Abstract
Background
porocarcinoma is a rare sort of skin cancer developing from sweat glands. Its clinical course and management are not well understood.
Objectives
the current meta-analysis is to address the presentation and management of porocarcinoma.
Data sources
Web of Science, PubMed, MEDLINE on OVID and Google scholar were searched for English-language studies published before December 1, 2016.
Results
The review of literature revealed 453 cases. From which 222 (49%) cases were male and female were 231 (51%). The mean age was 67.57 years. The mean duration of presentation was 5.57 years ranging from 4 days to 60 years of age. The most common site of affection is the head and neck (39.9%) followed by lower extremity (33.9%). Mass and nodule are the most common modes of presentation. Metastasis occurred at presentation in 110 (31%) cases. The most common organ to which porocarcinoma metastizes is the nearby lymph node (57.7%).
Conclusions
Porocarcinoma is an aggressive skin cancer. Surgery is the main modality of treatment.
Systematic review registration number
reviewregistry233.
Keywords: Porocarcinoma, Presentation, Management, Aggressive, Carcinoma
Highlights
-
•
Porocarcinoma is a rare sort of skin cancer developing from sweat glands.
-
•
Because of rarity of the problem, there is controversy regarding both presentation and management.
-
•
The aim of the current meta-analysis is to summarize all data regarding the disease.
1. Introduction
Porocarcinoma is a rare sort of skin cancer developing from sweat glands, specifically, it is a malignancy of the eccrine sweat glands [1]. Its etiology is not well understood. However, some studies have showed that the tumor developed from a pre-existing eccrine poroma. From others perspective, chronic light exposure, exposure to chemical agents and immunosuppression could be the predisposing factors for de novo eccrine porocarcinoma [2]. Porocarcinoma is a dangerous disease because of high rate of recurrence after resection and metastasis to vital organs [3], [4]. Because of rarity of the problem, there is controversy regarding both presentation and management [5], [6]. Lioyd et al. revealed features like a rapid increase in size, foul odor and fungating fleshy appearance while Kurashige and colleagues who collects 8 cases revealed that all cases of porocarcinoma presented with erosive reddish nodules [6], [7].
Controversy regarding treatment is also present [8]. Kurashige and colleagues who present 8 cases of porocarcinoma summarized that surgical resection should be done in all cases, as adjuvant therapy in form of local irradiation, while Fujimura et al. preferred surgical resection of the mass and giving adjuvant therapy only in special situation [7]. The aim of the current meta-analysis is to summarize all data regarding the presentation and management of cases with prorcarcinoma which was done in line with PRISMA guide line [9].
2. Methodology
Information sources and Search: Web of Science, PubMed, MEDLINE on OVID and Google scholar were searched for English-language studies published before December 1, 2016. The search key words were porocarcinoma, carcinoma of sweat gland and tumor of sweat gland. The data collection was supplemented by references cited by included articles.
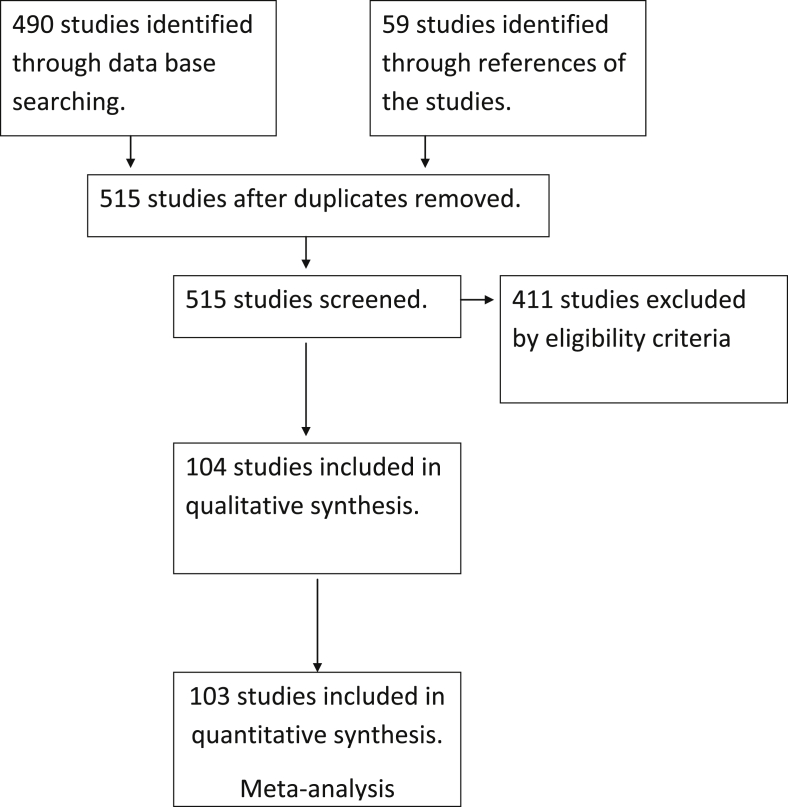
Eligibility criteria: For a study to be included in this meta-analysis, it should address at least one specific aim (clinical course, management, or both) of porocarcinoma (Fig. 1).
Fig. 1.
The process and flow of the literature review.
Data collection process: Data were taken directly from the articles by 4 authors independently. Investigators have not been contacted to obtain and confirm the data.
Data items: Several data were extracted and pooled from all included articles. Those articles were socio-demographic characteristics of the patients, sample size, presentations, duration of presentation, method of diagnosis, options for managements, recurrence rate and complications.
