Abstract
Diffuse idiopathic skeletal hyperostosis (DISH) is a systemic non-inflammatory disease of an unknown aetiology. It is characterized by ossification of the enthesis and may significantly affect the quality of life of the affected individuals. Despite the fact that this disease was first described more than 60 years ago and is a relatively common condition in the society, its awareness among clinician is still limited. An awareness of this entity and its mimicking conditions is essential so as to reach to an early diagnosis and avoid unnecessary investigations and treatment.
Keywords: Spine, Hyperostosis, Longitudinal ligament, Pain, Stiffness, Dysphagia
1. Introduction
Diffuse idiopathic skeletal hyperostosis (DISH) is a progressive non-inflammatory bone and entheses disease which reduces the quality of life and self sufficiency of patients.1 Despite significant prevalence, the awareness of this disease is low, and this often leads to misdiagnosis. The hallmark of this disease is the ossification of the ligaments and entheses in the prevertebral and prediscal regions of the spine.2 The hyperostotic calcification typically affects the anterolateral ligaments of the thoracic vertebrae. However, the cervical and lumbar vertebrae may also be affected. The diagnosis of DISH requires the radiological presence of free flowing ossification (like a flowing candle wax) of the anterior longitudinal ligaments of the spine over at least four consecutive levels.3 Peripheral involvement is not uncommon, but it is hard to ascribe to DISH in the absence of typical spinal changes.
The aetiology of DISH is unknown, but several authors have demonstrated its association with diabetes mellitus and advanced age.4, 5 Studies conducted in different population settings have shown that the incidence of DISH varies from 2.9% in an Asian population to between 15% and 25% in the Caucasian population.6, 7 With the demonstration of the close association between DISH and factors such as increased life expectancy, type 2 diabetes mellitus, and obesity which are attributes of modern affluent societies, the incidence of this condition is only expected to rise in the coming decades.8, 9
When symptoms occur in DISH, they are usually mild and evolve slowly over time. The symptoms may be in form of one or a combination of the following:
-
1.
Thoracic, lumbar and/or cervical pain
-
2.
Spinal stiffness
-
3.
Radiculopathy
-
4.
Polyarticular pain
-
5.
Monoarticular synovitis
More severe symptoms can also occur in the form of dysphagia, airway obstruction and increased risk of fractures of the spine.10, 11, 12 Many individuals with this condition may, however, be entirely asymptomatic, with ossification on imaging being an incidental finding.14, 15
The treatment of DISH is symptomatic and empirical. Surgery is indicated only when conservative measures fail in the patients that present with severe symptoms of dysphagia, airway obstruction and fractures.16, 17
2. Discussion
2.1. History and diagnostic criteria
DISH, also known as Forestier's disease was first described by Jacques Forestier and his student Juane Rotes-Querol in 1950 under the name ‘senile ankylosing vertebral hyperostosis.’18 It was later discovered that the disease also occurs in younger individuals, the name was then changed to ankylosing spinal hyperostosis (ASH).3 Further work by other researchers revealed that the disease affects other structures outside the axial skeleton. This resulted in another change in terminology to diffuse idiopathic skeletal hyperostosis (DISH) by Resnick and Niwayama following their work in 1976.19 It is the currently used terminology for the condition which specifically affects the enthesis. Enthesis is a part of the skeletatal system which is rich in collagen fibres, fibroblasts, other mesenchymal cells, fibrocartilage, and calcified matrix. It penetrates the bone cortex at its attachment.
