Abstract
This work is a narrative review of the evidence for an association of PTSD with incident cardiovascular disease (CVD) risk and the mechanisms that may carry that association, as well as the prevalence of PTSD due to CVD events and its associated prognostic risk. We discuss new research conducted since the publication of previous relevant systematic reviews and survey currently funded research in the portfolios of the two most active funders in the field. We conclude that PTSD is a risk factor for incident CVD, and a common psychiatric consequence of CVD events that may worsen CVD prognosis. There are many candidate mechanisms for the PTSD-CVD link, and a number of ongoing studies may soon point to the most important behavioral and physiological mechanisms to target in early phase intervention development. Similarly, targets are emerging for both individual and environmental interventions that may offset PTSD risk after CVD events.
Posttraumatic stress disorder (PTSD) is a psychiatric disorder that occurs in 7–8 % of civilians1,2 and as many as 20% of military veterans,3 although changes in diagnostic criteria may alter those estimates slightly. PTSD symptoms include re-experiencing symptoms, avoidance of trauma reminders, physiological hyperarousal, and persistent negative alterations in cognition and mood.4 Investigation of the association of PTSD symptoms with the development and prognosis of cardiovascular disease (CVD) began less than 20 years ago,5 but it has progressed rapidly thanks to the more established literature describing the effect of “stress” on cardiovascular risk.
Our current understanding of the link between PTSD and CVD is that PTSD is likely an independent risk factor for acute cardiac events including acute coronary syndromes (i.e., myocardial infarction or unstable angina) and possibly stroke. 6 The association of PTSD with CVD risk is likely carried through interacting behavioral and physiological mechanisms that relate to PTSD symptoms and, in turn, also influence CVD risk. It has also become clear that acute, potentially life-threatening CVD events can themselves cause PTSD, and that PTSD secondary to CVD events may be associated with increased risk for subsequent CVD events and mortality.7
This review will describe the emerging epidemiological, mechanistic, and intervention literature on the association of PTSD with (a) incident CVD risk in individuals exposed to potentially traumatic events such as combat and sexual assault, and (b) recurrent CVD risk in CVD patients who develop PTSD secondary to an acute CVD event. Where possible, we include the most recent systematic review and meta-analytic estimates, and report on research identified in systematic searches conducted July 2016. We also highlight important unanswered questions and active funded research in each area.
Epidemiological evidence for the link between PTSD and incident CVD risk
The majority of epidemiological studies to date have focused on risk for acute cardiac events specifically, and most have estimated the association in samples of veterans. Importantly, until recently, most studies were conducted in US samples.
PTSD and risk for incident acute cardiac events
A systematic review and meta-analysis of the prospective association of PTSD with incident acute cardiac events and cardiac-specific mortality included 5 published studies (N=401,712) that followed participants between 1 and 30 years, and found that PTSD was associated with a 53% increased risk for incident cardiac events or cardiac-specific mortality after adjustment for demographic, clinical, and psychosocial factors. After further adjustment for depression, the association was attenuated to 27%, but remained statistically significant. Most of the reviewed studies included samples comprised predominantly of male veterans with PTSD from the US, with more recent studies corroborating the increased CVD risk associated with PTSD in this population,8 but also for non-veteran populations from Europe and women.9,10 Since that meta-analysis was published, a retrospective cohort study that would have met its inclusion criteria was published. Berstianos and colleagues found a larger effect size than the meta-analytic estimate in 138,000 US military veterans aged 55 and older who were initially free of CVD, with an unadjusted 82% increased risk of incident MI events associated with PTSD diagnosis (3% of sample),11 which was attenuated to a 49% increased risk after adjustment for standard demographic, clinical, and psychiatric comorbidities. The size of the study and its effect size would likely revise the meta-analytic effect size estimate upward, suggesting that PTSD may be more strongly associated with incident CHD than previously thought, at least for older veterans.
PTSD and risk for incident stroke events
Given the overlapping risk factors and pathogenesis of acute coronary and cerebrovascular events, it is highly plausible that PTSD may also increase risk for stroke. A recent meta-analysis including two cohort studies revealed PTSD was associated with an increased risk of incident stroke (RR=2.36, 95% CI 2.11–2.65).12 Further, in the largest study (N=26,000), which was a national study of administrative records in Taiwan, established cardiovascular risk factors did not account for this relationship. Using the Danish National Patient Registry, a study found the association between PTSD and incident cases of ischemic stroke to be stronger in men (standardized incident rate= 2.4) than women (SIR= 1.3) after a median follow-up of seven years.9
New directions in epidemiological research on the PTSD-CVD link
PTSD is at least as common in women as it is in men. One of the limitations of the extant literature on PTSD and incident CVD events has been the reliance on secondary data analysis of overwhelmingly male samples of military veterans, with a few exceptions. Sumner and colleagues found that high levels of PTSD symptoms were associated with increased CVD risk (MI or stroke; with each comprising about half of the events in the combined outcome) in 50,000 women in the Nurses’ Health Study II (HR=1.60 [95% CI, 1.20–2.13]).10 Further, they found that health behaviors and medical risk factors explained nearly half of the association of PTSD with incident CVD. Given the sex differences in both PTSD and CVD risk and symptom presentation, more research in women is warranted.
Another important new development has been the investigation of the association of PTSD with new-onset venous thromboembolism (i.e., deep vein thrombosis and pulmonary embolism), as many of the risk factors for CVD events are also contributors to venous thromboembolism risk and the biological mechanisms that are likely responsible for the PTSD-CVD link are implicated in the development of venous thromboembolism as well. In another analysis of the Nurses’ Health Study II data, Sumner and colleagues found a graded association of PTSD symptoms with increased venous thromboembolism risk after adjustment for demographics, family history, and childhood adiposity.13 Women with the most severe PTSD symptoms had greater than double the venous thromboembolism risk of women who had never been exposed to trauma; HR=2.42 (95% CI, 1.83–3.20). However, unlike the association of PTSD with acute CVD events, PTSD’s association with venous thromboembolism did not appear to be explained by health behaviours or comorbidities. A nationwide study from Denmark also found the risk of incident venous thromboembolism to be higher in individuals with versus those without PTSD after a median follow-up of seven years (SIR=2.1, 95% CI, 1.7–2.7), although smoking was not taken into account as a confounding variable.9
Open questions in epidemiology
Is the PTSD-incident CVD link causal, and does PTSD treatment offset CVD risk?