Summary measures and Synthesis of results: Extracted data were calculated and re-analyzed totally. According to the variables, they are showed as percentage, mean values, and ranges of variation and percentages. The search in the medical literature revealed 104 studies which included 453 patients.
3. Result
The result reveals 453 patients. From which 222 (49%) case were male and female were 231 (51%). The mean age was 67.57 years ranging from 6 months to 97 years of age. The mean duration of presentation was 5.57 years ranging from 4 days to 60 years. The most common sites of affection are the head and neck (39.9%) followed by lower extremity (33.9%). Table 1 shows the distribution of the patients according to the site of affection. Mass and nodule are the most common modes of presentation. Table 2 shows presentation of the porocarcinoma with their frequency of appearance. Metastasis occurred at presentation in 110 (31%) cases. The most common organs to which porocarcinoma metastasize are the nearby lymph nodes (57.7%), followed by lung (12.8%). Table 3 shows the organs of metastasis.
Table 1.
Distribution of the patients according to the site of presentation.
| Site | Number (%) | References |
|---|---|---|
| Head and neck | 140 (39.9) | [3], [5], [7], [8], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45] |
| Lower extremity | 119 (33.9) | [8], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62] |
| Upper extremity | 31 (88) | [1], [8], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76] |
| Back | 18 (5.1) | [8], [77], [78], [79], [80], [81], [82], [83], [84] |
| Chest wall | 16 (4.6) | [85], [86], [87], [88] |
| Genitalia | 14 (4) | [8], [89], [90], [91], [92], [93], [94], [95] |
| Abdomen | 9 (2.6) | [8], [96], [97], [98], [99], [100], [101] |
| Perianal | 2 (0.6) | [102], [103] |
Table 2.
The most common presentations of porocarcinoma.
| Presentation | Number/Total | percentage |
|---|---|---|
| Mass and nodules | 109/153 | 71.2 |
| Ulcer | 28/153 | 18.3 |
| Plaque | 15/153 | 9.8 |
| swelling | 2/153 | 1.3 |
| Wart | 1/153 | 0.6 |
| papule | 1/153 | 0.6 |
| nevus | 1/153 | 0.6 |
Table 3.
The frequency of the organs to which porocarcinoma mostly metastasize.
| Site | Number/total | Percentage |
|---|---|---|
| Lymph nodes | 90/156 | 57.7 |
| Lung | 20/156 | 12.8 |
| Liver | 14/156 | 9 |
| Brain | 14/156 | 9 |
| Cutaneous | 9/156 | 5.8 |
| Bone | 5/156 | 3.2 |
| Breast | 1/156 | 0.6 |
| Stomach | 1/156 | 0.6 |
| Disseminated | 2/156 | 1.3 |
4. Discussion
Based on their findings, some authors stated that porocarcinoma is more common among male patients [7], [26]. The current metadata showed that porocarcinoma is evenly distributed according to the gender, both male and female are equally affected, (male 49% is nearly the same female 51%). The mean age of presentation is seventh and eighth decades of life (mean age 67.57 years, ranging from 7 months to 97 years) [34]. Most of the patients present with mass without symptoms (poroma) long time before converting to malignant type (porocarcinoma) [8], [62]. According to this study, the mean duration of presentation was 5.73 years. Robson and colleagues reported a case of porocarcinoma presented with history of 60 years of benign stable mass [30]. This finding may suggest that aggressive management of benign subcutaneous mass is advised to prevent malignant conversion especially when the diagnosis is not confirmed to be benign. The literature showed that most of the cases of porocarcinoma present with either nodule or mass [31]. The current meta-data also confirmed this finding and about 71.2% cases presented with either nodule or mass. Yamamoto and associates reported that majority of porocarcinoma lesions appear in the upper extremity (80%) while Shiohara and colleagues revealed the reverse of this finding. In their 12 case series, they reported that in 9 (75%) cases of them, the primary site was the lower extremity [30], [103]. Domere et al. stated that the most common primary sites for porocarcinoma are head and neck [28]. The result of this review confirmed the latter claim and found that in (39.9%) of the patients the primary sites were head and neck, followed by lower extremity (33.9%). The risk factors for developing porocarcinoma are not well understood. Several authors reported that their patients were in immune-compromised state. Some of them had history of immunosuppressive therapy and others decreased immunity from diseases [21], [26], [29]. Belin et al. studied two patients with porocarcinoma who received immunosuppressive medications, one for renal transplantation, and another for chronic lymphoid leukemia [26]. Mahomed and associates reported 5 cases of porocarcinoma with history of immune-compromised conditions, three of them were recipients of renal transplant and other two cases were the victims of acquired immune deficiency syndrome (AIDS) [29]. Owing to occurrence most commonly in sun exposed area (head, neck, hand, leg), some authors concluded that exposure to sun light is another risk factor [3], [5], [7], [10], [24]. In almost all cases, tissue biopsy was necessary for diagnosis in form of excisional, incisional and punch biopsy [21], [29]. In the literature, several histological features and subtype mentioned. These includes; ductal differentiation, nests of basaloid cells, squamoid tumor cells, infiltrative spinal cells, cells of acanthotic epidermis, Borst Judasson appearance, ulcerated epithelial tumor, bowenoid porocarcinoma, nests of small atypical cells, clear-cell, high infilterative pattern and hyperchromatic nuclear [7], [13], [26], [62], [72], [103], [102]. Surgery was the main mode of therapy with adjuvant chemoradiotherapy if metastasis and/or recurrence occurred [50], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104]. Metastasis was found in 110 (31%) cases [3], [10], [63], [65], [68], [73], [76], [86]. High rate of metastasis showed by this data reflects the real picture or due to the fact that physicians who encountered metastatic porocarcinoma are more likely to report their cases than the ones who did not encounter metastases is not known. The most common organs of metastasis are the regional lymph nodes (57.7%) [10], [63], [65], [73]. Although regional lymph node dissection was not performed routinely, high rate of metastasis to regional lymph nodes revealed by these meta-data may necessitate regional lymph node dissection. In spite of that there are no enough data to support routine lymph node dissection. Although most of the case series and case report did not mention the follow up and survival rate of the patient accurately, it can be seen in some report that porocarcinoma is very aggressive malignancy and kills the patient few months after the diagnosis regardless of the sort of management [67], [68], [69], [72], [95]. There are several limitations for study, first: the condition is rare. Second. The included papers were of different types. Third. Some of the papers did not report necessary data. Fourth. Some papers were so old that cannot be retrieved completely.
