Abstract
Background
Successful surgical treatment of late presenting infantile tibia vara (ITV) patient requires the correction of oblique deformities. The purpose of this study was to report on a new comprehensive approach to correct and prevent recurrence of these deformities with a single procedure.
Methods
Medical records of 23 consecutive children (7–18 years) with advanced ITV (29 knees) were retrospectively reviewed after a mean of 7.3 years postoperatively (range: 2–22 years). Indications for the corrective surgery were any child seven year or older with a varus mechanical axis angle (MAA) 10 degrees or greater or a varus anatomical axis angle (AAA) eleven degrees or greater and a medial tibial angle (MTA) slope less than 60 degrees. The deformities were corrected with a dome-shaped osteotomy proximal to the tibial tubercle with a midline vertical extension to the subchondral region of the joint and a lateral hemi-epiphysiodesis.
Results
At latest follow-up, means and medians of each tibial radiographic axis measurement improved significantly from preoperative values (p<0.001): MAA from 23 degrees to 4 degrees varus, AAA from 25 degrees varus to 1 degree valgus, MTA downward slope from 30 degrees to 78 degrees, posterior medial tibial angle (PMTA) from 59 degrees to 80 degrees. Seventy-nine percent and 74% had good to excellent results based on radiographic criteria and clinical questionnaire for satisfaction, pain and function, respectively. Two abnormal medial tibial plateau types were described.
Conclusion
This is the first study to use a single stage double osteotomy performed proximal to the tibial tubercle for the late-presenting ITV for children seven years of age or older. In addition to the effective correction of the four major tibial deformities, a lateral proximal tibial hemi-epiphysiodesis minimizes recurrence of tibia vara. A contralateral proximal tibial epiphysiodesis is recommended for treated skeletally immature patients with unilateral disease.
Level of Evidence
Therapeutic Level IV. See instructions for authors for a complete description of levels of evidence.
Introduction
Early untreated ITV as seen in the toddler is characterized clinically by progressive bowing of the leg and internal tibial torsion. Serial radiographs of the proximal tibia show the typical epiphyseal, growth plate, and metaphyseal changes: loss of height of the medial tibial epiphysis, increase of the downward sloping, and irregularity of medial growth plate and tibia vara.
The ideal time to reverse these changes is to brace the leg or perform a valgus tibial osteotomy before the age of three and four years, respectively [1–6]. However, if the disorder progresses to Langenskiöld Stage IV–VI or if there are significant residual deformities after treatment, a comprehensive surgical plan is required to correct the deformities in multiple planes.
There are several reports of single procedures reported to correct these deformities: valgus metaphyseal osteotomy, [7,8] medial tibial plateau elevation, [9–11] and medial epiphysiolysis of the growth plate [12]. Others have combined these procedures in one or two stages [13–18]. Recurrence of varus and persistence of abnormal medial articular slope of tibia may be due in part to failure to arrest a growing lateral growth plate or to correct the procurvatum [19,20]. Additional reporting on treatment outcomes with longer follow-up are needed before a modern consensus for treatment can be widely adopted.
We hypothesize that all the significant tibial deformities associated with late presenting ITV can be treated successfully in most instances with a single procedure based on a double tibial osteotomy done proximal to the tibial tubercle. It is the aim of this retrospective cohort study to report on a new comprehensive surgical approach to treat late presenting ITV with a single-stage double tibial osteotomy designed to correct the deformities and prevent recurrence.
Materials and Methods
Approval for this retrospective cohort study was granted by the Institutional Review Board. Medical records and radiographs of patients with late-presenting ITV were reviewed from two sites. Between January 1993 and June 2015, 26 patients with 33 limbs underwent the double osteotomy procedure. The inclusion criteria required each patient to be diagnosed originally with ITV. Indications for the corrective surgery were any child seven year or older with a varus mechanical axis angle (MAA) 10 degrees or greater or a varus anatomical axis angle (AAA) eleven degrees or greater and a medial tibial angle (MTA) slope less than 60 degrees. The minimal postoperative follow-up was two years. Two current patients with less than two years of follow-up were excluded and a third was lost to follow-up. 23 patients with 29 limbs remained eligible for study. During the 22-year study period, no other type of tibial osteotomy was performed for late-presenting ITV by the principal investigator.
Sixteen patients had bilateral ITV and seven patients had unilateral disease. In some bilateral cases, the procedure studied was only performed on one limb. All seven bilateral operated limbs and 13 unilateral cases were females. The average age at surgery was 9.9 years (7–18 years). Patients were followed for a mean length of 7.3 years (2–22 years) (Table 2). Previous to this procedure, 19 of 29 limbs (80%) had prior high tibial osteotomies and 21 patients were of African descent.
Table 2.
