Abstract
Objective
Describe the process of adapting an integrated medical and psychiatric self-management intervention to a smartphone application for middle-aged and older adults with serious mental illness using an adaptive systems engineering framework and user-centered design.
Methods
First, we determined the technical abilities and needs of middle-aged and older adults with serious mental illnesses using smartphones. Then, we developed smartphone content through principles of user-centered design and modified an existing smartphone platform. Finally, we conducted a usability test using “think aloud” and verbal probing.
Results
We adapted a psychosocial self-management intervention to a smartphone application and tested its usability. Ten participants (Mean age=55.3 years, SD=6.2) with serious mental illness and comorbid chronic health conditions reported a high level of usability and satisfaction with the smartphone application.
Conclusions
Middle aged and older adults with serious mental illness and limited technical abilities were able to participate in a process involving user-centered design and adaptation of a self-management intervention to be delivered by a smartphone. High usability ratings suggest that middle-aged and older adults with serious mental illness have the potential to use tailored smartphone interventions. Future research is indicated to establish effectiveness and to determine the type and intensity of clinical support needed to successfully implement smartphone applications as a component of community-based services for older adults with psychiatric and medical conditions.
Keywords: Psychosocial Intervention, Mobile Health Technology, Older Adults
Middle-aged and older adults with serious mental illness have higher rates of medical illness and are at an increased risk of premature death compared to adults of a similar age without mental illness [1]. Adults with serious mental illness and comorbid health conditions have 2 to 3 times higher health costs than the general population, and these costs can increase with age [2]. Illness self-management interventions have the potential to reduce risk factors associated with early mortality and to reduce the use of high-cost acute care services [3].
In a recent systematic review, our group identified nine integrated self-management interventions and concluded these interventions are feasible and acceptable, and have high likelihood of clinical effectiveness [3]. Despite promising evidence, these interventions have had limited implementation in clinical settings due to required use of professionals, intensity, duration, and related costs [3]. The clinical resources needed to implement self-management interventions present challenges for resource poor settings such as community mental health centers that are understaffed and underfunded. Innovative use of mobile health technology can help to overcome these barriers to practical implementation of community-based interventions and reach vulnerable populations [4].
The use of mobile health interventions by adults with serious mental illness is a highly promising approach that has been shown to be highly feasible and acceptable [4]. These technologies are associated with many advantages compared to traditional psychosocial interventions including the potential for individually tailored, just-in-time delivery along with wide dissemination and high population impact. However, the process of adapting an existing psychosocial intervention to a smartphone intervention requires adaptation for a high-risk group with limited health and technology literacy. The purpose of this report is to describe the process of adapting a psychosocial intervention to a smartphone intervention for middle-aged and older adults with serious mental illness and to discuss implications for the use of this approach in adapting other geriatric mental health interventions for broad implementation and dissemination.
Methods
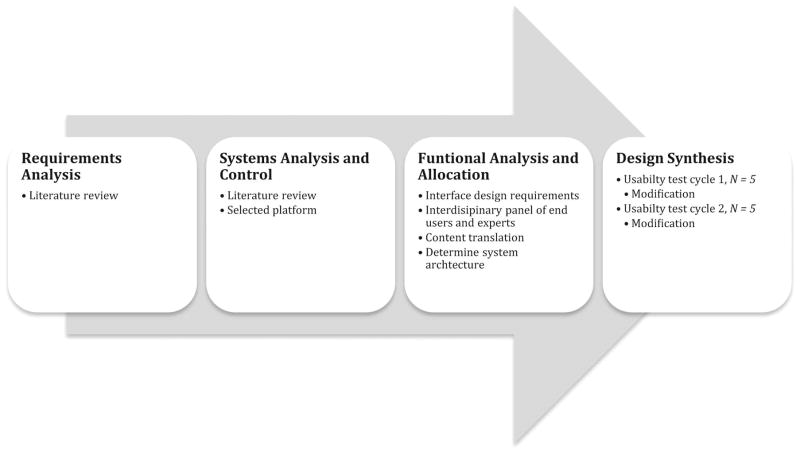
We used an adaptive systems engineering framework [5] and user-centered design [6] to guide the multi-stage iterative design and testing process (see Figure 1). Adaptive systems engineering is a transdisciplinary process that considers parts of a system in the development of a product [5]. As such, this framework allowed us to consider scalability factors (i.e., cost, time required, and resource allocation) while including user input throughout the development.
