Chronic pain is highly prevalent in the United States, affecting nearly one-third of the American population [1,2]. The economic impact of chronic pain is substantial with no clear indication that trends will change [2]. In an effort to combat the chronic pain epidemic, pharmacological approaches and specifically opioid prescription have increased exponentially [3]. Unfortunately, these approaches have been ineffective and include considerable risks including addiction and death [4–7]. Subsequently, non-pharmacological approaches are recommended as a first-line treatment option for individuals experiencing chronic pain [8]. As manual physical therapists, we are well positioned to meet the chronic pain challenge, offering a variety of non-pharmacological treatment options to our patients. Furthermore, our professional organizations are strongly advocating for patients and providers to choose our services over less safe options [9]. For manual physical therapists to play a key role in the management of individuals with chronic pain conditions, simply being a safer option is not good enough. Instead, we must practice in an effective manner as well.
Manual physical therapists can effectively treat patients with chronic pain and other musculoskeletal disorders; however, the field is at a crossroads. The traditional approach to manual therapy assumes that proper technique selection and precise implementation is the primary driver of a successful outcome [10,11]. In this view, the resultant outcomes are directly attributed to the applied intervention. A similar perspective on intervention may be witnessed in traditional medicine when, for example, a pharmaceutical agent is prescribed to manage cholesterol or blood pressure, or a surgical approach is elected based on abnormal imaging findings.
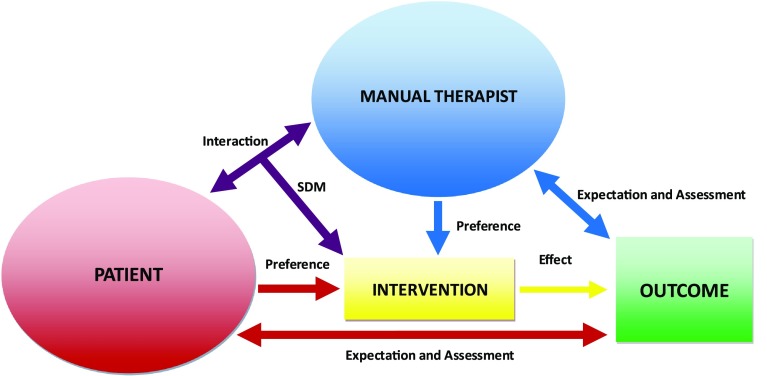
We propose manual physical therapists will only be recognized as ideal providers for individuals with chronic pain if we accept an updated paradigm acknowledging the complexity of the manual physical therapy experience and accept the robustness of varying contextual elements inherent in our interactions. For some clinicians, this will require a revolutionary shift in their perception of the development, maintenance, and modulation of pain [12]. Pain is an experience orchestrated by dynamic sensory, cognitive, and affective processes and is strongly influenced by patient’s expectations, mood, desires, and past experiences. Limiting pain perception to a peripheral impairment is outdated and a more comprehensive, albeit complex, approach to manual therapy accounts for a myriad of interacting factors impacting chronic pain outcomes (Figure 1).
Figure 1.
A comprehensive approach to manual physical therapy effectiveness accounting for interactions between patient, therapist, and intervention factors. Examples of factors include preferences, expectations, outcome assessment, and shared decision-making (SDM).
A comprehensive approach acknowledges the impact of patient and therapist factors, which not only include personal and condition-specific patient characteristics, but also the cultural biases, beliefs, and experiences of both the patient and therapist [13–15]. Additionally, this view acknowledges the interaction between patient and manual physical therapist, which may yield important outcome contributions, either directly (i.e. intervention selection) or indirectly (i.e. modified expectations or mood) [16,17]. Finally, this approach acknowledges the integration of targeted adjunct interventions such as psychosocial strategies and exercise that may (1) enhance the effectiveness of manual therapy for reducing the impact of pain, and/or (2) promote and maintain positive behavioral change [18,19].
This Special Issue of the Journal of Manual and Manipulative Therapy includes a series of manuscripts fitting a comprehensive approach to the utility of manual physical therapy for enhancing chronic pain outcomes. The primary aims of this Special Issue are to advance the understanding of chronic musculoskeletal pain and describe both adjunct interventions as well as elements of the manual physical therapy encounter with the potential to augment the clinical effectiveness. It is our hope this Special Issue will spark discussion towards how we, as manual physical therapists, can meet the growing challenge of effective management for our patients presenting with chronic pain.
The contributing authors of this Special Issue have provided an excellent overview of general pain considerations, adjunct interventions, and components of the manual physical therapy encounter that can enhance clinical effectiveness.
