Abstract
Background
To investigate the feasibility, effectiveness and safety of bilateral thoracic paravertebral block (TPVB) in the post anesthesia care unit (PACU) for pain relief in participants after laparotomy.
Methods
A single shot of bilateral TPVB with 25 ml of 0.2% ropivacaine and 5 mg dexamethasone in combination for both sides at the 8th thoracic transverse level (T8) was performed on 201 participants who complained moderate to severe pain on arrival to PACU after laparotomy. The visual analog scale (VAS) pain scores at rest and on cough, heart rate, blood pressure, and pulse oximetry before and after bilateral TPVB for up to 1 h were recorded. The VAS Pain scores at rest and on cough at 24 h after bilateral TPVB were also recorded.
Results
Bilateral TPVB was carried out successfully in all participants. The VAS pain scores at rest and on cough were 7.9 ± 1.6 and 8.7 ± 1.3 respectively pre-bilateral TPVB. The VAS pain scores at rest and on cough were significantly decreased to 1.1 ± 1.2 and 2.1 ± 1.6 respectively (P < 0.001) at 60 min after bilateral TPVB and to 2.1 ± 1.7 and 3.8 ± 1.9 at rest and on cough respectively ((P < 0.001) at 24 h after bilateral TPVB. At 10 min post-bilateral TPVB, only systolic blood pressure was reduced from 122 ± 19 mmHg to 111 ± 18 mmHg (P = 0.007) but then gradually became stable. No complications related to bilateral TPVB were observed.
Conclusion
Bilateral TPVB can be provided for pain relief to the participants who suffer from moderate to severe pain after upper laparotomy in the PACU.
Trial registration
Chinese Clinical Trial Registry: ChiCTR-ONN-16009229, Registered on 10 September 2016.
Keywords: Thoracic paravertebral block, Postoperative pain, Post anesthesia care unit
Background
Pain following laparotomy is a common complaint in the PACU. Good pain management improves participant satisfaction and facilitates shorter PACU/hospital stay [1]. Although pain management in the PACU has been improving with opioid-free strategies, opioids are still commonly used of analgesia for surgical participants with moderate to severe pain [2]. Intravenous opioids can provide rapid and effective analgesia but their undesired side effects, including pruritus, nausea and vomiting, urinary retention, and respiratory depression, result in discomfort or even lethal consequences [3, 4].
TPVB is a technique of which local anesthetic is injected into the thoracic paravertebral space. The thoracic paravertebral space is a wedge-shaped space lying on either side of the vertebral column that fills with adipose tissue containing intercostal nerve, dorsal ramus, intercostal vessels, rami communicantes, and sympathetic trunk [5]. Therefore, TPVB in either side could produce ipsilateral, segmental, somatic and sympathetic nerve blockade in contiguous thoracic dermatomes [5, 6]. It has been demonstrated that preoperative TPVB provides an excellent intraoperative and postoperative analgesia with less adverse effects in thoracic and abdominal surgery [7–12]. However, the effectiveness of TPVB as a rescue technique in the PACU for acute postoperative pain relief remains unknown. In this study, participants in the PACU who suffer moderate to severe pain after upper laparotomy were treated with a single-injection of local anesthetic via bilateral TPVB. Its effectiveness and safety profile were assessed prospectively.
Methods
The protocol was approved by the Ethics committee of West China Hospital, Sichuan University, China. Written informed consent was obtained from all participants prior to surgery. Participants were informed that they would be offered bilateral TPVB to be performed in the PACU if they reported moderate to severe pain which was not controlled adequately by the intraoperative and PACU analgesia that they had received. Inclusion criteria are: Age between 18 and 75 years; American Society of Anesthesiologists physical status 1 or 2; Laparotomy for hepatopancreatobiliary or gastrointestinal surgery; and participants with VAS pain score at rest ≥5 in the PACU. Exclusion criteria: allergy to local anesthetics; spinal deformity; coagulation disorders; local infection at the injection site. Accordingly, total 359 participants were recruited into this study.
After arrived in the operation room, heart rate, non-invasive blood pressure, and pulse oximetry were monitored in all participants. General anesthesia was induced with intravenous midazolam 0.05 mg/kg, sufentanyl 0.3–0.5 μg/kg, propofol 2–3 mg/kg and cis-atracurium 0.2 mg/kg. Anesthesia was maintained with sevoflurane or propofol together with remifentanil 0.2–0.3 μg/kg/min. Analgesia consisted of Paricoxib 40 mg administered 30 min before incision, and tramadol 100 mg intravenously 30 min before the end of surgery. A patient control analgesia pump was started 30 min before the end of surgery, containing 1 μg/ml sufentanyl and 5 mg/ml tramadol, with a continuous infusion rate of 2 ml/h, 0.5 ml bolus dose and lockout interval set to 15 min. All participants were extubated at the end of surgery prior to transferring to the PACU. The VAS pain score at rest/cough and modified Aldrete score were assessed as soon as participants arrived in the PACU. Those 201 participants with the rest VAS ≥ 5 and modified Aldrete score ≥ 9 were finally enrolled in the study (Fig. 1).