Summary of patient preoperative radiographic data and most recent follow-up postoperative data and results.
| Patient |
Location | Side | Langionskiold | Age at Surgery |
Follow up |
Anatomical Axisa |
Mechanical Axisb |
MTAc | PMTAd | ALFAe | Radiographic | Knee Range of Motion | Questionaire Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Follow-up | ||||||||||||||||||||
| (sex) | (yrs) | Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | Extension | Flexion | Extension | Flexion | ||||||
| 1 F | 1 | R | VI | 18.1 | 22.2 | −42 | 0 | −30 | −5 | 30 | 75 | 30 | 65 | 80 | 86 | Good | 0 | 120 | −10 | 145 | Fair |
| 2* F | 1 | L | VI | 10.5 | 19.9 | −20 | 0 | −17 | −4 | 53 | 83 | 47 | 90 | 84 | 86 | Good | 0 | 130 | 0 | 120 | Good |
| 3 F | 1 | R | VI | 9.6 | 15.6 | −21 | 3 | −17 | 0 | 35 | 90 | 85 | 89 | 90 | 90 | Good | 0 | 130 | 0 | 120 | Good |
| 4 F | 1 | R | VI | 8.8 | 10.8 | −28 | 8 | −22 | −3 | 32 | 63 | 77 | 78 | 81 | 80 | Excellent | −10 | 130 | 0 | 120 | Good |
| 5 F | 1 | R | V | 7.2 | 9.1 | −41 | −1 | −36 | −1 | 33 | 88 | 34 | 77 | 85 | 81 | Good | −10 | 100 | 0 | 100 | Poor |
| 1 | L | VI | 8.7 | 7.9 | −49 | 4 | −42 | −5 | 34 | 70 | 34 | 75 | 83 | 82 | Excellent | −10 | 100 | 0 | 100 | ||
| 6 F | 1 | R | VI | 8.7 | 8.0 | −20 | 0 | −16 | 1 | 35 | 75 | 47 | 87 | 82 | 86 | Good | 0 | 135 | 0 | 140 | Good |
| 1 | L | VI | 10.8 | 6.0 | −16 | 0 | −12 | −2 | 56 | 88 | 52 | 78 | 81 | 84 | Good | 0 | 135 | 0 | 140 | ||
| 7 F | 1 | R | V | 8.6 | 7.6 | −19 | 1 | −25 | −3 | 30 | 75 | 73 | 65 | 90 | 86 | Good | 0 | 140 | 0 | 150 | n/a |
| 8 F | 1 | L | VI | 8.3 | 6.9 | −14 | 4 | −12 | −2 | 26 | 71 | 35 | 85 | 81 | 81 | Excellent | 0 | 125 | −3 | 125 | n/a |
| 1 | R | VI | 8.6 | 6.3 | −15 | 6 | −11 | −2 | 22 | 65 | 33 | 89 | 82 | 82 | Excellent | 0 | 140 | −3 | 130 | ||
| 9 F | 1 | L | VI | 9.3 | 6.2 | −24 | −11 | −21 | −16 | 26 | 83 | 42 | 80 | 84 | 90 | Fair | 0 | 125 | −3 | 125 | n/a |
| 10* F | 1 | L | V | 12.2 | 4.9 | −30 | −2 | −24 | −5 | 48 | 80 | 51 | 80 | 83 | 86 | Excellent | 0 | 140 | 0 | 145 | Good |
| 11 F | 1 | L | V | 11.3 | 4.0 | −27 | 5 | −21 | 0 | 59 | 90 | 74 | 79 | 82 | 84 | Excellent | 0 | 140 | 0 | 140 | Good |
| 12 F | 1 | L | VI | 13 | 3.0 | −29 | 9 | −31 | 2 | 59 | 90 | 40 | 86 | 83 | 82 | Excellent | −5 | 125 | 0 | 120 | Fair |
| 1 | R | VI | 13 | 2.0 | −24 | −9 | −25 | −15 | 48 | 90 | 50 | 68 | 85 | 85 | Poor | −5 | 125 | 0 | 120 | ||
| 13* M | 1 | L | VI | 10.4 | 2.0 | −23 | −2 | −16 | −5 | 30 | 82 | 74 | 84 | 84 | 83 | Good | 0 | 130 | 0 | 130 | n/a |
| 14* F | 2 | R | VI | 9.4 | 10.0 | −25 | −2 | −32 | −10 | 13 | 61 | 61 | 90 | 90 | 85 | Poor | 0 | 130 | −3 | 125 | Fair |
| 15* M | 2 | L | VI | 10.4 | 9.1 | −32 | 4 | n/a | −5 | 33 | 76 | 64 | 82 | 87 | 89 | Excellent | 0 | 130 | 0 | 95 | Excellent |
| 16* F | 2 | L | V | 8.2 | 9.0 | −18 | 0 | n/a | 5 | 54 | 66 | 78 | 90 | 85 | 83 | Fair | 0 | 140 | 0 | 140 | Good |
| 17 F | 2 | L | VI | 12.7 | 8.4 | −32 | 2 | n/a | −3 | 27 | 66 | 80 | 70 | 85 | 86 | Excellent | 0 | 115 | 0 | 130 | Good |
| 18 F | 2 | L | VI | 11.3 | 5.2 | −37 | 4 | n/a | −1 | 53 | 90 | 90 | 88 | 83 | 83 | Good | 0 | 125 | 0 | 105 | Good |
| 19 F | 2 | R | VI | 7.7 | 5.2 | −12 | 8 | n/a | 0 | 50 | 67 | 50 | 90 | 85 | 88 | Good | 0 | 125 | −10 | 130 | Good |
| 2 | L | VI | 7.7 | 5.2 | −12 | 6 | n/a | 1 | 25 | 76 | 58 | 75 | 80 | 82 | Excellent | 0 | 120 | 0 | 120 | ||
| 20 F | 2 | R | VI | 6.7 | 4.2 | −40 | 7 | n/a | −1 | 35 | 89 | 75 | 86 | 81 | 83 | Excellent | −5 | 110 | −10 | 130 | Fair |
| 2 | L | VI | 6.7 | 4.2 | −32 | −10 | n/a | −16 | 50 | 90 | 80 | 84 | 80 | 80 | Fair | 0 | 95 | 0 | 120 | ||
| 21* M | 2 | R | V | 8.1 | 3.5 | −29 | 0 | n/a | −5 | 45 | 80 | 78 | 76 | 90 | 90 | Good | −5 | 145 | −5 | 135 | Excellent |
| 22 F | 2 | L | VI | 11.7 | 2.6 | −16 | −6 | n/a | −12 | 39 | 73 | 43 | 62 | 90 | 71 | Poor | −15 | 145 | −15 | 145 | Good |
| 23 M | 2 | L | V | 9.7 | 2.0 | −11 | 6 | n/a | 0 | 52 | 74 | 69 | 82 | 84 | 87 | Excellent | 0 | 150 | 0 | 150 | Excellent |
| Mean | 9.91 | 7.3 | −25.4 | 1.2 | −22.8 | −3.9 | 39.0 | 78.1 | 58.8 | 80.3 | 84.1 | 84.2 | −2.2 | 127.6 | −2.1 | 127 | |||||
| Median | 9.4 | 6.2 | −24.0 | 1.0 | −21.5 | −3.0 | 35.0 | 76.0 | 58.0 | 82.0 | 84.0 | 84.0 | 0 | 130 | 0 | 130 | |||||
Note: M = male. F = female. n/a = not available or did not complete survey.
= unilateral cases. All axis and angle measurements are in degrees.
. Mechanical Axis (normal ≤ 11)
. Anatomical Axis (normal ≤ ±5)
. MTA = Medial Tibial Angle (normal = 87±2)
. PMTA = Posterior Medial Tibial Angle (normal = 80±3)
. ALFA = Anatomical Lateral Femoral Angle (normal = 81±2).
The preoperative and most recent standing radiographic studies were used to measure correction of deformities and to assess severity with the Langenskiöld staging system [21]. A least two of the authors measured the five radiographic angles used in this study. Each angle was measured 3 times by each examiner and an average angle was was chosen for the use in the paper. Figure 1 shows the five angles measured: (A) MAA, (B) AAA, (C) MTA, (D) posterior medial tibial angle (PMTA), and (E) anatomic lateral femoral angle (ALFA) [22]. The preoperative MAA were not recorded for 11 of the 12 knees since these studies were not available. Complete correction of the four tibial and one femoral deformities were defined as a final MAA 0±5 degrees, AAA = 6±5 degrees, MTA = 87±4 degrees, PMTA or procurvatum = 80±6 degrees and LFA = 81±4 [13,23–25]. For MTA, PMTA and LFA an acceptable result was defined as falling within two standard deviations of the mean normal adult knee.
Fig. 1.
