Abstract
Background
The Afar people inhabit the sub-arid and arid part of Ethiopia. Recurrent drought and invasive encroaching plants are taking out plants that have cultural importance, and threaten the biodiversity and the associated traditional knowledge. Thus, the aim of the current study is to conduct an ethnobotanical survey and document medicinal and edible plants in Yalo Woreda in Afar regional state.
Methods
A cross-sectional ethnobotanical study was carried out in eight kebeles of Yalo Woreda from October 2015 to December 2016. One hundred sixty informants were selected using purposive sampling. The data on diseases, medicinal and edible plants were collected using semi-structure interview and group discussion. The statistical methods, informant consensus factor, fidelity level, and preference ranking were conducted to analyze the data.
Results
One hundred and six plants were reported; gender and age differences had implication on the number of plants reported by informants. The knowledge of medicinal plants among informants of each kebele was not different (p < 0.5) and was not associated in particular with the religious establishment in the kebeles (informant*kebeles, Eta square = 0.19). Family Fabaceae was the major plant species, and shrubs (44%) were dominant plants reported. Leaf (52.94%) and oral (68%) were primary plant part used for remedy preparation and route of application, respectively. The plants with low fidelity values Indigofera articulata (0.25), Cadaba farinosa (0.22), Cadaba rotundifolia (0.19), and Acalypha fruticosa (0.15) were used to treat the category of diseases with high informant consensus value (0.69). Sixteen edible plants were identified that were consumed during wet and dry seasons. Balanites aegyptiaca, Balanites rotundifolia, and Dobera glabra were ‘famine food’ that were collected and stored for years.
Conclusion
People in Yalo Woreda are more dependent on natural resources of the area for their livelihood. The threat of climatic change and encroaching invasive plants on medicinal and edible plants affects the traditional use of plants in the Yalo Woreda. The conservation of the plants in the home garden and natural habitat and integration of edible plants into agroforestry development programs in sub-arid and arid regions has to be encouraged to conserve plants of medical and economic importance.
Electronic supplementary material
The online version of this article (doi:10.1186/s13002-017-0166-7) contains supplementary material, which is available to authorized users.
Keywords: Afar people, Yalo Woreda, Ethnobotanical study, Traditional knowledge, Medicinal plants, Edible plants, Ethiopia
Background
Afar people are pastoralists that live in the Great Rift Valley of Ethiopia. Afar Regional State is located in the eastern part of Ethiopia, bordering the State of Eritrea in the northeast, Tigray in the northwest, Amhara in the southwest, Oromia in the south, the State of Somalia in the southeast and the Republic of Djibouti in the east [1]. The Erta Ale active volcano in the Danakil depression (120 m below sea level), the lowest point below sea level in Ethiopia is found in the northern part of the region. The Afar Regional state is subdivided into five administrative zones. The population of the area based on the 2007 census is 1,390,273 consisting of 775,117 men and 615,156 women with an estimated density of 14.38 people per square kilometer [2]. The estimated area of the region is 96,707 Km2 and lies between 8° 40′13″ to 14° 27′ 29″ N latitude and 39° 51′13″ to 42° 23′03″ E longitude. The climate of the region is semi-arid to arid with erratic rainfall, and altitude ranges from 120 m below sea level up to 1500 masl. The vegetation of the area is Acacia-Commiphora (Small-Leaved Deciduous) Woodland; 31.5% shrubland, 14.8% grassland, 1.75% woodland and 0.11% forestland with a large area (49.6%) of rocky, sandy and exposed soil [3–5].
The people in the Afar region have the lowest health and education coverage in the country with the highest food insecurity [6]. They are a traditional society that has native and unique information exchange system by word of mouth called ‘Dagu,’ which their livelihood is very much dependent on the information transferred through Dagu system. The information ranges from weather to availability of grazing lands for their animals, and peace and security of the region [4]. Nevertheless, the cultural transformation, expansion of modern education and development in the area could detach the younger generation from such cultural values and pastoral systems that lead to loss of traditional knowledge in general, and knowledge of medicinal and edible plants in particular [7, 8].
The Afar people mostly depend on their animals and their products, and vegetation of the area as a resource for their livelihood. The animal products milk, meat, and butter are used as the primary diet, and live animals, hide, and skin generates the pastoral’s economy. The vegetation of the area is associated with significant uses such as medicine, food for human and livestock, firewood, charcoal, building materials and for making household goods [1, 9, 10]. They often move from one place to another in search of food and water for their livestock [6]. The Afar people’s livestock proportion varies accordingly with the vegetation cover of the locality. The dominant animal in the reverine forest and with better grassland are cattle and sheep, in the drier parts of the region camel and goat are dominant, and in the arid zones camels are widely dominant animal [1].
The vegetation of the area is severely affected by increased overexploitation for charcoal production and clearing forests for settlement and agriculture [3]. Some of the woody and grass species are declining such as Acacia nilotica (L.) Willd. ex Del., Acacia senegal (L.) Willd., Acacia tortilis (Forssk.) Schweinf., Balanites aegyptiaca (van Tieghem) Blatter, Cordia gharaf (Forsk.), Ziziphus spina-christi (L.) Desf. Cenchrus species and Cynodon species are the most affected and young seedlings are not usually seen growing [1, 10–14]. The recent incidents in the Afar region is the invasive encroaching plants; Prosopis juliflora (Sw.) DC. (Woyane), Parthenium hysterophorus L. (white top weed), and Cryptostegia grandiflora Roxb. ex R. Br. (rubber vine) are taking out multipurpose trees, grassland, and bushes and transforming the region to the mono-species thick forest. Prosopis juliflora has an effect on the total biodiversity of the area by reducing their abundance, distribution, and ecological function and replacing grassland and natural forests. It is a cause for the fast disappearing of plants used by the people as medicine and food supplements in normal time and during a food shortage. Also, P. hysterophorus and C. grandiflora are a threat to grassland and livelihood of the people in the region. The vast destruction of the natural habitats leads to a gradual disappearance of the associated traditional knowledge of medicinal and edible plants [1, 6, 14–20].
The Afar people, in the past, depends on milk and its’ products as main diet and edible plants of the area as a source of food in harsh times. The intensification and severity of drought caused by the climatic change, in the pastoral area, complicated and disrupted the relationship between the society and natural environment [1]. At present, because of recurrent severe drought, massive loss of livestock and dependence on relief food, the Afar People has shifted their feeding habit, and it is a cause for loss of traditional knowledge of edible plants by the younger generation [8]. According to Alemu [21], the Afar elders were aware that their traditional way of life is changing in several respects including effects of cultivation, overexploitation, and bush encroachment that would result in a declining trend in all natural resources. Moreover, Atanga et al. [6] reported, based on the interview with the older livestock herders, that 63% of grazing plant species has disappeared within 25 years from the rangelands. Hence, there is a gradual erosion of knowledge of medicinal and edible plants in the society, which requires formal ethnobotanical documentation [1, 4, 19, 20]. On the other hand, the ethnobotanical studies conducted in the Afar Region are few, and most of these studies are carried out in Awash Park where the majority of the inhabitants are Oromo People [9, 10, 14–23]. Thus, the aim of this study is to survey the traditional knowledge of medicinal and edible plants of Afar People in Yalo Woreda (District), Zone 4, Afar Regional state. The study may be used as a foundation for pharmacological and nutritional studies and identification of useful plants of the region for conservation.
Methods
Study area
A cross-sectional ethnobotanical study was conducted in eight kebeles (smallest administrative division) of Yalo Woreda from October 2015 to December 2016. Yalo Woreda is located 732 km from Addis Ababa in Zone 4, the western part of Afar Regional State; bordering Megalea Woreda in the north, Gelina Woreda in the south, Teru Woreda in the east, and Alamata Woreda in the west (Fig. 1). The landscape varies from undulating hills to flat land, and the area of the Woreda is 822.75 Km2. The climate of the Woreda is kola (Lowland) with average minimum temperature of 21 °C and maximum 38 °C and with 500 mm annual average rainfall [24]. The kebeles are Dibina (12°23′45″ N, 39°52′58″ E, 890 masl); Gidi Elea (12°16′46″ N, 39°54′31″ E, 974 masl); Kolina Gabulea (12°23′24″ N, 39°56′57″ E, 811 masl); Mesgid (12° 21′45″ N, 39°52′44″ E, 865 masl); Rekrek (12°23′9″ N, 39°52′30″ E, 893 masl); Reku Dora (12°16′46″ N, 39°54′31″ E, 974 masl); Waleae (12°17′36″ N, 39°24′11″ E, 890 masl) and Wudayili (12° 19′26″ N, 39°44′21″ E, 874 masl).
Fig. 1.
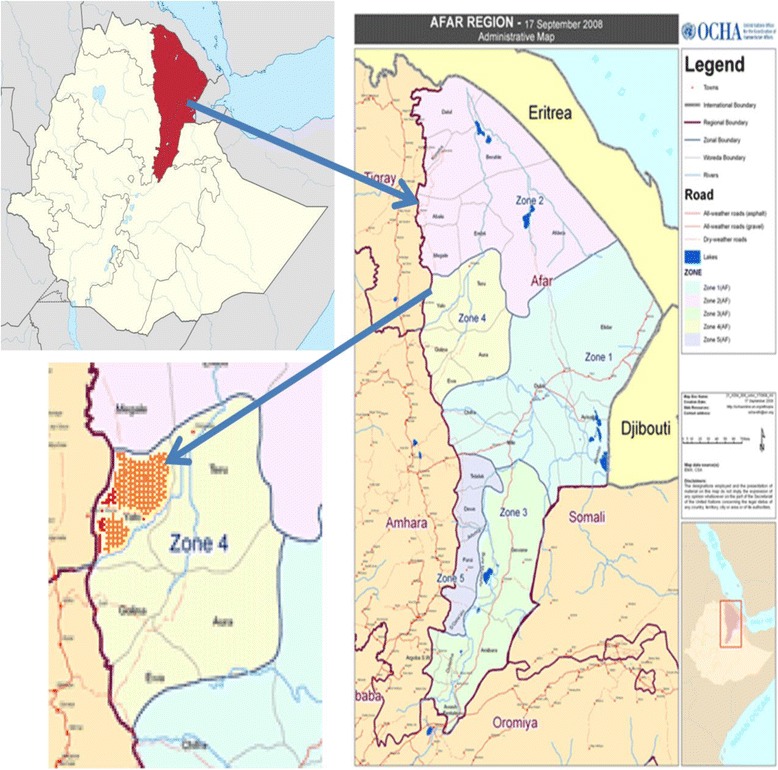
Study area. Orange tinted part shows Yalo Woreda in Afar Regional State
The population of Yalo Woreda, based on 2006 National census, was 54,263 in which 24,418 were female, 29,845 were males, 46,511 were rural, and 7752 were urban dwellers. The majority of the population (95%) is pastoralists, and 5% are semi-pastoralists [24]. The top ten causes of morbidity in Yalo Woreda are malaria, non-bloody diarrhea, pneumonia, lung and acute upper respiratory tract infection, acute febrile illness, urinary tract infection, bloody diarrhea, infection of the skin and subcutaneous tissue, dyspepsia and severe malnutrition [25]. In Yalo Woreda, there are 2220 cattle, 20,190 sheep, 73,389 goats, 14,819 camels and 2733 equine. The top ten veterinary important diseases are PPR, pox, pasteurellosis, CCPP, external parasite, internal parasite, ORF, foot rot, salmonellosis, and brucellosis [26].
Selection of informants and collection of data
The informants were selected with the assistance of elders, and Kebele Administrative Officers. One hundred and sixty informants, 20 from each kebele, were chosen from eight kebeles using purposive sampling. Thirty-seven were females, and 123 were males. The purpose of the study was briefed to the informant, elders and Kebele Administrators to get their consent before collection of data. After receiving their informed consent, ethnobotanical data were collected using semi-structured interview, observations, field visits, and group discussion with the assistance of a native translator. The data collected were the type of diseases treated, the name of plants used for treatment, parts used, methods of preparation and dosage. The information gathered on edible plants were the name of edible plants, parts used as a food source, and seasons or availability of an edible part, and time of consumption [27].
Collections of plant specimens and identifications
The voucher plant specimens were collected from Yalo Woreda during field walks with the informants, and initial identification was conducted on the site. The specimens of plants were pressed and taken to Aklilu Lemma Institute of Pathology for identification. The specimens were further identified by an expert at National Herbarium, Addis Ababa University by using Flora of Eretria and Ethiopia and comparing with herbaria samples and deposited in National Herbarium of Addis Ababa University.
Data analysis
A descriptive statistics, percentages, and frequency were used to analyze ethnobotanical data with Microsoft Excel 2007. Statistical test; one-way analysis of variance was performed with SPSS Advanced Statistics 20.0 to compare knowledge of male and female; among age groups, and kebeles.
Informant consensus factor (ICF), fidelity level (FL) and preference ranking
The diseases and remedies reported were grouped into ten categories based on the top ten diseases in the Woreda. The categories were acute febrile illness and malaria; external injury, eye, ear nose, and mouth infections; gastrointestinal disease; impotence; internal parasites; liver infection; respiratory and lung infection; skin and subcutaneous tissue infection; swellings and cancer; and urinary tract infection. The informant consensus factor (ICF) was calculated to determine the agreements of the informants on each remedy using the formula . Where number of use citations in each category (nur) minus the number of species used (nt), divided by the number of use citations in each category minus one where nur is the number of use citations and nt is the number of species used [28].
Fidelity Level (FL) was calculated to determine the percentage of informants reported the uses of a medicinal plant as a remedy for the same major ailment using the formula . Where Ip is the number of informants who independently indicated the use of a species for the same major ailment and Iu the total number of informants who mentioned the plant for any major ailment [29].
Preference ranking on plants that were reported by 15 and above informants that were used as a treatment for multiple diseases was conducted. Eight informants, one from each Kebele based on the number of medicinal plants reported by each informant, were selected to rank the plants according to their preference [27]. The informants were briefed on the marking of the plants that the most preferred was give the highest points (10) and least preferred was given the lowest point (1). Ten small plots labeled with one to ten was made, and each respondent was asked to put the plants in each plot. The mark given for each plant was recorded accordingly.