-
•
Maladaptive neuroplastic changes are evident in patients presenting with chronic pain conditions, suggesting intriguing targets for effective treatments. In the first paper, Carol Courtney and colleagues [20] present an overview of chronic pain mechanisms, especially related to alterations in pain sensitivity. Pain sensitivity can serve as a proxy measure for central sensitization – a phenomenon that may impact prognosis and treatment response – and perhaps provide a more effective therapeutic target for treating patients with chronic pain. The authors discuss the potential clinical relevance of pain sensitivity for informing intervention selection within a pain mechanism-based approach.
-
•
Patients with chronic musculoskeletal pain often report co-existing psychosocial complaints known to worsen their prognosis and limit the effectiveness of interventions. Manual therapists are in need of clinical strategies to minimize the influence of negative psychosocial factors and boost positive thinking and outlook. Renee Hill and colleagues [21] follow with a prospective study examining the effects of a specific intervention – mindfulness-based stress reduction (MBSR) – for influencing psychosocial distress. MBSR is an adjunct technique that can be implemented by non-psychologist clinicians within a manual physical therapy approach to enhance outcomes for high risk patients.
-
•
Manual therapy is often a component of a comprehensive treatment package and multiple interventions may interact to influence clinical response. Dominique Mouraux and colleagues [22] present a prospective study combining the principles of mirror visual feedback with a 3D augmented reality system for individuals presenting with chronic upper extremity neuropathic pain. After treatment, significant within and between-session improvements were observed in pain. Intervention such as mirror visual feedback with a 3D augmented reality system may augment manual therapy approaches by desensitizing the person and allowing a window for inclusion of complimentary treatment strategies.
-
•
The traditional clinical decision-making process is one in which the provider is authoritative, while the patient is expected to agree and adhere to the prescribed intervention. Shared decision-making (SDM) describes an interactive process in which the patient and provider work together to determine mutually acceptable treatment approaches. Yannick Tousignant–Laflamme and colleagues [23] conducted a systematic review on the effectiveness of SDM for patients with musculoskeletal pain complaints and found no studies meeting their criteria. The authors discuss the implications of these findings as well as potential limitations of a SDM approach for musculoskeletal pain.
-
•
Placebo is associated with a robust analgesic effect related to expectations. Placebo use is common in clinical practice; however, such practice is of questionable ethical integrity due to the required deception of the patient by the provider. Joel Bialosky and Michael Robinson [24] present a secondary analysis considering changes in mood and attitudes towards healthcare and the provider following disclosure of having received a placebo. Bialosky and Robinson found disclosure of having received a placebo intervention did not result in worsening of mood or attitudes towards healthcare or the provider and particularly if improvements were observed in clinical outcomes. The authors discuss the potential clinical implications of placebo disclosure in their paper.
-
•
Patient education is an important component of a manual physical therapy interaction and the manner and content of education, specifically related to pain, can greatly influence treatment effectiveness. Pain neuroscience education has become increasingly popular and more research is showing clinical benefits of a pain neuroscience approach. Adriaan Louw and colleagues [25] present an overview of a pain neuroscience education framework and discuss how this can be integrated to enhance manual physical therapy effects.
Manual physical therapists should recognize the multidimensional nature of chronic pain as well as the complex interactions of contributing factors accounting for manual therapy-related treatment effects. Continuing to attribute an effective manual physical therapy intervention to the correction of a peripheral impairment is too simplistic and prevents conscious attempts to augment contributing factors known to enhance outcomes in patients with chronic pain. While perhaps a safer avenue than opioids, we believe continuation of an outdated approach to manual physical therapy will result in suboptimal provision of care.
