free article] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer R, Williams J, Monahan P, Lowe B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Annals of Internal Medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 25.Liebschutz J, Saitz R, Brower V, Keane TM, Lloyd-Travaglini C, Averbuch T, Samet JH. PTSD in urban primary care: high prevalence and low physician recognition. J Gen Intern Med. 2007;22(6):719–726. doi: 10.1007/s11606-007-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peltzer K, Naidoo P, Matseke G, Louw J, McHunu G, Tutshana B. Prevalence of post-traumatic stress symptoms and associated factors in tuberculosis (TB), TB retreatment and/or TB-HIV co-infected primary public health-care patients in three districts in South Africa. Psychol Health Med. 2013;18(4):387–397. doi: 10.1080/13548506.2012.726364. [DOI] [PubMed] [Google Scholar]
- 27.Cwikel J, Zilber N, Feinson M, Lerner Y. Prevalence and risk factors of threshold and sub-threshold psychiatric disorders in primary care. Soc Psychiatry Psychiatr Epidemiol. 2008;43(3):184–191. doi: 10.1007/s00127-007-0286-9. [DOI] [PubMed] [Google Scholar]
- 28.Fedovskiy K, Higgins S, Paranjape A. Intimate partner violence: how does it impact major depressive disorder and post traumatic stress disorder among immigrant Latinas? J Immigr Minor Health. 2008;10(1):45–51. doi: 10.1007/s10903-007-9049-7. [DOI] [PubMed] [Google Scholar]
- 29.Fogarty CT, Sharma S, Chetty VK, Culpepper L. Mental Health Conditions are Associated With Increased Health Care Utilization Among Urban Family Medicine Patients. JABFM. 2008;21(5):398–407. doi: 10.3122/jabfm.2008.05.070082. [DOI] [PubMed] [Google Scholar]
- 30.Duran B, Oetzel J, Parker T, Malcoe LH, Lucero J, Jiang Y. Intimate Partner violence and Alcohol, drug, and mental disorders among american indian women from southwest tribes in primary care. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 2009;16(2):11–27. doi: 10.5820/aian.1602.2009.11. [DOI] [PubMed] [Google Scholar]
- 31.Freedy JR, Steenkamp MM, Magruder KM, Yeager DE, Zoller JS, Hueston WJ, Carek PJ. Post-traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010;27(6):615–624. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- 32.Gaynes BN, DeVeaugh-Geiss J, Weir S, Gu H, MacPherson C, Schulberg HC, Culpepper L, Rubinow DR. Feasibility and Diagnostic Balidity of the M-3 Checklist: A Brief, Self-Rated Screen for Depressive, Bipolar, Anxiety, and Post-Traumatic Stress Disorders in Primary Care. Annals of Family Medicine. 2010;8(2):160–169. doi: 10.1370/afm.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wrenn GL, Wingo AP, Moore R, Pelletier T, Gutman AR, Bradley B, Ressler KJ. The Effect of Resilience on Posttraumatic Stress Disorder in Trauma-Exposed Inner-City Primary Care Patients. J Natl Med Assoc. 2011;103(7):560–566. doi: 10.1016/s0027-9684(15)30381-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vera M, Juarbe D, Hernandez N, Oben A, Perez-Pedrogo C, Chaplin WF. Probable Posttraumatic Stress Disorder and Psychiatric Co-morbidity among Latino Primary Care Patients in Puerto Rico. J Depress Anxiety. 2012;1(5):124. doi: 10.4172/2167-1044.1000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bunevicius R, Liaugaudaite V, Peceliuniene J, Raskauskiene N, Bunevicius A, Mickuviene N. Factors affecting the presence of depression, anxiety disorders, and suicidal ideation in patients attending primary health care service in Lithuania. Scand J Prim Health Care. 2014;32(1):24–29. doi: 10.3109/02813432.2013.873604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Preville M, Lamoureux-Lamarche C, Vasiliadis H, Grenier S, Potvin O, Quesnel L, Gontijo-Guerra S, Machakra-Tahiri SD, Berbiche D. The 6-Month Prevalence of Posttraumatic Stress Syndrome (PTSS) Among Older Adults: Validity and REliability of the PTSS Scale. Can J Psychiatry. 2014;59(10):548–555. doi: 10.1177/070674371405901008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bener A, Abou-Saleh M, Dafeeah E, Bhugra D. The Prevalence and Burden of Psychiatric Disorders in Primary Health Care Visits in Qatar: Too Little Time? Journal of Family Medicine and Primary Care. 2015;4(1):89–95. doi: 10.4103/2249-4863.152262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eisenman D, Gelberg L, Liu H, Shapiro M. Mental Health and Health-Related Quality of Life Among Adult Latino Primary Care Patients Living in the United States With Previous Exposure to Political Violence. JAMA. 2003;290(5):627–634. doi: 10.1001/jama.290.5.627. [DOI] [PubMed] [Google Scholar]