Ethical consideration
Institute Review Board of Aklilu Lemma Institute of Pathobiology, Addis Ababa University, reviewed and ethically approved the study. The Yalo Woreda Administrators were enlightened about the importance of the documentation of medicinal and edible plants in the Woreda before getting their permission to conduct an ethnobotanical survey in each Kebele. Likewise, Kebele Officers, elders, and informants were briefed about the primary objective of the study to enable then to decide whether to participate in the study or not before receiving their consents.
Results
Traditional knowledge
The study revealed the rich knowledge of medicinal plants in Yalo woreda that was indicated by the number and diversity of medicinal plants reported. Informants reported 106 medicinal and edible plants. The age of female informants was from 18 to 70 with a mean age of 39.38 ± 2.31 years and males from 20 to 80 with a mean age of 42.30 ± 1.10 years. The number of plants reported by females was ranging from one to six and males from one to 22. The average number of medicinal plants identified by females (2.03 ± 0.17) was less than male (3.89 ± 0.17), and the difference was significant (p < 0.05). Male parents were the primary source of traditional knowledge (TK) in the study area (Fig. 2). Male informants reported forty-two veterinary importance plants of which females reported only two, Acacia oerfota (Forssk.) Schweinf. as a treatment for goat sickness and B. aegyptiaca as a remedy for cow skin infection and itching. The average number of plants reported by young informants (18 ≤ 39) was 2.31 ± 0.20, old informants (40 ≤ 70) was 3.72 ± 0.18, and the difference was significant (p < 05). The knowledge of informants was no associated with kebeles (informant*kebeles, Eta square = 0.19). The difference among the kebeles in the number of medicinal plants reported by each informant was not significant (p > 0.05).
Fig. 2.
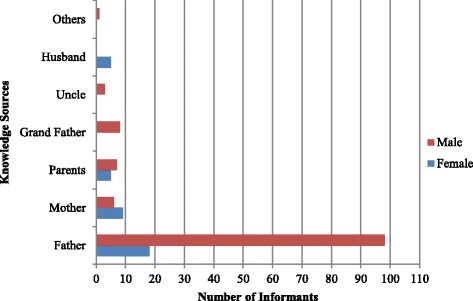
Traditional knowledge sources of medicinal and edible plants
Medicinal plants of public health importance
The informants reported 102 medicinal plants with public health importance distributed into 46 family and 79 genera. Family Fabaceae had 16 Species, followed by Lamiaceae and Solanaceae with six species each, Capparidaceae with five species, Boraginaceae and Loranthaceae with four species each, Acanthaceae, Amaranthaceae, Apocynaceae, Asteraceae, Cucurbitaceae, Euphorbiaceae, Tiliaceae, and Vitaceae with three species each (Table 1; Additional file 1). All the medicinal plants were harvested from natural vegetation.
Table 1.
Medicinal plants used for treatment of human and animal illness in Yalow Woreda, 2016
| Family | Scientific Name [References of other studies] | Disease | Parts | Application (Animal type) | FL | Voucher No. |
|---|---|---|---|---|---|---|
| Acanthaceae | Barleria homoiotrichia C. B. Clarke | Mumps | F | Topical | 0.60 | YA 046 |
| Herpes Zoster | B | Oral, nasal, body wash | ||||
| Justicia schimperiana (Hochst.ex Nees) T. Anders | Somnambulism | F | Oral, body wash | 0.33 | YA 022 | |
| Diphtheria | B | Oral | ||||
| Retained placenta | R | Oral (Camel) | ||||
| Ruellia patula Jacq. | Swelling | L | Oral | 0.67 | YA 021 | |
| Meningitis | WP | Nasal | ||||
| Aizoaceae | Aizoon canariensis L. | Head injury | L | Topical | 1.00 | YA 089 |
| Schizophrenia | WP | Inhaling | ||||
| Trianthema portulacastrum L.* | Hand swelling | L | Topical | 0.67 | YA 014 | |
| Snake Bite | WP | Nasal | ||||
| Herpes Zoster | WP | Nasal | ||||
| Alliaceae | Allium sativum L. | Somnambulism | Fr | Oral, body wash | 0.50 | YA 004 |
| Skin infection | Fr | Topical | ||||
| PPR | Fr | Oral (Cattle) | ||||
| Aloaceae | Aloe trichosantha A. Berger * | Diphtheria | L,S | Oral, body wash | 0.30 | YA 098 |
| Eye sickness | La | Eye-drop | ||||
| Snake bite | R | Oral, nasal, body wash | ||||
| Malaria | L | Oral | ||||
| Breast infection | L,S | Oral, nasal, body wash | ||||
| Delayed placenta | L,R | Oral | ||||
| Black leg/ joint illness | R | Topical (Cow oxen) | ||||
| Brucellosis | L, S | Oral, nasal, ear, body wash (Camel, cow, goat) | ||||
| Amaranthaceae | Aerva javanica (Burm.f.) Schultes | Breast infection | L | Nasal, body wash | 0.31 | YA 077 |
| Epistaxis | R | Oral, nasal | ||||
| Wound | L | Topical | ||||
| STIs | R | Oral, body wash | ||||
| Mastitis and contagious agalactia | L | Oral, nasal, body wash (Goat, cow) | ||||
| PPR | R | Nasal (Goat) | ||||
| Celosia polystachia (Forssk.) C.C. Towns.* | Breast cancer | L | Oral, nasal, topical | 0.47 | YA 103 | |
| Epilepsy | L | Oral | ||||
| Dyspepsia | L | Oral | ||||
| Typhoid | WP | Oral, wash body | ||||
| Jaundice | L | Oral | ||||
| EPTB | L | Oral | ||||
| Lung infection | YP | Oral | ||||
| Mumps | WP | Oral | ||||
| Blackleg | R | Oral, nasal (Cattle) | ||||
| Mastitis and contagious agalactia | L | Oral, nasal, ear, body wash (Camel, cow, goat) | ||||
| PPR | L | Oral (Cattle) | ||||
| Sericocomopsis pallida (S. Moore) Schinz* | Head wound | L | Topical | 1.00 | YA 002 | |
| Anacardiaceae | Rhus natalensis Bernh. ex C. Krauss | Swelling on body | L | Oral | 0.33 | YA 012 |
| Snake bite | R | Oral, tying | ||||
| Topical wound, External body infection | L | Topical insertion (Camel, Cattle) | ||||
| Apiaceae | Ferula communis L. | Somnambulism | F | Oral, body wash | 0.67 | YA 094 |
| Dyspepsia | F | Oral | ||||
| Schizophrenia | L | Body wash | ||||
| PPR | Fr | Oral (Cattle) | ||||
| Apocynaceae | Acokanthera schimperi (A. DC.) Schwein | Kidney infection | R | Oral, topical | 0.50 | YA 027 |
| Eye Infection | L/La | Eye-drop | ||||
| PPR | L | Oral, nasal (Cattle Camel) | ||||
| Pergularia tomentosa L. | Evil Eye | R | Body wash | 0.50 | YA 024 | |
| Snake Bite | L | Oral, nasal, ear | ||||
| Aristolochiaceae | Aristolochia bracteolata Lam. | Diphtheria | WP | Topical | 0.71 | YA 087 |
| Jaundice | WP | Oral | ||||
| Swelling on body | L | Oral, body wash | ||||
| Snake Bite | R | Oral | ||||
| Eye infection | L | Eye-drop | ||||
| Asclepiadaceae | Calotropis procera (Ait.) Ait.f. | Typhoid | FB, L | Oral, Nasal | 0.29 | YA 043 |
| Dyspepsia | F | Oral | ||||
| Breast swelling | L | Nasal, Topical | ||||
| Herpes Zoster | L | Nasal | ||||
| Mouth infection | B | Oral, mouth wash | ||||
| Black leg | YP | Oral, nasal (Cattle) | ||||
| Anthrax | S, L | Oral (Cattle) | ||||
| Mastitis and contagious agalactia | L | Oral, nasal, body wash (Camel, cow) | ||||
| Kanahia laniflora (Forssk.) R.Br.* | Flue | R | Sniffing, nasal | 0.40 | YA 073 | |
| Asthma | L | Inhaling | ||||
| Angina | R | Oral | ||||
| Schizophrenia | WP | Oral, nasal | ||||
| Asteraceae | Kleinia squarrosa Cufod.* | Somnambulism | L | Body wash | 0.50 | YA 020 |
| Eye infection | L | Eye-drop | ||||
| Parthenium hysterophorus L.* | Somnambulism | F | Oral | 1.00 | YA 093 | |
| Xanthium strumarium L. | Dyspepsia | WP | Oral, nasal | 1.00 | YA 030 | |
| Balanitaceae | Balanites aegyptiaca (van Tieghem) Blatter | Infant sickness | R | Oral | 0.43 | YA 095 |
| Breast cancer | L | Oral, nasal, body wash | ||||
| Lung Infection | R,B | Oral, nasal | ||||
| Kola kusil, | L | Oral, topical | ||||
| Mumps | L | Oral, nasal, body wash | ||||
| Dysentery | L.B | Oral | ||||
| Herpes Zoster | B /R | Oral, nasal | ||||
| Devil Disease | B | Oral | ||||
| Brucellosis | L | Oral (Cow, goat) | ||||
| Blackleg | R | Oral (Cow, goat) | ||||
| Trypanosomiasis | R | Oral (Cow, goat) | ||||
| CCPP | R | Oral (Cow, goat) | ||||
| Pastuerollosis | L | Oral (Cattle) | ||||
| Bovine TB | B | Oral, nasal (Cattle) | ||||
| Balanites rotundifolia (van Tiegn.) Blatter | Malaria | L | Oral | 0.43 | YA 008 | |
| Infant sickness | UP | Oral, nasal, ear, washing | ||||
| Mumps | R | Oral, nasal, body wash | ||||
| Flue, cough | L | Nasal, oral | ||||
| Breast cancer | L | Oral, topical | ||||
| ETPB | L | Oral, nasal, topical | ||||
| Jaundice | L,B | Oral | ||||
| Dyspepsia | L,R | Oral | ||||
| Eye injury | R | Eye-drop | ||||
| Bullet injury | B,S | Tying/ topical | ||||
| Herpes Zoster | L | Nasal, body wash | ||||
| Blackleg | R | Nasal (Goat) | ||||
| Mastitis and contagious agalactia | L | Oral (Cow, goat, Camel) | ||||
| Bovine pastuerollosis | L | Oral (Cattle) | ||||
| PPR | R | Nasal (Goat, sheep) | ||||
| Bovine TB | YP | Oral, nasal (Cattle) | ||||
| Boraginaceae | Bourreria orbicularis (Hutch. & E.A. Bruce) Thulin | Breast cancer | L | Oral | 1.00 | YA 065 |
| Brucellosis | L | Oral (Cow, goat) | ||||
| Bovine TB | Fr | Oral, nasal (Cattle) | ||||
| Cordia sinensis Lam. | Arthritis | WP | Topical insertion | 0.67 | YA 072 | |
| Topical wound infection | B | Topical (Cow, goat, Camel) | ||||
| Heliotropium cinerascens Steud. ex A. DC. | Head injury | L | Topical | 0.50 | YA 009 | |
| Arthritis | S | Topical insertion | ||||
| Leprosy | L | Topical | ||||
| Skin infection | L,R | Topical (Cow, goat, Camel) | ||||
| Heliotropium longiflorum (A. DC.) Jaub. & Spach | White on eye | B | Topical | 1.00 | YA 049 | |
| Brassicaceae | Lepidium sativum L. | Somnambulism | F | Oral, body wash | 0.67 | YA 084 |
| Devil Disease | F | Oral | ||||
| Dysentery | F | Oral, nasal | ||||
| Capparidaceae | Boscia coriacea Pax. | Retained Placenta | R | Tying | 0.55 | YA 016 |
| Leprosy | L | Topical | ||||
| Lung Infection | L | Oral | ||||
| Snake Bite | L,F | Oral, topical | ||||
| Cadaba farinosa Forssk. | Eye sickness | L | Fumigation | 0.22 | YA 078 | |
| Lung Infection | L | Sniffing, nasal | ||||
| Mitch/Flue | L | Sniffing, nasal | ||||
| Swelling on body | L | Topical, nasal | ||||
| Head Injury | L | Topical | ||||
| Breast cancer | L | Oral | ||||
| Dyspepsia | L | Oral, nasal | ||||
| Typhoid | L | Oral, nasal | ||||
| Angina Pectoris | L | Oral | ||||
| ETPB | S | Oral | ||||
| Anthrax | R | Oral, nasal | ||||
| Arthritis | R | Tying, topical | ||||
| Impotence | R | Oral, tying | ||||
| Infant sickness | L | Oral, nasal, body wash | ||||
| Mastitis and contagious agalactia | L | Oral, nasal, ear, body wash (Cow, goat) | ||||
| Anthrax | YP | Oral (Oxen) | ||||
| Bovine pastuerollosis | L | Oral (Cattle) | ||||
| Cadaba glandulosa Forssk. | Lung infection | L,S | Oral | 0.33 | YA 034 | |
| Meningitis | L | Oral, body wash | ||||
| Dyspepsia | L | Oral | ||||
| Breast cancer | L | Oral, nasal, topical | ||||
| Snake bite | L,R | Oral, nasal, topical | ||||
| Jaundice | L | Oral, body wash | ||||
| Tonsillitis | L | Oral, body wash | ||||
| Lung infection | L,R | Oral | ||||
| Typhoid | L | Oral, nasal | ||||
| Swelling on skin | L | Oral, topical | ||||
| Bovine pastuerollosis | L | Oral (Cattle) | ||||
| Cadaba rotundifolia Forssk | Arthritis | S | Topical | 0.19 | YA 003 | |
| Eye sickness | L | Fumigation | ||||
| Arthritis | S | Topical insertion | ||||
| Tonsillitis | L | Oral, nasal | ||||
| Flue/Mitch | L | Inhaling | ||||
| Retained Placenta | R | Oral | ||||
| Broken head | L | Topical insertion | ||||
| Snake Bite | L | Oral | ||||
| Retained Placenta | R | Oral, nasal (Camel, Cattle) | ||||
| External parasite | R | Topical (Cow, goat, sheep) | ||||
| Brucellosis | WP | Oral (Goat, camel, cow) | ||||
| ORF | UP | Oral (Goat, sheep) | ||||
| CCPP | WP | Oral (Goat) | ||||
| Bloating | R | Oral (Cattle) | ||||
| Bovine TB | L | Oral, nasal (Cattle) | ||||
| Capparis decidua (Forssk.) Edgew. | Anthrax | S | Oral (Cattle) | 1.00 | YA 085 | |
| Caryophyllaceae | Silene macrosolen Steud. ex A. Rich.* | Breast cancer | L | Oral | 0.50 | YA 104 |
| Diphtheria | L | Nasal | ||||
| Brucellosis | L | Oral (Cow, goat) | ||||