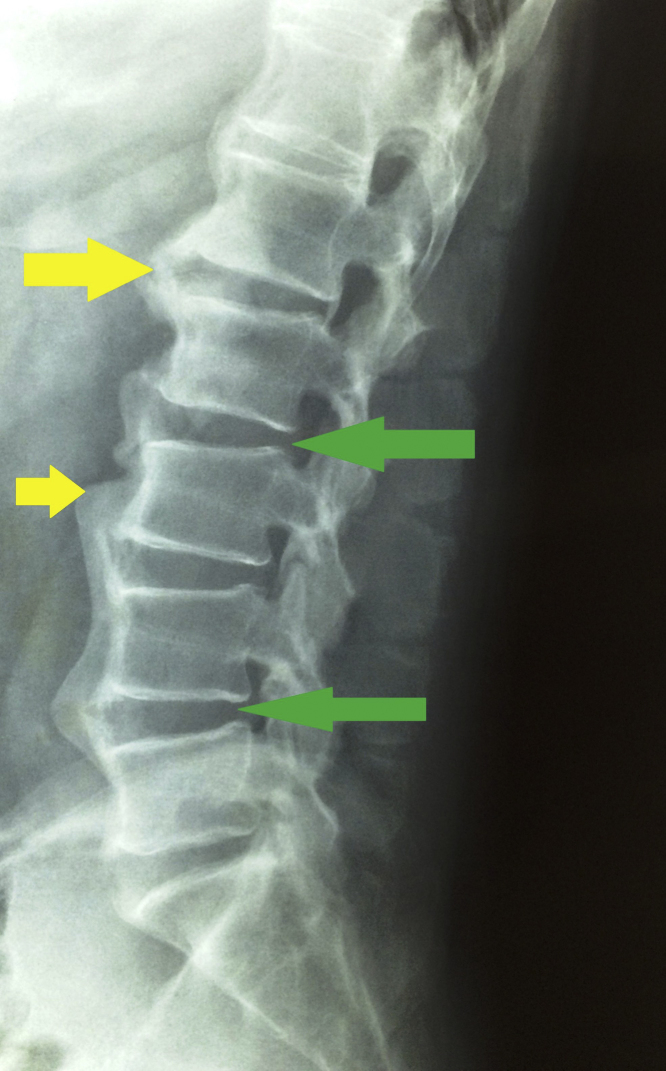
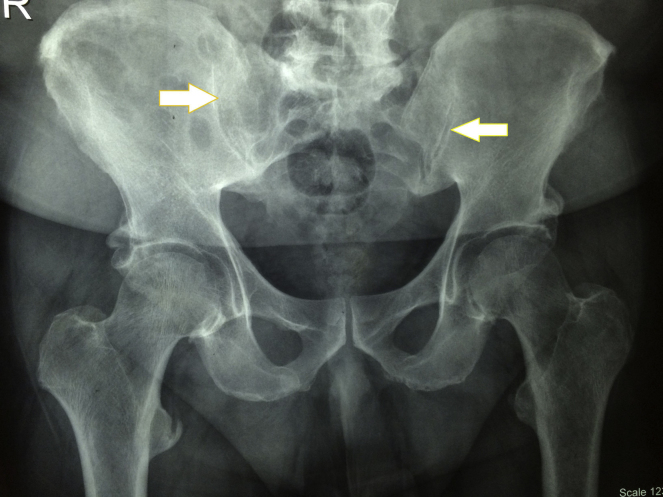
Various authors use different definitions for the diagnosis of DISH. These range from hyperostosis linking two vertebral bodies, without intervening disc disease and extend to different numbers of vertebrae connected by confluent anterior longitudinal ligament related new bone. The commonest criteria were that described by Resnick and Niwayama. The criteria are as follows19 (Fig. 1, Fig. 2):
-
1.
Flowing ossification of the anterior longitudinal ligament over four adjoining vertebrae (in the thoracic region).
-
2.
The sparing of the intervertebral disc spaces by the ossification.
-
3.
Non involvement of the apophyseal and sacroiliac joints by features of inflammation.
Fig. 1.
Lateral radiograph of the lumbo-sacral spine depicting the calcification (flowing ossification) of the anterior longitudinal ligament (yellow arrows). The relative sparing of the inter-vertebral disc is also seen (green arrows).
Fig. 2.
Antero-posterior radiograph of the pelvis depicting the sparing of the sacro-iliac joints (white arrows).
Julken et al. based their criteria on the presence of bridging ossification connecting the bodies of two adjoining vertebrae in the thoracic region.20 The other features of their criteria are similar to those of Resnick and Niwayama. Each of these two sets of criteria, however, failed to take into consideration the presence of peripheral manifestations in DISH. This problem was resolved by Utsinger et al. following their work in 2014.21 Their criteria reduced the spinal affectation to the presence of flowing ossification over three adjoining vertebral bodies and then the presence of peripheral enthesopathies. The different criteria used are summarized in Table 1.22
Table 1.
Criteria for definition of diffuse idiopathic skeletal hyperostosis.