- 39.Eytan A, Durieux-Paillard S, Whitaker-Clinch B, Loutan L, Bovier PA. Transcultural validity of a structured diagnostic interview to screen for major depression and posttraumatic stress disorder among refugees. J Nerv Ment Dis. 2007;195(9):723–728. doi: 10.1097/NMD.0b013e318142c9f6. [DOI] [PubMed] [Google Scholar]
- 40.Aragona M, Pucci D, Mazzetti M, Maisano B, Geraci S. Traumatic events, post-migration having difficulties and post-traumatic symptoms in first generation immigrants: a primary care study. Ann Ist Super Sanita. 2013;201349(2):169–175. doi: 10.4415/ANN_13_02_08. [DOI] [PubMed] [Google Scholar]
- 41.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, McFall M, Epler AJ, Bradley KA. Screening for post-traumatic stress disorder in female Veteran's Affairs patients; validation of the PTSD checklist. General Hospital Psychiatry. 2002;24(6):367–374. doi: 10.1016/s0163-8343(02)00207-4. [DOI] [PubMed] [Google Scholar]
- 42.Mori DL, Lambert JF, Niles BL, Orlander JD, Grace M, LoCastro JS. The BAI-PC as a Screen for Anxiety, Depression, and PTSD in Primary Care. Journal of Clinical Psychology in Medical Settings. 2003;10(3):187–192. [Google Scholar]
- 43.Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, Sheikh JI. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9(1):9–14. [Google Scholar]
- 44.Escalona R, Achilles G, Waitzkin H, Yager J. PTSD and somatization in women treated at a VA primary care clinic. Psychosomatics. 2004;45(4):291–296. doi: 10.1176/appi.psy.45.4.291. [DOI] [PubMed] [Google Scholar]
- 45.Magruder KM, Frueh BC, Knapp RG, Davis L, Hamner MB, Martin RH, Gold PB, Arana GW. Prevalence of posttraumatic stress disorder in Veterans Affairs primary care clinics. Gen Hosp Psychiatry. 2005;27(3):169–179. doi: 10.1016/j.genhosppsych.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 46.Spiro A, Hankin C, Mansell D, Kazis L. Posttraumatic Stress Disorder and Health Status: The Veterans Health Study. J Ambulatory Care Manage. 2005;29(1):71–86. doi: 10.1097/00004479-200601000-00008. [DOI] [PubMed] [Google Scholar]
- 47.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar CR. Bringing the War Back Home: Mental Health Disorders Among 103,788 US Veterans Returning From Iraq and Afghanistan Seen at Department of Veterans Affairs Facilities. Arch Intern Med. 2007;167(5):476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 48.Funderburk JS, Maisto SA, Sugarman DE, Wade M. The covariation of multiple risk factors in primary care: a latent class analysis. J Behav Med. 2008;31(6):525–535. doi: 10.1007/s10865-008-9176-1. [DOI] [PubMed] [Google Scholar]
- 49.Sugarman DE. Conversation pertaining to 2008 paper “The covariation of multiple risk factors in primary care: a latent class analysis”. In: Spottswood M, editor. Telephone conversation. 2015. [DOI] [PubMed] [Google Scholar]
- 50.Kinder LS, Bradley KA, Katon W, Ludman EJ, McDonell MB, Bryson CL. Depression, Posttraumatic Stress Disorder, and Mortality. Psychosom Med. 2008;70:20–26. doi: 10.1097/PSY.0b013e31815aac93. [DOI] [PubMed] [Google Scholar]
- 51.Andersen J, Wade M, Possemato K, Ouimette P. Association between posttraumatic stress disorder and primary care provider-diagnosed disease among Iraq and Afghanistan veterans. Psychosom Med. 2010;72(5):498–504. doi: 10.1097/PSY.0b013e3181d969a1. [DOI] [PubMed] [Google Scholar]