Figure 1.
Requirements Analysis
First, we determined that middle-aged and older adults with mental health disorders frequently have smartphones [7] and commonly use smartphones in their everyday life. Therefore, instead of introducing a new technology, we decided to use a smartphone since they were already accustomed to using this product. Next, we determined the features of the smartphone application necessary to match the technical abilities and needs of middle-aged and older adults with serious mental illnesses. This phase determined characteristics that will facilitate use by end-users. Through a literature review, we identified characteristics needed for smartphone apps that are specifically tailored for this population, including design features for persons with serious mental illness [8] and older adults [9] based on published recommendations (Table 1).
Table 1.
Smartphone Application Design Features for Middle-aged and Older Adults with Serious Mental Illnesses
| Identified Need | Design Feature |
|---|---|
| In real-world environments older adults commonly present with multimorbidity [29]. | Capacity to address multimorbidity |
| Patients adopt and engage with health technology more if a human is part of an intervention [15]. | Access to live and automated self- management support |
| Age-related memory loss and cognitive deficits results in poor medication adherence [30]. Notifications may help with medication management. | Behavioral tailoring for adherence |
| As the aging processes impacts recent memory or the formation of new memories [25]. Multimodal delivery of psychoeducation may decrease memory load. | Multimodal capacity |
| To facilitate adoption, on-demand features can be accessed at any time, in any place. | On-demand features |
| Adults with serious mental illness commonly experience depressive symptoms or anxiety [31] and difficulty in forming new memories [25] – both of which can inhibit working memory function [32] and motivation [33]. By contrast, game playing motivates engagement, learning, and behavioral change [34]. | Gamification techniques (e.g., visually showing their progress) |
| Adults with serious mental illness commonly have limited health and technology literacy and require specific design features [8]. | (1) Simple user interface; (2) functional features that do not divide attention; (3) two-layer branching logic; (4) clear navigation; (5) contrasting screen layout and colors; and (6) 14 point text. |
System Analysis
Next, we considered the resource demands (i.e., financial costs, time required, and resource allocation) required to develop a smartphone platform to deliver an interactive self-management program. We determined that building a smartphone application can take from seven months to a year, with related costs that can exceed $200,000 [10]. This time period is lengthy considering how rapidly technology advances. In addition, we considered the downstream costs associated with security, upgrading, and maintaining a smartphone application. Taking these considerations into account, we decided to use an existing platform to optimize scalability. We selected Wellframe, a Boston-based company. Wellframe originally developed the smartphone application and established the feasibility of the application to address cardiac rehabilitation with a sample of middle-aged and older adults [11] and to address health promotion with a sample of adults with serious mental illness [12]. As the smartphone architecture was already developed, our adaptation was restricted to text, video, and protocol.
Functional Analysis and Allocation
This phase identified the design of the interface. With end-user adoption in mind, we applied user-centered design principles to facilitate the development of smartphone application content and protocol. To promote use, user-centered design requires the inclusion of end-users early in the design process [6]. Since Integrated Illness Management and Recovery (I-IMR) has demonstrated effectiveness and was designed specifically for adults aged 50+ with serious mental illness and complex health conditions [13], we chose the I-IMR intervention for adaption to a smartphone application.
I-IMR is based on the stress vulnerability model [14], which asserts biological vulnerability and stress are impacted by factors that people have control over, such as coping skills. I-IMR is delivered by a masters-level clinician and a nurse in a community mental health setting [13]. I-IMR includes ten modules (see Table 2) and takes approximately 8 to 10 months to complete [13]. I-IMR combines evidence-based psychosocial interventions: psychoeducation, behavioral tailoring, relapse prevention training, and coping skills training [14].
Table 2.