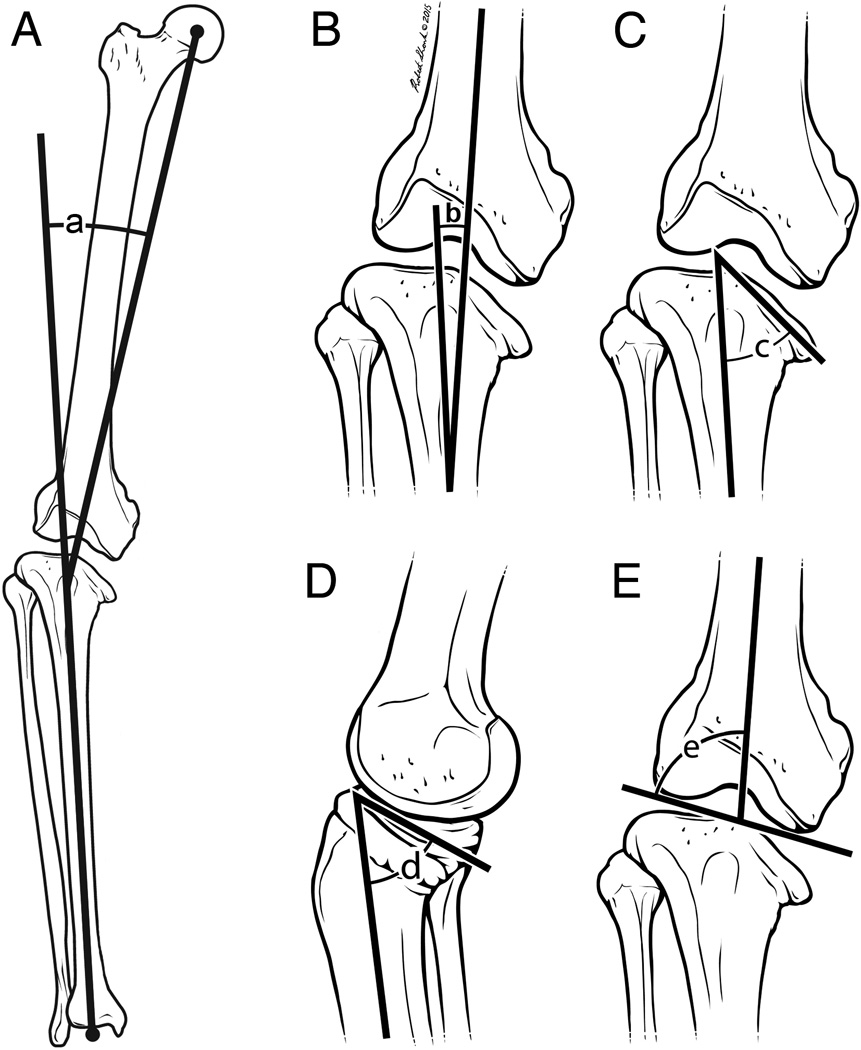
A–F The five lower limb bony angles measured on anteroposterior and lateral radiographs. (A) mechanical axis angle (MAA) formed by intersection of the femoral and tibial mechanical axes. (B) anatomical axis angle (AAA) formed by the intersection of the femoral and tibial anatomical axes (C) medial tibial angle (MTA) formed by the tibial mechanical axis and the slope of medial tibial plateau. (D) posterior medial tibial angle (PMTA) created by the tibial anatomical axis and slope of the medial tibial plateau on a lateral film. (E) anatomic lateral femoral angle (ALFA) which is the lateral angle formed by the intersection of femoral anatomical axis and a line draw through the femoral condyle.
A 12-item scale questionnaire was developed and administered postoperatively by phone or during clinic visits (Table 1) see electronic appendix. The survey was determined to be internally consisted by the Cronbach alpha method: α = 0.80 for the satisfaction and α = 0.71 for the pain symptoms and functioning measures [26,27]. Nineteen of 23 patients (83%) responded to the questionnaire.
Table 1.
A condensed version of the 12-item scale clinical outcome questionnaire administered to patients. Questions 1–5 assessed satisfaction. Questions 6–7 assessed pain and questions 8–12 assessed function.
| Outcome Questionnaire for Lower Extremity Deformity | ||
|---|---|---|
| Satisfaction (32 Points) | ||
| 1. Overall, how satisfied are you with how your surgery went? (16 points) | ||
| Very Satisfied (16) | Satisfied (12) | Neither satisfied nor dissatisfied (9) |
| Dissatisfied (6) | Very dissatisfied (0) | |
|
2. How would you rate the quality of interaction with your healthcare team, that is, all the healthcare providers you interacted with during your surgery and recovery? (4 points) | ||
| Excellent (4) | Good (3) | Satisfied (2) |
| Poor (1) | Inadequate (0) | |
| 3. How happy are you now with the appearance of your leg(s)? (4 points) | ||
| Extremely happy (4) | Very happy (3) | Moderately happy (2) |
| Not very happy (1) | Not at all happy (0) | |
| 4. How happy are you now with the way you walk? (4 points) | ||
| Extremely happy (4) | Very happy (3) | Moderately happy (2) |
| Not very happy (1) | Not at all happy (0) | |
| 5. How happy are you now with the speed at which you are able to walk? (4 points) | ||
| Extremely happy (4) | Very happy (3) | Moderately happy (2) |
| Not very happy (1) | Not at all happy (0) | |
| Pain (30 Points) | ||
|
6. Do you feel any pain in one or both of your knees when you walk, or do you not feel any pain in either knee when you walk? If you experience pain at how many miles do you experience knee pain when walking? Your best estimate will be fine. (15 points) | ||
| No Pain in either knee (15) | Knee pain at more than 2 miles (10) | |
| Knee pain at less than or equal to 2 miles (5) | Unable to walk (0) | |
|
7. Do you feel any pain in one or both of your knees when you run, or do you not feel any pain in either knee when you run? If you experience pain at how many miles do you experience knee pain when running? Your best estimate will be fine. (15 points) | ||
| No pain in either knee (15) | Knee pain at more than 1 mile (10) | |
| Knee pain at less than or equal to 1 mile (5) | Unable to run (0) | |
| Function (31 Points) | ||
|
8. As compared to your physical activity level before the surgery, how physically active would you say you are now? (8 points) | ||
| Much more active (8) | Somewhat more active (6) | Same as before (4) |
| Somewhat less active (2) | Much less active (0) | |
| 9. How much shorter does one leg feel compared to the other when standing or walking? (8 points) | ||
| Does not feel short (8) | Slightly short (6) | Moderately short (4) |
| Very short (2) | Extremely short (0) | |
| 10. How difficult is it for you to jump? (5 points) | ||
| Not at all difficult (5) | Somewhat difficult (4) | Moderately difficult (3) |
| Very difficult (2) | Extremely difficult (1) | Unable (0) |
| 11. How difficult is it for you to go up and down stairs? (5 points) | ||
| Not at all difficult (5) | Somewhat difficult (4) | Moderately difficult (3) |
| Very difficult (2) | Extremely difficult (1) | Unable (0) |
| 12. How difficult is it for you to squat or stoop? (5 points) | ||
| Not at all difficult (5) | Somewhat difficult (4) | Moderately difficult (3) |
| Very difficult (2) | Extremely difficult (1) | Unable (0) |
The value of each weighted response to the questionnaire is listed in Table 1. The total score for each patient was graded on a 93-point scale and recorded as a percentage. The patients were divided into four groups: excellent, good, and fair scores were divided into groups of 16 percentage points so that an excellent score was greater than 84%, good greater than 68% and fair greater than 52%, respectively. A poor score was less than 52%. This scale was chosen based upon our clinical data and the absence of any patient reported outcome scale for pediatric patients with limb deformity.
The radiographic results were determined from the four measured parameters which calculated one of the three deformities of the leg: varus at the knee, downward medial slope and posterior slope of the medial tibial plateau. Preoperatively, a small number of tibias had normal posterior slope for which correction credit was granted in each case. Again, the patients were grouped into four groups: excellent if three of the four radiographic measurements were corrected, good if either MAA or AAA and one other parameter was corrected, fair if one abnormal parameter was corrected, and poor if none of the abnormal measurements were corrected.