Koenen and Galea recently called on the field to rigorously address the question of causality in the PTSD-CVD link,14 and Koenen and colleagues have offered a compelling roadmap for researchers.15 They and others have argued that many of the studies which support the association relied on lengthy follow-up periods, and measured PTSD and CVD risk factors only once at the outset, and that PTSD is strongly related to other psychiatric risk factors as well as poor health behaviours, all of which vary over time and influence CVD risk. These issues, as well as the fact that few studies have estimated the effect of PTSD onset on health behaviours or CVD risk markers, make it impossible to determine whether PTSD causes CVD based on existing evidence.
One means of approaching the open causality question has been to examine potential shared genetic risk factors for both PTSD and CVD. Several carefully performed studies, using data from the Vietnam Era Twin Registry, applied a co-twin design in order to control for unmeasured genetic and familial confounders that could be shared between PTSD and CVD risk. There was little evidence that the association between PTSD and the increased risk for incident coronary heart disease (CHD), confirmed by quantitative measures of reduced myocardial perfusion, was confounded by genetic or other familial or shared environmental factors; the association was also not explained by adverse health behaviours and depression, thereby suggesting PTSD is a casual risk factor for CHD.16 A similarly independent association of PTSD with low heart rate variability that, moreover, was reversible after PTSD symptom resolution, supports the notion that alterations in autonomic nervous system function could be a causal underlying mechanism linking PTSD with CVD risk in male veterans.17 In contrast, the authors found that PTSD is not causally linked to subclinical atherosclerosis (i.e., carotid intima-media thickness and a proinflammatory state, as measured by elevated C-reactive protein), but that familial or shared environmental factors better account for that relationship.18
A number of ongoing studies may shed light on the causal association of PTSD with CVD risk. First, Koenen and colleagues (R01 MH101269) are using state-of-the-science approaches for inferring causality by determining if new-onset PTSD in CVD-free women produces changes in CVD risk biomarkers, and whether such changes are reversed when PTSD remits. Second, Watkins and colleagues (R01 HL130322) will examine how changes in PTSD symptoms after military veterans receive Cognitive Processing Therapy affect autonomic nervous system dysregulation, chronic systemic inflammation, and vascular endothelial dysfunction. Third, Scherrer and colleagues (R01 HL125424) will analyze Veterans Administration clinic data to determine whether PTSD treatment reduces CVD risk. They will also assess the influence of PTSD treatment on health behaviours. Together, these studies may yield important insights into the causal nature and reversibility of the PTSD-CVD link, and provide treatment targets for early phase intervention research.
Other issues
More studies are needed from non-US populations and non-Veteran populations. Epidemiological studies should improve estimates through rigorous adjustment for depression and lifestyle, as well as established CVD risk factors. Further, substantial progress in risk assessment research has shown that in addition to relative risks, which are the most commonly reported effect sizes for PTSD’s relationship with CVD risk, absolute risk assessment and population based risks (PARs) are warranted.
Mechanisms of the PTSD-CVD association
Trauma
A simplified model of the link between PTSD and CVD begins with the cardiovascular consequences that accompany the experience of a traumatic event. Exaggerated activity in many of the physiological mechanisms of the PTSD-CVD link can be observed in the acute posttrauma phase, as they are the normative psychological, behavioural, and physiological responses to extremely stressful, threatening events.19 In many studies, the magnitude of these responses are predictive of the development of PTSD.20,21 For most individuals, this exaggerated activity will return to near pre-trauma levels relatively quickly and, by 1 month post-trauma, will have normalized. For those who develop PTSD, the cognitive, behavioral, and physiological dysregulation continues.22
At the cognitive level, alterations in perceptions of general safety or vulnerability of the self, and the sources and predictability of threat in the world set the stage for a widening of the network of associations that cause internal or external stimuli to activate the individual’s fear network.23,24 This activation initiates the physiological cascade that defines the fight or flight response to threat.22 Simultaneously, the baseline physiological readiness to respond to threat cues is heightened, with observable differences in resting indicators of autonomic and HPA activation.25 When threat cues are perceived, physiological reactivity to those cues is exaggerated, mimicking the initial adaptive response to the traumatic event.26,27
Physiological mechanisms
Cardiovascular demand
Autonomic balance (i.e., the balance of sympathetic and parasympathetic activity) may be disrupted in PTSD, resulting in increased basal activity and intermittently exaggerated demand on the cardiovascular system.
Sympathetic nervous system activity appears to be exaggerated in PTSD. Patients with PTSD exhibit higher catecholamine levels and higher heart rate relative to those without PTSD,28 particularly after exposure to reminders of their index traumatic event.29,30 Decades of research point to heightened activation of the sympathetic nervous system in PTSD,31 but most of the evidence comes from laboratory studies showing that trauma reminders cause sympathetic nervous system activation, and large increases in heart rate in particular [i.e., a meta-analysis of lab studies suggests the median heart rate increase associated with trauma reminders is 10 beats per minute31].32,33,27 Short-term increases in heart rate magnify shear stress on the endothelium which, through the rupturing of a vulnerable atherosclerotic plaque, may trigger CVD events. High heart rate is a major risk factor for recurrent cardiac events and mortality in CVD patients.34
The parasympathetic nervous system serves to dampen sympathetic reactions to stress and promote calm behavioural states, and parasympathetic nervous system activation appears to be hampered in PTSD. Heart rate variability (HRV) is the most commonly assessed indicator of parasympathetic nervous system activity, and PTSD has been associated with low mean HRV (an index of parasympathetic nervous system withdrawal) on 24-hour Holter monitoring.35 Further, patients with PTSD have been shown to exhibit a substantial acute decrease in HRV when exposed to trauma cues in the lab, suggesting parasympathetic nervous system withdrawal. More evidence for autonomic dysregulation in PTSD include baroreflex dysfunction and increased QT intervals on ECG.36 These maladaptive alterations in threat responding may become chronic, and have direct links to CVD risk. Low HRV and reduced baroreflex sensitivity have been linked with carotid atherosclerosis, inflammation and hypercoagulability,37–39 and increased risk of incident and recurrent CVD. 40,41 Further, increased QT variability is a predictor of sudden cardiac death.42
Similarly, alterations in the activity of the hypothalamic-pituitary-adrenal (HPA) axis in patients with PTSD has been documented, including lower basal cortisol levels and lower daily cortisol output,43,44 but exaggerated cortisol response to stress. HPA dysregulation has been implicated in the development of heart failure and cardiac ischemia and has been associated with CVD mortality. HPA dysregulation influences blood pressure and coagulation, in part due to hormone secretions that directly effect the heart, blood vessels, and platelet activation.45 Over time, HPA dysregulation may result in increased negative feedback sensitivity of glucocorticoid receptors in the stress-response system, decreased glucocorticoid responsiveness,46 and lower urinary and plasma cortisol levels.