In conclusion, porocarcinoma presents with mass and nodule and affect head and neck in most of the cases. Tissue biopsy is the main method of diagnosis. It may develop from the benign counterpart (poroma) which may present several years before. It commonly metastasizes to lymph nodes. Wide local excision and regional lymph node dissection are adviced. Chemotherapy and radiotherapy are necessary when presented with metastasis and recurrence.
Ethical approval
Bioscience center.323.
Sources of funding
None.
Author contribution
Abdulwahid M. Salih, F.H. Kakamad, Hiwa O. Baba: substantial contribution of the concept and design, drafting the manuscript and final approval of the manuscript.
Rawezh Q.Salih, Hawbash M.R, Shvan H. Mohammed, Snur Othman: substantial contribution of the concept and design, acquisition of the data, final approval.
Yadgar A. Saeed, Imad J. Habibullah, Aso S. Muhialdeen, Rebaz O. Nawroly, Zuhair D. Hammood, Nawshirwan H. Abdulkarim: substantial contribution of the concept and design, analysis of data, drafting the manuscript, final approval of the data.
Conflicts of interest
None.
Research registration unique identifying number (UIN)
reviewregistry233.
Guarantor
Fahmi Hussein Kakamad, Fahmi.hussein@univsul.edu.iq.
References
- 1.Devi N.R., Valarmathi K., Lilly M., Satish S., Mishra N. Primary axillary porocarcinoma: a rare cutaneous tumour. J. Clin. Diagn. Res. 2016;10(2):4–6. doi: 10.7860/JCDR/2016/15278.7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luz Murilo de Almedia, Ogata Daniel Cury, Ribeiro Leandro Carvalho. Eccrine porocarcinoma (malignant Eccrine poroma) Clin. (Sao Paulo) 2010;65(7):739–742. doi: 10.1590/S1807-59322010000700014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeidan Youssef H., Jason Zauls A., Sharma Anand K. Treatment of Eccrine porocarcinoma with metastasis to parotid gland. J. Med. Case Rep. 2010;4:147. doi: 10.1186/1752-1947-4-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujimura Taku, Hashimoto Akira, Aiba Setsuya. Succesful treatment of eccrine porocarcinoma. Case Rep. Dermatol. 2014;6(2):159–163. doi: 10.1159/000365348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smita Surendra Masamatti, Chowdappa Vijaya. Eccrine porocarcinoma of scalp. J. Clin. Diagn. Res. Ser. online) 2016;1(1):1–16. doi: 10.7860/JCDR/2016/16083.7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lioyd Mark Sheldon, El-Muttardi Naguib, Robson A. Can. J. Plast. Surg. 2003;11(3):153–156. doi: 10.1177/229255030301100304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurashige Y., Minemura T., Nagatani T. Eccrine porocarcinoma: clinical and pathological report of eight cases. Case Rep. Dermatol. 2013;5(3):259–266. doi: 10.1159/000355606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehregan A.H., Hashimoto K., Rahbari H. Eccrine adenocarcinoma: a clinicopathologic study of 35 cases. Archiv. Dermatol. 1983;119(2):104–114. doi: 10.1001/archderm.119.2.104. [DOI] [PubMed] [Google Scholar]
- 9.Moher David, Liberati Alessandro, Tetzlaff Jennifer, Altmane Douglas G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int. J. Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed M.N., Kumar M.M., Ahmed S.M., Reddy N.V. Eccrine porocarcinoma of scalp with multiple secondaries arising after radiotherapy for hypopharyngeal carcinoma. J. Evol. Med. Dent. Sci. 2014;3(27):7574–7578. [Google Scholar]
- 11.Gerber P.A., Schulte K.W., Ruzicka T., Bruch-Gerharz D. Eccrine porocarcinoma of the head: an important differential diagnosis in the elderly patient. Dermatology. 2008;216(3):229–233. doi: 10.1159/000112931. [DOI] [PubMed] [Google Scholar]
- 12.Klenzner T., Arapakis I., Kayser G., Boedeker C.C. Eccrine porocarcinoma of the ear mimicking basaloid squamous cell carcinoma. Otolaryngol. Head Neck Surg. 2006;135(1):158–160. doi: 10.1016/j.otohns.2005.03.041. [DOI] [PubMed] [Google Scholar]
- 13.Bleier B.S., Newman J.G., Quon H., Feldman M.D., Kent K.K., Weinstein G.S. Eccrine porocarcinoma of the nose: case report and review of world literature. Archiv. Otolaryngol. Head Neck Surg. 2006;132(2):215–218. doi: 10.1001/archotol.132.2.215. [DOI] [PubMed] [Google Scholar]