I-IMR Self-Management Training Modules
| Session #1: Identifying Your Personal Recovery and Wellness Goals and Plan: Setting recovery and health goals and strategies to achieve goals to maximize functioning and orientation to the smartphone application. |
| Session #2: Psychoeducation: Psychoeducation on SMI and medical illness. |
| Session#3: Stress Vulnerability and Illness: Causes of mental illness and factors that impact its course. |
| Session #4: Building Social Supports and Recovery and Wellness: How to build social supports to improve well-being and sustain wellness. |
| Session #5: Medication Adherence Strategies: Behavioral tailoring and motivational techniques for psychiatric and medical medication adherence. |
| Session #6: Psychiatric and Medical Relapse Prevention: Identify warning signs and develop a relapse prevention plan for psychiatric symptoms. |
| Session #7: Coping with Psychiatric Symptoms and Health-related Stress and Solving Problems: Establish a step-by-step method managing psychiatric symptoms and problem solving. |
| Session #8: Coping with Stress, Chronic Pain and Medical Symptoms, and Solving Problems: Identifying stressors that exacerbate symptoms and strategies to cope with stress. |
| Session #9: Substance Abuse and Medication Misuse: Overcoming substance abuse and the effects on symptoms and functioning. |
| Session #10: A Guide to Navigating the Mental Health and Medical Healthcare System: Accessing mental health and medical health services and insurance benefits, making informed decisions. |
In order to improve usability, we assembled a transdisciplinary team of end-users and experts. Our team included clinicians, older adults with serious mental illness, peer specialists, physicians, and engineers. In consideration of implementation, stakeholders worked in the agency or received services in the agency where we wanted to deploy our intervention.
First, we developed a visual representation of how a user would navigate through the application. Next, we redesigned the content of the I-IMR manual to deliver on smartphone pages. Each smartphone page includes approximately 300 words. Finally, we used the Flesch-Kincaid Grade Level formula in Microsoft Word 2010 to modify the readability of the text. The original text in the I-IMR manual was written for clinicians at an 8th grade level. To enhance self-directed learning, we initially rewrote text to a 6th grade level and included short, simple sentences. To protect our intellectual property, we worked with lawyers at our home institution and added a copyright to our text and videos.
The smartphone application automatically progresses through each module over a three-month timespan. For example, a patient will participate in the self-advocacy module for seven days and learn daily self-advocacy skills. All modules can be repeated and extended beyond three-months based on the patients’ needs and preferences. This has the potential to create a self-sustaining system after intervention withdrawal. While patients are required to complete all modules, the smartphone application content can be personalized. For example, the application includes a daily self-management checklist that can be personalized by patients or a clinician. As patients complete their self-management tasks, their progress is displayed on the application.
Smartphone interventions can allow us to monitor behavior dynamically--in context and in real-time. For example, as patients use the application to complete their daily self-management checklist, data will be sent to the care management dashboard. If a patient describes signs of a potential relapse or failing to take their medication as prescribed, clinicians can pre-emptively intervene. The care management dashboard tracks patients’ progress and enables secure, HIPAA-compliant messaging to the smartphone application, and potentially has the capacity to integrate into electronic health records and existing workflow. The care management dashboard also provides the potential to identify reduced use of the application and prevent disengagement. High rates of discontinuation and attrition are a common limitation of smartphone interventions [15]. Including humans as interventionists in health technology interventions may help to promote adoption and sustained engagement [16].
Adaptation of Evidence-Based Principles from I-IMR
Psychoeducation
As repetition is an important part of mastery of new skills and habit formation [17], we incorporated videos that can be repeatedly accessed on the smartphone. Instead of clinicians reading descriptive information from the manual to a patient, we wrote scripts for videos, hired clinicians or patients with a serious mental illness as actors, and filmed videos on self-management techniques. Based on our prior usability assessments of smartphone applications, we determined the length of videos should not exceed three minutes.
Behavioral tailoring
Behavioral tailoring consists of helping patients develop a regular schedule for taking their medications [18]. Within the I-IMR manual, clinicians work with patients to write down these schedules on a piece of paper that a patient can carry with them. By contrast, the smartphone application includes a learning module on medication management and also enhances it through allowing patients to enter medications they are taking and set medication reminders.
Relapse prevention training
The goal of relapse prevention training is to help patients identify past experience with relapse and identify triggers and early warning signs. This process helps patients create a personalized relapse prevention plan. The I-IMR manual instructs clinicians to work with patients to write down their relapse prevention plan on a piece of paper and instructs them to carry it with them. While this may be an effective method, the smartphone application includes a relapse prevention plan that can be personalized by patients and accessed and updated at any time on the smartphone.
Coping skills training
In the I-IMR manual, to transition coping skills into the real- world, we relied solely on practice within the clinical settings. We enhanced the delivery of coping skills videos through the use of guided videos that can be accessed on the smartphone application. For example, we included progressive muscle relaxation videos to teach patients how to self soothe. These coping skills videos can be used as a resource if a patient wants to practice skills outside of the clinical setting or is experiencing a crisis.