Cardiovascular capacity
Chronic increases in cardiovascular demand degrade the capacity of the cardiovascular system to support that increased demand. The accumulation of time spent in a state of physiological hyperarousal and intermittent periods of exaggerated physiological reactivity to threat cues is thought to contribute to CVD risk through the development of a systemic proinflammatory state, and thus more rapid progression of atherosclerosis, endothelial dysfunction, hypertension, and more pronounced coronary ischemia under stress.
One of the earliest markers of degraded capacity to support increased cardiovascular demand is endothelial dysfunction. Endothelial cells form the inner lining of blood vessels, and are responsible for vasodilation and vasoconstriction in response to stimuli that determine cardiovascular demand. Endothelial dysfunction is a key early contributor to CVD risk through promotion of atherosclerosis, as insufficient vasodilation under conditions of high cardiovascular demand results in increased sheer stress on the arterial wall, inflammatory response, and activation of prothrombotic processes. Two studies have assessed the association of PTSD with endothelial dysfunction,47,48 and both found clinically significant reduction in flow mediated dilation of the brachial artery in participants with PTSD.
Two important studies are investigating the role of endothelial dysfunction in the PTSD-CVD link. Vaccarino and colleagues (R01 HL125246) are conducting a follow-up study of 281 male twin pairs (562 individuals) from the Vietnam Era Twin Registry 10 years after their baseline visit to determine whether PTSD is related to worsening of ischemic heart disease on PET myocardial perfusion imaging and its association with vascular and immune responses to traumatic memory tasks (i.e., peripheral vasoconstriction and biomarkers of endothelial injury and inflammation). Soufer and colleagues are conducting a VA-funded study (I01 CX000935) to determine whether PTSD diagnosis is associated with endothelial dysfunction during standard hyperemic probe and during emotional stress in military veterans, and whether change in PTSD symptom severity over 1 year is associated with change in the endothelial response to those challenges. They will also test the association of sympathetic, parasympathetic, and HPA axis activity with endothelial response.
PTSD symptom severity has been associated with a proinflammatory state.49–51 Increased inflammation is a key contributor to atherosclerosis, the process underlying atherothrombotic CVD, and some of the inflammatory markers that are elevated in PTSD have been linked to CVD events.52 In agreement with this, Ahmadi and colleagues found a dose-response relationship between PTSD and coronary artery calcium (CAC), and that the association of PTSD with mortality was strongest at high levels of CAC.53
A large body of cross-sectional studies exists on the associations of PTSD symptoms with a variety of inflammatory biomarkers.54–56 In a meta-analysis, significantly higher levels of IL-1β, IL-6, and interferon γ were found in patients with PTSD relative to controls, whereas IL-2, IL-4, IL-8, IL-10, soluble IL-2R, soluble IL-6R, C-reactive protein, and TNF-α did not differ by PTSD status.57 Although that meta-analysis suggested no significant association between PTSD and CRP in peripheral blood, Michopoulos et al reported that genetic variability in the CRP gene is associated with serum CRP concentration and PTSD symptom severity (N=2,698), as one SNP within the CRP gene (rs1130864) was significantly associated with increased PTSD symptoms, particularly hyperarousal.58 This suggests that there may be a genotype effect in the association of PTSD and CRP.
A recent prospective study of PTSD and inflammation further complicates the picture. Levels of C-reactive protein and PTSD symptoms were assessed pre- and post-deployment among 2,600 US Marines.59 Each 10-point increment in pre-deployment levels of C-reactive protein predicted a 51% greater likelihood of having any PTSD symptoms 3 months post-deployment. Related research suggests that dysregulations of the glucocorticoid signaling cascade, which influences inflammatory cytokines, might represent a vulnerability factor for the development of PTSD.60
Regarding putative cellular and molecular mechanisms underlying inflammatory processes in PTSD, chronically elevated catecholamine levels and a redistribution of catecholamine receptors, can increase cytokine production via stimulation of β-adrenergic receptors on immune cells and activity of the transcription factor nuclear factor-kappaB (NF-κB); the latter is also modulated by cortisol function.61 In agreement with this, higher NF-κB DNA binding activity of immune cells correlated positively with PTSD symptoms in women with early life abuse, but inversely with glucocorticoid sensitivity of in vitro stimulated pro-inflammatory cytokine production compatible with enhanced inflammatory system activity.62
Given the autonomic, HPA axis, endothelial, and inflammatory correlates of PTSD, it is not surprising that PTSD has been associated with increased clinic and ambulatory blood pressure, as the increased cardiovascular demand and decreased arterial capacity that define these correlates are the primary determinants of blood pressure. Most of the research on PTSD and risk for incident hypertension has been conducted in US veterans,63 with some studies finding resting systolic/diastolic BP differences as great as 11/9mmHg higher among those with PTSD.64 Those studies were mostly cross-sectional, but Burg and colleagues have found that PTSD was prospectively associated with at least a 20% increased risk for new onset hypertension in 250,000 veterans in VA health records data.65 Most importantly, they found that veterans with PTSD who received PTSD treatment were at no greater risk than those without PTSD for new-onset hypertension.