- 14.Ciesielski P., Górnicka B., Górnicki K., Kołodziejczak M., Siekierski P. Neck sweat gland cancer hemorrhage. Case study. ContempOncol. Pozn. 2013;17:100–102. doi: 10.5114/wo.2013.33784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masamatti S.S., Narasimha A., Bhat A., Chowdappa V. Eccrine porocarcinoma of the scalp: a rare case report with review of literature. J. Clin. Diagn. Res. 2016;10(1):15–16. doi: 10.7860/JCDR/2016/16083.7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phukan J.P., Sengupta S., Sinha A. Eccrine porocarcinoma of scalp: a rare case report. Iran. J. Pathol. 2015;10(1):65–68. [PMC free article] [PubMed] [Google Scholar]
- 17.Permi H.S., Bhat S.P., Prasad H.L.K., Bhat V.S. Eccrine porocarcinoma of scalp: an uncommon tumor at an unusual site. Indian J. Surg. Oncol. 2011;2(2):145–147. doi: 10.1007/s13193-011-0069-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rana R.E., Verma S.S., Puri V.A., Baliarsing A.S. Sweat gland tumor (Eccrine Porocarcinoma) of scalp: a rare tumor. Indian J. Plastic Surg. 2005;38(1):51–53. [Google Scholar]
- 19.Jeon H., Smart C. An unusual case of porocarcinoma arising on the scalp of a 22-Year-old woman. Am. J. Dermatopathol. 2015;37(3):237–239. doi: 10.1097/DAD.0000000000000111. [DOI] [PubMed] [Google Scholar]
- 20.Melgandi W., Benson R., Hakin A., Bhasker S. Porocarcinoma scalp with high risk features treated with surgery and adjuvant radiotherapy: a case report and review of literature. J. Egypt. Natl. Cancer Inst. 2016;28(3):195–198. doi: 10.1016/j.jnci.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Kim Y., Scolyer R.A., Chia E.M., Steven D., Ghabrial R. Eccrine porocarcinoma of the upper eyelid. Australas. J. Dermatol. 2005;46(4):278–281. doi: 10.1111/j.1440-0960.2005.00201.x. [DOI] [PubMed] [Google Scholar]
- 22.Zeidan Y.H., Zauls A.J., Bilic M., Lentsch E.J., Sharma A.K. Treatment of eccrine porocarcinoma with metastasis to the parotid gland using intensity-modulated radiation therapy: a case report. J. Med. Case Rep. 2010;4(1):147. doi: 10.1186/1752-1947-4-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mak S.T., Li K.K. Eccrineporocarcinoma of the eyelid in a Non-Caucasian patient. Ophthalmic Plastic Reconstr. Surg. 2015;31(6):166–168. doi: 10.1097/IOP.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 24.Chua P.Y., Cornish K.S., Stenhouse G., Barras C.W. A rare case of eccrine porocarcinoma of the eyelid. Semin. Ophthalmol. 2015;30(6):443–445. doi: 10.3109/08820538.2013.874475. [DOI] [PubMed] [Google Scholar]
- 25.D'Ambrosia R.A., Ward H., Parry E. Eccrine porocarcinoma of the eyelid treated with Mohs micrographic surgery. Dermatol. Surg. 2004;30(4):570–571. doi: 10.1111/j.1524-4725.2004.30181.x. [DOI] [PubMed] [Google Scholar]
- 26.Belin E., Ezzedine K., Stanislas S., Lalanne N., Beylot-Barry M., Taieb A. Factors in the surgical management of primary eccrine porocarcinoma: prognostic histological factors can guide the surgical procedure. Br. J. Dermatol. 2011;165(5):985–989. doi: 10.1111/j.1365-2133.2011.10486.x. [DOI] [PubMed] [Google Scholar]
- 27.Hirsh L.F., Enterline H.T., Rosato E.F., Rosato F.E. Sweat gland carcinoma. Ann. Surg. 1971;174(2):283. doi: 10.1097/00000658-197108000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.El-Domeiri A.A., Brasfield R.D., Huvos A.G., Strong E.W. Sweat gland carcinoma: a clinico-pathologic study of 83 patients. Ann. Surg. 1971;173(2):270. doi: 10.1097/00000658-197102000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahomed F., Blok J., Grayson W. The squamous variant of eccrine porocarcinoma: a clinicopathological study of 21 cases. J. Clin. Pathol. 2008;61(3):361–365. doi: 10.1136/jcp.2007.049213. [DOI] [PubMed] [Google Scholar]
- 30.Robson A., Greene J., Ansari N., Kim B., Seed P.T., McKee P.H., Calonje E. Eccrine porocarcinoma (malignant eccrine poroma): a clinicopathologic study of 69 cases. Am. J. Surg. Pathol. 2001;25(6):710–720. doi: 10.1097/00000478-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Shiohara J., Koga H., Uhara H., Takata M., Saida T. Eccrine porocarcinoma: clinical and pathological studies of 12 cases. J. Dermatol. 2007;34(8):516–522. doi: 10.1111/j.1346-8138.2007.00324.x. [DOI] [PubMed] [Google Scholar]