Design Synthesis
Next, we conducted a usability test. The usability test was approved by the Institutional Review Board at [blinded for review] and [blinded for review].
Participants
Usability studies commonly require a minimum of five participants to ensure the identification of usability issues [19]. As intervention development is an iterative process, we included two cycles of five participants. The first five participants completed the first usability test. With their feedback, we made modifications and developed a second version of the smartphone application. The final five participants reviewed the second version. The total sample included 10 adults aged 49+ years with medical illnesses (defined as cardiovascular disease, obesity, diabetes, high blood pressure, high cholesterol, osteoporosis, gastro esophageal reflux disease, osteoarthritis, chronic obstructive pulmonary disease, congestive heart failure, coronary artery disease) and bipolar disorder, major depressive disorder, schizophrenia, or schizoaffective disorder. Participants were recruited from two mental health outpatient programs in [blinded for review].
Recruitment
We reviewed medical charts to find participants that met inclusion criteria. Then, we contacted potential participants, provided a description of the study, and requested a verbal agreement to meet with the data collectors on-site.
Procedure
We informed participants about the purpose of the study, their voluntary inclusion in the study, and the confidentiality of the data. After agreeing to participate and providing informed consent, the data collectors screened for eligibility criteria.
We provided each participant with an iPhone 4S smartphone pre-loaded with the application. They received a 5-minute lesson on how to use a smartphone and the “think aloud” protocol [20]. “Think aloud” usability testing has helped detect design issues with adults with serious mental illness [21, 22]. The usability test lasted one-hour.
We asked participants to also complete tasks: (1) using the touch-screen icon to open the application; (2) reading articles; (3) swiping screen; (4) changing text size; (5) starting and stopping videos; (6) following peer-led videos; (7) writing and sending a text message; (8) opening daily tasks; (9) opening a relapse prevention plan; (10) using the pedometer; and (11) returning to the home page. We asked participants to use all smartphone application features and provide feedback on the content, language, layout, colors, videos, graphics, text size, readability, and navigation. We audio-recorded each session. One participant refused audio recording; however, data collectors wrote detailed notes from this session.
We then asked participants to complete a survey on their confidence using the application. We adapted this survey used in other smartphone application development studies with adults with serious mental illness [22]. The survey is based on the System Usability Scale [23], Post Study System Usability Questionnaire [24], and Usefulness, Satisfaction, and Ease questionnaire [25]. In response to participant feedback, we made systems modifications for improvement after the first five participants. We provided a $20 gift card for participation.
Data Analysis
Descriptive statistics were used to describe the characteristics of the sample and survey data. For task analysis, we calculated the percentage of the sample able to perform each task by themselves. The first two authors reviewed the think aloud comments and organized themes based on participants’ comments on each application page.
Results
Six participants had a psychotic disorder, four had a mood disorder, and all had medical illnesses (see Table 3). Participants’ age ranged from 49–66 years (M=55.3 years) and most identified as White (90%). Five of the participants owned a smartphone. Factors that deterred smartphone use included: typing on the smartphone (n=5), cost (n=3), and not understanding the smartphone (n=2).
Table 3.
Demographic Characteristics of the Study Sample
| N | % | |
|---|---|---|
| Age (mean) | 55.3 | |
| Gender | ||
| Female | 5 | 50 |
| Male | 5 | 50 |
| Race | ||
| White | 9 | 90 |
| Black/African American | 1 | 10 |
| Highest education completed | ||
| High School/GED | 6 | 60 |
| Bachelor’s Degree | 3 | 30 |
| Master’s Degree | 1 | 10 |
| Psychiatric Diagnosis | ||
| Schizophrenia | 2 | 20 |
| Schizoaffective Disorder | 4 | 40 |
| Bipolar Disorder | 3 | 30 |
| Major Depressive Disorder | 1 | 10 |
| 3 + chronic health conditions | 5 | 50 |
| Current Smartphone owner | 5 | 50 |
The following presents “think aloud” comments and modifications for both cycles of usability tests.