Operative Technique
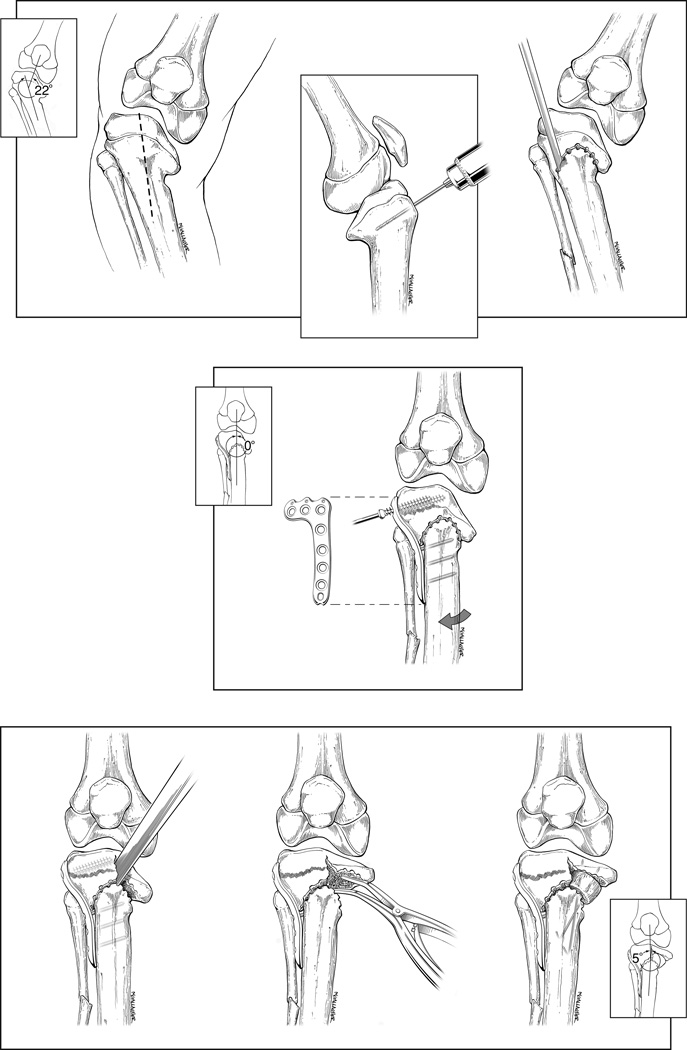
The main operative steps are illustrated in Figure 2. An oblique fibula osteotomy was performed. The proximal tibia was approached by a 14 cm midline straight skin incision from the midpatellar ligament, and down the anterior surface of the tibia (Fig. 2A). Strategically placed Chandler retractors protected the posterior neurovascular structures in the popliteal fossa. A subperiosteal dome osteotomy was outlined by multiple 3.2 mm holes 3 cm distal to the joint and centered about the tibial tubercle and extending out ot the medial and lateral cortices. The drill bit was angled distally and parallel to the joint subchondral bone on the sagittal plane (Fig. 2B). A lateral fluoroscopic radiograph was used to confirm the correct position of the drill bit. A 6 mm straight osteotome was used to connect the drill holes (Fig. 2C).
Fig. 2.
A–G Double tibial and fibular osteotomies surgical steps. (A) Skin incision. (B) drill bit is placed at apex of planned dome osteotomy and parallel to joint surface. (C) Dome osteotomy is outlined by drill holes and completed by osteotome. (D) lateral tibial plateau plate is applied with leg in corrected position and proximal to the growth plate. (E) Vertical osteotomy is performed from the apex of the dome osteotomy to subchondral bone. (F) Spinal laminar spreader is used to fully elevate the medial tibial plateau and corrects the posterior procurvatum. (G) elevated medial tibial plateau is supposed with bone graft-materials and stabilized with Kirschner wire(s).
The lower leg was extended fully and externally rotated to 10 degrees or to the same degree as the normal contralateral leg. The genu varus deformity was corrected to neutral or 5 degrees valgus. An electrocautery cord placed over the femoral head, knee and to the mid ankle joint confirmed the desired mechanical axis alignment with fluoroscopy. A 6-hole lateral tibial plateau plate was applied with the leg in the desired alignment (Fig. 2D). The lateral hemi-epiphysiodesis is accomplished by placing the proximal screws on the epiphyseal side of the the growth plate and then advancing them to the midline of the tibia so as not to interfere with the second vertical osteotomy.
The second osteotomy was performed with fluoroscopic guidance. An osteotome was placed anteriorly at the apex of the dome just medial to the proximal screw tips and extending proximal through the growth plate (Fig 2E). It was hammered into the bone vertically and parallel to the joint’s subchondral bone. The posterior cortex was osteotomized completely. A deeply placed spinal laminar spreader was used to completely hinge open the medial tibial plateau to correct its medial and posterior distal slopes (Fig. 2F). The maximally elevated plateau was supported by one or two full thickness diaphyseal fibula allografts, cut to fit the space. Iliac crest autograft is an alternative option. The impacted graft(s) was immobilized with one or two retrogradely placed Kirschner wire(s). At the end of the procedure, replacing a proximal screw(s) with longer one(s) may be considered provided that the graft complex is not disrupted.
A hemovac drain was placed. The periosteum was repaired. The tibialis anterior muscle was loosely and partially approximated over the drain and the wound was closed. Long-leg casts were applied for up to four months and discontinued if monthly radiographs determined evidence of bony union at both osteotomy sites. At that time, the patient was advanced from touch down weight bearing to full weight bearing.
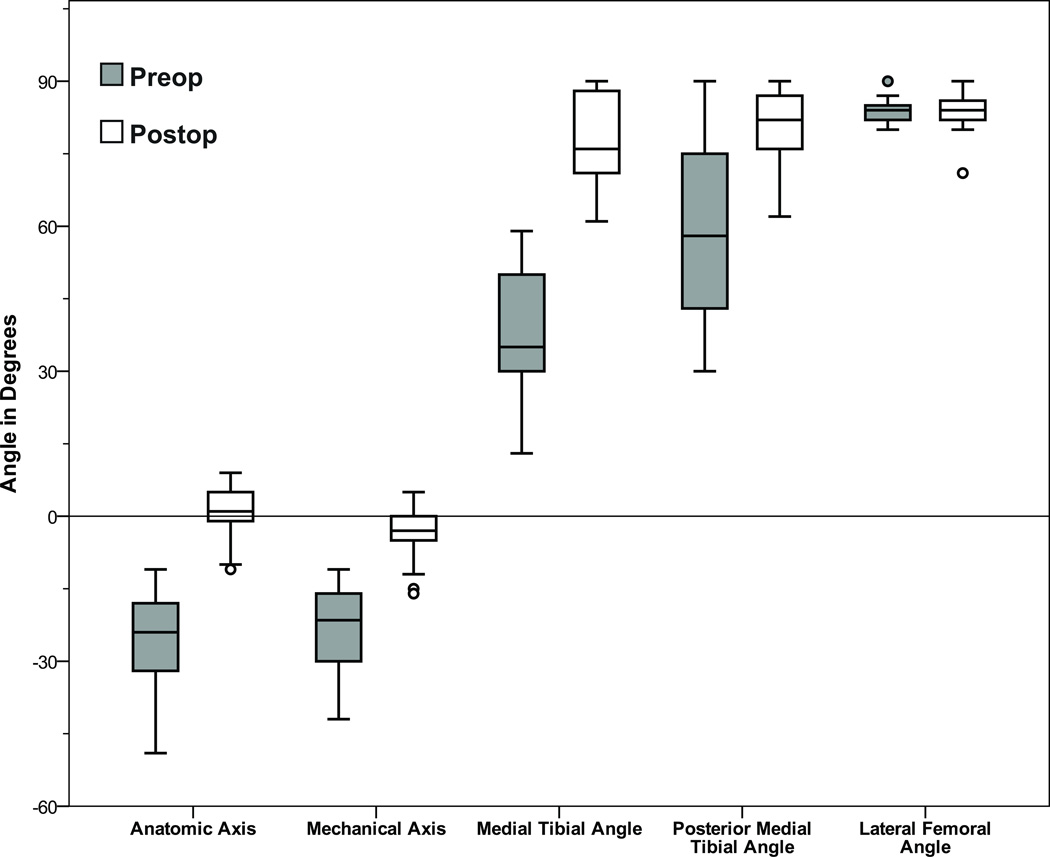
Statistical Analysis
The data for this study was imported into the SPSS software package, version 23 (Armonk, New York) for analysis. It was determined the radiographic parameters followed a non-parametric distribution. As a result, the medians are reported with the means, due to their robustness against outlier influence. For significance testing, the non-parametric Wilcoxon signed-rank test measured paired data. In all cases, statistical significance was set at the 0.05 level. The box-and-whisker-plot used in Figure 3 follows standard conventions.