- 32.Tidwell W.J., Mayer J.E., Malone J., Schadt C., Brown T. Treatment of eccrine porocarcinoma with Mohs micrographic surgery: a cases series and literature review. Int. J. Dermatol. 2015;54(9):1078–1083. doi: 10.1111/ijd.12997. [DOI] [PubMed] [Google Scholar]
- 33.Tolkachjov S.N., Hocker T.L., Camilleri M.J., Baum C.L. Treatment of PorocarcinomaWith mohs micrographic surgery: the mayo clinic experience. Dermatol. Surg. 2016;42(6):745–750. doi: 10.1097/DSS.0000000000000763. [DOI] [PubMed] [Google Scholar]
- 34.Urso C., Bondi R., Paglierani M., Salvadori A., Anichini C., Giannini A. Carcinomas of sweat glands: report of 60 cases. Archiv. Pathol. Lab. Med. 2001;125(4):498–505. doi: 10.5858/2001-125-0498-COSG. [DOI] [PubMed] [Google Scholar]
- 35.Xu Y.G., Aylward J., Longley B.J., Hinshaw M.A., Snow S.N. Eccrine porocarcinoma treated by Mohs micrographic surgery: over 6-year follow-up of 12 cases and literature review. Dermatol. Surg. 2015;41(6):685–692. doi: 10.1097/DSS.0000000000000382. [DOI] [PubMed] [Google Scholar]
- 36.Chow C.W., Campbell P.E., Burry A.F. Sweat gland carcinomas in children. Cancer. 1984;53(5):1222–1227. doi: 10.1002/1097-0142(19840301)53:5<1222::aid-cncr2820530533>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 37.Riera Leal L., Guevara Gutiérrez E., Barrientos García J.G., Madrigal Kasem R., Briseño Rodríguez G., Tlacuilo Parra A. Eccrine porocarcinoma: epidemiologic and histopathologic characteristics. Int. J. Dermatol. 2015;54(5):580–586. doi: 10.1111/ijd.12714. [DOI] [PubMed] [Google Scholar]
- 38.Fujimura T., Hashimoto A., Furudate S., Kambayashi Y., Haga T., Aiba S. Successful treatment of eccrine porocarcinoma metastasized to a cervical lymph node with CyberKnife radiosurgery. Case Rep. Dermatol. 2014;6(2):159–163. doi: 10.1159/000365348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gutermuth J., Audring H., Voit C., Trefzer U., Haas N. Antitumour activity of paclitaxel and interferon-alpha in a case of metastatic eccrine porocarcinoma. J. Eur. Acad. Dermatol. Venereol. 2004;18(4):477–479. doi: 10.1111/j.1468-3083.2004.00949.x. [DOI] [PubMed] [Google Scholar]
- 40.Lan C.C., Yu H.S., Liao W.T., Hsu R.C., Chung J.C., Tsai K.B. Clear cell eccrine porocarcinoma with extensive cutaneous metastasis and peripheral lymphocyte dysfunction. Br. J. Dermatol. 2003;149(5):1059–1063. doi: 10.1111/j.1365-2133.2003.05638.x. [DOI] [PubMed] [Google Scholar]
- 41.Latifi H., Mikaili P., Rozbehani N.A., Taherian S., Latifi K. Malignant eccrine poroma (eccrine porocarcinoma): report of a clinical case. Comp. Clin. Pathol. 2012;21(6):1131–1133. [Google Scholar]
- 42.Maguire C.A., Kazlouskaya V., Buchen D., Heller P., Elston D.M. Porocarcinoma with perineural invasion. Indian Dermatol. Online J. 2015;6(2):122. doi: 10.4103/2229-5178.153018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Asghar A.H., Mahmood H., Faheem M., Rizvi S., Khan K.A., Irfan J. Porocarcinoma: a rare sweat gland malignancy. J. Coll. Phys. Surg. Pak. 2009;19(6):389–390. [PubMed] [Google Scholar]
- 44.Bogner P.N., Fullen D.R., Lowe L., Paulino A., Sybil Biermann J., Sondak V.K. Lymphatic mapping and sentinel lymph node biopsy in the detection of early metastasis from sweat gland carcinoma. Cancer. 2003;97(9):2285–2289. doi: 10.1002/cncr.11328. [DOI] [PubMed] [Google Scholar]
- 45.Chang N.C., Tsai K.B. Eccrine porocarcinoma of the auricle: a case report. Kaohsiung J. Med. Sci. 2009;25(7):401–404. doi: 10.1016/S1607-551X(09)70534-0. [DOI] [PubMed] [Google Scholar]
- 46.Dewan P., Moir G., Cerio R., Harwood C. Aggressive eccrine porocarcinoma associated with haematological disorders: report of two cases. Clin. Exp. Dermatol. 2010;35(4):207–209. doi: 10.1111/j.1365-2230.2009.03739.x. [DOI] [PubMed] [Google Scholar]
- 47.Divvya B, Valluvan M, Tippoo R, Viswanathan P, Ramesh R. Malignant poroma synonym: porocarcinoma eccrine poroma malignant. J. Evol. Med. Dent. Sci.;1(3):4834–4838.
