Abstract
Background
Chronic lumbar radiculopathy has a lifetime prevalence of 5.3% in men and 3.7% in women. It usually resolves spontaneously, but up to 30% cases will have pronounced symptoms even after one year.
Aims
A prospective randomized single-blind study was conducted to compare the efficacy of caudal epidural steroid injection and selective nerve root block in management of pain and disability in cases of lumbar disc herniation.
Methods
Eighty patients with confirmed single-level lumbar disc herniation were equally divided in two groups: (a) caudal epidural and (b) selective nerve root block group, by a computer-generated random allocation method. The caudal group received three injections of steroid mixed with local anesthetics while selective nerve root block group received single injection of steroid mixed with local anesthetic agent. Patients were assessed for pain relief and reduction in disability.
Results
In SNRB group, pain reduced by more than 50% up till 6 months, while in caudal group more than 50% reduction of pain was maintained till 1 year. The reduction in ODI in SNRB group was 52.8% till 3 months, 48.6% till 6 months, and 46.7% at 1 year, while in caudal group the improvement was 59.6%, 64.6%, 65.1%, and 65.4% at corresponding follow-up periods, respectively.
Conclusions
Caudal epidural block is an easy and safe method with better pain relief and improvement in functional disability than selective nerve root block. Selective nerve root block injection is technically more demanding and has to be given by a skilled anesthetist.
Keywords: Selective nerve root block, SNRB, Caudal epidural, Disc prolapse, Lumbar radiculopathy
1. Introduction
Chronic lumbar radiculopathy is defined as a clinical syndrome of back and leg pain accompanied by sensory, reflex, or motor deficits in a nerve root distribution lasting for more than 12 weeks.1, 2, 3, 4 The lifetime prevalence of lumbar radiculopathy has been reported to be 5.3% in men and 3.7% in women.5, 6 Lumbar radiculopathy due to a prolapsed disc resolves spontaneously in 23–48% of patients, but up to 30% will still have pronounced symptoms after one year, 20% will be out of work, and 5–15% will undergo surgery.7, 8, 9, 10
2. Aims
A prospective randomized single-blind study was conducted to compare the efficacy of caudal epidural steroid injection and lumbar steroid injection (selective nerve root block) in management of pain associated with prolapsed lumbar intervertebral disc in patients who were not relieved by nonsurgical treatment modalities.
3. Materials and methods
The study was conducted in tertiary care hospital from December 2013 to December 2014. Patients of lumbar disc herniation at one level with backache and radiculopathy, who failed to respond to conservative therapy for duration of 6 weeks, were included in the study. The diagnosis of lumbar disc herniation was confirmed clinically and radiologically by MRI. The exclusion criteria included patients with prior back surgery, cauda equina syndrome, back pain or radiculopathy due to other causes (facet joint pain and spinal canal stenosis), pain secondary to traumatic spinal fracture, neoplastic and vascular causes, pregnancy, and lactating mothers.
The study was cleared by the Institutional Research Committee and the Ethical Committee. Informed written consent was taken from all those included in the study. The sample size was calculated based on significant pain relief considering a 0.05 two-sided significance level, a power of 80%, and an allocation ratio of 1:1; 40 participants in each group were estimated. There were 80 cases enrolled in the study. Computer-generated random allocation was done in two groups: (a) caudal epidural and (b) selective nerve root block group.
Written and informed consent for both the procedures was obtained from all subjects. The procedures were conducted under C-arm imaging control, by an orthopedic specialist in caudal epidural injection and by an anesthesia specialist in selective nerve route block group in an operation theater. The caudal group patients received 2 ml of methyl prednisolone (80 mg) along with10 ml of lignocaine (2%) diluted in 20 ml of normal saline. A total of 3 caudal epidural injections were given at an interval of 3 weeks irrespective of previous epidural injection effect. Selective nerve root block (SNRB) was given by a single injection of 2 ml of methyl prednisolone (80 mg) mixed with 5 ml of lignocaine (2%).