| Convolvulaceae | Seddera bagshawei Rendle | Impotence | R | Nasal | 0.40 | YA 050 |
| Swelling | WP | Oral | ||||
| Snake bite | L | Oral, nasal, body wash | ||||
| Seddera hirsute Dammer ex Hall. f. | Malaria | L | Oral, nasal, body wash | 0.40 | YA 055 | |
| Snake bite | S | Oral | ||||
| Malaria | WP | Oral | ||||
| Asthma | WP | Oral | ||||
| Impotence | WP | Oral | ||||
| Somnambulism | WP | Inhaling | ||||
| Cucurbitaceae | Citrullus colocynthis (L.) Schrad.* | Schizophrenia | L | Oral | 0.50 | YA 026 |
| Wart | S | Topical | ||||
| Citrullus lanatus (Thunb.) Matsum. & Nakai * | Mastitis and contagious agalactia | L | Nasal, body wash (Goat, camel, cow) | 1.00 | YA 025 | |
| Cucumis prophetarum L. | Swelling on body | WP | Oral | 0.38 | YA 028 | |
| Unable to Urinate | WP | Oral | ||||
| Eye injury | UP | Eye-drop | ||||
| Devil Disease | YB | Oral, nasal, wash body | ||||
| Skin infection | L | Oral, nasal (Cattle) | ||||
| Euphorbiaceae | Acalypha fruticosa Forssk. | Eye sickness | L | Fumigation | 0.15 | YA 086 |
| Tonsillitis | L | Oral, nasal | ||||
| Lung Infection | L | Inhaling | ||||
| Infant sickness | L | Oral, nasal, ear | ||||
| Breast cancer | L | Oral, nasal, topical | ||||
| Kola kusil | L | Oral, topical | ||||
| Epilepsy | L | Oral | ||||
| ETPB | L | Oral, wash body | ||||
| Bone breakage | L | Tying/topical | ||||
| Dyspepsia | L | Oral, nasal | ||||
| Herpes Zoster | L | Oral, nasal | ||||
| Schizophrenia | L | Oral | ||||
| Blackleg | L | Oral, nasal (Camel, cattle, goat) | ||||
| Bovine pasteurellosis | L | Nasal, oral (Cattle) | ||||
| Anthrax | L | Nasal, oral (Camel, cattle, goat) | ||||
| CCPP | L | Oral, nasal (Camel, cattle, goat) | ||||
| Bone breakage/ fractures | L | Topical (cattle, goat) | ||||
| Brucellosis | L | Oral (Cow, goat) | ||||
| Pastuerollosis | L | Oral (Cattle) | ||||
| PPR | L | Oral (Cattle) | ||||
| Acalypha indica L. | Malaria, chill | WP | Oral | 0.50 | YA 019 | |
| Snake bite | WP | Oral, nasal, body wash | ||||
| Jaundice | L | Oral | ||||
| Dyspepsia | L | Oral, nasal | ||||
| Breast infection | L | Oral, nasal, ear | ||||
| Lung Infection | L | Oral | ||||
| Herpes Zoster | L | Oral, nasal | ||||
| Snake Bite | L | Oral, nasal (Cow, camel, goat) | ||||
| Brucellosis | L | Oral, nasal, ear, body wash (Cow, camel, goat) | ||||
| PPR | L | Oral (cattle) | ||||
| Euphorbia triaculeata Forssk. | Jaundice | L | Nasal, wash body | 0.67 | YA 064 | |
| STIs | SR | Oral | ||||
| Dyspepsia | L, La | Oral | ||||
| Dysentery | L | Nasal, oral (Goat) | ||||
| Orf | L | Oral, nasal (Goat) | ||||
| Fabaceae | Acacia ehrenbergiana Hayne | Dyspepsia | B | Oral | 1.00 | YA 074 |
| Acacia mellifera (M. Vahl) Benth. | Flue | L/B | Sniffing, Oral | 0.47 | YA 075 | |
| Fire-burn | S | Topical | ||||
| Head/ bullet Injury | B,S | Tying, topical | ||||
| Eye injury | L | Eye-drop | ||||
| EPTB | L | Oral | ||||
| Birth labour | YB | Oral, body wash | ||||
| External infection | S | Topical (camel) | ||||
| PPR | L | Eye-drop (cattle) | ||||
| Acacia nilotica (L.) | Retained placenta | L,R | Oral, nasal | 0.75 | YA 041 | |
| Broken head | Br | Topical | ||||
| Acacia oerfota (Forssk.) Schweinf. | Arthritis | S,F | Topical | 0.35 | YA 045 | |
| Diphtheria | L | Oral, nasal, body wash | ||||
| STIs | R, B | Oral, body wash | ||||
| Breast cancer | L | Eye, nasal, topical | ||||
| Dyspepsia | L | Nasal, body wash | ||||
| Flue, coughing | B | Oral | ||||
| Devil Disease | R,L | Oral, nasal, body wash | ||||
| Scabies | L | Topical | ||||
| Sheep and Goat pox | L | Oral (Sheep, goat) | ||||
| Mastitis and contagious agalactia | L | Nasal, body wash (cow, goat, camel) | ||||
| Bovine TB | R | Oral, nasal (cattle) | ||||
| Acacia senegal (L.) Wild | Mumps | L | Topical, nasal | 0.67 | YA 091 | |
| Eye injury | B | Eye-drop | ||||
| Impotence | R | Oral, topical | ||||
| Acacia seyal Del. | Intestinal parasite | R | Oral | 0.67 | YA 039 | |
| Jaundice | L | Oral | ||||
| Acacia tortilis (Forssk.) Hayne. | External injury | L | Topical | 0.50 | YA 035 | |
| Infant sickness | L | Body wash | ||||
| Breast cancer | L | Oral. nasal, topical | ||||
| Brucellosis | L | Oral (Cow, goat) | ||||
| Dichrostachys cinerea (L.) Wight et Am. | Skin bleaching (cancer) | R | Oral | 0.67 | YA 037 | |
| Foot and mouth | B | Topical insertion (Cattle, goat, sheep) | ||||
| Indigofera articulata Gouan | Jaundice | R | Oral | 0.25 | YA 015 | |
| Epilepsy | L,R | Oral | ||||
| Fire burn | L | Topical | ||||
| Dyspepsia | L,S,R | Oral | ||||
| Epistaxis | L,R | Nasal, oral | ||||
| Snake Bite | R | Oral | ||||
| Swelling on body | L | Oral | ||||
| Brucellosis | L | Oral (Cow, goat) | ||||
| Indigofera oblongifolia Forsk. | Diphtheria | UP | Oral, nasal, ear, body wash | 0.45 | YA 013 | |
| Typhoid | L,S | Oral | ||||
| Herpes Zoster | R | Oral, ear, mouth wash | ||||
| Scorpion bite | Root | Oral, tying | ||||
| Devil illness | WP | Body wash | ||||
| Lung infection | L,R | Oral | ||||
| Dysentery | L,R | Oral | ||||
| Breast cancer | Leaf | Oral and body wash | ||||
| Angina | R | Oral | ||||
| Foot and mouth | GP | Topical insertion (Cattle) | ||||
| Pastuerollosis | L | Oral (Cattle) | ||||
| PPR | L | Oral (Cattle) | ||||
| Indigofera spicata Forsk. | Jaundice | R | Nasal, body wash | 1.00 | YA 070 | |
| Parkinsonia scioana (Chiov.) Brenan | Broken bone | B,R | Tying, topical | 0.67 | YA 081 | |
| Dyspepsia | B | Oral | ||||
| Senna alexandrina Mill. | Circumcise infection | La | Topical | 0.30 | YA 082 | |
| Dyspepsia | WP | Oral | ||||
| Infant sickness | L | Nasal | ||||
| Snake bite | L | Oral, nasal, topical | ||||
| Devil illness | L | Body wash | ||||
| Jaundice | B | Oral | ||||
| External injury | L | Topical | ||||
| Swelling on body | L | Topical | ||||
| Senna italica Mill. | Breast cancer | L | Oral, nasal, body wash | 0.50 | YA 083 | |
| Devil illness | L | Body wash | ||||
| Mumps | R,L | Oral, nasal | ||||
| Dyspepsia | L | Oral, nasal | ||||
| Retained placenta | S | Oral (Camel) | ||||
| Tamarindus indica L. | Lung infection | B | Oral, nasal | 0.50 | YA 063 | |
| Typhoid | B | Oral | ||||
| Trigonella foenum-graecum L.* | Epistaxis | R | Nasal | 0.50 | YA 017 | |
| Infant Sickness | S | Body wash | ||||
| Lamiaceae | Becium filamentosum (Forssk.) | Malaria | L | Oral | 0.55 | YA 033 |
| Lung Infection | L,S | Oral | ||||
| Dyspepsia | L | Oral | ||||
| Somnambulism | L | Oral, wash body | ||||
| Syphilis | F | Oral, nasal | ||||
| Birth labour | Br | Wash body | ||||
| Eye infection | L | Topical | ||||
| PPR | L | Oral (Cattle) | ||||
| Ocimum basilicum L.* | Internal parasites | L | Oral | 0.50 | YA 106 | |
| Swelling on skin | WP | Topical | ||||
| Ocimum spicatum Defl.* | Schizophrenia | R | Oral, nasal | 0.67 | YA 018 | |
| Snake Bite | R | Oral | ||||
| Ocimum urticifolium Roth. | Infant dysentery | L | Oral, nasal, body wash | 0.50 | YA 001 | |
| Diphtheria | WP | Oral, nasal, body wash | ||||
| Malaria | WP | Oral, nasal, body wash | ||||
| Dyspepsia | UP | Oral | ||||
| Herpes Zoster | L | Nasal | ||||
| Orthosiphon pallidus Royle ex Benth.* | Diphtheria | L | Oral, nasal, body wash | 1.00 | YA 101 | |
| Thymus schimperi Ronniger* | Snake bite | WP | Oral, body wash | 0.50 | YA 054 | |
| Devil Disease | S | Oral, body wash | ||||
| Internal parasites | R | Oral | ||||
| Loranthaceae | Oncocalyx glabratus (Engl.) M. Gilbert* | Bullet injury | S,L | Topical | 1.00 | YA 105 |
| Oncocalyx schimperi (A. Rich.) M. G. Gilbert | Jaundice | L | Oral | 0.50 | YA 029 | |
| Plicosepalus robustus Wiens & Polhill* | Herpes Zoster | WP | Oral, nasal, body wash | 0.75 | YA 076 | |
| Tapinanthus globiferus (A. Rich.) Tieghem* | Dyspepsia | L | Oral, ear, mouth wash | 0.50 | YA 079 | |
| Impotence | L | Oral | ||||
| Lythraceae | Lawsonia inermis L.* | Elephantiasis | L | Tying, topical | 1.00 | YA 059 |
| Malvaceae | Abutilon figarianum Guill. & Perro | Eye infection | R | Fumigation | 0.50 | YA 052 |
| Fire, swelling | L | Topical, oral | ||||
| Flue | L | Chewing, sniffing | ||||
| Hibiscus vitifolius L. | Angina Pectoris | R | Tying, topical | 1.00 | YA 047 | |
| Menispermaceae | Cocculus pendulus (J. R. & G. Forst) Diels* | Somnambulism | L | Oral, wash body | 0.29 | YA 053 |
| Retained Placenta | L | Oral | ||||
| Elephantiasis | S | Topical insertion | ||||
| Snake Bite | R | Oral | ||||
| Breast infection | R | Topical | ||||
| Moraceae | Dorstenia barnimiana Schweinf.* | Schizophrenia | WP | Inhaling | 1.00 | YA 088 |
| Moringaceae | Moringa oleifera Lam. | Snake Bite | R,B | Oral, tying | 1.00 | YA 032 |
| Nyctaginaceae | Commicarpus helenae (J.A. Schultes) Meikle | Breast infection | L | Nasal, body | 0.50 | YA 066 |
| Vomiting | L | Oral | ||||
| Elephantiasis | L | Topical | ||||
| Typhoid | WP | Oral, nasal | ||||
| Herpes Zoster | R | Nasal | ||||
| Mastitis and contagious agalactia | L | Nasal, body wash (Cow, goat, Camel) | ||||
| Commicarpus squarrosus (Heimerl) Standl.* | Trypanosomiasis | S | Nasal, ear, body wash (Camel) | 1.00 | YA 056 | |
| Oleaceae | Olea europaea L. subsp. cuspidata (Wall.ex G. Don) Cif. | Snake Bite | Stem | Oral, topical | 1.00 | YA 102 |
| Plumbaginaceae | Plumbago zeylanica L. | Meningitis | L | Oral, nasal | 0.75 | YA 006 |
| Scabies | L,R | Topical | ||||
| Skin infection | L | Oral, topical | ||||
| Poaceae | Cymbopogon commutatus (Steud.) Stapf | Jaundice | Tu | Oral, wash body | 0.50 | YA 005 |
| Eye Infection | L | Eye-drop | ||||
| Polygalacea | Polygala obtusissima Hochst. Ex Chod. | Flue | WP | Inhaling | 0.50 | YA 051 |
| Dyspepsia | R | Oral | ||||
| Asthma | R | Oral | ||||
| Ranunculaceae | Nigella sativa L.* | Somnambulism | S | Oral, body wash | 1.00 | YA 096 |
| Rhamnaceae | Ziziphus mauritiana Lam. | Retained placenta | L | Oral | 0.50 | YA 068 |
| Breast cancer | L | Oral | ||||
| Brucellosis | L | Oral (Cow, goat) | ||||
| Ziziphus spina-christi (L.) Desf. | Retained placenta | L | Oral | 0.43 | YA 069 | |
| Snake bite | YB | Oral | ||||
| Angina Pectoris | Root | Oral | ||||
| Dyspepsia | YB | Oral | ||||
| Rutaceae | Citrus lemon (L.) Bunn.f. | Somnambulism | F | Oral, wash body | 1.00 | YA 071 |
| Salvadoraceae | Dobera glabra (Forssk.) Poir. | Head Wound | B,L | Topical | 0.43 | YA 042 |
| ETPB | L | Oral | ||||
| Anthrax | L | Oral (Cow, oxen) | ||||
| Bloating | R | Oral (Cattle) | ||||
| Blackleg | R,L | Oral (Cattle) | ||||
| Skin infection | L | Topical (Cattle, camel) | ||||
| Sapotaceae | Mimusops kummel Bruce A. DC. | Dyspepsia | R | Oral | 1.00 | YA 038 |
| Selaginellaceae | Selaginella kraussiana (Kunze) A.Braun* | Fire burn | WP | Topical | 0.67 | YA 067 |
| Anthrax | UP | Nasal, oral (cattle, goat, sheep) | ||||
| Solanaceae | Capsicum annuum L. | Arthritis | S | Topical insertion | 1.00 | YA 060 |
| Anthrax | S | Oral (Cattle) | ||||
| Capsicum frutescens L. | Pasteurellosis | Fr | Nasal, oral (Camel) | 0.50 | YA 061 | |
| Flue | Fr | Nasal, oral (Camel) | ||||
| Solanum incanum L. | Schizophrenia | UP | Oral, inhaling | 0.50 | YA 100 | |
| Blackleg | R | Oral, nasal, topical (Cattle) | ||||
| CCPP | R | Oral, nasal (Goat) | ||||
| Lung infection | R | Oral, nasal (Camel) | ||||
| Solanum marginatum L. f. | Schizophrenia | L,R | Oral | 0.29 | YA 097 | |
| Mumps | L | Oral | ||||
| Meningitis | L | Oral | ||||
| Head injury | L | Topical | ||||
| Dyspepsia | L | Oral | ||||
| Pastuerollosis | L | Oral (Cattle) | ||||
| Solanum somalense Franchet. | Fire Burn | UP | Topical | 0.67 | YA 036 | |
| Typhoid | UP | Nasal | ||||
| Withania somnifera (L.) Dunal | Typhoid | R | Oral | 0.57 | YA 040 | |