| Authors | Criteria |
|---|---|
| Bywaters23 | Bridging of vertebral bodies with normal intervening disc space. |
| Julkunen20 | Presence of two hyperostotic bridges on lateral X-ray of the spine. |
| Harris24 | Presence of hypertrophic bony spurs with at least two bony bridges. No sacro-iliac joint ankylosis nor erosion. |
| Resnick and Niwayama19 | 1. Flowing ossification involving four contiguous vertebrae. |
| 2. Normal intervertebral disc. | |
| 3. Absence of facet joint anakylosis. | |
| 4. Absence of sacroiliac inflammatory changes. | |
| Arlet and MaziÉres25 | 1. Bridging ossification of three adjoining vertebrae in the thoracic region. |
| 2. Absence or minimal intervening disc disease. | |
| 3. No facet joint ankylosis. | |
| 4. Absence of sacro-iliac joints erosion or ossification. | |
| Utsinger21 | 1. Flowing ossification of four contiguous vertebral bodies. |
| 2. Minimal or no intervertebral joint disease. | |
| 3. Absence facet joint ankylosis. | |
| Rogers and Waldron26 | 1. Flowing ossification over three contiguous vertebrae. |
| 2. Evidence of features of extra-spinal DISH. | |
| 3. Absence of changes in the intervertebral disc space not required for diagnosis. | |
| Mata et al.27 | 1. Flowing ossification over four contiguous vertebrae. |
| 2. Presence of peripheral enthesopathies. | |
| CrubÉzy28 | Presence of bridging ossification over two intervertebral disc spaces in the thoracic region. |
| Presence of disc disease or sacroiliac joint fusion does not rule out the disease in elderly patients. |
Mata et al. in 1998, proposed an objective method of scoring the manifestations of DISH.29 This method is easily reproducible and utilizes the criteria described by Resnick and Niwayama. It scores the affected individuals by classifying each affected vertebra numerically depending on the extent of ossification. It also takes into consideration whether the bridging over the disc space is complete or partial.
2.2. Incidence of dish
Different studies give varying prevailing rates for DISH. It is mainly due to the lack of consensus on the exact definition of the condition. However, there has been some works that tried to estimate its prevalence based on uniform criteria as defined by Resnick et al.19 Cassin et al. in the 1990s estimated the incidence of more than 10%,in patients over 70 years of age.31 In another study, Holton et al. looked at 298 men above the age of 65 years and observed a prevalence of 42% which appeared to increase with age.14 Wienfield et al. in the analysis of data from hospital based populations in America concluded that the prevalence of DISH in patients above the age of 50 years was 25% for males and 15% for females. They observed an increase in prevalence at 70 years by 35% in men and 25% in females, respectively.32 These three studies were based on X-ray findings. More recently, Atsuhiko et al. conducted a study based on CT-scan findings and got a prevalence of 39% in males, and 14% of females.33 This is considerably higher than the figures obtained by other authors in the Asian population. The authors hypothesized that this considerable variation could be attributed to the incomplete diagnosis of DISH based on X-ray alone. Hence, reconstructed CT was adopted for the detailed evaluation conducted in the study. Table 2 33 gives a summary of the work done by various authors on the prevalence of DISH. From the preceding, it can be concluded that the condition is commoner in males than females and that the prevalence tends to increase with age. It mainly affects individuals over the age of 40 years. It is also commoner in Caucasians than in Africans and Asians.
Table 2.
Prevalence of DISH by different authors.
| Author | Race | Year | Age range | % age (male/female) |
|---|---|---|---|---|
| Resnick et al.19 | Caucasians | 1976 | 46–94 | 12/0 |
| Cassim et al.31 | African blacks | 1990 | Over 40 | 3.8/4.2 |
| Wienfeld et al.32 | Mixed race | 1997 | 50–90 | 25/5 |
| Kim et al.34 | Asian | 2004 | 50–99 | 5.4/0.8 |
| Westerveld et al.35 | Western Europe | 2008 | 50–91 | 22.7/12.1 |
| Kagotani et al.36 | Asian | 2014 | 23–94 | 22.0/4.8 |
| Atsuhiko et al.33 | Asian | 2015 | 40–89 | 23/10.9 (with X-ray) 38.7/13.9 (with CT) |
2.3. Aetiopathogenesis
The aetiology of DISH is still not clear. Some factors have however been hypothesized to be of relevance in the pathogenesis of this condition. These are environmental factors, genetic factors, drugs and metabolic factors.
In paleopathogenic studies, the prevalence of DISH in skeletons from cemeteries in churches and chapels, serving priests, monks and lay benefactors, was compared to lay cemeteries in adjacent regions serving the general population.36, 37 The authors found that skeletons deemed to be from high social status individuals had a significantly higher prevalence of DISH when compared to those considered to be of lower social status. The conclusion was that persons of high social status were excessively nourished, with probably increased rates of obesity. The diet of high social status individuals, such as those living in mediaeval monasteries, was high in animal fat and alcohol.36, 38 Mader et al. also found significantly higher waist circumference, in both men and women with DISH.39 The BMI was also statistically higher in both the men and women with DISH compared to the controls in their study, indicating the association with obesity.