A hypercoagulable state (i.e., too much coagulation activity and/or too little fibrinolytic activity) along with hyperactive (i.e. “sticky”) platelets might facilitate acute atherothrombotic CVD events in conjunction with endothelial dysfunction and inflammatory processes in PTSD.66 In one study, patients with PTSD had significantly higher levels of soluble tissue factor (median/IQR) than age, gender, and trauma-matched controls [163 pg/ml (142–256) vs 128 pg/ml (111–145); ].67 In contrast, there were no significant group differences in terms of fibrinogen, D-dimer, or activity levels of clotting factors VII, VIII, and XII, however, both fibrinogen and clotting factor VIII activity were linked to PTSD symptom severity and degree of hyperarousal in patients with PTSD.68 Among civilians with war-related chronic PTSD, von Willebrand factor antigen levels were significantly higher in PTSD than in non-PTSD controls and, moreover, the most severe PTSD cases had higher von Willebrand factor antigen and clotting factor VIII activity levels than those with less severe PTSD symptoms and controls.69 Baseline platelet activity did not differ between combat veterans with and without PTSD,70 but platelets from PTSD patients showed exaggerated reactivity to in vitro epinephrine/ADP stimulation mediated by the α2-adrenergic receptor.71
Hypercoagulability may be particularly important in CVD patients. In a study of patients being evaluated for acute coronary syndromes in the emergency department, pre-existing PTSD symptoms were associated with activated partial thromboplastin time.72 Procoagulant reactivity has also been observed under stress in response to a trauma-specific interview in patients with acute coronary syndrome-related PTSD.73
Behavioural factors
There are several plausible behavioral mechanisms linking PTSD with risk of CVD events, many of which likely interact with physiological mechanisms in a vicious cycle. PTSD has been associated with health risk behaviours, including smoking, physical inactivity, and obesity,74–76 as well as nonadherence to CVD risk-reducing medications. 77–79
Metabolic syndrome is an important risk factor for CVD. It is defined by central obesity, high blood pressure, low high density lipoprotein (HDL) cholesterol, elevated triglycerides and hyperglycemia. A recent meta-analysis of 9 studies (total N= 16,500) found that the prevalence of metabolic syndrome was significantly greater in individuals with PTSD relative to population-based controls (RR = 1.82; 95% CI = 1.72–1.92; p < 0.001).80 Likewise, type 2 diabetes mellitus is a powerful predictor of CVD risk. In a recent meta-analysis (N= 150,000), PTSD was associated with a 50% increased risk for type 2 diabetes (5 studies, RR = 1.49, 95% CI = 1.17–1.89).81
Sleep difficulties are common in PTSD, and may be associated with CVD risk. In a meta-analysis of 15 studies (24 cohorts; N= 475,000) short duration of sleep was associated with incident CHD (RR 1.48, 95% CI 1.22–1.80) and stroke (1.15, 1.00–1.31).82 The role of short or disrupted sleep in the PTSD-CVD link is an active area of mechanistic research. Burg and colleagues (R01 HL125587) will test whether objectively measured poor sleep may explain differential ambulatory blood pressure (BP) progression over 2 years, and whether successful PTSD treatment may improve sleep and BP progression.
An important behavioural pathway by which PTSD may influence CVD risk is through nonadherence to medications. PTSD has been associated with medication nonadherence in patients with acute coronary syndromes,83,84 transplant,85 stroke/TIA,86 established CVD, 75 and hypertension.87 Researchers have hypothesized that cognitive deficits as well as avoidance of medications as reminders of risk for CVD events may underlie this association.
For those with PTSD induced by acute CVD events, the very medications intended to be protective may serve as aversive reminders of the traumatic index stroke event, thereby prompting nonadherence.88,89 Participants with stroke-induced PTSD were 2.7 times (95% CI 1.7 – 4.2) more likely than those without to report nonadherence to medications. Similarly, patients with high acute coronary syndrome-induced PTSD symptom had poor aspirin adherence at 1-year follow-up.79
Open questions in mechanisms
A number of mechanisms for the link between PTSD and CVD risk have been identified, but as putative mechanisms proliferate, questions abound concerning the interactions among them and their relative importance as potential therapeutic targets. One example of research on the interaction of behavioral and physiological mechanisms in the PTSD-CVD link in a high risk CVD population is described below.
PTSD can be caused by CVD events
Although the layman (or cardiologist, or neurologist) may not judge CVD events to be sufficiently traumatic to cause PTSD, the DSM-IV and available meta-analytic data suggest that clinically relevant PTSD symptoms are common sequelae of CVD events. A growing body of literature has focused on PTSD due to CVD events, and its association with recurrent CVD risk. PTSD rates and short-term CVD risk are higher in this population than in the general population, but there are conceptual and diagnostic issues (first raised in research on PTSD secondary to cancer diagnosis and treatment) that complicate the study of PTSD secondary to an acute life-threatening illness. These issues and their implications have been elaborated recently for both cancer (See Cordova, Riba, & Spiegel review, Lancet Psychiatry, submitted90) and CVD.88
Epidemiological evidence for the link between PTSD secondary to CVD events and recurrent CVD risk
In a meta-analysis of 24 studies (N= 2383), Edmondson and colleagues found a 12% prevalence of PTSD secondary to acute coronary syndromes. Further, across the 3 studies that estimated the association, PTSD was associated with a doubling of risk for acute coronary syndromes recurrence or mortality (95% CI, 1.69–2.37) after adjustment for demographic, clinical, and psychosocial risk factors, including depression.91 Edmondson, Kronish, and colleagues (HL117832, HL128310, HL123368) are currently conducting a series of studies in a large (N=1,700) cohort of acute coronary syndromes patients to determine the prevalence and predictors of PTSD in acute coronary syndromes patients, and to test mechanisms of the PTSD-acute coronary syndromes recurrence risk association. In particular, they will focus on objectively measured adherence to medications, and the interaction of nonadherence to beta-blockers and the experience of intrusive thoughts (as measured by electronic momentary assessment) on ambulatory ECG markers of autonomic imbalance in the first months after an acute coronary syndromes event. They will also test the roles of physical activity and sleep.
A meta-analysis of 7 studies (N = 1,014 patients) found that 23% (95% CI, 15–34%) of mild to moderate stroke/transient ischemic attack (TIA) survivors develop PTSD in the first year after stroke.77,92–97 More recently, the first study to assess PTSD in a sample comprised exclusively of TIA patients found that 29% screened positive for PTSD at 3 months post-TIA.98 It is not clear whether stroke-induced PTSD is associated with secondary CVD risk, but Edmondson and Kronish (HL132347) will test the association in a large cohort of stroke/TIA patients (N=1000) followed for 1 year, and will determine whether medication nonadherence explains any association that is found.
Other acute cardiovascular events may also induce PTSD symptoms. Indeed, emerging qualitative research suggests that pulmonary embolism may provoke symptoms of PTSD.99
Open questions in PTSD secondary to CVD events
Research on PTSD secondary to CVD events is less advanced than research on the PTSD-incident CVD link, but the two are obviously strongly related. It is important to determine whether mechanisms for the likely PTSD-recurrent CVD association are the same as those that carry the PTSD-incident CVD association. The excess recurrence risk associated with PTSD after CVD events appears to be conferred in the first year after the index CVD event, which is a much shorter time frame than many of the putative PTSD-incident CVD mechanisms require.
Offsetting the CVD recurrence risk likely associated with PTSD is important,100 but offsetting risk for PTSD itself is preferable, and some interventions have shown promise.101 von Kanel and colleagues are currently conducting a study to test whether a single 45-min counseling session, targeting acute coronary syndrome-triggered traumatic reactions, delivered bedside in the coronary care unit within 48 hours reduces posttraumatic symptoms at 3 and 12 months follow-up.102 Hospital environment factors may also be targets for decreasing CVD-induced PTSD risk, as objectively measured overcrowding in the emergency department, and the perception of the hospital environment as hectic have been shown to increase risk for the development of PTSD.103,104
Summary
This paper offers an overview of the existing evidence for the association between PTSD and CVD risk, the mechanisms that may carry that association, and the risk of PTSD due to CVD events. It also highlighted a number of the innovative studies on target mechanisms currently being conducted with support from NHLBI and the VA. Neither our review of the literature nor our survey of ongoing research were comprehensive, but together they provide a reasonable framework for understanding the state of the field and the most fruitful directions forward.