3.1. Technique for caudal epidural injection
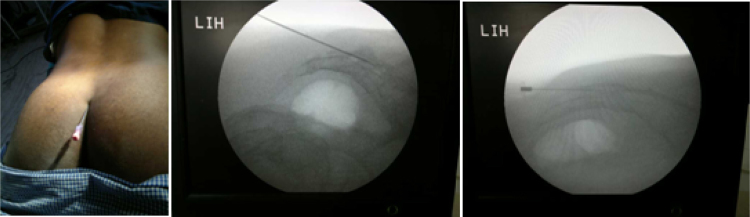
The entry point for caudal epidural injection is the sacral hiatus. The drug is administered to distribute the steroid cephalad in the epidural space. Patients were asked to lie down in prone position with a pillow under lower abdomen and pelvic. The needle puncture site was identified and marked on skin. After proper antiseptic dressing and draping, the proposed site of needle entry was infiltrated with local anesthetic. The procedure was performed under C-arm guidance. A 20-gauge spinal needle was introduced through sacral hiatus at about 45°. Once inside the sacral hiatus, the needle is horizontally advanced in cephalad direction using C-arm guidance into the epidural space (Fig. 1). The final position of needle was confirmed under C-arm. After removal of the stylus and aspiration to check for blood or CSF, the drug was injected.
Fig. 1.
Clinical and C-arm images showing needle placement for caudal epidural injection
3.2. Technique for nerve root blocks
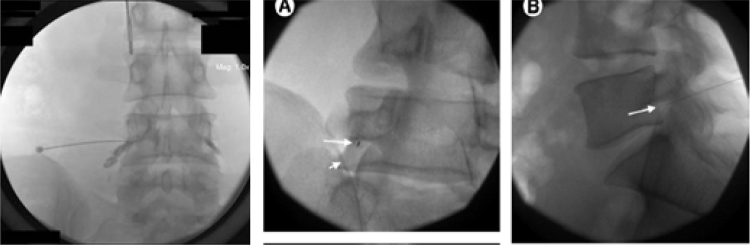
The patient was placed in a prone position. After painting and draping the area and identifying the affected level using anteroposterior and lateral fluoroscopic imaging, we infiltrate the skin 5–8 cm from midline with 2 ml of local anesthetic drug and a 20-gauge needle that was inserted and advanced until it comes in contact with the dorsal superior and medial aspect of the base of the transverse process. Here, we try to elicit the paresthesia along the affected root, and once the patient confirms the paresthesia, we inject 2 ml of radio-opaque dye and see the spread of the dye along the affected root using the C-arm, both in anterior and lateral views (Fig. 2). The position of needle can also be confirmed in oblique view, where the position of the needle should be in the middle of the eye of Scotty dog. Once confirmed, the drug is slowly injected. The procedure is repeated on the opposite side or to the other roots, if required, in a similar manner. After the procedure, patients were observed in postoperative room for one hour and were discharged thereafter.
Fig. 2.
Anteroposterior, lateral, and oblique C-arm images with needle placement and spread of dye along the nerve root.
All patients were assessed clinically and neurologically. The visual analog scale (VAS) pain score for assessment of pain and Oswestry Disability Scale (ODI) on a 0–50 point scale, in which a higher score represented greater disability to quantitate the level of function, was recorded initially and at follow-ups. Any decrement in the VAS pain scores of more than two scales was considered to be significant. In Oswestry Disability Scale (ODI), higher score represented greater disability. A positive response was defined as 50% or more pain relief within 3 weeks of the procedure along with at least a 40% reduction in ODI score. Any complication during the study period was recorded. The patients were given NSAIDs as rescue medications on an as and when needed. The patients were followed up at one month, 3 months, 6 months, and at 1 year after the procedure.
The data were analyzed by statistical software SPSS version 17.0. The categorical data were analyzed by using the Chi-square test, while the continuous variables were analyzed by using the Student t-test and repeated ANOVA, wherever required. The results were presented as median (range) and number (percentage) for continuous variables. P value <0.05 was considered as statistically significant and p values <0.001 as highly significant.
4. Results
There were a total of 80 patients (49 men and 31 women). Each group had 40 patients. The average age was 36.48 ± 10.5 (range: 18–62) years in SNRB group while it was 36.98 ± 11.3 in caudal group. The average height was 173.7 ± 8.1 cm (range: 152–187 cm) in SNRB group and 170.17 ± 9.02 in caudal group. The average weight was 79.93 ± 8.7 (range: 68–99) kg in SNRB group and 80.12 ± 9.6 kg in caudal group. The average duration of pain was 15.07 ± 3.3 months in SNRB group and 11.08 ± 3.8 in caudal group (Table 1). The demographic profile of both the groups was comparable.