Fig. 3.
Box and whisker plot used to show the preoperative and postoperative radiographic measurements. The median value is represented by the line within the vertical box. The box spans from the 25th to the 75th percentile. Minor and extreme outliers are denoted by circles and stars, respectively. Negative values indicate varus. Note with the exception of the lateral femoral angle results there was significant correction radiographically of the remaining deformities (p<0.001).
Source of Funding
A portion of the project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR000050.
Results
Radiographic Outcome
The results of the radiographic data which include mean and median are shown in Table 2 and Figure 3. The procedure improved each of the four tibial radiographic angles on a significance level <0.001. The preoperative and follow-up LFA of the femur did not change significantly.
Overall radiographic outcomes were good or excellent in 23 of 29 knees (79%), three were fair and three were poor. Of the seven unilateral knees, five had good or excellent outcomes and one had a fair result and one a poor result. Of the bilateral 22 knees, 18 had good or excellent results, two had fair and two had poor outcomes.
At most recent follow-up, the MAA was within the range of −5 to 5 degrees in 24 of 29 (83%) knees. The AAA was within the range of 11 to 1 degrees in fifteen of 29 (52%) knees. Additionally, the postoperative MTA and PMTA angles were within the normal adult range in 11 of 29 (38%) and 16 of 29 (55%) knees, respectively. Achieving the normal adult values for these 5 parameters were the goals we hoped to achieve in the study. Because of the complex and chronic nature of the multiple deformities in each patient it was not possible to achieve normal adult values in all cases of the deformities particularly the severe cases.
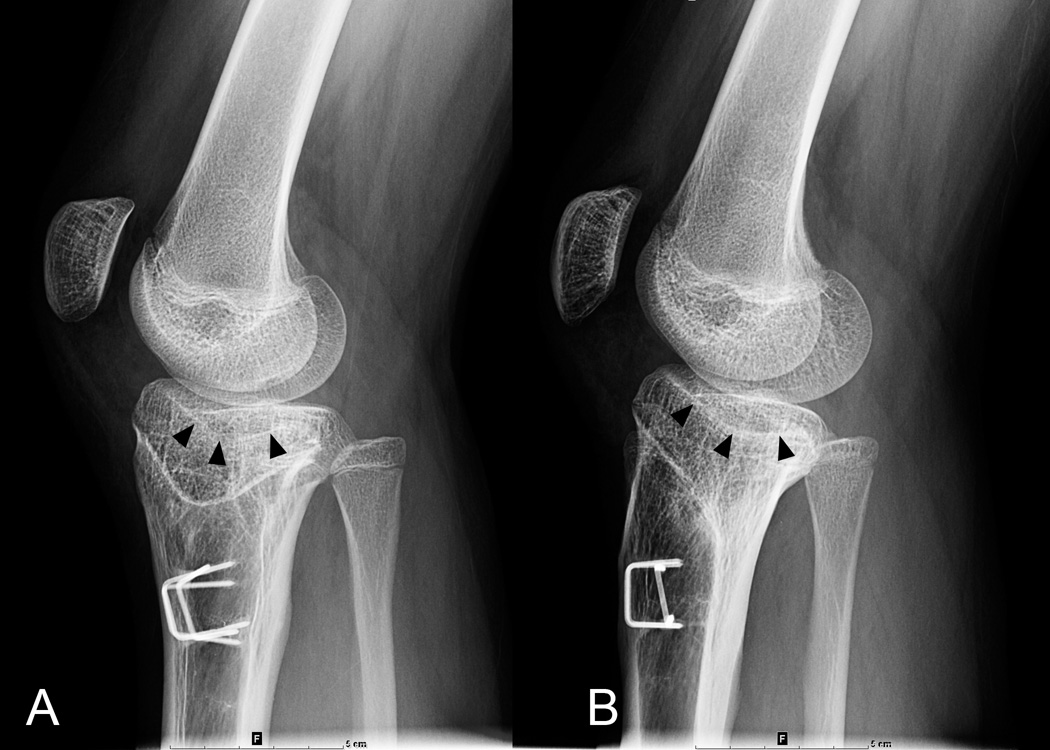
Two types of medial tibial plateau deformities were identified (Fig. 4). In Type 1 knees (n=19, 66%), the PMTA was greater than two standard deviations of normal (80±3 degrees) or a procurvatum slope greater than 16 degrees. In Type II knees (n=10, 34%), the PMTA was within two standard deviations or less than 16 degrees. Medial downward slope and central depression of the medial tibial plateau were present in both types. Increased central depression and persistent abnormal procurvatum of the medial tibial plateau may be important contributory factors for the premature development of knee osteoarthritis in these patients (Fig. 5).
Fig. 4.
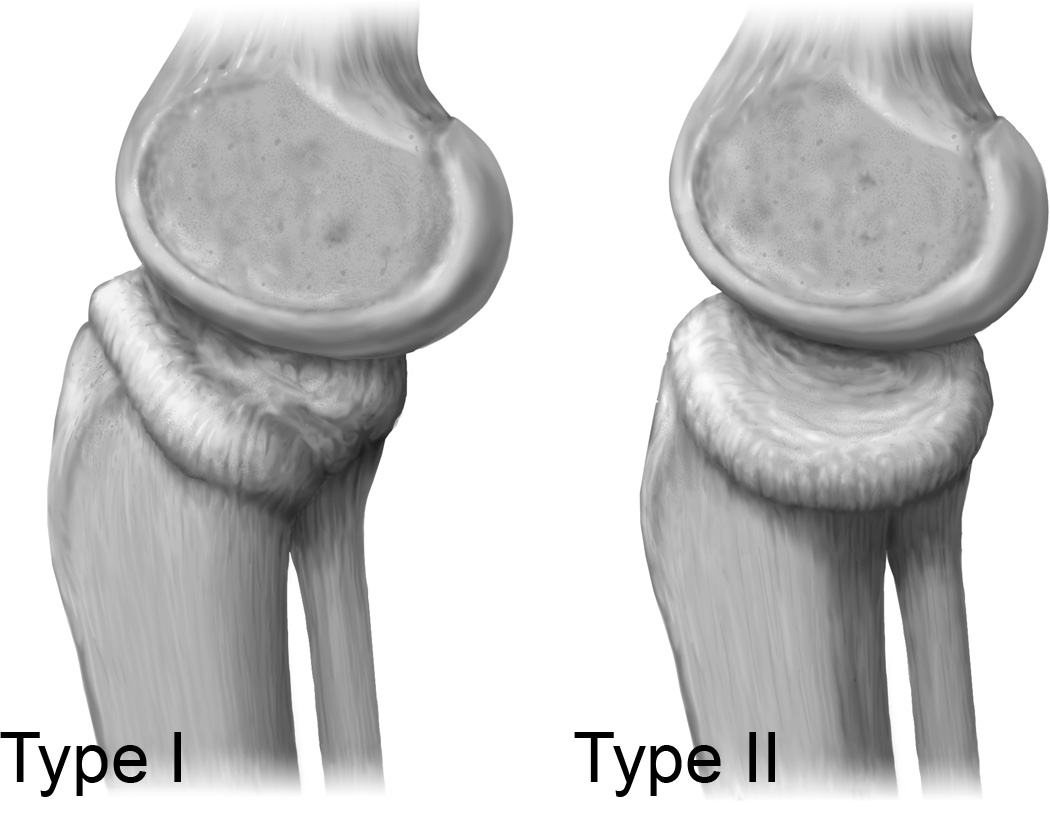
Type I and Type II deformity patterns of the medial tibial plateau were seen. Type I, both medial and posterior slopes were present. Type II, only the medial tibial slope inclination was noted. Increased central depression of the medial tibial tibial plateau was seen radiographically in both types.