On balance, existing epidemiological data suggest that PTSD is a risk factor for incident CVD and that the association is carried by mechanisms that characterize the human stress response, in conjunction with disrupted behavioral and lifestyle factors. Further, acute CVD events often cause PTSD, which in turn increases the risk for recurrent CVD events. The immediate post-CVD event period may be a particularly fertile area for intervention, as preventing PTSD development may be more efficient than treating PTSD for improving CVD and psychiatric prognoses simultaneously. A number of targets are emerging for both individual and environmental interventions that may offset PTSD risk after CVD events.
PTSD is a relatively unique psychiatric disorder, in that it has a clear onset after a traumatic event. Therefore, if it is a causal risk factor for CVD, interventions to offset PTSD risk or disrupt its behavioral and physiological sequelae should be prioritized. We do not know whether the association of PTSD with the risk of incident CVD is causal, and no RCT has been conducted to determine whether PTSD treatment can offset CVD risk. Further, although many candidate mechanisms for the PTSD-CVD association have been identified, we do not know which mechanisms are the most important targets for offsetting CVD risk when PTSD is present. Innovative research on the dynamics of PTSD symptoms and CV dysfunction may yield those targets soon.
These unanswered questions are critical to address, as the field of behavioral medicine has previously experienced the consequences of identifying depression as a psychiatric risk factor for CVD, observing potential mechanisms by which depression increases CVD risk, and unfortunately, not yet being able to translate those findings into effective CVD risk-reducing therapies. Therefore, the field must determine whether PTSD is a cause of CVD, conduct systematic investigations into the interactions of behavioral and biological mechanisms of the PTSD-CVD link, and, most importantly, carry out early phase intervention trials powered to influence those mechanisms and ultimately offset CVD risk.
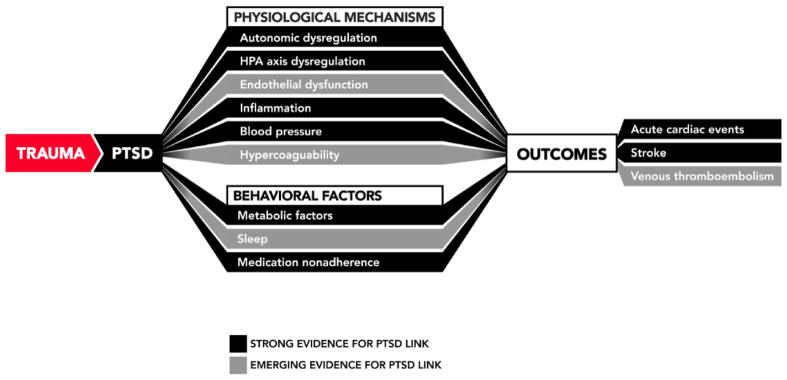
Figure 1. Mechanistic model of the PTSD-CVD association.
Figure 1 illustrates the current state of evidence linking PTSD with risk for CVD events, with mechanistic pathways depicted by arrows with designations for the current strength of evidence for the association. Although most research to date on PTSD and mechanisms of CVD risk has been cross-sectional, we attempt to illustrate the associations in a logical causal chain that synthesizes known temporal associations among mechanisms. The temporal order and causal relations among these variables should be tested in future research.
Table 1.
Associations supported by meta-analytic evidence
| Antecedent | Outcomes | Meta-analytic support |
|---|---|---|
| PTSD | CVD events | |
| Incident CHD | HR= 1.55 (95% CI 1.34–1.79); with adjustment for depression, HR= 1.27 (95% CI 1.08–1.49) Edmondson et al., 2013 |
|
| Incident stroke/TIA | RR= 2.36 (95% CI 2.11–2.65) Emdin et al., 2016 |
|
| Incident VTE | No | |
| Recurrent MI/unstable angina/mortality | RR= 2.0 (95% CI, 1.69–2.37) Edmondson et al., 2013 |
|
| Recurrent stroke/TIA | No | |
| Mechanisms | ||
| Type 2 diabetes | RR = 1.49, 95% CI = 1.17–1.89) Vancampfort et al., 2016 |
|
| Metabolic syndrome | OR= RR = 1.82; 95% CI = 1.72 –.92 Rosenbaum et al., 2015 |
|
| Blood pressure | Systolic; Unweighted d (SE)= .13 (.07) Diastolic; Unweighted d (SE) = .39 (.21) Buckley et al., 2001 |
|
| Inflammation | Greater IL-1β, IL-6, and interferon γ in PTSD Passos et al., 2015 |
|
| Cortisol | Unclear Klassens et al., 2012; Morris et al., 2012 |
|
| Endothelial dysfunction | No | |
| Obesity | OR = 1.35 (95% CI 1.05–1.74) Bartoli et al., 2015 |
|
| Smoking | 6/7 studies showed positive associations; ORs ranged 2.04–4.52 Fu et al., 2007 |
|
| Sleep | No | |
| Medication nonadherence | No | |
| ACS | PTSD | 12% screen positive (95% CI, 9%–16%) Edmondson et al., 2013 |
| Stroke/TIA | 23% screen positive (95% CI, 16–33%) Edmondson et. al., 2013 |
|
| VTE | No |
Key Challenges.
Is PTSD a cause of incident or recurrent CVD?
Can CVD surveillance in PTSD improve outcomes?
What are the most important behavioral or biological mechanisms to target for CVD risk reduction in PTSD?
Does PTSD treatment offset CVD risk?
Can individual or environmental interventions reduce PTSD risk in survivors of acute CVD events?
Search strategy.
Potentially relevant articles were identified by updating the searches for three previous systematic reviews on 1) stress/PTSD and coronary heart disease (2011 to 2016), 2) PTSD and acute coronary syndrome (2012 to 2016), and 3) PTSD and stroke (2013 to 2016). In all cases, the databases searched were Ovid MEDLINE, PsycINFO, PILOTS, and Scopus, and the updated searches were run on July 7, 2016. For each search all relevant subject heading and free text terms were used to represent PTSD OR stress, AND coronary heart disease, OR acute coronary syndrome OR stroke. The total number of references retrieved was 2,204 and 1,589 after duplicates had been removed. We identified currently funded research from two of the most active funders of the field-the National Institutes of Health and the Veterans Administration, using NIH Reporter.