Cycle 1
In the first version, the first five participants were able to independently navigate the smartphone and completed all of the tasks. They responded positively to the placement of smartphone features including the pedometer and relapse prevention plans, and also liked the two-layer branching logic used in the daily self-management task list. They reported enjoying the positive images in the articles. They commented on (1) the grade-level of the text, “for the everyday people, they are not educated, people around here don’t have [college degrees], if they are lucky they have a GED, and the lingo, jargon is beyond what they can understand”; (2) the length of videos, "I didn’t like the video, it was too long”; and (3) and the length of the text, “take the whole paragraph…and put a space between them [sentences]”. All participants positively regarded the videos, and they did not have a preference for the age of the person in the video.
Cycle 2
For the second version, we responded to the first five participants’ comments and shortened text and videos and reduced the reading level from 6th grade to 4th grade. For cycle 2, the remaining five participants were also able to independently navigate the smartphone and completed all of the tasks. They also responded positively to the placement of features and the two-layer branching logic. Participants’ “think aloud” comments indicated they preferred the second version, “you can use the app in a room full of people”, “having the app would be really handy", and “you guys are giving good information that this is just an app, not medical information” (Table 4). They did recommend the inclusion of transcripts below the videos, so people could choose to read video transcripts or watch videos.
Table 4.
Selected Usability Test Comments
| “The nice thing about having the multiple size text is that if you wear glasses and you’re crying and want some support, you can access the app” |
| “Having the app would be really handy" |
| “You guys are giving good information that this is just an app, not medical information” |
| "People with mental illness sometimes wake up in a fog and it would be nice to have a reminder list.” |
| “Few times a day I would like to know how to cope with stress” |
| "I think deep breathing is very helpful, its calms you down, calms the mind” |
| "If a doctor was saying ‘keep track of your medicine’, I would use it.” |
| “It was nice, yes, I can relate [referring to video]” |
| “You can use the app in a room full of people” |
Table 5 reports the aggregate results from both cycles of usability tests. As shown, the majority of participants felt comfortable, very confident and satisfied using the application. Since we were satisfied with all of the participants responses and also the “think aloud” comments, we determined two cycles of usability tests adequately identified usability issues.
Table 5.
Usability of the Smartphone Application Among Middle-Aged and Older Adults with Serious Mental Illness and Chronic Health Conditions
| Disagree | Neutral | Agree | |
|---|---|---|---|
| I think that I would like to use the App often | 0 (0%) | 2 (20%) | 8 (80%) |
| I found the App to be very complicated | 8 (80%) | 2 (20%) | 0 (0%) |
| I thought the App was easy to use | 0 (0%) | 1 (10%) | 9 (90%) |
| I think that I would need the support of a technical person to be able to use the App | 6 (60%) | 1 (10%) | 3 (30%) |
| I found that the different parts of the App work well together | 0 (0%) | 0 (0%) | 10 (100%) |
| I thought there was too much inconsistency in the App | 8 (80%) | 2 (20%) | 0 (0%) |
| I would imagine that most people would learn to use the App very quickly | 0 (0%) | 3 (30%) | 7 (70%) |
| I found the App very awkward to use | 10 (100%) | 0 (0%) | 0 (0%) |
| I felt very confident using the App | 0 (0%) | 2 (20%) | 8 (80%) |
| I needed to learn a lot of thing before I could get going with the App | 6 (60%) | 4 (40%) | 0 (0%) |
| Overall, I am satisfied with how easy it is to use the App | 0 (0%) | 1 (10%) | 9 (90%) |
| I was able to complete the “modules” quickly in the App | 0 (0%) | 1 (10%) | 9 (90%) |
| I felt comfortable using the App | 0 (0%) | 0 (0%) | 10 (100%) |
| It was easy to learn to use the App | 0 (0%) | 0 (0%) | 10 (100%) |
| Whenever I made a mistake using the App I could recover easily and quickly | 0 (0%) | 0 (0%) | 10 (100%) |
| It was easy to find the information I needed | 0 (0%) | 2 (20%) | 8 (80%) |
| The information provided for the App was easy to understand | 0 (0%) | 1 (10%) | 9 (90%) |
| How things appeared on the screen was clear | 0 (0%) | 1 (10%) | 9 (90%) |
| If I have access to the App I will use it | 1 (10%) | 0 (0%) | 9 (90%) |
| I am satisfied with the App | 0 (0%) | 3 (30%) | 7 (70%) |
| I would recommend the App to a friend | 0 (0%) | 2 (20%) | 8 (80%) |
| The App is fun to use | 0 (0%) | 1 (10%) | 9 (90%) |
| The App works the way I want it to | 0 (0%) | 2 (20%) | 8 (80%) |
| I feel I need to have the App | 2 (20%) | 6 (60%) | 2 (20%) |
| The App can help me manage my symptoms | 0 (0%) | 2 (20%) | 8 (80%) |
| The App was interactive enough | 1 (10%) | 2 (20%) | 7 (70%) |
Of the ten participants, they reported they would use the application daily if they felt encouraged by peers (n=10) doctors (n=8), case managers (n=8), or family or friends (n=8). Other factors that would increase their engagement included knowing how to use a smartphone (nine “agreed”), having a free smartphone (ten “agreed”), reminders on the smartphone (nine “agreed”), and fun things to do on the smartphone like watch videos or use Facebook (ten “agreed”).