- 52.Haskell S, Gordon K, Mattocks K, Duggal M, Erdos J, Justice A, Bradndt C. Gener Differences in Rates of Depression, PTSD, Pain, Obesity, and Military Sexual Trauma Among Connecticut War Veterans of Iraq and Afghanistan. Journal of Women's Health. 2010;19(2):267–271. doi: 10.1089/jwh.2008.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG. PTSD symptoms, hazardous drinking, and health functioning among U.S.OEF and OIF veterans presenting to primary care. J Trauma Stress. 2010;23(1):108–111. doi: 10.1002/jts.20482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zivin K, Pfeiffer P, Szymanski B, Valenstein M, Post E, Miller E, McCarthy J. Initiation of Primary Care--Mental Health Integration Programs in the VA Health System. Medical Care. 2010;48(9):843–851. doi: 10.1097/MLR.0b013e3181e5792b. [DOI] [PubMed] [Google Scholar]
- 55.Mitchell KS, Rasmusson A, Bartlett B, Gerber MR. Eating disorders and associated mental health comorbidities in female veterans. Psychiatry Research. 2014;219:589–591. doi: 10.1016/j.psychres.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohanty AF, Muthukutty A, Carter ME, Palmer MN, Judd J, Helmer D, McAndrew LM, Garvin JH, Samore MH, Gundlapalli AV. Chronic Multisymptom Illness Among Female Veterans Deployed to Iraq and Afghanistan. Medical Care. 2015;4(S1):S143–148. doi: 10.1097/MLR.0000000000000314. [DOI] [PubMed] [Google Scholar]
- 57.Trivedi R, Post E, Sun H, Pomerantz A, Saxon A, Piette J, Maynard C, Arnow B, Curtis I, Fihn S, Nelson K. Prevalence, Comorbidity, and Prognosis of Mental Health Among US Veterans. American Journal of Public Health. 2015;105(12):2564–2569. doi: 10.2105/AJPH.2015.302836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wingenfeld K, Whooley MA, Neylan TC, Otte C, Cohen BE. Effect of current and lifetime posttraumatic stress disorder on 24-h urinary catecholamines and cortisol: Results from the Mind Your Health Study. Psychoneuroendocrinology. 2015;52:83–91. doi: 10.1016/j.psyneuen.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Solomon Z, Weisenberg M, Schwarzwald J, Mikulincer M. Posttraumatic stress disorder among frontline soldiers with combat stress reaction: the 1982 Israeli experience. Am J Psychiatry. 1987;144(4):448–454. doi: 10.1176/ajp.144.4.448. [DOI] [PubMed] [Google Scholar]
- 60.Breslau N, Peterson EL, K RC, Schultz LR. Short screening scale for DSM-IV posttraumatic stress disorder. Am J Psychiatry. 1999;156(6):908–911. doi: 10.1176/ajp.156.6.908. [DOI] [PubMed] [Google Scholar]
- 61.Escolas SM, Arata-Maiers R, Hildebrandt EJ, Maiers AJ, Mason ST, Baker MT. The impact of attachment style on posttraumatic stress disorder symptoms in postdeployed service members. US Army Med Dep J. 2012 Jul-Sep;:54–61. [PubMed] [Google Scholar]
- 62.Declercq F, Palmans V. Two subjective factors as moderators between critical incidents and the occurrence of post traumatic stress disorders: adult attachment and perception of social support. Psychol Psychother. 2006;79(Pt 3):323–337. doi: 10.1348/147608305X53684. [DOI] [PubMed] [Google Scholar]
- 63.Armour C, Elklit A, Shevlin M. Attachment typologies and posttraumatic stress disorder (PTSD), depression and anxiety: a latent profile analysis approach. Eur J Psychotraumatol. 2011;2 doi: 10.3402/ejpt.v2i0.6018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry. 1992;14(4):237–247. doi: 10.1016/0163-8343(92)90094-q. [DOI] [PubMed] [Google Scholar]
- 65.Craven MA, Bland R. Depression in Primary Care: Current and Future Challenges. Canadian Journal of Psychiatry. 2013;2013(58):8. doi: 10.1177/070674371305800802. [DOI] [PubMed] [Google Scholar]
- 66.Roberts AL, Agnew-Blais JC, Spiegelman D, Kubzansky LD, Mason SM, Galea S, Hu FB, Rich-Edwards JW, Koenen KC. Posttraumatic Stress Disorder and Incidence of Type 2 Diabetes Mellitus in a Sample of Women: A 22-Year Longitudinal Study. JAMA Psychiatry. 2015 doi: 10.1001/jamapsychiatry.2014.2632. Published Last Modified Date|. Accessed Dated Accessed|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Walker EA, Katon W, Russo J, Ciechanowski P, Newman E, Wagner AW. Health care costs associated with posttraumatic stress disorder symptoms in women. Arch Gen Psychiatry. 2003;60(4):369–374. doi: 10.1001/archpsyc.60.4.369. [DOI] [PubMed] [Google Scholar]