Table 1.
Showing demographic data of studied patients.
| Demographic parameter | Groups |
p value | |||||
|---|---|---|---|---|---|---|---|
| SNRB |
Caudal |
||||||
| N | Mean ± SD | Range | N | Mean ± SD | Range | ||
| Age (year) | 40 | 36.48 ± 10.5 | (18–62) | 40 | 36.98 ± 11.3 | (19–58) | 0.839 |
| Weight (kg) | 40 | 79.93 ± 8.7 | (68–99) | 40 | 80.12 ± 9.6 | (66–99) | 0.922 |
| Height (cm) | 40 | 173.70 ± 8.1 | (152–187) | 40 | 170.17 ± 9.02 | (145–187) | 0.070 |
| Duration of pain (months) | 40 | 15.07 ± 3.3 | (9–26) | 40 | 11.08 ± 3.8 | (3–19) | 0.000 |
| Onset of pain (acute) | 40 (100%) | 40 (100%) | A | ||||
Intervertebral disc prolapse was seen at L1–L2 level in 3 cases (2 in SNRB and 1 in caudal group), at L3–L4 level in 16 cases (8 each in SNRB and caudal group), at L4–L5 level in 43 cases (20 in SNRB group and 23 in caudal group), and at L5–S1 level in 18 cases (10 in SNRB group and 8 in caudal group). In SNRB group, the initial VAS was 7.65 ± 0.5, which reduced to 4.07 ± 0.9 at one-year follow-up, while in caudal group, initial VAS was 7.42 ± 0.6, which was reduced to 3.10 ± 1.5. In SNRB group, the initial ODI was 78.20 ± 2.8, which reduced to 41.70 ± 5.5 at one-year of follow-up, while in caudal group, the initial ODI was 78.15 ± 5.4, which reduced to 27.00 ± 14.1 at one-year of follow-up (Table 2). In both groups, there was decrease in ODI of more than 40%, it is considered significant in terms of reduction of disability (Table 2). One case in caudal epidural injection group (L1–2) and 4 cases in selective nerve root block group (L4–5 & L5–S1) failed to show a positive response within 3 weeks after the injection. There were no complications observed in our study. No patient was lost to follow-up.
Table 2.
Showing degree of improvement in VAS and ODI for Caudal and SNRB groups at follow-up.
| VAS |
ODI |
|||||||
|---|---|---|---|---|---|---|---|---|
| SNRB (Mean ± SD) | Improved (%) | Caudal (Mean ± SD) | Improved (%) | SNRB (Mean ± SD) | Decreased (%) | Caudal (Mean ± SD) | Decreased (%) | |
| Initial | 7.65 ± 0.5 | – | 7.42 ± 0.6 | – | 78.20 ± 2.8 | – | 78.15 ± 05.4 | – |
| After 1 month | 3.23 ± 0.5 | 57.7% | 2.85 ± 0.7 | 61.0% | 36.90 ± 7.1 | 52.8% | 31.55 ± 08.7 | 59.6% |
| After 3 months | 3.40 ± 0.7 | 55.5% | 3.00 ± 1.2 | 61.5% | 39.55 ± 5.1 | 52.8% | 27.60 ± 11.8 | 64.6% |
| After 6 months | 3.60 ± 0.8 | 52.9% | 2.93 ± 1.3 | 59.6% | 40.20 ± 5.2 | 48.6% | 27.20 ± 13.9 | 65.1% |
| After 1 year | 4.07 ± 0.9 | 46.8% | 3.10 ± 1.5 | 58.2% | 41.70 ± 5.5 | 46.7% | 27.00 ± 14.1 | 65.4% |
5. Discussion
Epidural steroid injections for lumbar radiculopathy have been used since 1953.11 Along with mechanical compression of nerve roots, lumbar radiculopathy can be triggered by different proinflammatory chemical agents, causing ectopic neuron firing.12, 13, 14, 15, 16 Steroids injected into the epidural space or around the affected nerve root are thought to inhibit these inflammatory mediators. It is believed that epidural steroid injection reduces inflammatory edema of the injured nerve roots, decreases sensitization of the dorsal horn neurons, and suppresses the transmission of nociceptive C-fibers.17
Epidural injections are the most common pharmacological interventions performed in nonsurgical pain management of lower back pain. The drug used most commonly is either a local anesthetic or a corticosteroid or a combination of local anesthetic and steroid. There have been diverse claims of better efficacy in relieving pain and improvement of functions by all of these different drug combinations, but the recent evidence shows that local anesthetics with or without steroids are equally effective.18, 19, 20, 21 We had used methyl prednisolone (80 mg), though no added advantage of giving the medication in higher dose has been reported.22, 23 Three principal routes have been used to deliver medication into the lumbar epidural space: (a) the caudal route, (b) the transforaminal route, and (c) interlaminar route.24