Fig. 1.

Participant recruitment flow chart
Participants were placed in the left lateral decubitus position. A 2- to 5- MHz curved array transducer (M-Turbo, Sonosite, Bothell, USA) was used to scan from the midline laterally to identify the following anatomical landmarks: spinous process, transverse process, and the paravertebral space at the target vertebral level. The 8th thoracic transverse process was identified using ultrasound guidance from the 12th thoracic transverse process. An in-plane needle guidance technique with a 10 cm, 22 G insulated needle (PAJUNK GmbH Medizin technologie, Geisingen, Germany) was used to perform the right lateral TPVB under aseptic conditions. After perforating the costotransverse ligament, 0.2% ropivacaine 25 ml mixed with 5 mg dexamethasone was injected after confirming a negative aspiration for blood. Anterior movement of the pleura indicated the appropriate spread of the local anaesthetic mixture in the paravertebral space (Fig. 2a, b). An out plane needle guidance technique was performed on the contralateral side using the same drug combination (Fig. 2c, d).
Fig. 2.

Ultrasound guided baliteral thoracic paravertebral block at T8 level. a and b illustrating the plane needle insertion to the right T8 paravertebral space. c and d illustrating the plane needle insertion to the left T8 paravertebral space. TP = Transverse process, TPV = Thoracic paravertebral space
The VAS pain score at rest and on cough, heart rate, blood pressure, and pulse oximetry before and after bilateral TPVB for up to 1 h were recorded by every 10 min. Hypotension was defined as a systolic blood pressure < 90 mmHg within 1 h after bilateral TPVB. The VAS pain score at rest and on cough 24 h after bilateral TPVB were also recorded.
Statistical analyses were performed with SAS for (Windows, version 9.13). The quantitative data were presented as mean ± SD. The categorical data were presented as frequency and/or percentage. Binary logistic regression and multivariate logistic regression models were used to identify risk factors of hypotension after bilateral TPVB.
Results
Effective bilateral TPVB was achieved in 139 male and 62 female participants with age 52.8 ± 12.1 years and BMI 22.0 ± 2.8 kg/m2. The length of surgery was 178.9 ± 62.7 min. No complications associated with the bilateral TPVB (pneumothorax, pleural puncture, nerve injury, or vascular puncture) were observed in this study.
The VAS scores at rest and on cough were rapidly reduced from 7.9 ± 1.6 and 8.7 ± 1.3 of baseline before bilateral TPVB to 3.3 ± 2.2 and 4.2 ± 2.3 10 min after bilateral TPVB respectively (P < 0.001) and then gradually decreased to 1.1 ± 1.2 and 2.1 ± 1.6 respectively (P < 0.001) at 1 h after injection (Fig. 3). No rescue analgesic was needed after bilateral TPVB in those patients after bilateral TPVB during their PACU stay. The VAS scores were 2.1 ± 1.6 and 3.8 ± 1.9 at rest and on cough 24 h after bilateral TPVB.
Fig. 3.

VAS pain scores at rest and cough before and after bilateral TPVB
Systolic blood pressure was significantly decreased to 111 ± 18 mmHg (P < 0.001) at 10 min after bilateral TPVB from the baseline of 123 ± 19 mmHg. By definition, hypotension (systolic blood pressure < 90 mmHg) occurred in 24 patients (11.9%). However, they were closely monitored and their systolic blood pressure were gradually returned to the baseline within 60 min after bilateral TPVB (Fig. 4). With a binary logistic regression model analysis, body weight, operative time, systolic blood pressure, diastolic blood pressure and mean blood pressure lower readings before bilateral TPVB were risk factors for hypotension (Table 1). Using multivariate logistic regression model analysis, low systolic blood pressure before bilateral TPVB and heavy body weight were indentified to be independent risk factors for hypotension after bilateral TPVB (Table 2). Diastolic blood pressure was to be a similar pattern trend change as systolic blood pressure (Fig. 4). No significant changes of SPO2 and heart rate were found throughout the study (Fig. 5).
Fig. 4.