Studies have shown that there is an increased incidence of DISH in individuals who have type-2 diabetes mellitus and the presence of abnormal glucose tolerance.40, 41 Some metabolic factors with the ability to stimulate bone formation through the proliferation of osteoblasts, chondrocytes and fibroblasts have also been associated with DISH. These metabolic factors include insulin-like growth factor 1, insulin and growth hormone.42, 43, 44 The exact pathway through which these lead to the new bone formation, especially in the entheseal regions in DISH is still unknown.
The genetic factors associated with DISH include human leucocyte antigen (HLA) and collagen type v alpha 1 (COL5A1). The environmental factors and drugs include fluoride, vitamin A, isotretinon, etretinate, acitretinate, acitretin and other vitamin A derivatives.45, 46 Some studies have also shown anassociation with other risk factors for stroke and a higher risk of developing coronary artery disease.39, 47 Patients with DISH are thus advised to adopt strategies to decrease the risk of these complications.
2.4. Clinical features
The frequency, severity, and nature of complaints among the patients with DISH vary depending on the location of the ossification. Many patients with this condition based on incidental X-ray findings may, however, be free of any form of symptoms.
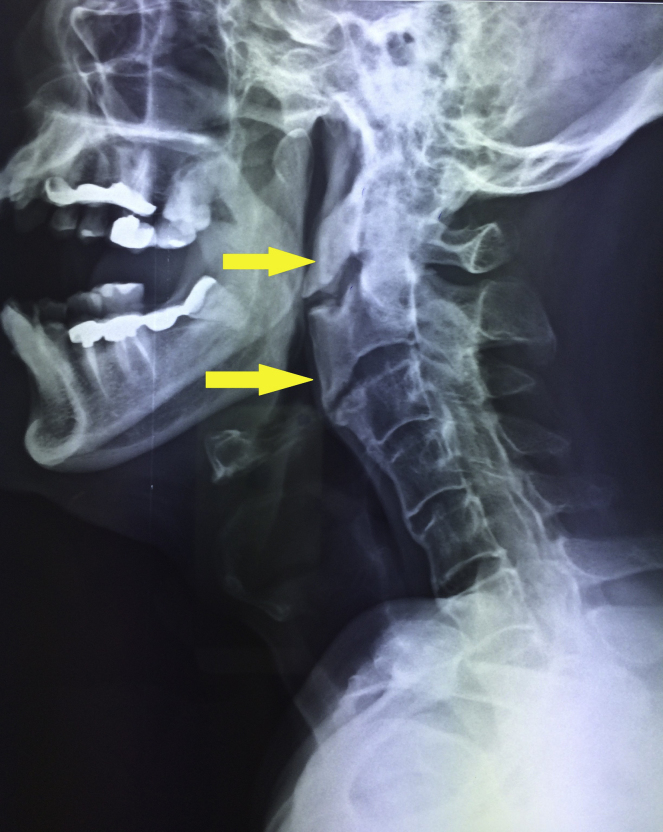
The commonest manifestations of DISH are directly related to the effects on the spine. These include spinal pain, and radicular symptoms like pain, paraesthesia, numbness and weakness in the extremities.48 They can also present with a reduced range of motion in the spine and predisposition to the development of unstable spinal fractures.13, 49 Airway obstruction may occur due to tracheal compression by large osteophytes.16, 50, 51, 52 Dysphagia can also occur typically as a result of a combination of factors. The factors include mass effect by osteophytes (Fig. 3), injury to the recurrent laryngeal nerve, inflammation and fibrosis of the oesophageal wall due irritation by osteophytes.10, 53, 54
Fig. 3.
Lateral radiograph of the cervical spine showing the calcification of the anterior longitudinal ligament with large osteophytes contributing to dysphagia.
The manifestations of DISH are not limited to the spine. Some peripheral locations can also be involved. The features of peripheral involvement include55:
-
1.
It affects joints that are not usually involved in primary osteoarthritis. These include the elbows, wrists, ankles, shoulders, and metacarpophalangeal joints.
-
2.
There is marked level of hypertrophic changes when compared with that seen in joints affected by primary osteoarthritis.
-
3.
There is the presence of major bony excrescences at some sites adjacent to peripheral joints such as the elbow, hips, shoulders, knees and ankles.
-
4.
The presence of extra-articular calcification and ossification. The affected sites are the tibia tubercles, the calcaneus, patella and the olecranon process of the ulna.
These factors are responsible for the joint stiffness and pain that may be associated with DISH.