Fig. 5.
A–B Lateral views of (A) right and (B) left knees 5 years postoperatively. Note the increased depression of the central portion of the medial tibial plateau (black arrow heads).
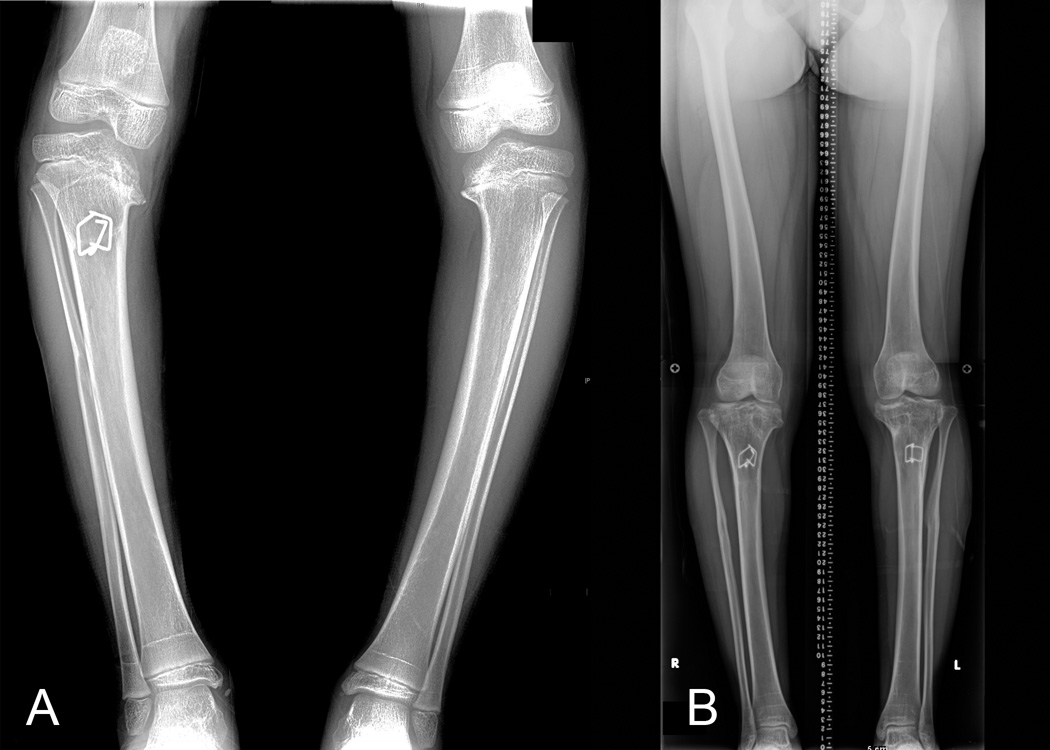
Questionnaire Outcome
The questionnaire outcome results of the 19 patients studied can be found in Table 3. Eighteen were overall satisfied with the surgery. Patients with bilateral ITV did not have a lower limb discrepancy greater than one centimeter regardless of treatment on either tibia (Fig. 6). For the seven unilateral ITV cases the average shortening of the operative leg was 24mm (8–35mm) at follow-up. Two of these patients underwent contralateral proximal tibial epiphysiodesis (Fig. 7).
Table 3.
Summary of the patient reported clinical outcomes subdivided by bilateral and unilateral disease and summary of patients’ reported outcome by satisfaction, pain, and function.
| Outcome | All Patients | Bilateral Disease |
Unilateral Disease |
|---|---|---|---|
| Excellent | 3 | 1 | 2 |
| Good | 11 | 8 | 3 |
| Fair | 4 | 3 | 1 |
| Poor | 1 | 1 | 0 |
| Total | 19 | 13 | 6 |
| Satisfaction | Pain | Function | |
|---|---|---|---|
| Excellent | 9 | 9 | 5 |
| Good | 6 | 3 | 11 |
| Fair | 4 | 1 | 1 |
| Poor | 0 | 6 | 2 |
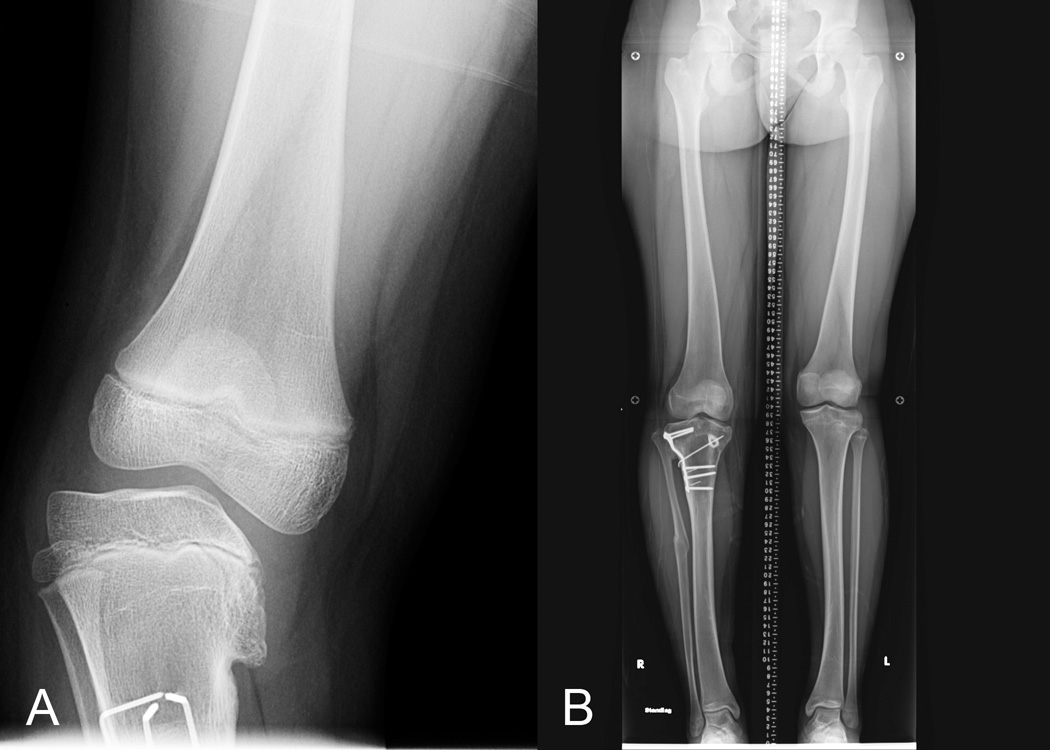
Fig. 6.
Case 6 patient with bilateral ITV (A) preoperative radiographs and (B) bilateral correction of mechanical axes measured within one degrees of zero. Limb length discrepancy was less than one cm.
Fig. 7.
Case 7, unilateral case, MAA at follow-up was 0 degrees. Subsequent, contralateral epiphysiodesis of proximal tibia limited the limb length discrepancy to eight mm.