- 48.Montes Torres A., Pérez Plaza A., Llamas Velasco M., Gordillo C., De Argila D., García C. Eccrine porocarcinoma with extensive cutaneous metastases. Int. J. Dermatol. 2016;55:156–160. doi: 10.1111/ijd.13121. [DOI] [PubMed] [Google Scholar]
- 49.Obi M., Satoh T., Yokozeki H., Nishioka K. Eccrine porocarcinoma with Bowenoid changes: epithelial membrane antigen is not a useful marker for malignant tumours arising from eccrine gland structures. Actadermato-venereologica. 2004;84(2):142–144. doi: 10.1080/00015550310006211. [DOI] [PubMed] [Google Scholar]
- 50.Serhrouchni K.I., Harmouch T., Chbani L., El Fatemi H., Sekal M., Hammas N. Eccrine carcinoma: a rare cutaneous neoplasm. Diagn. Pathol. 2013;8(1):15. doi: 10.1186/1746-1596-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sharathkumar H.K., Hemalatha A.L., Deepthi B.R., AnkitaSoni R.V. Eccrine porocarcinoma: a case report. J. Clin. Diagn. Res. 2013;7(12):2966–2967. doi: 10.7860/JCDR/2013/6964.3707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sheff J.S., MacDougall D.B. Unusual case of porocarcinoma of the foot with no clinically evident dermatologic manifestations. J. Foot Ankle Surg. 2005;44(5):412–414. doi: 10.1053/j.jfas.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 53.Suzaki R., Shioda T., Konohana I., Ishizaki S., Sawada M., Tanaka M. Dermoscopic features of eccrine porocarcinoma arising from hidroacanthoma simplex. Dermatol. Res. Pract. 2010;1(1) doi: 10.1155/2010/192371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vandeweyer E., Renoirte C., Musette S., Gilles A. Eccrine porocarcinoma: a case report. ActaChirurgicaBelgica. 2006;106(1):121–123. doi: 10.1080/00015458.2006.11679853. [DOI] [PubMed] [Google Scholar]
- 55.Goel R., Contos M.J., Wallace M.L. Widespread metastatic eccrine porocarcinoma. J. Am. Acad. Dermatol. 2003;49(5):252–254. doi: 10.1016/s0190-9622(03)00444-4. [DOI] [PubMed] [Google Scholar]
- 56.González López M.A., Vázquez López F., Soler T., Gómez Diéz S., Garcia Y.H., Manjón J.A. Metastatic eccrine porocarcinoma: a 5.6-Year follow up study of a patient treated with a combined therapeutic protocol. Dermatol. Surg. 2003 Dec 1;29(12):1227–1232. doi: 10.1111/j.1524-4725.2003.29393.x. [DOI] [PubMed] [Google Scholar]
- 57.Hong Y.J., Oh J.E., Choi Y.W., Myung K.B., Choi H.Y. A case of clear cell eccrine porocarcinoma. Ann. Dermatol. 2010;22(3):330–332. doi: 10.5021/ad.2010.22.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ishida M., Hotta M., Kushima R., Okabe H. A case of porocarcinoma arising in pigmented hidroacanthoma simplex with multiple lymph node, liver and bone metastases. J. Cutan. Pathol. 2011;38(2):227–231. doi: 10.1111/j.1600-0560.2009.01440.x. [DOI] [PubMed] [Google Scholar]
- 59.Lloyd M.S., El-Muttardi N., Robson A. Eccrine porocarcinoma: a case report and review of the literature. Can. J. Plastic Surg. 2003;11(3):153. doi: 10.1177/229255030301100304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lowney A.C., Mc Aleer M.A., O'Connor K., Fitzgibbon J.F., Bourke J.F. Eccrine porocarcinoma arising within an area of Bowen disease. Clin. Exp. Dermatol. 2012;37(2):136–138. doi: 10.1111/j.1365-2230.2011.04167.x. [DOI] [PubMed] [Google Scholar]
- 61.Manimaran D. Eccrine porocarcinoma associated with an eccrine poroma. Online J. Health Allied Sci. 2014;13(2):5. [Google Scholar]
- 62.Baroni A., Russo T., Piccolo V., Siano M., Russo D., Nacca L. Opportunistic metastatic porocarcinoma after saphenous venectomy for coronary bypass surgery. Clin. Exp. Dermatol. 2013;38(5):507–510. doi: 10.1111/ced.12032. [DOI] [PubMed] [Google Scholar]
- 63.Plunkett T.A., Hanby A.M., Miles D.W., Rubens R.D. Metastatic eccrine porocarcinoma: response to docetaxel (Taxotere) chemotherapy. Ann. Oncol. 2001;12(3):411–414. doi: 10.1023/a:1011196615177. [DOI] [PubMed] [Google Scholar]
- 64.Raheemullah A., Allamaneni S., Weber S., Singh R. Eccrine porocarcinoma presenting as a hand cyst. J. Hand Surg. 2016;41(11):425–427. doi: 10.1016/j.jhsa.2016.07.112. [DOI] [PubMed] [Google Scholar]
- 65.Ramirez Y., Fellegara G., Bugiani M. Eccrine porocarcinoma with carcinomatous lymphangitis in a patient with history of arsenic exposure: a case report. Int. J. Surg. Pathol. 2012;20(5):515–518. doi: 10.1177/1066896911428738. [DOI] [PubMed] [Google Scholar]
- 66.Vaz Salgado M., García C.G., Martin L., Antonio J., Guerra E., Benito A. Porocarcinoma: clinical evolution. Dermatol. Surg. 2010;36(2):264–267. doi: 10.1111/j.1524-4725.2009.01412.x. [DOI] [PubMed] [Google Scholar]
- 67.Vleugels F.R., Girouard S.D., Schmults C.D., Ng A.K., Russell S.E., Wang L.C. Metastatic eccrine porocarcinoma after Mohs micrographic surgery: a case report. J. Clin. Oncol. 2012;30(21):188–191. doi: 10.1200/JCO.2011.40.6843. [DOI] [PubMed] [Google Scholar]