| Evil eye | R | Oral, inhaling | ||||
| Swelling on skin | L | Oral, topical | ||||
| ETPB | L | Oral | ||||
| Sterculiaceae | Sterculia africana (Lour.) Fiori* | Infant sickness | L | Oral | 0.50 | YA 090 |
| Swelling on skin | Leaf | Topical | ||||
| Tiliaceae | Grewia erythraea Schweinf. | Head wound | S,B | Topical | 0.36 | YA 062 |
| Flue | L, B | Inhaling | ||||
| Typhoid | L | Oral | ||||
| Broken bone | R | Topical | ||||
| Dyspepsia | L,S,B | Oral, nasal | ||||
| Arthritis | R | Topical insertion | ||||
| Wart | B | Topical | ||||
| Infant Sickness | L,R | Nasal, body wash | ||||
| Leprosy | R | Topical | ||||
| Grewia villosa | Broken bone | R | Tying, topical | 0.40 | YA 048 | |
| Impotence | R | Oral, body wash | ||||
| Jaundice | WP | Oral, nasal | ||||
| Foot and mouth | S | Nasal, oral (Cattle, goat, sheep) | ||||
| Verbenaceae | Premna oligotricha Baker* | Retained placenta | L | Oral | 1.00 | YA 023 |
| Priva curtisiae Kobuski* | Typhoid, Mitch | L | Oral, nasal | 1.00 | YA 099 | |
| Vitaceae | Cissus quadrangularis L. | Leprosy | YB | Oral, topical | 0.33 | YA 044 |
| ETPB, lung infection | YB | Oral, topical | ||||
| Swelling on neck, chest | YP | Oral, nasal (Cattle) | ||||
| Cissus rotundifolia (Forssk.) Vahl | Devil Disease | RL | Inhaling | 0.50 | YA 080 | |
| Cyphostemma burgeri Vollesen* | Snake Bite | R | Oral | 0.50 | YA 007 | |
| Hand swelling | L | Topical | ||||
| Zygophyllaceae | Fagonia paulayana Wagner & Vierh.* | Infant sickness | UP | Oral, Nasal | 1.00 | YA 031 |
| Fagonia schweinfurthii Hadidi | Tonsillitis | R | Oral | 0.50 | YA 010 | |
| Jaundice | WP | Oral, body wash | ||||
| Infant sickness | L | Oral, body wash | ||||
| Lung infection | R | Oral, body wash | ||||
| Mastitis and contagious agalactia | WP | Nasal, body wash (Cow, goat, camel) |
B bark, C climber, F flower, Fr fruit, L leaf, La latex, R root, S stem, Br branch, UP upper part, WP whole plant, YP young plant
*new reports in Afar region
Ethnoveterinary medicinal plants
Thirty-nine of the plant species were used to treat human as well as livestock diseases, but Capparis decidua (Forssk.) Edgew., Capsicum frutescens L., and Commicarpus squarrosus (Heimerl) Standl. were only used in the treatment of livestock. The plants were distributed into 21 Family and 42 genera. Fabaceae was represented by six species followed by Capparidaceae with four species, Boraginaceae, Euphorbiaceae, Solanaceae with three species each, and Aloaceae, Amaranthaceae, Apocynaceae, Balanitaceae, Cucurbitaceae, Nyctaginaceae with two species each and the rest with one species each (Table 1; Additional file 2).
Habit and parts of medicinal plants
The majority of medicinal plants were shrubs (44%), followed by herbs (28%), trees (21%), and climbers (7%). The leaf (52.94%) was used in the majority of the remedy preparations followed by root (16.99%), whole plant (6.86%), bark (5.07%), young branch (4.25%), fruit (3.27%) and stem (3.27%) (Fig. 2). The remedies were prepared from fresh (95%), dry (4%) and either fresh or dry (1%) parts. Few remedy preparation from seed (67%), whole plant (19%), fruit (15%), and bark (13%) were from dried parts whereas the majority of the remedies were prepared from fresh plant parts (Fig. 3).
Fig. 3.
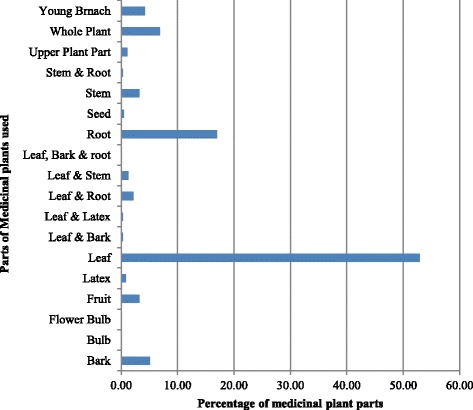
Parts of plants used for the preparation of remedies
Preparation, dosage, and mode of treatment
The majority of the treatments were prepared from a single plant (80%) and some from a mixture of multiple plants (20%). The health conditions treated with a mixture of plants were coughing blood through mouth and nostrils; knee sickness and swelling; breast swelling and infection; infant illness and fever; sleepwalking; epilepsy; devil illness; sudden illness, fever, dysentery, and vomiting; witchcraft disease; bovine brucellosis; and pasteurellosis. Forty-eight plants were used in multiple plant preparation. The most popular plants in the preparations were A. fruticosa (40%), A. tortilis (25%), B. rotundifolia (25%), Indigofera oblongifolia Forsk. (17%), C. farinosa (15%), Celosia polystachia (Forssk.) C.C. Towns. (13%), Becium filamentosum (Forssk.) Chiov. (10%) and C. rotundifolia (10%) (Table 1; Aditional Files 1 and 2).
The primary methods of preparation of remedies were crushing and pounding. The crushing and pounding were done using two stones one flat shaped and the other oval or spherical shaped to fit into the hands. The diluents were water, the blood of a black goat, and milk of goat or camel. The oral (68%) was the major route of administration of treatments followed by topical (16%), nasal (10%), eye (3%) and body wash (2%) (Fig. 4). The filtrate was applied orally, through nostril, and as an ear and eye drop. The residue was used for body washing. Camel’s milk was given as an antidote for remedies that upset or cause irritation of the stomach and honey was added to those preparations with a bitter taste. Treatments applied topically were charred, ground and the powder was mixed with butter to make a paste. The parts of medicinal plants that were inserted into a cut made in the knee, breast, or swollen body parts were mixed with salt, pepper, or butter. Fresh plants were chewed, and the juice was swallowed before a meal for a day. The remedies for some diseases were boiled in the evening, and the filtrate was taken before breakfast in the morning. Some diseases were treated with a combination of routes in both human and livestock treatments (Table 1; Additional files 1 & 2).
Fig. 4.
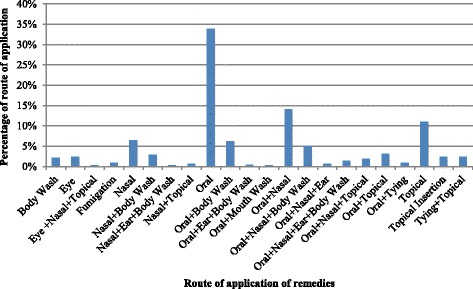
Routes of application of treatments
The dosages taken orally were measured using a small coffee cup (~5 ml), glass (~20 ml), and tin can (~50 ml) for humans and large tin can (~3lt) for animals. The coffee cup was used to provide remedies to a child and tin cans for adults based on the symptoms and physical condition of the patients. The medication applied as eyedrops, eardrops and through nostrils was five to ten drops while in the treatment of animals thin bamboo stem about ten centimeters long was used. The application of remedies for flu, sleepwalking, and devil illness was inhaling the smoke, fume, and steam the patient is covered by overcoat/blanket or sniffing of crushed or powdered fresh plant parts wrapped with locally weaved close. Sniffing was not administered to children under age of five (Additional files 1 and 2). The majority of the treatments were given only once in the morning as a single dose or three times in a day or for two to seven days. However, some treatments were given only once for all animals as a vaccine to prevent and stop the transmission of the contagious disease such as CBPP, anthrax, blackleg, and bovine pasteurellosis (Additional file 2).
Fidelity value and informants consensus factor
The medicinal plants reported by few informants (one to two) or that were used only as a treatment for an ailment had FL value of 1.00. Dorstenia barnimiana Schweinf. was used as a treatment for schizophrenia, and Priva curtisiae Kobuski as a treatment for typhoid/typhus, headache, and fever and had FL value of 1.00 (Table 1). On the other hand, medicinal plants that were used to treat a variety of ailments had lower FL values. Indigofera articulata (0.25), C. farinosa (0.22), C. rotundifolia (0.19), and A. fruticosa (0.15) were used to treat diseases ranging from human to livestock and were reported by more than 20 informants.
The informant consensus factor was calculated by pulling to gather the human and animal ailments into ten categories. The values obtained were in agreement with the top ten causes of morbidity and mortality in the Yalo Woreda. Malaria and febrile diseases had the highest (ICF = 0.69) value followed by internal and liver infection (0.67), and gastrointestinal disease and internal parasite (0.62) (Table 2).
Table 2.
Informant consensus value of category of diseases of public health and livestock importance in Yalow Woreda
| Category | Species | (%) All Species | Use citations | (%) All use citations | ICF |
|---|---|---|---|---|---|
| Acute febrile illness and malaria | 32 | 31% | 102 | 18% | 0.69 |
| Internal and liver infection | 55 | 54% | 166 | 29% | 0.67 |
| Gastrointestinal disease, internal parasite | 50 | 49% | 129 | 23% | 0.62 |
| Swellings and cancer | 45 | 44% | 102 | 18% | 0.56 |
| Flue, headache | 25 | 25% | 54 | 10% | 0.55 |
| Eye, ear nose, and mouth | 35 | 34% | 63 | 11% | 0.45 |
| Respiratory and lung infection | 26 | 25% | 41 | 7% | 0.38 |
| External injury and external parasite | 28 | 27% | 44 | 8% | 0.37 |
| Skin and subcutaneous tissue infection | 30 | 29% | 43 | 8% | 0.31 |
| Snake and scorpion bite | 20 | 20% | 28 | 5% | 0.30 |
| Devil disease, schizophrenia, epilepsy | 25 | 25% | 34 | 6% | 0.27 |
| Birth related and urinary tract infection. | 18 | 18% | 23 | 4% | 0.23 |
| Impotence | 6 | 6% | 7 | 1% | 0.17 |
Preference ranking
The preference ranking of medicinal plants reported by 15 and more informants and used as a remedy for multiple diseases is shown in Table 3. The medicinal plants were ranked based on their healing potential of a disease. Balanites rotundifolia and A. fruticosa were used as remedies for diseases such as breast cancer, dyspepsia, epilepsy, ETPB, eye sickness, herpes zoster, infant disease, jaundice, lung infection, and malaria. Cadaba glandulosa Forssk. and Celosia polystachia (Forssk.) C.C. Townsend had the lowest two ranks and used as a treatment for stomach ache, bloody dysentery, fever and sudden illness. (Additional files 1 and 2).
Table 3.
Preference ranking of medicinal plants predominantly cited as remedies for humans and animal in Yalo Woreda
| Plants used in treatment of multiple diseases | R1 | R2 | R3 | R4 | R5 | R6 | R7 | R8 | Total | Rank |
|---|---|---|---|---|---|---|---|---|---|---|
| Acacia mellifera | 6 | 8 | 6 | 7 | 7 | 8 | 7 | 8 | 57 | 9 |
| Acacia oerfota | 7 | 7 | 8 | 6 | 8 | 7 | 8 | 7 | 58 | 8 |
| Acalypha fruticosa | 9 | 9 | 8 | 9 | 9 | 8 | 9 | 8 | 69 | 2 |
| Acalypha indica | 8 | 8 | 9 | 8 | 8 | 9 | 8 | 9 | 67 | 3 |
| Balanites aegyptiaca | 8 | 7 | 8 | 9 | 8 | 8 | 7 | 8 | 63 | 5 |
| Balanites rotundifolia | 9 | 8 | 9 | 9 | 8 | 9 | 9 | 9 | 70 | 1 |
| Cadaba farinosa | 7 | 7 | 8 | 9 | 8 | 8 | 8 | 9 | 64 | 4 |
| Cadaba glandulosa | 7 | 6 | 8 | 7 | 6 | 6 | 7 | 8 | 55 | 10 |
| Cadaba rotundifolia | 8 | 7 | 8 | 8 | 8 | 7 | 8 | 7 | 61 | 7 |
| Celosia polystachia | 6 | 7 | 7 | 8 | 7 | 6 | 6 | 7 | 54 | 11 |
| Indigofera oblongifolia | 7 | 6 | 7 | 8 | 9 | 7 | 9 | 9 | 62 | 6 |
Edible plants and duration of gathering
Informants reported 16 edible plants and 56% of these plant species were trees and 44% were shrubs. Fourteen of the plants were nutraceutical; Rosa abyssinica R. Br. and Ximenia americana L. were used only as edible plants. All edible fruits were eaten raw (Table 4). The duration of gathering and consumption were dependent on the availability of edible parts and seasons. Boscia coriacea Pax., Carissa spinarum L., Dobera glabra (Forssk.) Poir., Mimusops kummel A. DC., R. abyssinica, Tamarindus indica L., and Z. spina-christi were gathered in Gilal as food supplements. Balanites aegyptiaca, B. rotundifolia, and Cordia sinensis Lam. were collected in Hagay as an alternative food. Grewia bicolor Juss., Grewia erythraea Schweinf., Rhus natalensis Krauss, Ruellia patula Jacq., and X. americana were gathered in Sugum-Karma and used as dietary supplements Balanites aegyptiaca, B. rotundifolia, C.sinensis, and D. glabra were sold in open markets and had economic importance.