The mean BMI at follow-up was 36 (range 19–70). At follow-up knees achieved a mean of 127 degrees of flexion (range 95–150 degrees. Three of 4 knees with 10 degrees of flexion contracture reoperatively gained full extension at follow-up. And 3 of 4 knees developed knee contractures of 10–15 degrees postoperatively. The remaining 25 knees were able to fully extend to 0 degrees. Increased obesity contributed to those patients with decrease knee flexion.
Increased internal tibial torsion which was present in each patient preoperatively was corrected to approximately 10 degrees of external rotation at the time of surgery. We were unable to accurately measure the patients’ thigh-foot angle without formal gait analysis studies, however, in the clinic setting angle appeared to improve to within 20 degrees of internal or external rotation in all cases.
There were no cases of avascular necrosis, nonunion, or compartment syndrome in our patients. There was one superficial infection, a deep infection and a wound dehiscence. There was also a transient and a permanent partial common peroneal nerve paresis. The latter occurred in Case 26, who had a BMI of 42, Type I diabetes and preoperatively had an anatomical axis of 32 degrees of varus.
Discussion
The oblique deformity seen in late-presenting ITV treated with a single-stage double tibial osteotomy performed proximal to the tibial tubercle gave good to excellent radiographic results in 23 of 29 knees (79%). Also, the 19 clinical outcomes questionnaires reported good to excellent outcomes in 14 of 19 patients. Those results compare most favorably to other comparable recent studies [18,28].
We attribute the three poor and three fair radiographic results to under-correction of the varus deformity. This was primarily due to failure to correct the varus with the dome part of the osteotomy to 0–5 degrees valgus since a proximal lateral tibial hemi-epiphysiodesis is performed. The vertical osteotomy which is used to elevate the medial tibial plateau is not expected to add more than 5 degrees of additional valgus correction because of the presence of the medial meniscus and unossified tibial plateau [20].
Limb length is preserved since no significant bone is removed to correct the varus and internal torsion. Since the osteotomy is performed at the level of the apex of the tibial deformity only axial correction without translocation is necessary to correct the varus [29]. It is important for anyone attempting this procedure to feel comfortable at performing the posterior tibial corticotomies as described. The popliteal and medial inferior geniculate arteries are in the immediate vicinity of the posterior corticotomies and are partially protected by the muscle belly of the popliteus muscle (Fig. 8).
Fig. 8.
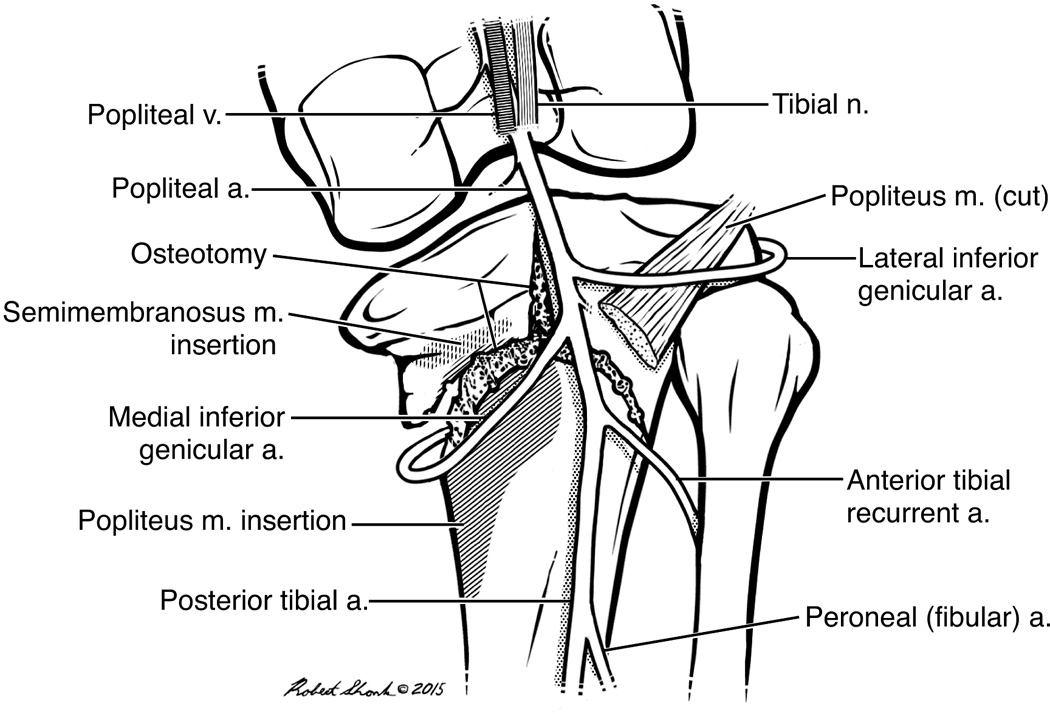
Anatomical illustration of the posterior view of the double osteotomy it relates to the arterial vessels in and about the popliteal fossa. The deeper popliteus muscle belly offers some protection to the vessels.
An in-depth research of the ITV literature failed to cite any studies using external fixators with more than 9 patients and or with a mean follow-up greater that 29 months [8, 11, 13]. In one study 6 cases treated with the Taylor Spatial Frame were followed on average of 29 months [8]. They reported good results in all cases with the use of Schoenecker criteria. Also another study of 7 patients with and average follow-up of 29 months reported on their use of the Ilizarov Frame [13]. All their patients were improved and they were pleased with the results. We believe that these external fixator devices are better suited for the adolescent tibia vara where depression of the medial tibial plateau is less severe and where it’s elevation of the medial tibial plateau is required.
Others have attempted to rate the surgical outcome of treatment of the complex oblique deformity [13, 18, 28]. Though none have used all four of the major radiographic parameters and thus we feel their ratings are incomplete. The same can be said for assessing clinical outcomes on levels of pain. We sought to expand on previous attempts with a more comprehensive method involving four radiographic measures and a clinical outcome instrument to better evaluate and standardize results.
Based on the data collected and tabulated (Table 2) no patient had a MAA or AAA less than 11 degrees. This does not mean that the same patient had a MAA equal to an AAA. In reviewing the literature for patients with ITV, either the AAA [13, 18] or MAA [28] is used to calculate results. Here we used both measurements so as to compare our data with these publications. Since the measurements of the AAA is readily available in all radiology facilities, it can be used in defining our indication criteria. On the other hand, the MAA which may not be readily available in some radiology departments is a more accurate measurement of the lower limb alignment in the frontal plane. The addition of 6 degrees to the AAA to create a MAA was not always reproducible in our patient population. And this we believe is mainly due to the difficulty in defining the correct anatomical line of the femur and tibia which may present with varying degrees of varus and rotation for a given patient. These anatomical lines can also be affected by a knee subluxation. We found that the MAA which bypasses these issues to be easier and more reliable to measure that the AAA.
There are several limitations to the study. First, the techniques used to take the radiographs might not always have been standardized. Also, the actual measurements of the radiographic angles were subjected to individual bias. Second, the severity and chronicity of the oblique deformity of the medial tibial plateau made the comparison of some radiographic measurements to the normal stringent adult values difficult to achieve with the exception of the MAA and to a lesser extent the AAA. Third, a relatively small patient population may lead to inaccurate conclusions. This concern was off-set by high patient participation, the same principal medical team and a moderately long period of follow-up. This study’s size compares most favorably to other studies mentioned.