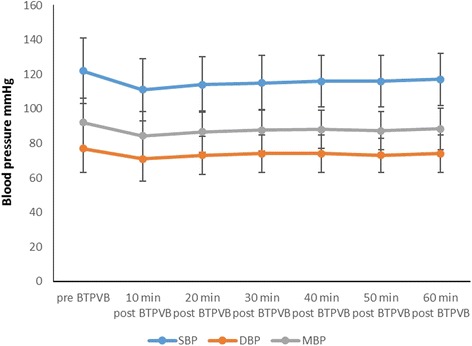
The changes of systolic blood pressure, diastolic blood pressure and mean blood pressure before and post bilateral TPVB
Table 1.
Binary logistic regression model for risk factors of hypotension after bilateral TPVB
| Variable | Hypotensive group 24 | Non-Hypotensive group 177 | P | OR |
|---|---|---|---|---|
| Sex(male/female) | 18/6 | 120/57 | 0.477 | 1.425 |
| Age | 51 ± 11 | 53 ± 12 | 0.465 | 0.987 |
| Body weight | 63.9 ± 8.8 | 58.8 ± 9.4 | 0.015* | 1.059 |
| Height | 166.2 ± 6.8 | 164.1 ± 7.4 | 0.202 | 1.039 |
| BMI | 22.9 ± 2.6 | 21.8 ± 2.8 | 0.053 | 1.170 |
| Operative time | 205 ± 49 | 174 ± 66 | 0.030* | 1.007 |
| Heart rate | 82 ± 14 | 80 ± 14 | 0.674 | 1.007 |
| Systolic blood pressure | 107 ± 16 | 125 ± 19 | <0.001* | 0.938 |
| Diastolic blood pressure | 71 ± 15 | 78 ± 13 | 0.011* | 0.957 |
| Mean blood pressure | 83 ± 14 | 94 ± 14 | 0.001* | 0.938 |
| VAS pain score rest | 7.6 ± 1.9 | 7.8 ± 1.6 | 0.618 | 0.937 |
| VAS pain score cough | 8.4 ± 1.6 | 8.7 ± 1.3 | 0.381 | 0.873 |
BMI Body Mass Index, VAS Visual Analog Scale,* P < 0.05
Table 2.
Multivariate logistic regression model for risk factors of hypotension
| Variable | Estimate | StdErr | Wald | P | OR |
|---|---|---|---|---|---|
| BW | 0.066 | 0.026 | 6.357 | 0.012 | 1.068 |
| Systolic blood pressure | −0.066 | 0.017 | 15.567 | <0.001 | 0.936 |
BW Body Weight
Fig. 5.
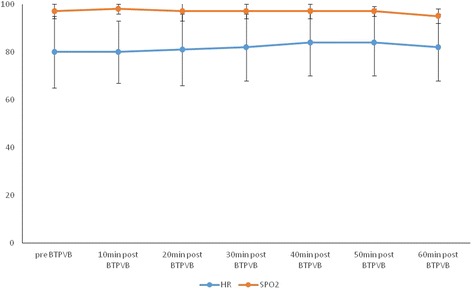
Heart rate and SPO2 before and after bilateral TPVB
Discussion
Our results showed that ultrasound-guided bilateral TPVB is an effective rescue analgesic technique for moderate and severe pain which is not adequately controlled by conventional intravenous analgesia after upper laparotomy.
It has been reported that in thoracic surgeries, unilateral TPVB was as effective as epidural analgesia but with much less side effects [13, 14]. Furthermore, considerable evidence showed that TPVB in addition to GA provide a better postoperative pain control with fewer adverse effects when compared GA alone in video-assisted thoracoscopic surgery and breast surgery [15–17]. However, it was not often reported to be used for postoperative pain relief after laparotomy under GA. Richardson et al. have reviewed 541 participants undergoing bilateral TPVB in 12 various studies, and they concluded that bilateral TPVB is safe and effective for thoracic and abdominal surgery [12]. However, the methods and outcomes in those studies are variable. Although many studies found that unilateral TPVB produced similar analgesia efficacy as compared with epidural block for thoracic surgery, a few studies have yet been compared bilateral TPVB with epidural analgesia for laparotomy which is generally considered to be a standard approach for postoperative pain relief after laparotomy. Recently Schreiber et al. found that there was modest analgesic advantage of thoracic epidural over bilateral TPVB for participants after open liver resection [18]. However, as the author also pointed out, technical risk and rare but serious complications such as epidural hematoma, perioperative hypotension related to epidural block can not be ignored. Furthermore, Schreiber et al. used a traditional landmark-based method for TPVB catheter insertion instead of ultrasound guidance or intraoperative placement by surgeons under direct vision, which may lead to more variable analgesic efficacy.