DISH can also present with some other features which include oesophageal reflux disease, odynophagia, aphonia, dysphonia, aspiration pneumonia, and difficulty with endotracheal intubation.56
2.5. Differential diagnosis
Some conditions may mimic DISH based on the presence of bony excrescences similar to those seen in the condition (Table 3). Spondylosis deformans and Ankylosing spondylitis are however the two conditions that are most similar to DISH. Spondylosis deformans is the commoner of the two. It can be differentiated from DISH based on the fact that it spares the anterior longitudinal ligament of the spine. Ankylosing spondylitis, on the other hand, is a relatively rare condition with an incidence of 0.05–1.4% as against DISH that has an incidence of 2.9–25% of the population.13, 30 This condition is a chronic inflammatory rheumatoid disorder that characteristically affects young Caucasian males.13, 30 In AS, the patients, usually have symptoms and also present with associated conditions like ulcerative colitis, iritis, oruveitis. Pathologically, there is the presence of sacroiliac and apophyseal joint fusion or sclerosis and sacroiliac joint inflammation.30 The earliest symptoms of these include back pain and stiffness. The inflammation progressively involves the intervertebral joints, leading to spondylitis, as well as the large peripheral joints including the knees, the hips, and the shoulders. The patient in very severe cases may after many years develop characteristic postural abnormalities like “Bechterew scoop”. The cause of AS is attributed to a combination of environmental and genetic factors which are still unknown. Research has however revealed the influence of several genes in the development of the disorder. The implicated genes include HLA-B27, ERAP1, IL1A, and IL23R.30
Table 3.
Differences between DISH and AS.
| Diffuse Idiopathic Skeletal Hyperostosis (DISH) | Ankylosing Spondylitis (AS) | |
|---|---|---|
| Aetiology | Idiopathic | Autoimmune |
| Incidence | 2.9–25.0% | 0.05–1.4% |
| Age of onset | >45 years | <30 years |
| Sex ratio {M/F} | 2:1 | 3:1 |
| Clinical features | Pain, radiculopathy, dysphagia, risk of spinal and peripheral fractures | Pain, spinal stiffness, characteristic postural abnormalities, involvement of large peripheral joints |
| Radiological features | Affects anterior longitudinal ligaments of the spine, spares intervertebral discs and SI joints | Intervertebral joint fusion, especially the SI joints |
| Laboratory investigations | Non-specific and inconclusive | High ESR and CRP Presence of HLA-B27 (in most cases) |
| Associated diseases | Obesity, diabetes mellitus, Hypervitaminosis A | Autoimmune conditions like iritis, uveitis, ulcerative colitis |
| Treatment | Symptomatic | Disease modifying drugs, non-steroidal anti-inflammatory drugs, surgery (occasionally) |
Table 4 summarizes the differences between DISH and AS.
Table 4.
Differential diagnosis of DISH.
| • Ankylosing Spondylitis |
| • Spondylosis deformans |
| • Degenerative spinal |
| • Disease |
| • Melorheostosis |
| • Fluorosis |
| • Osteomalacia |
| • Acromegaly |
| • Hypervitaminosis A |
| • Retinoids |
| • Pachydermoperiostosis |
| • Hypophosphatemia |
| • Hypoparathyroidism |
2.6. Treatment
The treatment of DISH is mostly symptomatic and empirical. The measures adopted include physiotherapy, analgesics, anti-inflammatory drugs, muscle relaxants, sedation, physical therapy and management of associated metabolic disorders.16 Surgery is usually required when conservative measures fail in patients with severe conditions like airway obstruction, dysphagia, and fractures.17, 52, 57
3. Conclusion
DISH was first described more than six decades ago but despite this, its awareness is still limited among clinicians. This may result in misdiagnosis, unnecessary investigations, and treatment. It is thus imperative to have this condition at the back of the mind when assessing patients that present with musculoskeletal pain. Future studies in this condition should focus on unravelling the causes of DISH so as to develop possible preventive and therapeutic measures.
Conflicts of interest
The authors have none to declare.