Conclusions
This report describes the process of adapting a psychosocial intervention to a smartphone application for middle-aged and older adults with serious mental illness. User-centered design enabled us to target the unique needs of middle-aged and older adults with serious mental illness and produce a more useable product. This process has implications for use of smartphone applications in other populations of older adults with mental health disorders by enhancing in-person sessions and facilitating the delivery of personalized evidence-based interventions outside of conventional clinical settings, resulting in increased reach, effectiveness, and potential cost savings.
User-Centered Design and Appropriate User-Interface
User-centered design and the appropriate user-interface for middle-aged and older adults with serious mental illness helped us produce a more useable product. Participants felt the application was easy to learn how to use, thought the application could help manage symptoms, and were satisfied with the application. Despite half the sample not owning a smartphone, all of the participants independently navigated the smartphone application.
We attribute this high level of usability to the inclusion of users early in the development phase. This enabled us to refine features designed specifically for adults with serious mental illness [8] and have sensitivity to potential age-related changes in older adults with respect to memory, attention, sensory abilities, and factors that affect cognitive aging [9]. For example, age-related changes in recall memory [26] and visual acuity [27] can decrease smartphone use and diminish intervention effects. Successful adaptations for older adults with mental health conditions warrant a modified smartphone intervention interface. For example, enlarged fonts and use of age-appropriate videos instead of text can facilitate intervention delivery and uptake.
Clinical Relevance of Adapting a Psychosocial Intervention to a Smartphone Intervention
Smartphone applications can enhance in-person sessions and facilitate the delivery of personalized interventions outside of the clinical setting. Smartphone technology allows clinicians to increase the intensity and dose of evidence-based psychosocial intervention components. Evidence-based practices are inconsistently implemented across clinical settings, potentially diluting the impact of these interventions [28]. Smartphone applications provide an opportunity for implementation of evidence-based principles to improve clinical outcomes without variation in delivery of intervention components. Smartphones may also allow adaptation of interventions to patient needs and preferences and may increase the effectiveness of care.
Smartphone application interventions have the potential to alter the patient-clinician relationship. With smartphone interventions, clinicians can actively and continuously monitor patients and: (1) support treatment plans through virtual care, (2) automatically detect problematic behaviors and deliver tailored interventions while patients are outside of the clinical setting, and (3) facilitate care coordination between cross systems. Through this approach, clinicians have dynamic, data driven tools that may be used to inform clinical decision-making. Although smartphone applications require a financial investment, they have the potential augment care and increase efficiencies of telehealth programs. Smartphone applications also potentially facilitate patient engagement in participatory, personalized, and preventative care. As the healthcare industry increasingly embraces prevention and illness self-management, it is important for physicians and patients to be actively involved in designing and developing new technologies supporting these approaches.
Limitations
This usability study had several limitations. First, participants evaluated the smartphone application by using it for an hour, in contrast to extended use over time that would likely identify additional recommendations for modification. Further, as we examined usability for one-hour in a clinical environment, it is not known if people will use the smartphone application in a real-world environment and if the smartphone application intervention is effective. Second, though the sample size met usability test requirements [19], our study group consisted of an ethnically and racially homogeneous group, potentially limiting generalizability to ethnically diverse populations. Third, the sample included both middle aged and older adults, potentially limiting implications for older frail adults. Fourth, the sample was selected to assess usability, and did not specifically focus on recruiting clinically unstable and high-need patients. This might reflect the personal perception of having a low need for the application, despite endorsing very high ratings of satisfaction. Fifth, we modified the standard procedure that Wellframe recommends for training patients in using the smartphone application potentially reducing the perceived usability; however, participants reported high usability ratings based on our modified protocol. Sixth, participants commented on features that could not be modified due to technology constraints within the system (i.e., two people reported confusion when they accessed the visual representation of tasks completed). These findings may be used in future adaptation efforts. Finally, the smartphone application has capacity to work on an iPhone and Android, but it was only tested on an iPhone. The differences in the application are minimal between the two operating systems (iPhone and Android).