Table 4.
Edible plants consumed by Afar people in Yalow Woreda
| Voucher Number | Family | Scientific Name (Citations) | Habit | Local plant name | Mode of consumption |
|---|---|---|---|---|---|
| YA 021 | Acanthaceae | Ruellia patula Jacq. | Shrub | Boboyta | The outer cover is eaten fresh. It is collected and consumed by herd boys, and it is not stored and has a mild test. |
| YA 012 | Anacardiaceae | Rhus natalensis Krauss | Tree | Dewa/ Sofa | Whole fruit, after trashing using both hands, is eaten fresh. It is sweet and consumed by all age groups. It collected and mostly consumed by herd boys |
| YA 092 | Apocynaceae | Carissa spinarum L. | Shrub | Titita | It has sweet to sour test, collected and consumed by all age groups |
| YA 095 | Balanitaceae | Balanites aegyptiaca (van Tieghem) Blatter | Tree | Udayto | The outer cover is eaten fresh, and the inside is eaten boiled and can be stored. It is collected by housewives, herd boys, and men and consumed by all age groups. It has a mild test and stored for a drought period. |
| YA 008 | Balanitaceae | Balanites rotundifolia (Van Tiegn.) Blatter | Shrub Small tree | Alayto | The outer part is eaten fresh. The internal part is bitter, hence, soaked in water overnight and followed by two to three times washing, boiled and consumed by all age groups. Housewives and herd boys collect and stored for drought period as a food source. It is also consumed fresh by diabetic patients. |
| YA 072 | Boraginaceae | Cordia sinensis Lam. | Tree | Madera/ Ledo | It is collected by boys and housewives. It is sweet as honey and has more fat. It is preferably given to children under five years and women that have given birth. It is eaten before breakfast and dinner. |
| YA 016 | Capparidaceae | Boscia coriacea Pax. | Tree | Homura/ Aytneba | It too sour and only one crushed fruit is taken for smoothening taste by older individuals that take milk as food for a longer period. It is used as medicine to avoid dyspepsia. |
| YA 063 | Fabaceae | Tamarindus indica L. | Tree | Hura | It has a mild taste between sour, and bitter. It is collected by herd boys and housewives and eaten fresh. The whole fruit is chewed, and the seeds are spat. |
| YA 058 | Olacaceae | Ximenia americana L. | Tree | Helelea | It is sweet, succulent fruit collected by herd boys and consumed by all age groups. |
| YA 069 | Rhamnaceae | Ziziphus spina-christi (L.) Desf. | Tree | Kusra | It collected by herd boys and housewives and eaten fresh by all age groups. |
| YA 011 | Rosaceae | Rosa abyssinica Lindley | Shrub | Atim | It is sweet and collected and consumed by all age groups. The whole fruit is eaten fresh, and only seeds are spat. |
| YA 042 | Salvadoraceae | Dobera glabra (Forssk.) Poir. | Shrub | Gasera/ Mudua/ | The outer part is eaten fresh and inner part is taken as food boiled mixed with Alayto during drought season. It collected by housewives and herd boys, stored for drought season, and consumed by all age groups. |
| YA 038 | Sapotaceae | Mimusops kummel A. DC. | Tree | Yelow Eta | Unripe fruit is collected by boys and buried in the soil until it ripens and becomes red. The whole fruit is consumed by all age groups. Unripe fruit is not edible and assumed to be poisonous. |
| YA 057 | Tiliaceae | Grewia bicolor Juss. | Tree | Hebele | It is collected by herd boys, and whole fruit is consumed after the hairy outer part is cleaned. It is sweet and eaten by all age groups |
| YA 062 | Tiliaceae | Grewia erythraea Schweinf. | Shrub | Hidayto | It is sweet fruit collected by herd boys and consumed by all age groups and is not stored |
| YA 048 | Tiliaceae | Grewia villosa Willd. | Shrub | Habeleyta | It is collected by herd boys and consumed fresh by all age groups. |
Discussion
Traditional knowledge and medicinal plants of human and veterinary importance
The number and diversity of medicinal plants reported by informants show the rich traditional knowledge in Yalo Woreda and the number of medicinal plants reported is more than the studies conducted in Afar and neighboring regions [10, 17, 22, 30–34]. The transference of traditional knowledge in the study area is from male parent to their sons since females have low status in the society and do not inherit property on the same basis to the male [4, 6]. The study conducted in Namibia indicated similar practice [35]; the females learn by routine observation whereas the boys are taught by their parents besides regular observation [22, 36–39]. The vertical transference of TK from father to son is a common phenomenon in Ethiopia, Africa, and Asia [17, 22, 35, 40–48]. However, studies conducted on knowledge of medicinal plants in Ankober district, Samburu district, Kenya and in South America show no difference in the average number of plants reported either by female or male respondents [47, 49, 50]. The division of labor in the society has determined the TK difference between female and male. The female informants in Yalo woreda reported only three plants with veterinary importance since the males are the sole livestock herders in the region and responsible for the animals’ wellbeing [37–39, 44]. The ethnoveterinary knowledge in pastoral society is acquired from their parents during grazing that indicates females’ knowledge of ethnoveterinary medicinal plants is less than men, which is similar to results reported by other studies on important ethnoveterinary plant [44, 51–54].
The number of medicinal plants reported in the study area increased with age, and the older informants reported more medicinal plants than the younger individual [36, 50, 52, 55]. Abera [56] has shown in the study conducted, in Ghimbi District, on Oromo people that the young generation is losing the interest in using medicinal plants because of changes induced by development and abandons of rural life. This phenomenon leads to the disappearance of associated traditional knowledge and interrupts transference of knowledge to next generations [16, 35, 47, 57–61]. Similarly, the study conducted, in the semi-arid region of Brazil, has shown that age and income difference had implications on knowledge of informants and correlated to some plants that have an effect on the traditional knowledge of younger generation [40, 50]. The transference of knowledge in the Afar family is similar to most of the pastoral areas where youngsters learn knowledge of medicinal plants from the elders during grazing. A child in Maasai pastoralists’ society in Eastern Africa has to learn and identify grasses and plants with medicinal importance in their area during grazing. The boys are taught in the field and at home, though girls are taught by their mothers and grandmothers only at home [62].
The religious establishments in Mesgid and Rekrek Kebeles and other cultural aspects had no association with traditional knowledge of medicinal plants in Yalo Wereda [63]. Though, Abu-Rabia [64] reported that knowledge of plants of nomadic pastoralists in Middle East countries originated from the sayings of Prophet Muhammad’s on health and illness: ‘The Medicine of the Prophet”. Also, the study conducted around Debre Libanos monastery has shown that the knowledge of the people varies based on the distance from the Monastery since religion is one of the aspects of variation in TK among the different societies in Ethiopia [45, 63, 65–68].
The medicinal plants reported by the people in Yalo Woreda are also reported by ethnobotanical studies conducted in semi-arid and arid regions in Ethiopia. Most of the medicinal plants are drought resistant, and many of them are a member of Acacia-Commiphora Woodland [1, 10, 17, 21, 22, 41, 46, 68]. The medicinal plants were collected from natural vegetation since the majority (95%) of the population is pastoralists, and the rest are urban dwellers without a home garden. In Ethiopia, the majority of the traditional medicines are prepared from plants collected from the wild [9, 53, 69–74]. The culture of conservation of medicinal plants in the home garden is not practiced in many regions of Ethiopia. Conservation of the medicinal plants is a requirement since the recurrent drought imposed by climatic changes has an impact on the natural vegetation. The other threat to the vegetation of the study area is the spread of invasive species such as P. juliflora that are replacing the plants with cultural values and changing vegetation to monotype bushes and forests. The people in Djibouti and Borena pastoralists areas reported a similar scenario where encroachment of invasive plants has resulted in a loss of valuable plants and degradation of the rangeland that indicates the necessity of further additional ethnobotanical studies in Afar region [1, 9, 15–18, 32, 57, 60, 75–78].
The medicinal plants reported in Yalo Woreda are also reported by other studies conducted in Afar and other areas where the Afar people are inhabitants. Bahru et al. [10] reported fourteen plant species and Beche et al. [34] reported ten plant species in the studies conducted around the Awash National Park. Meragiaw [23] reported twelve plant species in a study carried out in Aba’ala Woreda; Seifu et al. [22] reported nine plant species in a study conducted in Chifra District; and Belayneh et al. [41] reported 14 plant species in a study carried out in pastoral and agro-pastoral communities in Erer Valley of Babile Woreda. The survey conducted in the region of Randa, Djibouti reported 46 plant species [17]. The studies commonly reported Acacia mellifera (M. Vahl) Benth., .A. oerfota, .A. tortilis, B. aegyptiaca, Balanites rotundifolia (van Tiegn.) Blatter, Cadaba farinosa Forssk., Cadaba rotundifolia Forssk, Cissus quadrangularis L., Indigofera articulata Gouan, Olea europaea L. subsp. cuspidata (Wall.ex G. Don) Cif., Solanum incanum L., Withania somnifera (L.) Dunal, Ziziphus spina-christi (L.) Desf. The similarity in the naming of plants by the individuals in these study areas indicates similarity in their cultural and traditional practices. Furthermore, the use of the plants in broad geographic regions adds value to the therapeutic potential of the medicinal plants in Yalo Woreda [12, 17, 23, 34, 43, 69]. However, 29 medicinal plants are new reports by Yalo Woreda informants compared to other studies conducted in Afar region, which are used as a treatment for different health conditions in Ethiopia and elsewhere. [10, 14, 16, 32, 35, 41, 47, 48, 50, 56, 60, 62, 66, 69, 71, 76, 78–89]. Nevertheless, some of the plants are not documented in the reviewed ethnobotanical studies in Ethiopia. Citrullus lanatus (Thunb.) Matsum. & Nakai, Cyphostemma burgeri Vollesen, Dorstenia barnimiana Schweinf. that are used as a treatment for various diseases in Yalo Woreda are edible plants in other parts of Ethiopia [81, 90–92]. Fagonia paulayana Wagner & Vierh. used as a remedy for infant sickness in Yalo Woreda has a similar purpose to other Fagonia spp. reported in Pakistan [93, 94]. Plicosepalus robustus Wiens & Polhill is a parasitic plant that grows on Cadaba farinosa Forssk., and used as a treatment for an infection on skin and mouth, and tooth decay has a similar effect as Plicosepalus curviflorus Tiegh. and Plicosepalus acaciae Zucc. [95–97] with high activity against bacterial infections, and Plicosepalus nummulariifolius (Franch.)Wiens& Polhill. used as a treatment to gastritis in Djibouti [17]. Priva curtisiae Kobuski used as a treatment for typhoid, headache, and fever in Yalo Woreda has similar medicinal uses to species within the same genus; Priva cordifolia Druce, Priva flabelliformis (Mold.) R. Fernand and Priva lappulacea (L.) Pers. used as a treatment for different health conditions in Uganda and Martinique [98, 99]. Selaginella kraussiana (Kunze) A.Braun is used to treat sickness related to burning and wound; studies conducted on another species of Selaginella reported as a treatment to wound, anticancer and antimalarial in different parts of the world [100–102].
Fabaceae are major plant species reported as remedies to treat livestock diseases similar to other studies in the country [17,22,34.41,44,58,69,85], but in the study conducted in Ada’ar District, Afar regional state, Asclepiadaceae and Capparidaceae are dominant plant species reported as a treatment to livestock [9]. The ethnoveterinary plants reported in the current study such as A. oerfota, Acalypha fruticosa Forssk., B. aegyptiacus, Calotropis procera (Ait.) Ait.f., C. frutescens, C. quadrangularis and S. incanum. Are utilized by other societies as a treatment for varies type of animal health conditions [9, 13, 17, 20, 22, 25, 35, 41, 44, 51, 55, 71, 77, 79, 81]. Giday and Teklehaymanot [9] reported seventeen plant species in Ada’ar District, Afar Regional State; Gradé [58] reported seventeen plant species in pastoral Karamoja, Northern Uganda; Dharani [103] reported 10 plant species in East Africa and Sori [104] reported ten plant species in Borana Pastoralists, Southern Ethiopia [9, 13, 17, 20, 22, 25, 35, 41, 44, 51, 55, 69, 71, 79, 81]. The number of ethnoveterinary plants reported in Yalo woreda is more than many studies conducted in Ethiopia [30, 53, 55, 60, 70, 72–74, 87, 104–109] even though studies undertaken in some societies reported a higher number of ethnoveterinary plants [9, 43, 77, 104, 110, 111]. It indicates the rich knowledge of ethnoveterinary important plants in the study area since the people are highly dependent on the animals for their living [43, 58, 60, 69, 70, 104]. The Afar people seasonally migrates in search of grazing and water for their animals and utilize plants from the natural vegetation to treat animal’s illness through trial and error that profoundly contributed to the knowledge of individual herders. The plants employed for treating a disease are diverse, which is the outcome of experience gained by the various informants during grazing. The individual herder is responsible for the well-being of the livestock and uses plants found in the grazing area in addition to the knowledge passed from their parents to manage animal health conditions [9, 54, 58, 112].