References
- 1.Belanger T.A., Rowe D.E. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. J Am Acad Orthop Surg. 2001;9:258–267. doi: 10.5435/00124635-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Resnick D., Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH) Radiology. 1976;119(June (3)):559–568. doi: 10.1148/119.3.559. [DOI] [PubMed] [Google Scholar]
- 3.Forestier J., Lagier R. Ankylosing hyperostosis of the spine. Clin Orthop Relat Res. 1971;74:65–81. [PubMed] [Google Scholar]
- 4.Denko C.W., Malemud C.J. Body mass index and blood glucose: correlations with serum insulin, growth hormone, and insulin-like growth factor-1 levels in patients with diffuse idiopathic skeletal hyperostosis (DISH) Rheumatol Int. 2006;26:292–329. doi: 10.1007/s00296-005-0588-8. [DOI] [PubMed] [Google Scholar]
- 5.Kiss C., Szilagyi M., Paksy A. Risk factors for diffuse idiopathic skeletal hyperostosis: a case–control study. Rheumatology (Oxford) 2002;41:27–30. doi: 10.1093/rheumatology/41.1.27. [DOI] [PubMed] [Google Scholar]
- 6.Kim S.K., Choi B.R., Kim C.G. The prevalence of diffuse idiopathic skeletal hyperostosis in Korea. J Rheumatol. 2004;31:2032–2035. [PubMed] [Google Scholar]
- 7.Weinfeld R.M., Olson P.N., Maki D.D. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Skelet Radiol. 1997;26:222–225. doi: 10.1007/s002560050225. [DOI] [PubMed] [Google Scholar]
- 8.Smyth S., Heron A. Diabetes and obesity: the twin epidemics. Nat Med. 2006;12:75–80. doi: 10.1038/nm0106-75. [DOI] [PubMed] [Google Scholar]
- 9.Organization World Health Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]
- 10.Mader R. Clinical manifestations of diffuse idiopathic skeletal hyperostosis of the cervical spine. Semin Arthritis Rheum. 2002;32:130–135. doi: 10.1053/sarh.2002.33726. [DOI] [PubMed] [Google Scholar]
- 11.Pascal-Moussellard H., Drossard G., Cursolles J.C. Myelopathy by lesions of the craniocervical junction in a patient with forestier disease. Spine. 2006;31:E557–E560. doi: 10.1097/01.brs.0000225972.24608.be. [DOI] [PubMed] [Google Scholar]
- 12.Stechison M.T., Tator C.H. Cervical myelopathy in diffuse idiopathic skeletal hyperostosis. Case report. J Neurosurg. 1990;73:279–282. doi: 10.3171/jns.1990.73.2.0279. [DOI] [PubMed] [Google Scholar]
- 13.Westerveld L.A., Verlaan J.J., Oner F.C. Spinal fractures in patients with ankylosing spinal disorders. A systematic review of the literature on treatment, neurological status and complications. EUR Spine J. 2009;18:145–156. doi: 10.1007/s00586-008-0764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holton K.F., Denard P.J., Yoo J.U. Diffuse idiopathic skeletal hyperostosis (DISH) and its relation to back pain among older men: the MrOS study. Semin Arthitis Rheum. 2011;41(October (2)):131–138. doi: 10.1016/j.semarthrit.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlapbach P., Beyeler C., Gerber N.J. Diffuse idiopathic skeletal hyperostosis (DISH) of the spine: a cause of back pain? A controlled study. Br J Rheumatol. 1989;28(August (4)):299–303. doi: 10.1093/rheumatology/28.4.299. [DOI] [PubMed] [Google Scholar]
- 16.Al-Herz A., Snip J.P., Clark B., Esdaile J.M. Exercise therapy for patients with DISH. Clin Rhuematol. 2008;27:207–210. doi: 10.1007/s10067-007-0693-z. [DOI] [PubMed] [Google Scholar]
- 17.Umerah B.C., Mukherjee B.K., Ibekwe O. Cervical spondylosis and dysphagia. J Laryngol Otol. 1991;95:1179–1184. doi: 10.1017/s0022215100092008. [DOI] [PubMed] [Google Scholar]
- 18.Forestier J., Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950;9:321–330. doi: 10.1136/ard.9.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Resnick D., Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH) Radiology. 1976;119:559–568. doi: 10.1148/119.3.559. [DOI] [PubMed] [Google Scholar]
- 20.Julkunen H., Heinonen O.P., Knekt P., Maatela J. The epidemiology of hyperostosis of the spine together with its symptoms and related mortality in a general population. Scand J Rheumatol. 1975;4:23–27. [PubMed] [Google Scholar]