Instead of multiple injection at different thoracic level, a single injection of thoracic paravertebral block on each side at the T8 level was performed to reduce procedure time in a cohort of participants who were already in considerable pain. A previous study investigated the spread of local anesthetic in cadavers, and found no difference in paravertebral segment spread over 3–4 vertebral segments between a single versus dual-injection technique [19]. Our study showed that a single injection with large volume can provide good analgesic effect for large middle abdominal incision, indicating that multi-injections are not necessary.
Dynamic VAS scores at rest and on cough showed that bilateral TPVB provided effective analgesia with a rapid onset, supporting the use of bilateral TPVB in the PACU as an effective rescue analgesic technique. The rapid onset could be explained by the spinal nerve in the thoracic paravertebral space lacking both an epineurium and part of the perineurium, and with only a thin membranous root sheath. All these could enhance rapid local anaesthetic penetration, providing effect and rapid analgesia [20]. A mild decrease of systolic pressure without further treatment at 10 min after block and no changes of heart rate and SPO2 indicated that bilateral TPVB has minimal inhibitory effects on cardiorespiratory system.
Our study is limited as we assessed the efficacy of bilateral TPVB as a rescue technique for inadequate analgesia from our standard intravenous regimen, rather than comparing the efficacy of bilateral TPVB prior to surgery. A different study is required to test that research question. Furthermore, our study is observational without epidural block and or intravenous analgesic as the control groups and therefore we couldn’t conclude if bilateral TPVB gives better pain relief and has less side effects. Lastly, only a single shot was conducted and therefore, it is not known how the picture of bilateral TPVB with continuous infusions by catheter insertion is when compared with a single shot injection. Anyhow, our study showed that bilateral TPVB under the aid of ultrasound guide at the T8 level in the PACU provides immediate and good analgesia for patients suffering moderate or severe pain after laparotomy without significant side effects. However, due to the nature of the observatory study reported here, clinical trials are needed to further confirm its clinical safety and effectiveness.
Conclusions
In summary, the use of ultrasound guided bilateral TPVB as a rescue analgesic technique in the PACU is effective and provides rapid onset of analgesia.
Acknowledgements
The authors are grateful to the nurses in the PACU from the department of anesthesiology, West China Hospital, who contributed to this study.
Funding
This research was supported by a grant from the National Natural Science Foundation of China (No. 81601074).
Availability of data and materials
The raw data of the current study are available from the corresponding author on reasonable request.
Authors’ contributions
FL conceived and designed the study, performed the experiments and drafted the manuscript. HZ collected the experimental data and assisted with data analysis. YZ conceived the study. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethics committee of West China Hospital approved this study under number 2015/09. An informed consent was presented to all patients prior to enrollment in the study group. Written informed consent to participate were obtained from all the participants.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- PACU
Post anesthesia care unit
- T8
8th thoracic transverse level
- TPVB
Thoracic paravertebral block
- VAS
Visual analog scale.
Contributor Information
Fei Liu, Email: 30333870@qq.com.
HuanKai Zhang, Email: zhanghuankaimazui@163.com.
Yunxia Zuo, Phone: +86-18980601541, Email: 769574913@qq.com.