The caudal route was used more often in earlier studies, but in later studies, interlaminar route is more often used. Presently, transforaminal route is in vogue.25 All three routes have their own advantages and complexities. The caudal route utilizes larger volumes of drug and is given away from the pathology site, but it is the easiest and safest route with minimal risk of dural puncture.26, 27 The interlaminar route delivers the drug closer to the pathology site, and requires lesser amount of medication, but is has a limited utility in multilevel disc protrusion and requires a greater level of skill on part of the interventionist. The transforaminal approach is most advantageous as medications are delivered closest to the probable source of the irritated nerve root, requires least amount of medication, and this approach results in better ventral epidural spreading than the interlaminar approach, but requires a skilled radiologist or an anesthetist besides the use of fluoroscopy or a CT scan.21, 28, 29, 30
There are many studies evaluating role of lumbar epidural steroid injections (LESI) either by transforaminal route or by caudal route in the management of low back pain resulting from various causes.21, 30, 31, 32, 33, 34, 35. But there are only few studies comparing results of caudal epidural steroid injection and SNRB in management of lumbar PIVD21, 36, 37; however, there is only one study where both the procedures for PIVD have been reviewed for its technical ease and results.38
In the present study, the initial pain score (VAS) was 7.65 ± 0.5 in SNRB group, which reduced to 4.07 ± 0.9 at one-year follow-up. The reduction in pain score was 57.5% at 1 month, 55.5% at 3 months, and 52.9% at 6 months (Table 2). Even though the pain had increased at 1-year follow-up (46.8%) from that compared to 6-month follow-up period (52.9%), the reduction in pain scores was statistically significant (p = 0.001) at all follow-ups. In caudal group, initial VAS score was 7.42 ± 0.6, which had reduced to 61.0% at 1 month, 61.5% at 3 months, 59.6% at 6 months, and 58.2% at 1-year follow-up stage. Here also, the reduction in pain was more than 50% and was statistically significant (p = 0.001) till 1-year follow-up period. When we compare the results in both groups in terms of pain relief (VAS), the relief was more in caudal group at 3 months (short-term), 6 months (midterm), and one-year (long-term) follow-up, indicating better response than SNRB group.
The initial ODI in SNRB group was 78.20 ± 2.8, which reduced to 41.70 ± 5.5 at 1-year period. This showed improvement of 52.8% at 1-month and 3-month periods, 48.6% at 6 months, and 46.7% at 1-year period (Table 2). While in caudal group, the improvement was 59.6% at 1 month, 64.6% at 3 months, 65.1% at 6 months, and 65.4% at 1-year period. There was a steady decrease in ODI values in all follow-up periods in caudal group, which remained statistically significant at 1-year follow-up period (Table 3). This was not seen in SNRB group. In both, SNRB and caudal group, there was a decrease in ODI of more than 40%, which is considered significant in terms of reduction of disability. Also, the change in ODI in both groups was statistically significant at all follow-up periods (Table 3). On comparing the data of ODI, the decrease was more in caudal group (27.00 ± 14.1) than SNRB group (41.70 ± 5.5), suggesting that the decrease in disability was more in caudal group at 3 months (short-term), 6 months (midterm), and one-year (long-term) follow-up. Moreover, the decrease in disability index continued at all follow-up periods even till 1-year follow-up (Table 2).