- 21.Utsinger P.D., Resnick D., Shapiro R. Diffuse skeletal abnormalities in Forestier disease. Arch Intern Med. 1976;136:763–768. [PubMed] [Google Scholar]
- 22.Pillai S., Littlejohn G. Metabolic factors in diffuse idiopathic skeletal hyperostosis – a review of clinical data. Open Rheumatol J. 2014;8:116–128. doi: 10.2174/1874312901408010116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bywaters E.G.L., Doyle F.H., Oakley N. Senile hyperostotic ankylosing spondylosis (Forestier and Querol) in diabetes mellitus. Arthritis Rheum. 1966;9:495. [Google Scholar]
- 24.Harris J., Carter A.R., Glick E.N., Storey G.O. Ankylosing hyperostosis. I. Clinical and radiological features. Ann Rheum Dis. 1974;33:210–215. doi: 10.1136/ard.33.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arlet J., Mazieres B. La maladie hyperostique. Rev Med Interne. 1985;5:553–564. doi: 10.1016/s0248-8663(85)80037-0. [DOI] [PubMed] [Google Scholar]
- 26.Rogers J., Waldron T. DISH and the monastic way of life. Int J Osteoarcheol. 2001;11:357–365. [Google Scholar]
- 27.Maat G.J.R., Mastwijk R.W., Van der Velde E.A. Skeletal distribution of degenerative changes in vertebral osteophytosis, vertebral osteoarthritis and DISH. Int J Osteoarchaeol. 1995;5:289–298. [Google Scholar]
- 28.Crubezy E., Crubezy-Ibanez E. Evaluation of diagnostic criteria for hyperostotic diseases on a series of skeletons. Epidemiological implications. Rev Rhum Ed Fr. 1993;60:586–590. [PubMed] [Google Scholar]
- 29.Mata S., Chlem R.K., Fortin P.R., Joseph L., Esdaile J.M. Semin Arthritis Rheum. 1998;28(October (2)):88–96. doi: 10.1016/s0049-0172(98)80041-3. [DOI] [PubMed] [Google Scholar]
- 30.Ghasemi R., Attaya H., Lesha E. Ankylosing spondylitis: a state of the art factual bone. World J Radiol. 2015;28:236–252. doi: 10.4329/wjr.v7.i9.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Casin B., Mody G.M., Rubin D.L. The prevalence of diffuse idiopathic skeletal hyperostosis in African blacks. Br J Rheumatol. 1990;29:131–132. doi: 10.1093/rheumatology/29.2.131. [DOI] [PubMed] [Google Scholar]
- 32.Weinfield R.M., Olson P.N., Maki D.D., Griffiths H.J. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwestern Metropolitan hospital populations. Skelet Radiol. 1997;26:222–225. doi: 10.1007/s002560050225. [DOI] [PubMed] [Google Scholar]
- 33.Hirasawa A., Wakao N., Kamiya M. The prevalence of diffuse idiopathic skeletal hyperostosis in Japan – the first report of measurement by CT and review of the literature. J Orthop Sci. 2016;21(3):287–290. doi: 10.1016/j.jos.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 34.Kim S.K., Choi B.R., Kim C.G. The prevalence of diffuse idiopathic skeletal hyperostosis in Korea. J Rheumatol. 2004;31(10):2032–2035. [PubMed] [Google Scholar]
- 35.Westerveld L.A., van Ufford H.M., Verlaan J.J., Oner F.C. The prevalence of diffuse idiopathic skeletal hyperostosis in an outpatient population in The Netherlands. J Rheumatol. 2008;35(8):1635–1638. [PubMed] [Google Scholar]
- 36.Kagotani R., Yoshida M., Muraki S. Prevalence of diffuse idiopathic skeletal hyperostosis (DISH) of the whole spine and its association with lumbar spondylosis and knee osteoarthritis: the ROAD study. J Bone Min Metab. 2014;33(2):221–229. doi: 10.1007/s00774-014-0583-9. [DOI] [PubMed] [Google Scholar]
- 37.Holgate R.L., Steyn M. Diffuse idiopathic skeletal hyperostosis: diagnostic, clinical, and paleopathological considerations. Clin Anat. 2016;(March) doi: 10.1002/ca.22716. [DOI] [PubMed] [Google Scholar]
- 38.Schneider H.J., Glaesmer H., Klotsche J. Accuracy of anthropometric indicators of obesity to predict cardiovascular risk. J Clin Endocrinol Metab. 2007;92:589–594. doi: 10.1210/jc.2006-0254. [DOI] [PubMed] [Google Scholar]