- 68.Wong A., Hughes C., Luu X., Ricci A., Babigian A. Subungal malignant eccrine porocarcinoma: an unusual presentation. Eur. J. Plastic Surg. 2013;36(2):131–133. [Google Scholar]
- 69.De Giorgi V., Sestini S., Massi D., Papi F., Lotti T. Eccrine porocarcinoma: a rare but sometimes fatal malignant neoplasm. Dermatol. Surg. 2007;33(3):374–377. doi: 10.1111/j.1524-4725.2007.33077.x. [DOI] [PubMed] [Google Scholar]
- 70.Ioannidis S., Antoniou A., Patsatsi A., Kostogloudis N., Demiri E., Foroglou P. Eccrine porocarcinoma of the thumb in a patient with chronic exposure to benzene glue. J. Hand Microsurg. 2015;7(1):157–160. doi: 10.1007/s12593-014-0132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Marone U., Caracò C., Anniciello A.M., Di Monta G., Chiofalo M.G., Di Cecilia M.L. Metastatic eccrine porocarcinoma: report of a case and review of the literature. World J. Surg. Oncol. 2011;9(1):32. doi: 10.1186/1477-7819-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Arslan D., Tatlı A.M., Uysal M., Kaplan M.A. Eccrine porocarcinoma: a case report and literature review. J. Clin. Exp. Investig. 2013;4(3):370–373. [Google Scholar]
- 73.Bhat W., Akhtar S., Khotwal A., Platt A.J. Primary eccrine porocarcinoma of the finger with transit forearm and axillary metastasis. Ann. Plastic Surg. 2011;66(4):344–346. doi: 10.1097/SAP.0b013e3181e35c8d. [DOI] [PubMed] [Google Scholar]
- 74.Mandaliya H., Nordman I. Metastatic eccrine porocarcinoma: a rare case of successful treatment. Case Rep. Oncol. 2016;9(2):454–456. doi: 10.1159/000448073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kurokawa I., Urakawa Y., Senba Y., Kawabata E., Nishimura K., Omoto Y., Tokime K., Mizutani H., Tsubura A. Keratin profiles may differ between intraepidermal and intradermal invasive eccrine porocarcinoma. Oncol. Rep. 2006;16(3):473–478. [PubMed] [Google Scholar]
- 76.Salih Abdulwahid M., Kakamad F.H., Essa Rawand A., Rauf Goran M., Masrur S.A., Shvan H.M. Porocarcinoma: a systematic review of literature with a single case report. Int. J. Surg. Case Rep. 2017;30(1):13–16. doi: 10.1016/j.ijscr.2016.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Müller N.S., Zschoche C., Hartschuh W., Lonsdorf A.S. Zosteriform metastases of eccrine porocarcinoma mimicking eruptive seborrhoeic keratoses. Actadermato-venereologica. 2015;95(2):245–246. doi: 10.2340/00015555-1902. [DOI] [PubMed] [Google Scholar]
- 78.Ou C.L., Cheng C.J., Wang K.H. Porocarcinoma in situ showing follicular differentiation: a case report. DermatologicaSinica. 2012;30(2):47–50. [Google Scholar]
- 79.Thuruthil R.R., Jayalakshmy P.S., Sukumar V. A case of recurrent eccrine porocarcinoma with regional lymph nodal metastasis, arising on a Bowen's disease patch. Indian J. Surg. 2015;77(1):182–184. doi: 10.1007/s12262-015-1255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ueo T., Kashima K., Daa T., Kondoh Y., Yanagi T., Yokoyama S. Porocarcinoma arising in pigmented hidroacanthoma simplex. Am. J. Dermatopathol. 2005;27(6):500–503. doi: 10.1097/01.dad.0000148874.20941.43. [DOI] [PubMed] [Google Scholar]
- 81.Johr R., Saghari S., Nouri K. Eccrine porocarcinoma arising in a seborrheic keratosis evaluated with dermoscopy and treated with Mohs' technique. Int. J. Dermatol. 2003;42(8):653–657. doi: 10.1046/j.1365-4362.2003.01779.x. [DOI] [PubMed] [Google Scholar]
- 82.Blum A., Metzler G., Bauer J. Polymorphous vascular patterns in dermoscopy as a sign of malignant skin tumors. Dermatology. 2005;210(1):58–59. doi: 10.1159/000081486. [DOI] [PubMed] [Google Scholar]
- 83.Cowden A., Dans M., Militello G., Junkins-Hopkins J., Voorhees A.S. Eccrine porocarcinoma arising in two African American patients: distinct presentations both treated with Mohs micrographic surgery. Int. J. Dermatol. 2006;45(2):146–150. doi: 10.1111/j.1365-4632.2006.02735.x. [DOI] [PubMed] [Google Scholar]
- 84.Acosta-Arencibia A., Abrante-Expósito B., Ramos-Gordillo M. Multiple recurrent eccrine porocarcinoma with inguinal metastasis. A case report. Cirugía Cir. (English Ed. 2016;84(1):73–76. doi: 10.1016/j.circir.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 85.Chen I.S., Kuo H.W., Eng H.L. Porocarcinoma in a patient with chronic arsenism and multiple Bowen's disease: case report. Dermatol. Surg. 2005;31(9):1149–1151. [PubMed] [Google Scholar]
- 86.Aaribi I., Mohtaram A., Ben Ameur El Youbi M., Kharmoum J., El Kabous M., Mrabti H. Successful management of metastatic eccrine porocarcinoma. Case Rep. Oncol. Med. 2013;1(1) doi: 10.1155/2013/282536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Goh S.G., Dayrit J.F., Calonje E. Sarcomatoid eccrine porocarcinoma: report of two cases and a review of the literature. J. Cutan. Pathol. 2007;34(1):55–60. doi: 10.1111/j.1600-0560.2006.00556.x. [DOI] [PubMed] [Google Scholar]