Most of the medicinal plants used for the preparation of remedies were shrubs and trees that are available throughout the year. The shrubs and trees are dominantly used for the preparation of medications in most sub-arid and arid regions since the plants survive and are available in dry seasons. Trees and shrubs are used in the preparation of medications in pastoralists area such as in Borena pastoralists, 56% of remedies are prepared from trees and shrubs, and in Ada’ar District, Afar Reginal state 67.3% of ethnoveterinary plants are shrubs [9, 34, 41, 43, 48, 68, 72, 113, 120, 123]. In Yalow Woreda, the majority of remedies are prepared from fresh leaves; similar to the reports by most of the ethnobotanical studies conducted in Ethiopia and elsewhere [9,34,35 43 53,60,71,74,76] though some societies in Ethiopia prefer to use root [46, 47, 69, 72, 89, 114] and Karamoja pastoralist uses bark for the preparation of remedies [36, 57, 58, 69, 78]. The uses of the leaf would better protect the plants than roots unless the people considers in using lateral roots than the taproots, which enable the plants to draw water from depth. On the other hand, excessive defoliation could also endanger the regeneration and survival of the plants in semi-arid and arid areas [17, 60]. Fresh plant parts and leaf are predominantly used in traditional treatments in Ethiopia. The use of fresh parts lessens the depletion of ingredients that affects the healing potential of the remedies through drying and storage. The people, when using fresh plants, they assume that ingredients in the plant are not lost through drying and curing potential is more than dried once [35, 41, 46, 76, 77, 115].
The practice of single plant for remedy preparation is common than a combination treatment in many studies conducted in Ethiopia and elsewhere [9, 30, 58] Nevertheless, in some regions such as in Gindeberet district, Western Ethiopia, 94% of the preparations are made from a mixture of multiple plant species [41, 49, 54, 58, 71, 82, 113]. The number of plants in multiple plant treatment ranged from two to ten and administered to disease where single plant preparations effectiveness is low. The people in the area perceived that use of multiple plants in preparation of ethnomedicine adds up the curing potential and confer synergetic effects [58]. On the other hand, the use of multiple plants to treat a disease is an indication of the prevalence and severity of illness in the region [41, 56, 58, 113]. The most popular plants used in multiple plant preparations in Yalo Woreda and other societies are A. fruticosa [53, 104], A. tortilis [20, 54, 64, 81, 115], B. aegyptiaca [19–21, 53, 62, 71, 104], B. rotundifolia [104, 116], Indigofera oblongifolia Forsk. [53, 104], C. farinosa [13, 53, 116], Celosia polystachia (Forssk.) C.C. Towns.), Becium filamentosum (Forssk.) Chiov. [41, 43] and C. rotundifolia [19, 53, 116].
The primary methods of preparation of remedies, crushing and pounding and diluents such as water and milk are similarly reported by other studies in Ethiopia [58, 60, 69]. The oral is the major route of administration of treatments in Yalo Woreda and a primary route of administration reported by many studies in Ethiopia and elsewhere [51–53, 56, 62, 77]. The application of remedies such as eye, nasal and ear drops, body washing, and insertion into a cut made in the knee, breast, or swollen body parts are dominantly used by other studies [9, 17, 43, 44, 54, 58, 69, 78, 82, 117]. The knowledge about health conditions of both humans and animals as in many studies in Ethiopia and Africa determines the types of treatment and the dosage. The measurement of a dose is related to the effectiveness of the remedy and levels of poisoning that has been determined through long years of trial and error [48, 54, 71]. The knowledge of standard practices considered in the management of remedies in traditional human healthcare systems is important factors to determine dosage, route, and frequency of applications [69, 78]. The treatment of animals is related to the manner of feeding and physical movement and, in most case, treatment is discontinued as the animal feeding, and physical status is improved, or sign of illness disappears. The remedies are given until the animal fully recovers, or its physical conditions are improved [51, 54].
The informants in the study area had displayed high consensus values on the plants used as a remedy that indicated the popularity and therapeutic value of the plants in the society and the prevalence of the disease in the area [46, 47]. The category of diseases with high ICF values are acute febrile illness and malaria; internal, liver and gastrointestinal infection, and internal parasite. The Yalo Woreda is malarious, and the people used 37 plant species to treat the illness, and 57 plant species as a treatment for liver and gastrointestinal infections that are developed over long years of trial and error similar to other studies conducted in the country [36, 41, 72, 77, 88]. The ethnobotanical study conducted in pastoral area Samburu district, Kenya has similar result that malaria and GIT are treated with 15 to 20 medicinal plants [49]. The majority of the plants with fidelity value of 1.00 was reported by few informants (one to two) and was used only as a treatment for an ailment. Aizoon canariensis L. is used to treat devil disease and madness, On the other hand, medicinal plants that were used to treat a variety of ailments had lower FL values. The values, in such cases, may not indicate the disagreement among the informants [51, 55] rather it means that these plants are more favored by the local people in the treatment of a variety of diseases such as diphtheria, typhoid, herpes zoster, scorpion bite, devil illness, ETPB, lung infection, dysentery, breast cancer, and angina [36, 41, 51]. The medicinal plants reported by 15 and more informants and used as a remedy for multiple diseases were ranked based on their healing potential of a disease. Balanites rotundifolia and A. fruticosa are used as remedies for diseases such as breast cancer, dyspepsia, epilepsy, ETPB, eye sickness, herpes zoster, infant disease, jaundice, lung infection, and malaria [17, 40, 57, 64, 68, 69, 81]. These plants have lower FL values indicating the popularity of the plants as a treatment for a variety of diseases. Therefore, preference ranking does not necessarily indicate healing potential of plants but also their popularity and may be abundance in the study area since their fruits are edible. Other societies also report the medicinal plants as a remedy for multiple diseases such as throat infection, stomachache/diarrhea; sexual incompetence of male; body infection; skin wound, snake bite, madness, typhus, eye problem, anthrax; rabies [10, 13, 22, 37, 64, 76, 82].
Wild edible plants of Yalo Woreda
The wild edible plant parts are all eaten fresh, and duration of gathering and consumption are dependent on the availability of edible parts and seasons [34, 41, 46, 78]. The seasons are determined by the extent of rain and drought in the region. Sugum is the period of little rainfall (March to April), and Karma (June to September) is the main rain season. Gilal (October to February) and Hagay (May to June) are the dry seasons. Hagay extends to Karma and Gilal to Sugum depending on the length of rain and drought period [10–12, 80]. Borena, Kara, and Kwego pastoralist and people in semiarid areas in Ethiopia also consume the edible plants reported such as B. aegyptiaca, B. rotundifolia, Dobera glabra (Forssk.) Poir., Carissa spinarum L., C.sinensis, G. bicolor, G. villosa, T.amarindus indica L., X americana and Z. spina-christi [12, 13, 71, 78, 80, 118]. The people in semi-arid and arid areas rely more on edible plants compared to people that inhabit humid regions and highlands. These plants serve as food security during the dry season in semi-arid and arid areas where the recurrent drought have a dominant effect on animal’s productivity and could be developed to food crops to alleviate food shortage [78, 81, 119, 120]. Balanites aegyptiaca and B. rotundifolia and D. glabra are ‘famine food’ that are collected and stored for years in dry condition to be used in drought period to avoid starvation [12, 78, 80, 121]. These wild edible plants have been consumed by pastoralist people living in semi-arid and arid regions to alleviate food insecurity such as in the 1971 and 72 starvation in Ethiopia that severely affected Afar’s livestock. Similarly, Feyssa et al. [12] indicated that people in semi-arid and arid regions of Oromia state in Ethiopia, survived by eating fruits of D. glabra at the time of severe hunger. The wild edible fruits identified in Yalo Woreda with wider geographical distribution and altitude ranges are consumed by many societies in Ethiopia as reserve food to fill gaps between farming and harvest times where most poor farmers exhaust their crops. Unlike other parts of Ethiopia leaves, roots, and stems are not used as food in the Yalo Woreda [10–14, 20, 34, 46, 60, 62, 68, 78–81, 116, 119, 120, 122, 123]. Balanites aegyptiaca, B. rotundifolia, C.sinensis, and D. glabra, are sold in open markets and had economic importance [41]. Adults in eastern Sudan consume Balanites aegyptiaca, Z. spina-christi, and T. indica and have economic significance, and also have high marketability in other parts of Ethiopia [8, 34, 46, 62, 79, 123, 124].
Conclusion
The people in Yalo Woreda possess a wealth of traditional knowledge on the treatment of both human and livestock health conditions, and edible plants. Fabaceae are the dominant plant species used in Ethnomedicine preparations. The people use a variety of measurements to quantify dosage and route of application in the administration of remedies. The edible plants are used as food security and generate the pastoralist economic. All the plants with medicinal and economic importance are collected from the wide and conservation is not practiced in the area. Hence, conservation of the plants in the home garden and in the natural vegetation is a necessity against the recurrent drought and climatic changes that negatively affect the vegetation of the area, to protect the associated traditional knowledge from fast disappearing and ensure sustainable use of the plants in the traditional healthcare system. The integration of edible plants in the food sufficiency strategies in the area has to be considered since animal productivity is severely affected by encroaching invasive plants and recurrent drought. The holistic soil and water conservation policy that is being implemented in other parts of the country has to be employed in the region to save the natural vegetation that is also the repository for the medicinal and edible plants for future pharmacological and nutritional studies.
Additional files
Medicinal plants used for treatment of human illness, Yalow Woreda, 2016 (B = bark, C = climber, F = flower, Fr = fruit, L = leaf, La = latex, R = root, S = stem, Br = branch, UP = upper part WP = whole plant, YP = young plant). (DOCX 179 kb)
Medicinal plants used to treat animal illness, Yalow Woreda, 2016. (B = bark, C = climber, F = flower, Fr = fruit, L = leaf, La = latex, R = root, S = stem, Br = branch, UP = upper part WP = whole plant, YP = young plant). (DOCX 66 kb)
Acknowledgments
I would like to thank the informants, the Yalo Woreda elders, and the administrative officers for their holistic collaboration and assistance in data and specimens collection. I also thank Ato Melaku Wondafrash, National Herbarium of Addis Ababa University, for identification of the plants.
Funding
Vice President Office of Research and Technology Transfer funded the study.
Availability of data and materials
All the data collected and used in this paper are submitted as Additional files 1 and 2.
Abbreviations
- CCPP
Contagious caprine pleuropneumonia
- Orf
Contagious pustular dermatitis, contagious ecthyma
- PPR
Peste des petits ruminants
- SPSS
Statistical Package for the Social Sciences
Authors’ contributions
Not applicable.
Ethics approval and consent to participate
Institute Review Board of Aklilu Lemma Institute of Pathobiology, Addis Ababa University approved the study and the informants, the Yalo Woreda elders, and the administrative officers gave their verbal consent before the commencement of data and specimens collection.
Consent for publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s13002-017-0166-7) contains supplementary material, which is available to authorized users.
References
- 1.Biru A, Adem A, Eshete B, Hailu B, Mahmud M, Temesgen D, et al. Afar National Regional State Programme of plan on adaptation to climate change. Semera: Environmental Protection Authority of the Federal Democratic Republic of Ethiopia; 2010. [Google Scholar]
- 2.CSA (Central Statistical Authority). Summary and statistical report of the 2007. Population and Housing Census. Addis Ababa, Ethiopia; 2008.
- 3.Lawry S, McLain R, Kassa H. Strengthening the resiliency of dryland forest-based livelihoods in Ethiopia and South Sudan: a review of literature on the interaction between dryland forests, livelihoods and forest governance. Working Paper, Bogor, Indonesia: CIFOR. 2015;82
- 4.Luizza MW, Wakie T, Evangelista PH, Jarnevich CS. Integrating local pastoral knowledge, participatory mapping, and species distribution modeling for risk assessment of invasive rubber vine (Cryptostegia grandiflora) in Ethiopia’s Afar region. Ecol Soc. 2016;21(1):22. doi: 10.5751/ES-07988-210122. [DOI] [Google Scholar]
- 5.Ethiopian Biodiversity Institute (EBI). Acacia-Commiphora Woodland Ecosystem. http://www.ebi.gov.et/biodiversity/ecosystems-of-ethiopia/acacia-commiphora-woodland-ecosystem/. Accessed 9 Jan 2017.
- 6.Atanga NL, Treydte AC, Birner R. Assessing the sustainability of different small-scale livestock production Systems in the Afar Region. Ethiopia Land. 2013;2:726–755. [Google Scholar]
- 7.Reda KT. Social organization and cultural institutions of the Afar of northern Ethiopia. International Journal of Sociology and Anthropology. 2011;3(11):423–429. [Google Scholar]
- 8.Satheesh N. Review on distribution, nutritional and medicinal values of Casimiroa edulus L lave- an underutilized fruit in Ethiopia. Am-Euras J Agric & Environ Sci. 2015;15(8):1574–1583. [Google Scholar]
- 9.Giday M, Teklehaymanot T. Ethnobotanical study of plants used in management of livestock health problems by Afar people of Ada’ar district, Afar regional state. Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2013;9:8. doi: 10.1186/1746-4269-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bahru T, Asfaw Z, Demissew S. Indigenous knowledge on plant species of material culture (construction, Traditional Arts & Handicrafts) used by the Afar and Oromo nations in and around the Awash National Park, Ethiopia. Global Journal of Human Social Science. 2012;12(11):1–20. [Google Scholar]
- 11.Tsegaye D, Balehgn M, Gebrehiwot K, Haile M, G/Samuel G, Tilahun M, et al. The Role of Garsa (Dobera glabra) for Household Food Security at Times of Food Shortage in Aba’ala Wereda, North Afar: Ecological Adaptation and Socio-economic Value. A study from Ethiopia. Drylands Coordination Group Report No. 49; 2007. http://www.drylands-group.org. Accessed 06 Jan 2017.