Table 3.
Showing the differences of VAS and ODI at follow-up and their significance in both groups.
| Difference between | VAS |
ODI |
||
|---|---|---|---|---|
| SNRB Mean ± SD (p value) |
Caudal Mean ± SD (p value) |
SNRB Mean ± SD (p value) |
Caudal Mean ± SD (p value) |
|
| Initial-1 month | 4.43 ± 0.7 (0.001) | 4.57 ± 0.8 (0.001) | 41.30 ± 7.7 (0.001) | 46.60 ± 08.2 (0.001) |
| Initial-3 months | 4.25 ± 0.8 (0.001) | 4.42 ± 1.2 (0.001) | 38.65 ± 5.9 (0.001) | 50.55 ± 11.7 (0.001) |
| Initial-6 months | 4.05 ± 0.9 (0.001) | 4.50 ± 1.4 (0.001) | 38.00 ± 5.8 (0.001) | 50.95 ± 13.9 (0.001) |
| Initial-1 year | 3.58 ± 1.1 (0.001) | 4.33 ± 1.5 (0.001) | 36.50 ± 6.3 (0.001) | 51.15 ± 03.9 (0.001) |
The procedure did not show a positive response in one case (L1–2). In this case, though the beneficial effect was seen, the relief of pain was only 40% and improvement in ODI score did not reach up to cut-off criteria (>40% reduction) to be labeled as positive response. This may be because the level of pathology was much higher and the effect of drug was not as good as that at lower level. There were 4 cases labeled as nonresponders in SNRB group. These cases had disc herniation at L5–S1 level. Giving a successful nerve root block for S1 is technically more demanding and requires to be done under CT scan imaging. We had not used CT scan imaging in our study for any procedure.
The results of caudal epidural group in this study were comparable to the results of various similar studies available in literature in terms of VAS (reduction of pain by 58.2% at end of year) and ODI (decrease in disability index by 65.4% at the end of one year). Kumar et al. in their study showed similar results while treating PIVD cases by caudal epidural injection.32 Similar results were also seen by Manchikanti et al. (2008), who reported significant pain relief (≥50%) in 79–81% of the patients with significant improvement in functional status (40% or greater reduction in Oswestry scores) in 83–91% of the patients at the end of one-year follow-up.39 Sayegh et al. also observed the same results as they compared the results of caudal epidural injections with and without steroid in cases of low backache and sciatica in long-term follow-up.34
Karppinen et al. (2001) observed that periradicular infiltration of corticosteroids for sciatica produces a short-term benefit in terms of improvement in leg pain.40
6. Conclusions
Our study has shown that caudal epidural block is an easy and safe method with better short-term, midterm, and long-term pain relief and improvement in functional disability than selective nerve root block in cases of lumbar intervertebral disc herniation and can be given by an orthopedic surgeon. Selective nerve root block injection is technically more demanding and has to be given by a trained physician.
Conflicts of interest
The authors have none to declare.