Acknowledgments
Dr. Edmondson was supported by NIH grants HL128497, HL117832, HL128310, and HL132347 from the National Heart, Lung, and Blood Institute and grant AG052175 from the National Institute on Aging.
Footnotes
Conflict of interest: Dr. Edmondson has nothing to disclose. Dr. von Kanel received honoraria from Vifor AG, Switzerland, for services that are unrelated to the content of this article.
Author contributions: DE completed the literature search and initial manuscript draft, DE and RvK wrote the manuscript and are responsible for the final product.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kessler RC, Birnbaum HG, Demler O, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R) Biol Psychiatry. 2005;58:668–76. doi: 10.1016/j.biopsych.2005.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 3.Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health. 2009;99:1651–8. doi: 10.2105/AJPH.2008.150284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. DSM 5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 5.Gander M-L, von Kanel R. Myocardial infarction and post-traumatic stress disorder: frequency, outcome, and atherosclerotic mechanisms. Eur J Cardiovasc Prev Rehabil. 2006;13:165–72. doi: 10.1097/01.hjr.0000214606.60995.46. [DOI] [PubMed] [Google Scholar]
- 6.Edmondson DE, Kronish IM, Shaffer JA, Falzon L, Burg MM. Posttraumatic Stress Disorder and Risk for Coronary Heart Disease: A Meta-analytic Review. Am Heart J. 2013;166:806–14. doi: 10.1016/j.ahj.2013.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS ONE [Electronic Resource] 2012;7:e38915. doi: 10.1371/journal.pone.0038915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beristianos MH, Yaffe K, Cohen B, Byers AL. PTSD and Risk of Incident Cardiovascular Disease in Aging Veterans. Am J Geriatr Psychiatry. 2016;24:192–200. doi: 10.1016/j.jagp.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Gradus JL, Farkas DK, Svensson E, et al. Associations between stress disorders and cardiovascular disease events in the Danish population. BMJ Open. 2015;5:e009334. doi: 10.1136/bmjopen-2015-009334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sumner JA, Kubzansky LD, Elkind MS, et al. Trauma Exposure and Posttraumatic Stress Disorder Symptoms Predict Onset of Cardiovascular Events in Women. Circulation. 2015;132:251–9. doi: 10.1161/CIRCULATIONAHA.114.014492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beristianos MH, Yaffe K, Cohen B, Byers AL. PTSD and Risk of Incident Cardiovascular Disease in Aging Veterans. Am J Geriatr Psychiatry. 2016;24:192–200. doi: 10.1016/j.jagp.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 12.Emdin CA, Odutayo A, Wong CX, Tran J, Hsiao AJ, Hunn BH. Meta-Analysis of Anxiety as a Risk Factor for Cardiovascular Disease. m J Cardiol. 2016;118:511–9. doi: 10.1016/j.amjcard.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 13.Sumner JA, Kubzansky LD, Kabrhel C, et al. Associations of Trauma Exposure and Posttraumatic Stress Symptoms With Venous Thromboembolism Over 22 Years in Women. J Am Heart Assoc. 2016;5:e003197. doi: 10.1161/JAHA.116.003197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koenen KC, Galea S. Post-traumatic stress disorder and chronic disease: open questions and future directions. Soc Psychiatry Psychiatr Epidemiol. 2015;50:511–3. doi: 10.1007/s00127-015-1035-0. [DOI] [PubMed] [Google Scholar]
- 15.Koenen KC, Sumner JA, Gilsanz P, et al. Post-traumatic stress disorder and cardiometabolic disease: improving causal inference to inform practice. Psychol Med. 2016:1–17. doi: 10.1017/S0033291716002294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaccarino V, Goldberg J, Rooks C, et al. Posttraumatic Stress Disorder and Incidence of Coronary Heart Disease: A Twin Study. J Am Coll Cardiol. 2013;62:970–8. doi: 10.1016/j.jacc.2013.04.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah AJ, Lampert R, Goldberg J, Veledar E, Bremner JD, Vaccarino V. Posttraumatic Stress Disorder and Impaired Autonomic Modulation in Male Twins. Biol Psychiatry. 2013;73:1103–10. doi: 10.1016/j.biopsych.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plantinga L, Bremner JD, Miller AH, et al. Association between posttraumatic stress disorder and inflammation: a twin study. Brain Behav Immun. 2013;30:125–32. doi: 10.1016/j.bbi.2013.01.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shalev A, Sahar T, Freedman S, et al. A prospective study of heart rate response following trauma and the subsequent development of posttraumatic stress disorder. Arch Gen psychiatry. 1998;55:553–9. doi: 10.1001/archpsyc.55.6.553. [DOI] [PubMed] [Google Scholar]
- 20.Shalev AY, Peri T, Brandes D, Freedman S, Orr SP, Pitman RK. Auditory startle response in trauma survivors with posttraumatic stress disorder: a prospective study. Am J Psychiatry. 2000;157:255–61. doi: 10.1176/appi.ajp.157.2.255. [DOI] [PubMed] [Google Scholar]
- 21.Yehuda R, McFarlane A, Shalev A. Predicting the development of posttraumatic stress disorder from the acute response to a traumatic event. Biol Psychiatry. 1998;44:1305–13. doi: 10.1016/s0006-3223(98)00276-5. [DOI] [PubMed] [Google Scholar]
- 22.Yehuda R, LeDoux J. Response Variation following Trauma: A Translational Neuroscience Approach to Understanding PTSD. Neuron. 2007;56:19–32. doi: 10.1016/j.neuron.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Dalgleish T. Cognitive approaches to posttraumatic stress disorder: the evolution of multirepresentational theorizing. Psychol Bull. 2004;130:228. doi: 10.1037/0033-2909.130.2.228. [DOI] [PubMed] [Google Scholar]
- 24.Foa EB, Steketee G, Rothbaum BO. Behavioral/cognitive conceptualizations of post-traumatic stress disorder. Behav Ther. 1989;20:155–76. [Google Scholar]