- 12.Feyssa DH, Njoka JT, Asfaw Z, Nyangito MM. Seasonal availability and consumption of wild edible plants in semiarid Ethiopia: implications for food security and climate change adaptation. Journal of Horticulture and Forestry. 2011;3(5):138–149. [Google Scholar]
- 13.Feyssa HD, Njoka JT, Asfaw Z, Nyangito MM. Comparative analysis of indigenous knowledge on use and management of wild edible plants: the case of central east Shewa of Ethiopia. Ethnobotany Research & Applications. 2012;10:287–304. doi: 10.17348/era.10.0.287-304. [DOI] [Google Scholar]
- 14.Bahru T, Asfaw Z, Demissew S. Wild edible plants: sustainable use and management by indigenous communities in and the buffer area of Awash National Park. Ethiopia. SINET: Ethiop. J. Sci. 2013;36(2):93–108. [Google Scholar]
- 15.Kebede AT. Sustaining the Allideghi grassland of Ethiopia: influence of pastoralism and vegetation change. Utah State University:PhD Dissertation. 2009;
- 16.Yohannes T, Awas T, Demissew S. Survey and documentation of the potential and actual invasive alien plant species and other biological threats to biodiversity in Awash National Park. Ethiopia Management of Biological Invasions. 2011;2:3–14. doi: 10.3391/mbi.2011.2.1.01. [DOI] [Google Scholar]
- 17.Hassan-Abdallah A, Merito A, Hassan S, Aboubaker D, Djama M, Asfaw Z, et al. Medicinal plants and their uses by the people in the region of Randa. Djibouti Journal of Ethnopharmacology. 2013;148:701–13. [DOI] [PubMed]
- 18.Wakie TT, Evangelista PH, Jarnevich CS, Laituri M. Mapping current and potential distribution of non-native Prosopis juliflora in the Afar region of Ethiopia. PLoS One. 2014;9:11. doi: 10.1371/journal.pone.0112854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehari AT. Ethnobotanical study of Dess’a forest, north-eastern escarpment of Ethiopia, with emphasis on use and management of forest resources by the local people. MSc. Thesis: Addis Ababa University, School of Graduate Studies; 2008. [Google Scholar]
- 20.Ashagre M, Asfaw Z, Kelbessa E. Ethnobotanical study of wild edible plants in Burji District, Segan area zone of southern nations, nationalities and peoples region (SNNPR) Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2016;12:32. doi: 10.1186/s13002-016-0103-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alemu DT. Impact of land use on vegetation resources with emphasis on woody vegetation in the semi-arid area of Abala District, north Afar, Ethiopia. PhD Dissertation: University of Nairobi, Range Management Department; 1999. [Google Scholar]
- 22.Seifu T, Asres K, Gebre-Mariam T. Ethnobotanical and Ethnopharmaceutical studies on medicinal plants of Chifra District, Afar region. North Eastern Ethiopia Ethiop Pharm J. 2006;24:41–58. [Google Scholar]
- 23.Meragiaw M. Wild useful plants with emphasis on traditional use of medicinal and edible plants by the people of Aba'ala, North-eastern Ethiopia. J Med Plant Herb Ther Res. 2016;4:1–16. [Google Scholar]
- 24.Sector offices: Report of Yalo Woreda, Afar Regional State, Sector offices (2016).
- 25.Health Office . Report of Yalo Woreda health Office. 2016. [Google Scholar]
- 26.Pastoral and Rural Development Office: Report of Pastoral and Rural Development Office (2016).
- 27.Martin G. Ethnobotany: a method manual. London: Chapman and Hall; 1995. [Google Scholar]
- 28.Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers’consencus and cultural importance. Social Sci Med. 1998;47:1863–1875. doi: 10.1016/S0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- 29.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on the rational analysis of an ethnopharmacological field survey among Bedouins in Negev Desert. Israel Journal of Ethnopharmacology. 1986;16:275–287. doi: 10.1016/0378-8741(86)90094-2. [DOI] [PubMed] [Google Scholar]
- 30.Hunde D, Asfaw Z, Kelbessa E. Use of traditional medicinal plants by people of ‘Boosat’ sub district, central eastern Ethiopia. Ethiop J Health Sci. 2006;16(2):141–155. [Google Scholar]
- 31.Yirga G. Ethnobotanical study of medicinal plants in and around Alamata, southern Tigray, northern Ethiopia. Curr Res J Biol Sci. 2010;2(5):338–344. [Google Scholar]
- 32.Birhane E, Aynekulu E, Mekuria W, Endale D. Management, use and ecology of medicinal plants in the degraded dry lands of Tigray, northern Ethiopia. Journal of Medicinal Plants Research. 2011;5(3):309–318. [Google Scholar]
- 33.Moravec I, Fernandez E. Vlkova1 M, Milella L. ethnobotany of medicinal plants of northern Ethiopia. Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas. 2014;13(2):126–134. [Google Scholar]
- 34.Beche D, Gebeyehu G, Feyisa K. Indigenous utilization and Management of Useful Plants in and around Awash National Park. Ethiopia J Plant Biol Soil Health. 2016;3(1):12. [Google Scholar]
- 35.Cheikhyoussef A, Shapi M, Matengu K, Ashekele HM. Ethnobotanical study of indigenous knowledge on medicinal plant use by traditional healers in Oshikoto region. Namibia Journal of Ethnobiology and Ethnomedicine. 2011;7:10. doi: 10.1186/1746-4269-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Teklehaymanot T. Ethnobotanical study of knowledge and medicinal plants use by the people in Dek Island in Ethiopia. J Ethnopharmacol. 2009;124:69–78. doi: 10.1016/j.jep.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 37.Singhal R. Medicinal plants and primary health care: the role of gender. J Health Manag. 2005;7:2. doi: 10.1177/097206340500700208. [DOI] [Google Scholar]
- 38.Torres-Avilez W, deMedeiros PM, Albuquerque UP. Effect of Gender on the Knowledge of Medicinal Plants: Systematic Review and Meta-Analysis. Evidence-Based Complementary and Alternative Medicine. 2016:13. [DOI] [PMC free article] [PubMed]
- 39.Nalule AS, Mbaria JM, Olila D, Kimenju JW. Ethnopharmacological practices in management of livestock helminthes by pastoral communities in the drylands of Uganda. Livestock Research for Rural Development. 2011; 23 (2).
- 40.de Almeida CBR, Ramos MA, de Amorim ELC, de Albuquerque UP. Comparison of knowledge about medicinal plants for three rural communities in the semi-arid region of northeast of Brazil. J Ethnopharmacol. 2010;127(3):674–684. doi: 10.1016/j.jep.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 41.Belayneh A, Asfaw Z, Demissew S, Bussa NF. Medicinal plants potential and use by pastoral and agro-pastoral communities in Erer Valley of Babile Wereda. Eastern Ethiopia Journal of Ethnobiology and Ethnomedicine. 2012;8:42. doi: 10.1186/1746-4269-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mathez-Stiefel SL, Vandebroek I. Distribution and transmission of medicinal plant knowledge in the Andean highlands: a case study from Peru and Bolivia. Evid Based Complement Alternat Med. 2012;18 doi:10.1155/2012/959285. [DOI] [PMC free article] [PubMed]
- 43.Eshete MA, Kelbessa E, Dalle G. Ethnobotanical study of medicinal plants in Guji agro-pastoralists, blue Hora District of Borana zone, Oromia region. Ethiopia Journal of Medicinal Plants Studies. 2016;4(2):170–184. [Google Scholar]
- 44.Parthiban R, Vijayakumar S, Prabhu S, Yabesh JGEM. Quantitative traditional knowledge of medicinal plants used to treat livestock diseases from Kudavasal taluk of Thiruvarur district, Tamil Nadu. India Revista Brasileira de Farmacognosia. 2016;26:109–121. doi: 10.1016/j.bjp.2015.07.016. [DOI] [Google Scholar]
- 45.Ayantunde AA, Briejer M, Hiernaux P, Udo HMJ, Tabo R. Botanical Knowledge and its Differentiation by Age, Gender and Ethnicity in Southwestern Niger. Hum Ecol. 2008;36:(6):881–889.
- 46.Balemie K, Kebebew F. Ethnobotanical study of wild edible plants in Derashe and Kucha districts. South Ethiopia Journal of Ethnobiology and Ethnomedicine. 2006;2:53. doi: 10.1186/1746-4269-2-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lulekal E, Asfaw Z, Kelbessa E, Van Damme P. Ethnomedicinal study of plants used for human ailments in Ankober District, north Shewa zone, Amhara region. Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2013;9:63. doi: 10.1186/1746-4269-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Belayneh A, Bussa NF. Ethnomedicinal plants used to treat human ailments in the prehistoric place of Harla and Dengego valleys, eastern Ethiopia. J Ethnobiol Ethnomed. 2014;10:18. doi: 10.1186/1746-4269-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nanyingi MO, Mbaria JM, Lanyasunya AL, Wagate CG, Koros KB, Kaburia HF, et al. Ethnopharmacological survey of Samburu district. Kenya Journal of Ethnobiology and Ethnomedicine. 2008;4:14. doi: 10.1186/1746-4269-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Silva FDS. Ramo MAs, Hanazaki N, de Albuquerque UP. Dynamics of traditional knowledge of medicinal plants in a rural community in the Brazilian semi-arid region. Brazilian Journal of Pharmacognosy. 2011;21(3):382–391. doi: 10.1590/S0102-695X2011005000054. [DOI] [Google Scholar]
- 51.Alhaji NB, Babalobi OO. Participatory epidemiology of Ethnoveterinary practices Fulani pastoralists used to manage contagious bovine pleuropneumonia and other cattle ailments in Niger state. Nigeria Journal of Veterinary Medicine. 2015;10 10.1155/2015/460408 [DOI] [PMC free article] [PubMed]
- 52.Yineger H, Kelbessa E, Bekele T, Lulekal E. Ethnoveterinary medicinal plants in Bale Mountains National Park. Ethiopia J Ethnopharmacol. 2007;112:55–70. doi: 10.1016/j.jep.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 53.Yirga G, Teferi M, Gidey G, Zerabruk S. An ethnoveterinary survey of medicinal plants used to treat livestock diseases in Seharti-Samre district. Northern Ethiopia Afr J Plant Sci. 2012;6:113–119. [Google Scholar]
- 54.Gakuubi MM, Wanzala W. A survey of plants and plant products traditionally used in livestock health management in Buuri district, Meru County. Kenya Gakuubi and Wanzala Journal of Ethnobiology and Ethnomedicine. 2012;8:39. doi: 10.1186/1746-4269-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Seid MA, Tsegay BA. Ethnobotanical survey of traditional medicinal plants in Tehuledere district, south Wollo. Ethiopia Journal of Medicinal Plants Research. 2011;5(26):6233–6242. [Google Scholar]
- 56.Abera B. Medicinal plants used in traditional medicine by Oromo people, Ghimbi District. Southwest Ethiopia Journal of Ethnobiology and Ethnomedicine. 2014;10:40. doi: 10.1186/1746-4269-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Flatie T, Gedif T, Asres K, Tsige G-MT. Ethnomedical survey of Berta ethnic group Assosa zone, Benishangul-Gumuz regional state, mid-west Ethiopia. J Ethnobiol Ethnomed. 2009;5:14. doi: 10.1186/1746-4269-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gradé JT. Ethnoveterinary Knowledge in Pastoral Karamoja, Northern Uganda. Ghent University, Faculty of Bioscience Engineering: Ph.D. Thesis; 2008.
- 59.Quinlan MB, Quinlan RJ. Modernization and medicinal plant knowledge in a caribbean horticultural village. Med Anthropol Q. 2007;21:169–192. doi: 10.1525/maq.2007.21.2.169. [DOI] [PubMed] [Google Scholar]
- 60.Wondimu T, Asfaw Z, Kelbessa E. Ethnobotanical study of food plants around Dheeraa' town, Arsi. Ethiopia SINET: Ethiop J Sci. 2006;29(1):71–80. doi: 10.1016/j.jep.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 61.Kidane B, van der Maesen LJG, van Andel T, Asfaw Z, Sosef MSM. Ethnobotany of wild and semi-wild edible fruit species used by Maale and Ari ethnic communities in southern Ethiopia. Ethnobotany Research & Applications. 2014;12:455–471. doi: 10.17348/era.12.0.455-471. [DOI] [Google Scholar]
- 62.Sindiga I. Indigenous (medical) knowledge of the Maasai. Indigenous Knowledge and Development Monitor. 1994. http://www.nuffic.nl/ciran/ikdm/ Accessed 1/09/2016.
- 63.Menendez-Baceta G, Aceituno-Mata L, Reyes-García V, Tardío J, Salpeteur M, Pardo-de-Santayana M. The importance of cultural factors in the distribution of medicinal plant knowledge: a case study in four Basque regions. J Ethnopharmacol. 2015;161:116–127. doi: 10.1016/j.jep.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 64.Abu-Rabia A. Urinary diseases, and ethnobotany among pastoral nomads in the Middle East. J Ethnobiol Ethnomed. 2005;1:4. doi: 10.1186/1746-4269-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pankhurst R. A historical examination of traditional Ethiopian medicine and surgery. Ethiopia Medical Journal. 1965;3:157–172. [Google Scholar]
- 66.Abebe D, Ayehu A. Medicinal plants and enigmatic health practices of northern Ethiopia. B.S.P.E: Addis Ababa, Ethiopia; 1993. [Google Scholar]
- 67.Teklehaymanot T, Giday M, Medhin G, Mekonnen Y. Knowledge and use of medicinal plants by people around Debre Libanos monastery in Ethiopia. J Ethnophamacol. 2007;111:271–283. doi: 10.1016/j.jep.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 68.Maundu PM, Ngugi GW. Kabuye CHS. National Museum of Kenya: Traditional Food Plants of Kenya; 1999. [Google Scholar]
- 69.Lulekal E, Kelbessa E, Bekele T, Yineger H. An ethnobotanical study of medicinal plants in Mana Angetu District, southeastern Ethiopia. Journal of Ethnobiology and Ethnomedicine Journal of Ethnobiology and Ethnomedicine. 2008;4:10. doi: 10.1186/1746-4269-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Birhanu T, Abera D. Survey of ethnoveterinary medicinal plants at selected Horro Gudurru districts, western Ethiopia. African J Plant Sci. 2015;9(3):185–192. doi: 10.5897/AJPS2014.1229. [DOI] [Google Scholar]
- 71.Chekole G, Asfaw Z, Kelbessa E. Ethnobotanical study of medicinal plants in the environs of Tara-gedam and Amba remnant forests of Libo Kemkem District, northwest Ethiopia. J Ethnobiol Ethnomed. 2015;11:4. doi: 10.1186/1746-4269-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mesfin F, Demissew S, Teklehaymanot T. An ethnobotanical study of medicinal plants in Wonago Woreda, SNNPR. Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2009;5:28. doi: 10.1186/1746-4269-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tadesse B, Mulugeta G, Fikadu G, Sultan A. Survey on ethno-veterinary medicinal plants in selected Woredas of east Wollega zone, western Ethiopia. Journal of Biology, Agriculture and Healthcare. 2014;4(17):97–105. [Google Scholar]
- 74.Tekle Y. Medicinal plants in the ethno veterinary practices of Bensa Woreda. Southern Ethiopia Open Access Library Journal. 2015;2 [Google Scholar]
- 75.Afar National Regional State (ANRS). A strategic plan for the sustainable development, conservation, and management of the woody biomass resources. Final report. Ethiopia, Addis Ababa; 2004.