In conclusion, to our knowledge, this is the first study to present the technique and outcome of a single stage double tibial osteotomy performed proximal to the tibial tubercle for late presenting ITV for children seven years or older. This comprehensive operation effectively corrects, in most cases, the four known deformities of tibial vara. A contralateral proximal tibial epiphysiodesis is recommended in the skeletally immature patient with unilateral disease. Based upon our outcomes, we are comfortable in recommending this technique for ITV patients.
Supplementary Material
Acknowledgments
We thank Kaleigh Sands and Priyanka Nasa from the Center of Clinical and Translational Science for their assistance with the clinical outcome questionnaire.
Sources of Support: National Center for Advancing Translational Sciences, at the University of Illinois School of Medicine at Chicago, National Institutes of Health, through Grant UL1TR000050 was used in part to fund this research study. No authors received any funding personally.
Footnotes
The authors declare that they do not have a conflict of interest.
References
- 1.Ferriter P, Shapiro F. Infantile tibia vara: factors affecting outcome following proximal tibial osteotomy. J Pediatr Orthop. 1987 Jan-Feb;7(1):1–7. [PubMed] [Google Scholar]
- 2.Loder RT, Johnston CE. Infantile tibia vara. J Pediatr Orthop. 1987 Nov-Dec;7(6):639–646. [PubMed] [Google Scholar]
- 3.Greene WB. Infantile Tibia Vara. J Bone Joint Surg Am. 1993 Jan;75(1):130–143. doi: 10.2106/00004623-199301000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Zionts LE, Shean CJ. Brace treatment of early infantile tibia vara. J Pediatr Orthop. 1998 Jan-Feb;18(1):102–109. [PubMed] [Google Scholar]
- 5.Richards BS, Katz DE, Sims JB. Effectiveness of brace treatment in early infantile Blount’s disease. J Pediatr Orthop. 1998 May-Jun;18(3):374–380. [PubMed] [Google Scholar]
- 6.Raney EM, Topoleski TA, Yaghoubian R, et al. Orthotic treatment of infantile tibia vara. J Pediatr Orthop. 1998 Sep-Oct;18(5):670–674. doi: 10.1097/00004694-199809000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Blount WP. Tibia vara: Osteochondrosis deformans tibiae. J Bone Joint Surg Am. 1937;19(1):1–29. [Google Scholar]
- 8.Feldman DS, Madan SS, Koval KJ, et al. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop. 2003 May-Jun;23(3):387–391. [PubMed] [Google Scholar]
- 9.Jones S, Hosalkar HS, Hill RA, et al. Relapsed infantile Blount’s disease treated by hemiplateau elevation using the Ilizarov frame. J Bone Joint Surg Br. 2003 May;85(4):565–571. doi: 10.1302/0301-620x.85b4.13602. [DOI] [PubMed] [Google Scholar]
- 10.Tavares JO, Molinero K. Elevation of medial tibial condyle for severe tibia vara. J Pediatr Orthop B. 2006 Sep;15(5):362–369. doi: 10.1097/01202412-200609000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Janoyer M, Jabbari H, Rouvillain JL, et al. Infantile Blount’s disease treated by hemiplateau elevation and epiphyseal distraction using a specific external fixator: preliminary report. J Pediatr Orthop B. 2007 Jul;16(4):273–280. doi: 10.1097/01.bpb.0000210591.35652.84. [DOI] [PubMed] [Google Scholar]
- 12.Beck CL, Burke SW, Roberts JM, et al. Physeal bridge resection in infantile Blount disease. J Pediatr Orthop. 1987 Mar-Apr;7(2):161–163. doi: 10.1097/01241398-198703000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Schoenecker PL, Meade WC, Pierron RL, et al. Blount’s disease: a retrospective review and recommendations for treatment. J Pediatr Orthop. 1985 Mar-Apr;5(2):181–186. [PubMed] [Google Scholar]
- 14.Gregosiewicz A, Wośko I, Kandzierski G, et al. Double-elevating osteotomy of tibiae in the treatment of severe cases of Blount's disease. J Pediatr Orthop. 1989 Mar-Apr;9(2):178–181. [PubMed] [Google Scholar]
- 15.Accadbled F, Laville JM, Harper L. One-step treatment for evolved Blount's disease: four cases and review of the literature. J Pediatr Orthop. 2003 Nov-Dec;23(6):747–752. [PubMed] [Google Scholar]
- 16.Hefny H, Shalaby H, El-Kawy S, et al. A new double elevating osteotomy in management of severe neglected infantile tibia vara using the Ilizarov technique. J Pediatr Orthop. 2006 Mar-Apr;26(2):233–237. doi: 10.1097/01.bpo.0000218530.59233.ab. [DOI] [PubMed] [Google Scholar]
- 17.Andrade N, Johnston CE. Medial epiphysiolysis in severe infantile tibia vara. J Pediatr Orthop. 2006 Sep-Oct;26(5):652–658. doi: 10.1097/01.bpo.0000230338.03782.75. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy JJ, MacIntyre NR, Hooks B, et al. Double osteotomy for the treatment of severe Blount disease. J Pediatr Orthop. 2009 Mar;29(2):115–119. doi: 10.1097/BPO.0b013e3181982512. [DOI] [PubMed] [Google Scholar]
- 19.Hofmann A, Jones RE, Herring JA. Blount’s disease after skeletal maturity. J Bone Joint Surg Am. 1982 Sep;64(7):1004–1009. [PubMed] [Google Scholar]
- 20.Sabharwal S. Blount disease. J Bone Joint Surg Am. 2009 Jul;91(7):1758–1776. doi: 10.2106/JBJS.H.01348. [DOI] [PubMed] [Google Scholar]
- 21.Langenskiold A. Tibia vara (osteochondrosis deformans tibiae); a survey of 23 cases. Acta Chir Scand. 1952 Mar 26;103(1):1–22. [PubMed] [Google Scholar]
- 22.Gugenheim JJ. Clinical Evaluation Including Imaging. In: Sabharwal S, editor. Pediatric Lower Limb Deformities. New York: Springer International Publishing; 2016. pp. 15–36. [Google Scholar]
- 23.Brown GA, Amendola A. Radiographic evaluation and preoperative planning for high tibial osteotomies. Oper Tech Sports Med. 2000 Jan;8(1):2–14. [Google Scholar]
- 24.Ferrick MR, Birch JG, Albright M. Correction of non-Blount's angular knee deformity by permanent hemiepiphyseodesis. J Pediatr Orthop. 2004 Jul-Aug;24(4):397–402. doi: 10.1097/00004694-200407000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Rozbruch SR, Hamdy RC. Limb Lengthening and Reconstruction Case Atlas. New York: Springer International Publishing; 2015. p.xxxiii-Liii. [Google Scholar]
- 26.George D, Mallery P. 11.0 update. 4th. Boston: Allyn & Bacon; 2003. SPSS for Windows step by step: A simple guide and reference. [Google Scholar]
- 27.Graham B, Green A, James M, et al. Measuring patient satisfaction in orthopaedic surgery. J Bone Joint Surg Am. The Journal of Bone and Joint Surgery Inc. 2015 Jan 7;97(1):80–84. doi: 10.2106/JBJS.N.00811. [DOI] [PubMed] [Google Scholar]
- 28.van Huyssteen AL, Hastings CJ, Olesak M, et al. Double-elevating osteotomy for late-presenting infantile Blount’s disease. J Bone Joint Surg Br. 2005 May;87(5):710–715. doi: 10.1302/0301-620X.87B5.15473. [DOI] [PubMed] [Google Scholar]
- 29.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992 Jul;(280):48–64. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.