- 25.De Kloet C, Vermetten E, Geuze E, Kavelaars A, Heijnen C, Westenberg H. Assessment of HPA-axis function in posttraumatic stress disorder: pharmacological and non-pharmacological challenge tests, a review. J Psychiatr Res. 2006;40:550–67. doi: 10.1016/j.jpsychires.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Lindauer RTL, van Meijel EPM, Jalink M, Olff M, Carlier IVE, Gersons BPR. Heart Rate Responsivity to Script-Driven Imagery in Posttraumatic Stress Disorder: Specificity of Response and Effects of Psychotherapy. Psychosom Med. 2006;68:33–40. doi: 10.1097/01.psy.0000188566.35902.e7. [DOI] [PubMed] [Google Scholar]
- 27.Liberzon I, Abelson JL, Flagel SB, Raz J, Young EA. Neuroendocrine and Psychophysiologic Responses in PTSD: A Symptom Provocation Study. Neuropsychopharmacology. 1999;21:40–50. doi: 10.1016/S0893-133X(98)00128-6. [DOI] [PubMed] [Google Scholar]
- 28.Buckley TC, Kaloupek DG. A meta-analytic examination of basal cardiovascular activity in posttraumatic stress disorder. Psychosom Med. 2001;63:585–94. doi: 10.1097/00006842-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Pitman RK, Lanes DM, Williston SK, et al. Psychophysiologic Assessment of Posttraumatic Stress Disorder in Breast Cancer Patients. Psychosomatics. 2001;42:133–40. doi: 10.1176/appi.psy.42.2.133. [DOI] [PubMed] [Google Scholar]
- 30.Pitman RK, Orr SP, Forgue DF, de Jong JB, Claiborn JM. Psychophysiologic assessment of posttraumatic stress disorder imagery in Vietnam combat veterans. Arch Gen Psychiatry. 1987;44:970. doi: 10.1001/archpsyc.1987.01800230050009. [DOI] [PubMed] [Google Scholar]
- 31.Pole N, Pole N. The psychophysiology of posttraumatic stress disorder: a meta-analysis. Psychol Bull. 2007;133:725–46. doi: 10.1037/0033-2909.133.5.725. [DOI] [PubMed] [Google Scholar]
- 32.Murburg MM, McFall ME, Lewis N, Veith RC. Plasma norepinephrine kinetics in patients with posttraumatic stress disorder. Biol Psychiatry. 1995;38:819–25. doi: 10.1016/0006-3223(95)00044-5. [DOI] [PubMed] [Google Scholar]
- 33.McFall ME, Veith RC, Murburg MM. Basal sympathoadrenal function in posttraumatic distress disorder. Biol Psychiatry. 1992;31:1050–6. doi: 10.1016/0006-3223(92)90097-j. [DOI] [PubMed] [Google Scholar]
- 34.Fox KM. Current status: heart rate as a treatable risk factor. Eur Heart J. 2011;13(suppl C):C30–C6. [Google Scholar]
- 35.Lakusic N, Fuckar K, Mahovic D, Cerovec D, Majsec M, Stancin N. Characteristics of heart rate variability in war veterans with post-traumatic stress disorder after myocardial infarction. Mil Med. 2007;172:1190–3. doi: 10.7205/milmed.172.11.1190. [DOI] [PubMed] [Google Scholar]
- 36.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice:: The emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–51. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 37.Haensel A, Mills PJ, Nelesen RA, Ziegler MG, Dimsdale JE. The relationship between heart rate variability and inflammatory markers in cardiovascular diseases. Psychoneuroendocrinology. 2008;33:1305–12. doi: 10.1016/j.psyneuen.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.von Kanel R, Nelesen RA, Ziegler MG, Mausbach BT, Mills PJ, Dimsdale JE. Relation of autonomic activity to plasminogen activator inhibitor-1 plasma concentration and the role of body mass index. Blood Coagul Fibrinolysis. 2007;18:353–9. doi: 10.1097/MBC.0b013e3281139c67. [DOI] [PubMed] [Google Scholar]
- 39.von Kanel R, Orth-Gomer K. Autonomic function and prothrombotic activity in women after an acute coronary event. J Womens Health (Larchmt) 2008;17:1331–7. doi: 10.1089/jwh.2007.0764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.La Rovere MT, Bigger JT, Jr, Marcus FI, Mortara A, Schwartz PJ. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. Lancet. 1998;351:478–84. doi: 10.1016/s0140-6736(97)11144-8. [DOI] [PubMed] [Google Scholar]
- 41.Bigger JT, Jr, Fleiss JL, Steinman RC, Rolnitzky LM, Kleiger RE, Rottman JN. Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation. 1992;85:164–71. doi: 10.1161/01.cir.85.1.164. [DOI] [PubMed] [Google Scholar]
- 42.Piccirillo G, Magrì D, Matera S, et al. QT variability strongly predicts sudden cardiac death in asymptomatic subjects with mild or moderate left ventricular systolic dysfunction: a prospective study. Eur Heart J. 2007;28:1344–50. doi: 10.1093/eurheartj/ehl367. [DOI] [PubMed] [Google Scholar]
- 43.Meewisse ML, Reitsma JB, de Vries GJ, Gersons BP, Olff M. Cortisol and post-traumatic stress disorder in adults: systematic review and meta-analysis. Br J Psychiatry. 2007;191:387–92. doi: 10.1192/bjp.bp.106.024877. [DOI] [PubMed] [Google Scholar]
- 44.Morris MC, Compas BE, Garber J. Relations among posttraumatic stress disorder, comorbid major depression, and HPA function: a systematic review and meta-analysis. Clin Psychol Rev. 2012;32:301–15. doi: 10.1016/j.cpr.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bedi US, Arora R. Cardiovascular manifestations of posttraumatic stress disorder. J Natl Med Assoc. 2007;99:642–9. [PMC free article] [PubMed] [Google Scholar]
- 46.Yehuda R. Advances in understanding neuroendocrine alterations in PTSD and their therapeutic implications. Ann NY Acad Sci. 2006;1071:137–66. doi: 10.1196/annals.1364.012. [DOI] [PubMed] [Google Scholar]
- 47.Grenon SM, Owens CD, Alley H, et al. Posttraumatic Stress Disorder Is Associated With Worse Endothelial Function Among Veterans. J Am Heart Assoc. 2016;5:e003010. doi: 10.1161/JAHA.115.003010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Violanti JM, Fekedulegn D, Hartley TA, et al. Police trauma and cardiovascular disease: association between PTSD symptoms and metabolic syndrome. Int J Emerg Ment Health. 2006;8:227–37. [PubMed] [Google Scholar]
- 49.von Kanel R, Begre S, Abbas CC, Saner H, Gander M-L, Schmid J-P. Inflammatory biomarkers in patients with posttraumatic stress disorder caused by myocardial infarction and the role of depressive symptoms. Neuroimmunomodulation. 2010;17:39–46. doi: 10.1159/000243084. [DOI] [PubMed] [Google Scholar]