- 76.Yineger H, Yewhalaw D. Traditional medicinal plant knowledge and use by local healers in Sekoru District, Jimma zone. Southwestern Ethiopia Journal of Ethnobiology and Ethnomedicine. 2007;3:24. doi: 10.1186/1746-4269-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Megersa M, Asfaw Z, Kelbessa E, Beyene A, Woldeab B. An ethnobotanical study of medicinal plants in Wayu Tuka District, east Welega zone of Oromia regional state. West Ethiopia Journal of Ethnobiology and Ethnomedicine. 2013;9:68. doi: 10.1186/1746-4269-9-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Teklehaymanot T, Giday M. Quantitative ethnobotany of medicinal plants used by Kara and Kwego semi-pastoralist people in lower Omo River Valley, Debub Omo zone, southern nations, nationalities and peoples regional state. Ethiopia Journal of Ethnopharmacology. 2010;130:76–84. doi: 10.1016/j.jep.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 79.Assefa A, Abebe T. Wild edible trees and shrubs in the semi-arid lowlands of southern Ethiopia. Journal of Science and Development. 2011;1(1):1–19. [Google Scholar]
- 80.Feyssa DH, Njoka JT, Nyangito MM, Asfaw Z. Nutraceutical wild plants of semi-arid east Shewa, Ethiopia: contribution to food and healthcare security of semiarid people. Research Journal of Forestry. 2011;5(1):1–16. doi: 10.3923/rjf.2011.1.16. [DOI] [Google Scholar]
- 81.Gemedo-Dalle T, Maass BL, Isselstein J. Plant biodiversity and ethnobotany of Borana pastoralists in southern Oromia. Ethiopia Economic Botany. 2005;59(1):43–65. doi: 10.1663/0013-0001(2005)059[0043:PBAEOB]2.0.CO;2. [DOI] [Google Scholar]
- 82.Zerabruk S, Yirga G. Traditional knowledge of medicinal plants in Gindeberet district, western Ethiopia. S Afr J Bot. 2012;78:165–169. doi: 10.1016/j.sajb.2011.06.006. [DOI] [Google Scholar]
- 83.Amenu E. Use and management of medicinal plants by indigenous people of Ejaji area (Chelya Woreda) west Shoa, Ethiopia: an ethnobotanical approach. MSc. Thesis: Addis Ababa University; 2007. [Google Scholar]
- 84.Kubmarawa D, Ajoku GA, Enwerem NM, Okorie DA. Preliminary phytochemical and antimicrobial screening of 50 medicinal plants from Nigeria. Afr J Biotechnol. 2007;6(14):1690–1696. [Google Scholar]
- 85.Giday M, Ameni G. An ethnobotanical survey on plants of veterinary importance in two woredas of southern Tigray, northern Ethiopia. SINET: Ethiop J Sci. 2003;26(2):123–136. [Google Scholar]
- 86.Etana B. Ethnobotanical study of traditional medicinal plants of Goma Wereda, Jima zone of Oromia region, Ethiopia. MSc. Thesis: Addis Ababa University; 2010. [Google Scholar]
- 87.Teklay A, Abera B, Giday M. An ethnobotanical study of medicinal plants used in Kilte Awulaelo District. Tigray Region of Ethiopia Journal of Ethnobiology and Ethnomedicine. 2013;9:65. doi: 10.1186/1746-4269-9-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tolossa K, Debela E, Athanasiadou S, Tolera A, Ganga G, Houdijk JGM. Ethno-medicinal study of plants used for treatment of human and livestock ailments by traditional healers in south Omo. Southern Ethiopia Journal of Ethnobiology and Ethnomedicine. 2013;9:32. doi: 10.1186/1746-4269-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maryo M, Nemomissa S, Bekele T. An ethnobotanical study of medicinal plants of the Kembatta ethnic group in Enset-based agricultural landscape of Kembatta Tembaro (KT) zone, southern Ethiopia. Asian Journal of Plant Science and Research. 2015;5(7):42–61. [Google Scholar]
- 90.Erhirhie EO, Ekene NE. Medicinal values on Citrullus lanatus (watermelon): pharmacological review. Int J Res Pharmaceut Biomed Sci. 2013;4(4):1305–1312. [Google Scholar]
- 91.Ocho DL, Struik PC, Price LL, Kelbessa E, Kolo K. Assessing the levels of food shortage using the traffic light metaphor by analyzing the gathering and consumption of wild food plants, crop parts and crop residues in Konso. Ethiopia Journal of Ethnobiology and Ethnomedicine. 2012;8:30. doi: 10.1186/1746-4269-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Addis G, Asfaw Z, Woldu Z. Ethnobotany of wild and semi-wild edible plants of Konso ethnic community. South Ethiopia Ethnobotany Research & Applications. 2013;11:121–141. [Google Scholar]
- 93.Memon AH, Rind FMA, Laghari MGH, Mughal UR, Memon N, Gilal RA, et al. Common folk medicinal and ethnomedicinal uses of thirty medicinal plants of districts Dadu and Jamshoro, Sindh. Pakistan Sindh Univ Res Jour. 2008;40(2):89–108. [Google Scholar]
- 94.Rehman K, Mashwani ZR, Khan MA, Ullah Z, Chaudhary HJ. An ethnobotanical perspective of traditional medicinal plants from the Khattak tribe of Chonthra Karak. Pakistan Journal of Ethnopharmacology. 2015;165:251–259. doi: 10.1016/j.jep.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 95.Elegamia AA, Elnima EI, Muddathir AK, Omer ME. Antimicrobial activity of Plicosepalus acacia. Fitoterapia. 2001;72:431–434. doi: 10.1016/S0367-326X(01)00268-4. [DOI] [PubMed] [Google Scholar]
- 96.Al-Fatimi M, Wurster M, Schröder G, Lindequist U. Antioxidant, antimicrobial and cytotoxic activities of selected medicinal plants from Yemen. J Ethnopharmacol. 2007;111:657–666. doi: 10.1016/j.jep.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 97.Saadabi MA, Moglad EH. Experimental evaluation of certain Sudanese plants used in folkloric medicine for their antibacterial activity (in- vitro tests) J Appl Sci Res. 2011;7(3):253–256. [Google Scholar]
- 98.Longuefosse JL, Nossin E. Medical ethnobotany survey in Martinique. J Ethnopharmacol. 1996;53:117–142. doi: 10.1016/0378-8741(96)01425-0. [DOI] [PubMed] [Google Scholar]
- 99.Tabuti JRS, Kukunda CB, Kaweesi D, Ossy MJ, Kasilo OMJ. Herbal medicine use in the districts of Nakapiripirit, Pallisa, Kanungu, and Mukono in Uganda. J Ethnobiol Ethnomed. 2012;8:35. doi: 10.1186/1746-4269-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Batista R, Júnior AJS, de Oliveira AB. Plant-derived antimalarial agents: new leads and efficient Phytomedicines. Part II Non-Alkaloidal Natural Products Molecules. 2009;14:3037–3072. doi: 10.3390/molecules14083037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Setyawan AD. Review: recent status of Selaginella (Selaginellaceae) research in Nusantara. Bio Diversit As. 2011;12(2):112–124. [Google Scholar]
- 102.Almeida JRGS, de Sá PGS, Macedo LARO, Filho JAS, Oliveira VR, Filho JMB. Phytochemistry of the genus Selaginella (Selaginellaceae) J Med Plants Res. 2013;7(25):1858–1868. [Google Scholar]
- 103.Dharani N, Yenesew A, Aynekulu E, Tuei B, Jamnadass R. Traditional ethnoveterinary medicine in East Africa: a manual on the use of medicinal plants. The World Agroforestry Centre (ICRAF), Nairobi, Kenya: Dawson IK ed; 2015. [Google Scholar]
- 104.Sori T, Bekana M, Adugna G, Kelbessa E. Medicinal plants in the Ethnoveterinary practices of Borana pastoralists, southern Ethiopia. Intern J Appl Res Vet Med. 2004;2(3):220–225. [Google Scholar]
- 105.Zenebe G, Zerihun M, Solomon Z. An ethnobotanical study of medicinal plants in Asgede Tsimbila District, northwestern Tigray. Northern Ethiopia Ethnobotany Research & Applications. 2012;10:305–320. doi: 10.17348/era.10.0.305-320. [DOI] [Google Scholar]
- 106.Gebrezgabiher G, Kalayou S, Sahle S. An ethno-veterinary survey of medicinal plants in woredas of Tigray region, northern Ethiopia. International Journal of Biodiversity and Conservation. 2013;5(2):89–97. [Google Scholar]
- 107.Bekalo TH, Woodmatas SD, Woldemariam ZA. An ethnobotanical study of medicinal plants used by local people in the lowlands of Konta special Woreda, southern nations, nationalities and peoples regional state. Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2009;5:26. doi: 10.1186/1746-4269-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Araya S, Abera B, Giday M. Study of plants traditionally used in public and animal health management in Seharti Samre District, southern Tigray. Ethiopia Journal of Ethnobiology and Ethnomedicine. 2015;11:22. doi: 10.1186/s13002-015-0015-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Paulos B, Fenta TG, Bisrat D, Asres K. Health seeking behavior and use of medicinal plants among the Hamer ethnic group, south Omo zone, southwestern Ethiopia. J Ethnobiol Ethnomed. 2016;12:44. doi: 10.1186/s13002-016-0107-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lulekal E, Asfaw Z, Kelbessa E, Van Damme P. Ethnoveterinary plants of Ankober District, north Shewa zone, Amhara region. Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2014;10:21. doi: 10.1186/1746-4269-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tamiru F, Terfa W, Kebede E, Dabessa G, Roy RK, Sorsa M. Ethnoknowledge of plants used in veterinary practices in Dabo Hana District, West Ethiopia. Journal of Medicinal Plant Research. 2013;7(40):2960–2971. [Google Scholar]
- 112.Caudell MA, Quinlan MB, Quinlan RJ, Call DR. Medical pluralism and livestock health: ethnomedical and biomedical veterinary knowledge among east African agropastoralists. J Ethnobiol Ethnomed. 2017;13:7. doi: 10.1186/s13002-017-0135-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Giday M, Teklehaymanot T, Animut A, Mekonnen Y. Medicinal plants of the Shinasha, Agew-Awi and Amhara peoples in northwest Ethiopia. J Ethnopharmacol. 2007;110:516–525. doi: 10.1016/j.jep.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 114.Endalew A. Use and Management of Medicinal Plants by indigenous people of Ejaji area (Chelya Wereda) west Shewa. Ethiopia: An Ethnobotanical Approach. M.Sc. Thesis. Addis Ababa University; 2007. [Google Scholar]
- 115.Assefa A, Abebe T. Ethnobotanical study of wild medicinal trees and shrubs in Benna Tsemay District, southern Ethiopia. Journal of Science & Development. 2014;2(1):17–33. [Google Scholar]
- 116.Lulekal E, Asfaw Z, Kelbessa E, Van Damme P. Wild edible plants in Ethiopia: a review on their potential to combat food insecurity. Africa Focus. 2011;24:71–121. [Google Scholar]
- 117.Qasim M, Abideen Z, Adnan MY, Ansari R, Gul B, Khan MA. Traditional ethno-botanical uses of medicinal plants from coastal areas of Pakistan. Journal of Coastal Life Medicine. 2014;2(1):22–30. [Google Scholar]
- 118.Teklehaymanot T, Giday M. Ethnobotanical study of wild edible plants of Kara and Kwego semi-pastoralist people in lower Omo River Valley, Debub Omo zone, SNNPR. Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2010;6:23. doi: 10.1186/1746-4269-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Alemayehu G, Asfaw Z, Kelbessa E. Plant diversity and ethnobotany in Berehet District, north Shewa zone of Amhara region (Ethiopia) with emphasis on wild edible plants. Journal of Medicinal Plants Studies. 2015;3(6):93–105. [Google Scholar]
- 120.Asfaw Z, Tadesse M. Prospects for sustainable use and development of wild food plants in Ethiopia. Econ Bot. 2001;55(1):47–62. doi: 10.1007/BF02864545. [DOI] [Google Scholar]
- 121.Gebrekirstos A, Demel Teketay D, Mitlöhner R. Responses of Dobera glabra and eight co-occurring species to drought and salinity stress at a savanna-scrub ecotone: implications in the face of climate change. Open Journal of Forestry. 2014;4:327–337. doi: 10.4236/ojf.2014.44039. [DOI] [Google Scholar]
- 122.Tebkew M, Asfaw Z, Zewudie S. Underutilized wild edible plants in the Chilga District, north-western Ethiopia: focus on wild woody plants. Journal of Agriculture & Food Security. 2014;3:12. doi: 10.1186/2048-7010-3-12. [DOI] [Google Scholar]
- 123.Salih NKEM, Ali AH. Wild food trees in eastern Nuba Mountains, Sudan: use, diversity, and threatening factors. J Agric Rural Dev Trop Subtrop. 2014;115(1):1–7. [Google Scholar]
- 124.Aref IM, El Atta HA, Al Ghtani AA. Ecological study on Dobera glabra Forssk. At Jazan region in Saudi Arabia. Journal of Horticulture and Forestry. 2009;1(10):198–204. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Medicinal plants used for treatment of human illness, Yalow Woreda, 2016 (B = bark, C = climber, F = flower, Fr = fruit, L = leaf, La = latex, R = root, S = stem, Br = branch, UP = upper part WP = whole plant, YP = young plant). (DOCX 179 kb)
Medicinal plants used to treat animal illness, Yalow Woreda, 2016. (B = bark, C = climber, F = flower, Fr = fruit, L = leaf, La = latex, R = root, S = stem, Br = branch, UP = upper part WP = whole plant, YP = young plant). (DOCX 66 kb)
Data Availability Statement
All the data collected and used in this paper are submitted as Additional files 1 and 2.