References
- 1.Bardiau FM, Taviaux NF, Albert A, Boogaerts JG, Stadler M. An intervention study to enhance postoperative pain management. Anesth Analg. 2003;96:179–185. doi: 10.1097/00000539-200301000-00038. [DOI] [PubMed] [Google Scholar]
- 2.Gandhi K, Baratta JL, Heitz JW, Schwenk ES, Vaghari B, Viscusi ER. Acute pain management in the postanesthesia care unit. Anesthesiol Clin. 2012;30:1–15. doi: 10.1016/j.anclin.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Aubrun F, Mazoit JX, Riou B. Postoperative intravenous morphine titration. Br J Anaesth. 2012;108:193–201. doi: 10.1093/bja/aer458. [DOI] [PubMed] [Google Scholar]
- 4.Ho KY, Gan TJ, et al. Opioid-related adverse effects and treatment options. In: Sinatra RS, de Leon-Casasola OA, Ginsberg B, et al., editors. Acute pain management. New York: Cambridge University Press; 2009. pp. 406–415. [Google Scholar]
- 5.Karmakar MK. Thoracic Paravertebral block. Anesthesiology. 2001;95:771–780. doi: 10.1097/00000542-200109000-00033. [DOI] [PubMed] [Google Scholar]
- 6.Krediet AC, Moayeri N, van Geffen GJ, Bruhn J, Renes S, Bigeleisen PE, Groen GJ. Different approaches to ultrasound-guided thoracic Paravertebral block: an illustrated review. Anesthesiology. 2015;123:459–474. doi: 10.1097/ALN.0000000000000747. [DOI] [PubMed] [Google Scholar]
- 7.Komatsu T, Kino A, Inoue M, Sowa T, Takahashi K, Fujinaga T. Paravertebral block for video-assisted thoracoscopic surgery: analgesic effectiveness and role in fast-track surgery. Int J Surg. 2014;12:936–939. doi: 10.1016/j.ijsu.2014.07.272. [DOI] [PubMed] [Google Scholar]
- 8.TerkawiAS, Tsang S, Sessler DI, Terkawi RS, Nunemaker MS, Durieux ME, Shilling A. Improving Analgesic Efficacy and Safety of Thoracic Paravertebral Block for Breast Surgery: A Mixed-Effects Meta-Analysis. Pain Physician. 2015;18:757–80. [PubMed]
- 9.Baik JS, Oh AY, Cho CW, Shin HJ, Han SH, Ryu JH. Thoracic Paravertebral block for Nephrectomy: a randomized, controlled. Observer-Blinded Study Pain Med. 2014;15:850–856. doi: 10.1111/pme.12320. [DOI] [PubMed] [Google Scholar]
- 10.Marqués A, García R, Gómez F, Giammaria F. Ultrasound-guided paravertebral block for management of abdominal pain after transarterial embolization using drug-eluting beads loaded with irinotecan. J Vasc Interv Radiol. 2013;24:1416–1417. doi: 10.1016/j.jvir.2013.04.033. [DOI] [PubMed] [Google Scholar]
- 11.Chen H, Liao Z, Fang Y, Niu B, Chen A, Cao F, Mei W, Tian Y. Continuous right thoracic paravertebral block following bolus initiation reduced postoperative pain after right-lobe hepatectomy: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2014;39:506–512. doi: 10.1097/AAP.0000000000000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richardson J, Lonnqvist PA, Naja Z. Bilateral thoracic paravertebral block: potential and practice. Br J Anaesth. 2011;106(2):164–171. doi: 10.1093/bja/aeq378. [DOI] [PubMed] [Google Scholar]
- 13.Ding X, Jin S, Niu X, Ren H, Fu S, Li Q. A comparison of the analgesia efficacy and side effects of Paravertebral compared with epidural blockade for Thoracotomy: an updated meta-analysis. PLoS One. 2014;9:e96233. doi: 10.1371/journal.pone.0096233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeung JH, Gates S, Naidu BV, Wilson MJ, Gao Smith F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016, 21;2:CD009121. [DOI] [PMC free article] [PubMed]
- 15.Matyal R, Montealegre-Gallegos M, Shnider M, Owais K, Sakamuri S, Shakil O, Shah V, Pawlowski J, Gangadharan S, Hess P. Preemptive ultrasound-guided paravertebral block and immediate postoperative lung function. Gen Thorac Cardiovasc Surg. 2015;63(1):43–8. [DOI] [PubMed]
- 16.Amlong C, Guy M, Schroeder KM, Donnelly MJ. Out-of-plane ultrasound-guided paravertebral blocks improve analgesic outcomes in patients undergoing video-assisted thoracoscopic surgery. Local Reg Anesth. 2015;15(8):123–128. doi: 10.2147/LRA.S86853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–852. doi: 10.1093/bja/aeq265. [DOI] [PubMed] [Google Scholar]
- 18.Schreiber KL, Chelly JE, Lang RS, Abuelkasem E, Geller DA, Marsh JW, Tsung A, Sakai T. Epidural versus Paravertebral nerve block for postoperative analgesia in patients undergoing open liver resection: a randomized clinical trial. Reg Anesth Pain Med. 2016;41(4):460–468. doi: 10.1097/AAP.0000000000000422. [DOI] [PubMed] [Google Scholar]
- 19.Cowie B, McGlade D, Ivanusic J, Barrington MJ. Ultrasound-guided thoracic paravertebral blockade: a cadaveric study. Anesth Analg. 2010;110:1735–1739. doi: 10.1213/ANE.0b013e3181dd58b0. [DOI] [PubMed] [Google Scholar]
- 20.Baik JS, Oh AY, Cho CW, Shin HJ, Han SH, Ryu JH. TPVB for nephrectomy: a randomized, controlled, observer-blinded study. Pain Med. 2014;15:850–856. doi: 10.1111/pme.12320. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data of the current study are available from the corresponding author on reasonable request.