References
- 1.Price C., Arden N., Coglan L., Rogers P. Cost-effectiveness and safety of epidural steroids in the management of sciatica. Health Technol Assess. 2005;9:1–58. doi: 10.3310/hta9330. [DOI] [PubMed] [Google Scholar]
- 2.Waddell G. 2nd ed. Churchill Livingstone; 2004. The Back Pain Revolution. [Google Scholar]
- 3.Fairbank J.C. Sciatic: an archaic term. Br Med J. 2007;335:112. doi: 10.1136/bmj.39275.951343.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koes B.W., van Tulder M.W., Peul W.C. Diagnosis and treatment of sciatica. Br Med J. 2007;334:1313–1317. doi: 10.1136/bmj.39223.428495.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heliovaara M., Impivaara O., Sievers K. Lumbar disc syndrome in Finland. J Epidemiol Community Health. 1987;41:251–258. doi: 10.1136/jech.41.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Konstantinou K., Dunn K.M. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976) 2008;33:2464–2472. doi: 10.1097/BRS.0b013e318183a4a2. [DOI] [PubMed] [Google Scholar]
- 7.Karppinen J., Ohinmaa A., Malmivaara A. Cost effectiveness of periradicular infiltration for sciatica: subgroup analysis of a randomized controlled trial. Spine (Phila Pa 1976) 2001;26:2587–2595. doi: 10.1097/00007632-200112010-00013. [DOI] [PubMed] [Google Scholar]
- 8.Vad V.B., Bhat A.L., Lutz G.E., Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976) 2002;27:11–16. doi: 10.1097/00007632-200201010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Bush K., Cowan N., Katz D.E., Gishen P. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow-up. Spine (Phila Pa 1976) 1992;17:1205–1212. doi: 10.1097/00007632-199210000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Weber H., Holme I., Amlie E. The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. Spine (Phila Pa 1976) 1993;18:1433–1438. [PubMed] [Google Scholar]
- 11.Goebert H.W., Jr., Jallo S.J., Gardner W.J., Wasmuth C.E. Painful radiculopathy treated with epidural injections of procaine and hydrocortisone acetate: results in 113 patients. Anesth Analg. 1961;40:30–34. [PubMed] [Google Scholar]
- 12.Rydevik B., Brown M.D., Lundborg G. Pathoanatomy and pathophysiology of nerve root compression. Spine (Phila Pa 1976) 1984;9:7–15. doi: 10.1097/00007632-198401000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Goupille P., Jayson M.I., Valat J.P., Freemont A.J. The role of inflammation in disk herniation-associated radiculopathy. Semin Arthritis Rheum. 1998;28:60–71. doi: 10.1016/s0049-0172(98)80029-2. [DOI] [PubMed] [Google Scholar]
- 14.Autio R.A., Karppinen J., Kurunlahti M., Haapea M., Vanharanta H., Tervonen O. Effect of periradicular methylprednisolone on spontaneous resorption of intervertebral disc herniations. Spine (Phila Pa 1976) 2004;29:1601–1607. doi: 10.1097/01.brs.0000132511.46818.67. [DOI] [PubMed] [Google Scholar]
- 15.Muramoto T., Atsuta Y., Iwahara T., Sato M., Takemitsu Y. The action of prostaglandin E2 and triamcinolone acetonide on the firing activity of lumbar nerve roots. Int Orthop. 1997;21:172–175. doi: 10.1007/s002640050144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nygaard O.P., Mellgren S.I., Osterud B. The inflammatory properties of contained and non-contained lumbar disc herniation. Spine (Phila Pa 1976) 1997;22:2484–2488. doi: 10.1097/00007632-199711010-00004. [DOI] [PubMed] [Google Scholar]
- 17.Slipman C.W., Lipetz J.S., Jackson H.B., Rogers D.P., Vresilovic E.J. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000;81:741–746. doi: 10.1016/s0003-9993(00)90104-7. [DOI] [PubMed] [Google Scholar]
- 18.Ng L., Chaudhary N., Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain: a randomized, double-blind, controlled trial. Spine (Phila Pa 1976) 2005;30:857–862. doi: 10.1097/01.brs.0000158878.93445.a0. [DOI] [PubMed] [Google Scholar]
- 19.Quraishi N.A. Transforaminal injection of corticosteroids for lumbar radiculopathy: systematic review and meta-analysis. Eur Spine J. 2012;21(February (2)):214–219. doi: 10.1007/s00586-011-2008-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manchikanti L., Cash K.A., Pampati V., Falco F.J. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active-control trial. Pain Phys. 2014;17:E489–E501. [PubMed] [Google Scholar]