Through adapting the psychosocial intervention to a smartphone application, we created a self-directed intervention and reduced the duration of the original intervention from 10–12 months to 3-months. The process described in this report has potential implications for other high-risk groups of older adults with complex needs and limited technical abilities by using principles of adaptive systems engineering framework [5] and user-centered design [6]. Smartphone interventions provide promising opportunities to advance clinical effectiveness and increase reach beyond traditional settings and change the way healthcare is delivered. High usability ratings suggest that middle-aged and older adults with serious mental illness have the potential to use tailored smartphone interventions. Future research is indicated to establish effectiveness and to determine the type and intensity of clinical support needed to successfully implement smartphone applications as a component of community-based services for older adults with psychiatric and medical conditions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Walker E, McGee R, Druss B. Mortality in mental disorders and global disease burden implications. A systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartels SJ, Clark R, Peacock WJ, et al. Medicare and medicaid costs for schizophrenia patients by age cohort compared with costs for depression, dementia, and medically ill patients. Am J Geriatr Psychiatry. 2003;11:648–57. doi: 10.1176/appi.ajgp.11.6.648. [DOI] [PubMed] [Google Scholar]
- 3.Whiteman KL, Naslund JA, Di Napoli E, et al. Systematic review of general medical and psychiatric self-management interventions for adults with serious mental illness. Psychiatr Services. 2016 doi: 10.1176/appi.ps.201500521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naslund JA, Marsch LA, McHugo GJ, et al. Emerging mHealth and eHealth interventions for serious mental illness: A review of the literature. J Ment Health. 2015;24:321–32. doi: 10.3109/09638237.2015.1019054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shenhar A, Bonen Z. The new taxonomy of systems: Toward an adaptive systems engineering framework. TIEEE transactions on systems, man, and cybernetics-part a Systems and Humans. 1997;27:137–145. [Google Scholar]
- 6.Samaras GM, Horst RL. A systems engineering perspective on the human-centered design of health information systems. J Biomed Inform. 2005;38:61–74. doi: 10.1016/j.jbi.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 7.Ben-Zeev D, Davis KE, Kaiser S, et al. Mobile technologies among people with serious mental illness: Opportunities for future services. Adm Policy Ment Health. 2012;40:340–343. doi: 10.1007/s10488-012-0424-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rotondi AJ, Sinkule J, Haas GL, et al. Designing websites for persons with cognitive deficits: Design and usability of a psychoeducational intervention for persons with severe mental illness. Psychol Serv. 2007;4:202–224. doi: 10.1037/1541-1559.4.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nielsen J. Usability engineering. London: Academic press; 1994. [Google Scholar]
- 10.Formotus. [Accessed June 26, 2016];App development costs. 2016 Jun 17; Available at: http://www.formotus.com/14018/blog-mobility/figuring-the-costs-of-custom-mobile-business-app-development.