- 39.Mader R., Novofestovski I., Adawi M., Lavi I. Metabolic syndrome and cardiovascular risk in patients with diffuse idiopathic skeletal hyperostosis. Semin Arthritis Rheum. 2009;38:361–365. doi: 10.1016/j.semarthrit.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 40.Hajkova Z., Streda A., Skrha F. Hyperostotic spondylosis and diabetes mellitus. Ann Rheum Dis. 1965;24:536–543. doi: 10.1136/ard.24.6.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Julkunen H., Karava R., Viljanen V. Hyperostosis of the spine in diabetes mellitus and acromegaly. Diabetologia. 1966;2:123–126. doi: 10.1007/BF00423021. [DOI] [PubMed] [Google Scholar]
- 42.Mader R., Verlaan J.J. Bone exploring factors responsible for bone formation in DISH. Nat Rev Rheumatol. 2012;8:10–12. doi: 10.1038/nrrheum.2011.189. [DOI] [PubMed] [Google Scholar]
- 43.Sarzi-Puttini P., Atzeni F. New developments in our understanding of DISH (diffuse idiopathic skeletal hyperostosis) Curr Opin Rheumatol. 2004;16:287–292. doi: 10.1097/00002281-200405000-00021. [DOI] [PubMed] [Google Scholar]
- 44.Moskowitz R.W., Boja B., Denko C.W. The role of growth factors in degenerative joint disorders. J Rheumatol Suppl. 1991;27:147–148. [PubMed] [Google Scholar]
- 45.DiGiovanna J.J., Helfgott R.K., Gerber L.H., Peck G.L. Extraspinal tendon and ligament calcification associated with long-term therapy with etretinate. N Engl J Med. 1986;315:1177–1182. doi: 10.1056/NEJM198611063151901. [DOI] [PubMed] [Google Scholar]
- 46.Troillet N., Gerster J.C. Forestier disease and metabolism disorders. A prospective controlled study of 25 cases. Rev Rheum Ed Fr. 1993;60:274–279. [PubMed] [Google Scholar]
- 47.Miyazawa N., Akiyama I. Diffuse idiopathic skeletal hyperostosis associated with risk factors for stroke: a case–control study. Spine. 2006;31:E225–E229. doi: 10.1097/01.brs.0000214949.75361.f4. discussion E230. [DOI] [PubMed] [Google Scholar]
- 48.Epstein N.E. Simultaneous cervical diffuse idiopathic skeletal hyperostosis and ossification of the posterior longitudinal ligament resulting in dysphagia or myelopathy in two geriatric North Americans. Surg Neurol. 2000;53:427–431. doi: 10.1016/s0090-3019(00)00227-5. [DOI] [PubMed] [Google Scholar]
- 49.Vengust R., Mihalic R., Turel M. Two different causes of acute respiratory failure in a patient with diffuse idiopathic skeletal hyperostosis and ankylosed cervical spine. Eur Spine J. 2010;19(suppl 2):S130–S134. doi: 10.1007/s00586-009-1159-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Caminos C.B., Cenoz I.Z., Louis C.J., Otano T.B., Esáin B.F., Pérez de Ciriza M.T. Forestier disease: an unusual cause of upper airway obstruction. Am J Emerg Med. 2008;26:1072. doi: 10.1016/j.ajem.2008.03.048. e1–1072.e3. [DOI] [PubMed] [Google Scholar]
- 51.Nelson R.S., Urquhart A.C., Faciszewski T. Diffuse idiopathic skeletal hyperostosis: a rare cause of Dysphagia, airway obstruction, and dysphonia. J Am Coll Surg. 2006;202:938–942. doi: 10.1016/j.jamcollsurg.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 52.Vaishya R., Vijay V., Agarwal A.K. An unusual cause or dysphagia. Apollo Med. 2012;12(4):287–288. [Google Scholar]
- 53.Masiero S., Padoan E., Bazzi M., Ponzoni A. Dysphagia due to diffuse idiopathic skeletal hyperostosis: an analysis of five cases. Rheumatol Int. 2010;30:681–685. doi: 10.1007/s00296-009-0967-7. [DOI] [PubMed] [Google Scholar]
- 54.Carlson M.L., Archibald D.J., Graner D.E., Kasperbauer J.L. Surgical management of dysphagia and airway obstruction in patients with prominent ventral cervical osteophytes. Dysphagia. 2011;26:34–40. doi: 10.1007/s00455-009-9264-6. [DOI] [PubMed] [Google Scholar]
- 55.Mader R., Sarzi-Puttini P., Atzeni F. Extraspinal manifestations of diffuse idiopathic skeletal hyperostosis. Rheumatology (Oxford) 2009;48(December (12)):1478–1481. doi: 10.1093/rheumatology/kep308. [DOI] [PubMed] [Google Scholar]
- 56.Verlaan J.J., Boswijk P.F., de Ru J.A., Dhert W.J., Oner F.C. Diffuse idiopathic skeletal hyperostosis of the cervical spine: an underestimated cause of dysphagia and airway obstruction. Spine J. 2011;11:1058–1067. doi: 10.1016/j.spinee.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 57.Debnath U.K., Vaishya R., Varma H.S. Patella fracture in a patient with Forestier's disease. Acta Orthop Belg. 1992:58–63. [PubMed] [Google Scholar]