- 88.Cursino F.D., Teixeira L., Lima E.D., Lima M.D., Rodrigues S.C., Takano D. Porocarcinoma: case report. An. Bras. Dermatol. 2011;86(6):1201–1204. doi: 10.1590/s0365-05962011000600024. [DOI] [PubMed] [Google Scholar]
- 89.Nakazawa T., Kondo T., Sato E., Motosugi U., Niu D., Mochizuki K. Subcutaneous porocarcinoma clinically presenting as a soft tissue tumor. J. Cutan. Pathol. 2015;42(11):897–902. doi: 10.1111/cup.12576. [DOI] [PubMed] [Google Scholar]
- 90.Grayson W., Loubser J.S. Eccrine porocarcinoma of the penis. J. Urol. 2003;169(2):611–612. doi: 10.1097/01.ju.0000043668.85485.c7. [DOI] [PubMed] [Google Scholar]
- 91.Ma H., Liao M., Qiu S., Lu R., Lu C. Eccrine poroma and porocarcinoma on the same unusual location: report on two cases. An. Bras. Dermatol. 2015;90(3):69–72. doi: 10.1590/abd1806-4841.20153415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kalogeraki A., Tamiolakis D., Tsagatakis T., Geronatsiou K., Haniotis V., Kafoussi M. Eccrine porocarcinoma: cytologic diagnosis by fine needle aspiration biopsy (FNAB) ActaMédica Port. 2013;26(4):467–470. [PubMed] [Google Scholar]
- 93.Adegboyega P.A. Eccrine porocarcinoma of the vulva: a case report and review of literature. Int. J. Gynecol. Pathol. 2011;30(1):95–100. doi: 10.1097/PGP.0b013e3181ea11b1. [DOI] [PubMed] [Google Scholar]
- 94.Choi C.M., Cho H.R., Lew B.L., Sim W.Y. Eccrine porocarcinoma presenting with unusual clinical manifestations: a case report and review of the literature. Ann. Dermatol. 2011;23(1):s79–s83. doi: 10.5021/ad.2011.23.S1.S79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kurisu Y., Tsuji M., Yasuda E., Shibayama Y. A case of eccrine porocarcinoma: usefulness of immunostain for s-100 protein in the diagnoses of recurrent and metastatic dedifferentiated lesions. Ann. Dermatol. 2013;25(3):348–351. doi: 10.5021/ad.2013.25.3.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Parmar N., Mohamed M., Elmoghrabi A., McCann M. Eccrine Porocarcinoma presenting as an abdominal wall mass in a patient with ulcerative colitis—a rare case report. Int. J. Surg. Case Rep. 2016;23:40–43. doi: 10.1016/j.ijscr.2016.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zheng L.Q., Han X.C., Huang Y., Li H.W., Niu X.D., Li J. Porocarcinoma coexisting at a site of Bowen disease in a 63-year-old woman. Clin. Exp. Dermatol. 2015;40(3):293–297. doi: 10.1111/ced.12534. [DOI] [PubMed] [Google Scholar]
- 98.Hoshina D., Akiyama M., Hata H., Aoyagi S., Sato-Matsumura K.C., Shimizu H. Eccrine porocarcinoma and Bowen's disease arising in a seborrhoeic keratosis. Clin. Exp. Dermatol. 2007;32(1):54–56. doi: 10.1111/j.1365-2230.2006.02260.x. [DOI] [PubMed] [Google Scholar]
- 99.Jeon J., Kim J.H., Baek Y.S., Kim A., Seo S.H., Oh C.H. Eccrine poroma and eccrine porocarcinoma in linear epidermal nevus. Am. J. Dermatopathol. 2014;36(5):430–432. doi: 10.1097/DAD.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 100.Lee J.B., Oh C.K., Jang H.S., Kim M.B., Jang B.S., Kwon K.S. A case of porocarcinoma from pre-existing hidroacanthoma simplex: need of early excision for hidroacanthoma simplex? Dermatol. Surg. 2003;29(7):772–774. doi: 10.1046/j.1524-4725.2003.29195.x. [DOI] [PubMed] [Google Scholar]
- 101.Choi S.H., Kim Y.J., Kim H., Kim H.J., Nam S.H., Choi Y.W. A rare case of abdominal porocarcinoma. Archiv. Plastic Surg. 2014;41(1):91–93. doi: 10.5999/aps.2014.41.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Iannicelli E., Galluzzo A., Salvi P.F., Ziparo V., David V. A large porocarcinoma of perineal region: MR findings and review of the literature. Abdom. Imaging. 2008;33(6):744–747. doi: 10.1007/s00261-007-9356-4. [DOI] [PubMed] [Google Scholar]
- 103.Borgognoni L., Pescitelli L., Urso C., Brandani P., Sestini S., Chiarugi C. A rare case of anal porocarcinoma treated by electrochemotherapy. Future Oncol. 2014;10(15):2429–2434. doi: 10.2217/fon.14.141. [DOI] [PubMed] [Google Scholar]
- 104.Rutten Arno, Requena Luis, Requena Celia. Clear-cell porocarcinoma in situ; a cytologic variant of porocarcinoma in situ. Am. J. Dermatopathol. 2000;24(1):67–71. doi: 10.1097/00000372-200202000-00014. [DOI] [PubMed] [Google Scholar]
Further reading
- 105.Yamamoto Osamu, Haratake Joji, Yokoyama Shigeo, Imayama Shuhei, Asahi Masakazu. A histopathological and ultrastructural study of eccrine porocarcinoma with special reference to its subtypes. Virchows Arch. A Pathol. Anat. 1992;420:395–401. doi: 10.1007/BF01600510. [DOI] [PubMed] [Google Scholar]