- 11.Forman D, LaFond K, Panch T, et al. Utility and efficacy of a smartphone application to enhance the learning and behavior goals of traditional cardiac rehabilitation: A feasibility study. J Cardiopulm Rehabil Prev. 2014;34:327–334. doi: 10.1097/HCR.0000000000000058. [DOI] [PubMed] [Google Scholar]
- 12.Macias C, Panch T, Hicks Y, et al. Using smartphone apps to promote psychiatric and physical well-being. Psychiatr Q. 2015;86:505–519. doi: 10.1007/s11126-015-9337-7. [DOI] [PubMed] [Google Scholar]
- 13.Bartels SJ, Pratt S, Mueser K, et al. Integrated IMR for psychiatric and general medical illness for adults aged 50 or older with serious mental illness. Psychiatric Services. 2014;3:330–337. doi: 10.1176/appi.ps.201300023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zubin J, Spring B. Vulnerability: A new view of schizophrania. J Abnorm Psychol. 1977;86:103–126. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]
- 15.Mattila E, Orsama A, Ahtinen A, et al. Personal health technologies in employee health promotion: Usage activity, usefulness, and health-related outcomes in a 1-Year randomized controlled trial. JMIR Mhealth Uhealth. 2013;1:e16. doi: 10.2196/mhealth.2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohr DC, Cuijpers P, Lehman K. Supportive accountability: A model for providing human support to enhance adherence to eHealth interventions. JMIR. 2011;13:e30. doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ausubel D. The acquisition and retention of knowledge: A cognitive view. New York, NY: Kluwer Academic Publishers; 2000. [Google Scholar]
- 18.Mueser KT, Corrigan PW, Hilton DW, et al. Illness management and recovery for severe mental illness: a review of the research. Psychiatr Serv. 2002;53:1272–84. doi: 10.1176/appi.ps.53.10.1272. [DOI] [PubMed] [Google Scholar]
- 19.Macefield R. How to specify the participant group size for usability studies: A practitioner’s guide. J Usuability Studies. 2009;5:34–45. [Google Scholar]
- 20.Black AC, Serowik KL, Schensul JJ, et al. Build a better mouse: Directly-observed issues in computer use for adults with SMI. Psychiatr Q. 2013;84:81–92. doi: 10.1007/s11126-012-9229-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vilardaga R, Rizo J, Kientz J. User experience evaluation of a smoking cessation app in people with serious mental illness. Nicotine Tob Res. 2015;18:1032–1038. doi: 10.1093/ntr/ntv256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ben-Zeev D, Kaiser SM, Brenner CJ, et al. Development and usability testing of FOCUS: a smartphone system for self-management of schizophrenia. Psychiatric Rehabilitation Journal. 2013;36:289–96. doi: 10.1037/prj0000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brooke J. SUS-A quick and dirty usability scale. Usability Evaluation in Industry. 1996:189–194. [Google Scholar]
- 24.Lewis J. Psychometric evaluation of the poststudy system usability questionnaire: the PSSUQ. Paper from Proceedings of the Human Factor Society Annual Meeting; October 1996; pp. 1259–1260. [Google Scholar]
- 25.Lund A. Measuring usability with the USE questionnaire. Usability Interface. 2001;8:3–6. [Google Scholar]
- 26.Hasher L, Zacks R. Working memory, comprehension, and aging: A review and a new view. Psychol Learn Motiv. 1989;22:193–225. [Google Scholar]
- 27.Crews J, Campbell V. Vision impairment and hearing loss among community-dwelling older Americans: Implications for health and functioning. Am J Public Health. 2004;94:823–829. doi: 10.2105/ajph.94.5.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Institute of Medicine. [Accessed November 20, 2015];Crossing the quality chasm: A new health system for the 21st century. 2001 Mar 1; Available at: http://iom.edu/Reports/2001/Crossing-the-Quality-Chasm-A-New-Health-System-for-the-21st-Century.aspx.
- 29.Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. doi: 10.1093/epirev/mxs009. [DOI] [PubMed] [Google Scholar]
- 30.Insel K, Morrow D, Brewer B, et al. Executive function, working memory, and medication adherence among older adults. J Gerontol. 2006;61:102–107. doi: 10.1093/geronb/61.2.p102. [DOI] [PubMed] [Google Scholar]
- 31.Bottlender R, Strauss A, Möller HJ. Prevalence and background factors of depression in first admitted schizophrenic patients. Acta Psychiatr Scand. 2000;101:53–160. doi: 10.1034/j.1600-0447.2000.90063.x. [DOI] [PubMed] [Google Scholar]
- 32.Richards JM, Gross J. Emotion regulation and memory: The cognitive costs of keeping one's cool. J Pers Soc Psychol. 2000;79:410–424. doi: 10.1037//0022-3514.79.3.410. [DOI] [PubMed] [Google Scholar]
- 33.Layne C. Motivational deficit in depression. People's expectations x outcomes' impacts. J Clin Psychol. 1980;36:647–652. doi: 10.1002/1097-4679(198007)36:3<647::aid-jclp2270360306>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 34.Kapp K. The gamification of learning and instruction: Game-based methods and strategies for training and education. San Franciso, CA: John Wiley & Sons; 2012. [Google Scholar]