- 21.Manchikanti L., Singh V., Pampati V., Falco F.J., Hirsch J.A. Comparison of the efficacy of caudal, interlaminar, and transforaminal epidural injections in managing lumbar disc herniation: is one method superior to the other? Korean J Pain. 2015;28(January (1)):11–21. doi: 10.3344/kjp.2015.28.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kang S.S., Hwang B.M., Son H.J. The dosage of corticosteroid in transforaminal epidural steroid injections for lumbar radicular pain due to a herniated disc. Pain Phys. 2011;14(July–August (4)):361–370. [PubMed] [Google Scholar]
- 23.McCahon R.A., Ravenscroft A., Hodgkinson V., Evley R., Hardman J. A pilot study of the dose–response of caudal methylprednisolone with levobupivacaine in chronic lower back pain. Anaesthesia. 2011;66:595–603. doi: 10.1111/j.1365-2044.2011.06764.x. [DOI] [PubMed] [Google Scholar]
- 24.Manchikanti L., Singh V., Kloth D. Interventional techniques in the management of chronic pain: Part 2.0. Pain Phys. 2001;4:24–96. [PubMed] [Google Scholar]
- 25.Andreisek G., Jenni M., Klingler D. Access routes and reported decision criteria for lumbar epidural drug injections: a systematic literature review. Skeletal Radiol. 2013;42(December (12)):1683–1692. doi: 10.1007/s00256-013-1713-5. [DOI] [PubMed] [Google Scholar]
- 26.Conn A., Buenaventura R.M., Datta S., Abdi S., Diwan S. Systematic review of caudal epidural injections in the management of chronic low back pain. Pain Phys. 2009;12:109–135. [PubMed] [Google Scholar]
- 27.Manchikanti L., Boswell M.V., Singh V. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Phys. 2009;12(July–August (4)):699–802. [PubMed] [Google Scholar]
- 28.Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Phys. 2000;3:374–398. [PubMed] [Google Scholar]
- 29.Boswell M.V., Hansen H.C., Trescot A.M., Hirsch J.A. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Phys. 2003;6:319–334. [PubMed] [Google Scholar]
- 30.Parr A.T., Manchikanti L., Hameed H. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Phys. 2012;15(May–June (3)):E159–E198. [PubMed] [Google Scholar]
- 31.Manchikanti L., Singh V., Cash K.A., Pampati V., Damron K.S., Boswell M.V. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: a randomized, controlled, double blind trial with a two-year follow-up. Pain Phys. 2012;15(July–August (4)):273–286. [PubMed] [Google Scholar]
- 32.Manchikanti L., Pampati V., Benyamin R.M., Boswell M.V. Analysis of efficacy differences between caudal and lumbar interlaminar epidural injections in chronic lumbar axial discogenic pain: local anesthetic alone vs. local combined with steroids. Int J Med Sci. 2015;12(3):214–222. doi: 10.7150/ijms.10870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumar S., Verma R., Singh S. Is it worth to give steroid in caudal epidural injections? A prospective randomized controlled study. Sci J Med Sci. 2014;3(7):331–336. [Google Scholar]
- 34.Sayegh F.E., Kenanidis E.I., Papavasiliou K.A. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: a prospective, randomized, double-blind clinical trial. Spine. 2009;34:1441–1447. doi: 10.1097/BRS.0b013e3181a4804a. [DOI] [PubMed] [Google Scholar]
- 35.Singh H., Kaur M., Nagpal S., Gupta S. Role of caudal epidural steroid injections in lumbar disc prolapse. J Indian Med Assoc. 2010;108(May (5)):287–288. 290–91. [PubMed] [Google Scholar]
- 36.Mendoza-Lattes S., Weiss A., Found E., Zimmerman B., Gao Y. Comparable effectiveness of caudal vs. transforaminal epidural steroid injections. Iowa Orthop J. 2009;29:91–96. [PMC free article] [PubMed] [Google Scholar]
- 37.Ploumis A., Christodoulou P., Wood K.B., Varvarousis D., Sarni J.L., Beris A. Caudal vs transforaminal epidural steroid injections as short-term (6 months) pain relief in lumbar spinal stenosis patients with sciatica. Pain Med. 2014;15(March (3)):379–385. doi: 10.1111/pme.12318. [DOI] [PubMed] [Google Scholar]
- 38.Eckel T.S., Bartynski W.S. Epidural steroid injections and selective nerve root blocks. Tech Vasc Interv Radiol. 2009;12(March (1)):11–21. doi: 10.1053/j.tvir.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 39.Manchikanti L., Singh V., Cash K.A., Pampati V., Damron K.S., Boswell M.V. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 2—Disc herniation and radiculitis. Pain Phys. 2008;11:801–815. [PubMed] [Google Scholar]
- 40.Karppinen J., Malmivaara A., Kurunlahti M. Periradicular infiltration for sciatica: a randomized controlled trial. Spine. 2001;26:1059–1067. doi: 10.1097/00007632-200105010-00015. [DOI] [PubMed] [Google Scholar]