References
- [1].Johannes CB, Le TK, Zhou X, et al. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain. 2010;11(11):1230–1239. 10.1016/j.jpain.2010.07.002 [DOI] [PubMed] [Google Scholar]
- [2].Institute of Medicine (U.S.) Committee on advancing pain research care and education. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington (DC): National Academies Press; 2011. Xvii:p. 364. [PubMed] [Google Scholar]
- [3].Kenan K, Mack K, Paulozzi L. Trends in prescriptions for oxycodone and other commonly used opioids in the united states, 2000–2010. Open Med. 2012;6(2):e41–e47. [PMC free article] [PubMed] [Google Scholar]
- [4].Cicero TJ, Surratt H, Inciardi JA, et al. Relationship between therapeutic use and abuse of opioid analgesics in rural, suburban, and urban locations in the United States. Pharmacoepidemiol Drug Saf. 2007;16(8):827–840. 10.1002/(ISSN)1099-1557 [DOI] [PubMed] [Google Scholar]
- [5].Rudd RA, Aleshire N, Zibbell JE, et al. Increases in drug and opioid overdose deaths – United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50–51):1378–1382. 10.15585/mmwr.mm6450a3 [DOI] [PubMed] [Google Scholar]
- [6].Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–574. 10.1146/annurev-publhealth-031914-122957 [DOI] [PubMed] [Google Scholar]
- [7].Abdel Shaheed C, Maher CG, Williams KA, et al. Efficacy, tolerability, and dose-dependent effects of opioid analgesics for low back pain: a systematic review and meta-analysis. JAMA Intern Med. 2016;176(7):958–968. 10.1001/jamainternmed.2016.1251 [DOI] [PubMed] [Google Scholar]
- [8].Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. 10.15585/mmwr.rr6501e1 [DOI] [PubMed] [Google Scholar]
- [9].American Physical Therapy Association Position paper on opioid abuse and the role of physical therapy. Available from: http://www.Moveforwardpt.Com/choose-physical-therapy-over-opioids-for-pain-management-choosept
- [10].Bialosky JE, Simon CB, Bishop MD, et al. Basis for spinal manipulative therapy: a physical therapist perspective. J Electromyogr Kinesiol. 2012;22(5):643–647. 10.1016/j.jelekin.2011.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Henderson CN. The basis for spinal manipulation: chiropractic perspective of indications and theory. J Electromyogr Kinesiol. 2012;22(5):632–642. 10.1016/j.jelekin.2012.03.008 [DOI] [PubMed] [Google Scholar]
- [12].George SZ. Pain management: roadmap to revolution. American physical therapy association annual conference john h.P. Maley lecture; Nashville, TN; 2016. [Google Scholar]
- [13].Bialosky JE, Bishop MD, Cleland JA. Individual expectation: an overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Phys Ther. 2010;90(9):1345–1355. 10.2522/ptj.20090306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Nijs J, Roussel N, Paul van Wilgen C, et al. Thinking beyond muscles and joints: therapists’ and patients’ attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Man Ther. 2013;18(2):96–102. 10.1016/j.math.2012.11.001 [DOI] [PubMed] [Google Scholar]
- [15].Houben RM, Ostelo RW, Vlaeyen JW, et al. Health care providers’ orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. Eur J Pain. 2005;9(2):173–183. 10.1016/j.ejpain.2004.05.002 [DOI] [PubMed] [Google Scholar]
- [16].Wilson S, Chaloner N, Osborn M, et al. Psychologically informed physiotherapy for chronic pain: patient experiences of treatment and therapeutic process. Physiotherapy. 2016;103(1):98–105. [DOI] [PubMed] [Google Scholar]
- [17].Ferreira PH, Ferreira ML, Maher CG, et al. The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Phys Ther. 2013;93(4):470–478. 10.2522/ptj.20120137 [DOI] [PubMed] [Google Scholar]
- [18].Schabrun SM, Chipchase LS. Priming the brain to learn: the future of therapy? Man Ther. 2012;17(2):184–186. 10.1016/j.math.2011.12.001 [DOI] [PubMed] [Google Scholar]
- [19].Barker KL, Heelas L, Toye F. Introducing acceptance and commitment therapy to a physiotherapy-led pain rehabilitation programme: an Action Research study. Br J Pain. 2016;10(1):22–28. 10.1177/2049463715587117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Courtney CA, Fernandez-de-Las Penas C, Bond S. Mechanisms of chronic pain – key considerations for appropriate physical therapy management. J Man Manip Ther. 2017;25(3):118–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hill RJ, McKernan L, Wang L, et al. Changes in psychosocial well-being after mindfulness-based stress reduction: a prospective cohort study. J Man Manip Ther. 2017;25(3):128–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Mouraux D, Brassinne E, Sobczak S, et al. 3d augmented reality mirror visual feedback therapy applied to the treatment of persistent, unilateral upper extremity neuropathic pain: a preliminary study. J Man Manip Ther. 2017;25(3):137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tousignant-Laflamme Y, Christopher S, Clewley D, et al. Does shared decision making result in better health related outcomes for individuals with painful musculoskeletal disorders? J Man Manip Ther. 2017;25(3):144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bialosky JE, Robinson ME. Placebo disclosure does not result in negative changes in mood or attitudes towards healthcare or the provider. J Man Manip Ther. 2017;25(3):151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Louw A, Puentedura EJ, Nijs J. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017;25(3):160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]