- 68.Bajor LA, Ticlea AN, Osser DN. The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An Update on Posttraumatic Stress Disorder. Harvard Review of Psychiatry. 2011;19:240–258. doi: 10.3109/10673229.2011.614483. [DOI] [PubMed] [Google Scholar]
- 69.Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight-Eily LR, Chapman DP, Abraido-Lanza AF, Pearson JL, Anderson CW, Gelenberg AJ, Hennessy KD, Duffy FF, Vernon-Smiley ME, Nease DE, Jr, Williams SP Community Preventive Services Task F. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42(5):525–538. doi: 10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 70.Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, Dickens C, Coventry P. Collaborative care for depression and anxiety problems. The Cochrane Library. 2012;(10):1–277. doi: 10.1002/14651858.CD006525.pub2. [DOI] [PubMed] [Google Scholar]
- 71.Fortney JC, Pyne JM, Kimbrell TA, Hudson TJ, Robinson DE, Schneider R, Moore WM, Custer PJ, Grubbs KM, Schnurr PP. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):58–67. doi: 10.1001/jamapsychiatry.2014.1575. [DOI] [PubMed] [Google Scholar]
- 72.Engel CC, Oxman T, Yamamoto C, Gould D, Barry S, Stewart P, Kroenke K, Williams JW, Jr, Dietrich AJ. RESPECT-Mil: feasibility of a systems-level collaborative care approach to depression and post-traumatic stress disorder in military primary care. Military Medicine. 2008;173(10):935–940. doi: 10.7205/milmed.173.10.935. [DOI] [PubMed] [Google Scholar]
- 73.Engel CC, Bray RM, Jaycox LH, Freed MC, Zatzick DF, Lane ME, Brambilla D, Olmsted KR, Vandermaas-Peeler R, Litz B, Unutzer J, Katon WJ. Implementing collaborative primary care for depression and posttraumatic stress disorder: Design and sample for a randomized trial in the U.S. military health system. Contemporary Clinical Trials. 2014;39:310–319. doi: 10.1016/j.cct.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 74.Hoerster KD, Jakupcak M, Stephenson KR, Fickel JJ, Simons CE, Hedeen A, Dwight-Johnson M, Whealin JM, Chaney EF, Felker BL. A Pilot Trial of Telephone-Based Collaborative Care Management for PTSD Among Iraq/Afghanistan War Veterans. Telemedicine and e-Health. 2015;21(1):42–47. doi: 10.1089/tmj.2013.0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schnurr PP, Friedman MJ, Oxman T, Dietrich AJ, Smith MW, Shiner B, Forshay E, Gui J, Thurston V. RESPECT-PTSD: re-engineering systems for the primary care treatment of PTSD, a randomized controlled trial. J Gen Intern Med. 2013;28(1):32–40. doi: 10.1007/s11606-012-2166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Meredith LS, Eisenman D, Han B, Green BL, Kaltman S, Wong EC, Sorbero M, Vaughan C, Cassells A, Zatzick DF, Diaz C, Hickey S, Kurz JR, Tobin JN. Impact of Collaborative Care for Underserved Patients with PTSD in Primary Care: a Randomized Controlled Trial. Journal of General Internal Medicine. 2016;31(5):509–517. doi: 10.1007/s11606-016-3588-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Katon W, Lin EH, Von Korff M, Ciechanowski P, Ludman E, Young B, Peterson D, Rutter CM, McGregor M, McCulloch D. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;30(363):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Callahan CM, Kroenke K, Counsell SR, Hendrie HC, Perkins AJ, Katon W, Noel PH, Harpole L, Hunkeler E, Unutzer J, Investigators I. Treatment of depression improves physical functioning in older adults. J Am Geriatr Soc. 2005;53(3):367–373. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- 79.Unutzer J, Katon W, Fan MY, Schoenbaum M, Lin EH, Della Penna RD, Powers D. Long-term cost effects of collaborative care for late-life depression. Am J Manag Care. 2008;14(2):95–100. [PMC free article] [PubMed] [Google Scholar]
- 80.Niles AN, Sherbourne CD, Roy-Byrne PP, Stein MB, Sullivan G, Bystritsky A, Craske MG. Anxiety treatment improves physical functioning with oblique scoring of the SF-12 short form health survey. Gen Hosp Psychiatry. 2013;35(3):291–296. doi: 10.1016/j.genhosppsych.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Von Korff M. Individualized stepped care of chronic illness. West J Med. 2000;172:133–137. doi: 10.1136/ewjm.172.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]