- 50.von Kanel R, Hepp U, Kraemer B, et al. Evidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorder. J Psychiatr Res. 2007;41:744–52. doi: 10.1016/j.jpsychires.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 51.Michopoulos V, Rothbaum AO, Jovanovic T, et al. Association of CRP Genetic Variation and CRP Level With Elevated PTSD Symptoms and Physiological Responses in a Civilian Population With High Levels of Trauma. Am J Psychiatry. 2014;172:353–62. doi: 10.1176/appi.ajp.2014.14020263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaptoge S, Di Angelantonio E, Lowe G, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132–40. doi: 10.1016/S0140-6736(09)61717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ahmadi N, Hajsadeghi F, Mirshkarlo HB, Budoff M, Yehuda R, Ebrahimi R. Post-traumatic stress disorder, coronary atherosclerosis, and mortality. Am J Cardiol. 2011;108:29–33. doi: 10.1016/j.amjcard.2011.02.340. [DOI] [PubMed] [Google Scholar]
- 54.Pace TW, Heim CM. A short review on the psychoneuroimmunology of posttraumatic stress disorder: from risk factors to medical comorbidities. Brain Behav Immun. 2011;25:6–13. doi: 10.1016/j.bbi.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 55.Baker DG, Nievergelt CM, O’Connor DT. Biomarkers of PTSD: neuropeptides and immune signaling. Neuropharmacology. 2012;62:663–73. doi: 10.1016/j.neuropharm.2011.02.027. [DOI] [PubMed] [Google Scholar]
- 56.Gill JM, Saligan L, Woods S, Page G. PTSD is associated with an excess of inflammatory immune activities. Perspect Psychiatr Care. 2009;45:262–77. doi: 10.1111/j.1744-6163.2009.00229.x. [DOI] [PubMed] [Google Scholar]
- 57.Passos IC, Vasconcelos-Moreno MP, Costa LG, et al. Inflammatory markers in post-traumatic stress disorder: a systematic review, meta-analysis, and meta-regression. Lancet Psychiatry. 2015;2:1002–12. doi: 10.1016/S2215-0366(15)00309-0. [DOI] [PubMed] [Google Scholar]
- 58.Michopoulos V, Rothbaum AO, Jovanovic T, et al. Association of CRP genetic variation and CRP level with elevated PTSD symptoms and physiological responses in a civilian population with high levels of trauma. Am J Psychiatry. 2015;172:353–62. doi: 10.1176/appi.ajp.2014.14020263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eraly SA, Nievergelt CM, Maihofer AX, et al. Assessment of Plasma C-Reactive Protein as a Biomarker of Posttraumatic Stress Disorder Risk. JAMA Psychiatry. 2014;71:423–31. doi: 10.1001/jamapsychiatry.2013.4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Van Zuiden M, Kavelaars A, Geuze E, Olff M, Heijnen CJ. Predicting PTSD: pre-existing vulnerabilities in glucocorticoid-signaling and implications for preventive interventions. Brain Behav Immun. 2013;30:12–21. doi: 10.1016/j.bbi.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 61.Brouwers CJ, Wolf JM, von Känel R. Inflammatory markers in PTSD. In: Martin CR, Preedy VR, Patel VB, editors. Comprehensive Guide to Post-Traumatic Stress Disorder. Switzerland: Springer International Publishing; 2016. pp. 979–93. [Google Scholar]
- 62.Pace TWW, Wingenfeld K, Schmidt I, Meinlschmidt G, Hellhammer DH, Heim CM. Increased peripheral NF-kappa B pathway activity in women with childhood abuse-related posttraumatic stress disorder. Brain Behav Immun. 2012;26:13–7. doi: 10.1016/j.bbi.2011.07.232. [DOI] [PubMed] [Google Scholar]
- 63.Buckley TC, Kaloupek DG. A meta-analytic examination of basal cardiovascular activity in posttraumatic stress disorder. Psychosom Med. 2001;63:585–94. doi: 10.1097/00006842-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 64.Paulus EJ, Argo TR, Egge JA. The Impact of Posttraumatic Stress Disorder on Blood Pressure and Heart Rate in a Veteran Population. J Traum Stress. 2013;26:169–72. doi: 10.1002/jts.21785. [DOI] [PubMed] [Google Scholar]
- 65.Burg M, Brandt C, Buta E, et al. Risk for incident hypertension associated with PTSD in military veterans, and the effect of PTSD treatment. Psychosom Med. 2016 Aug 3; doi: 10.1097/PSY.0000000000000376. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Austin AW, Wissmann T, Von Kanel R. Stress and hemostasis: An update. Semin Thromb Hemost. 2013;39:902–12. doi: 10.1055/s-0033-1357487. [DOI] [PubMed] [Google Scholar]
- 67.von Kanel R, Hepp U, Traber R, et al. Measures of endothelial dysfunction in plasma of patients with posttraumatic stress disorder. Psychiatry Res. 2008;158:363–73. doi: 10.1016/j.psychres.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 68.von Kanel R, Hepp U, Buddeberg C, et al. Altered blood coagulation in patients with posttraumatic stress disorder. Psychosom Med. 2006;68:598–604. doi: 10.1097/01.psy.0000221229.43272.9d. [DOI] [PubMed] [Google Scholar]
- 69.Robicsek O, Makhoul B, Klein E, Brenner B, Sarig G. Hypercoagulation in Chronic Post-Traumatic Stress Disorder. Isr Med Assoc J. 2011;13:548–52. [PubMed] [Google Scholar]
- 70.Vidovic A, Vilibic M, Markotic A, et al. Baseline level of platelet-leukocyte aggregates, platelet CD63 expression, and soluble P-selectin concentration in patients with posttraumatic stress disorder: a pilot study. Psychiatry Res. 2007;150:211–6. doi: 10.1016/j.psychres.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 71.Vidovic A, Grubisic-Ilic M, Kozaric-Kovacic D, et al. Exaggerated platelet reactivity to physiological agonists in war veterans with posttraumatic stress disorder. Psychoneuroendocrinology. 2011;36:161–72. doi: 10.1016/j.psyneuen.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 72.Ho VT, Shimbo D, Duer-Hefele J, Whang W, Chang M, Edmondson D. Posttraumatic stress disorder symptoms and hypercoagulability during emergency department evaluation for acute coronary syndrome. IJC Metab Endocr. 2016;11:1–2. doi: 10.1016/j.ijcme.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.von Kanel R, Abbas CC, Schmid J-P, et al. Momentary stress moderates procoagulant reactivity to a trauma-specific interview in patients with posttraumatic stress disorder caused by myocardial infarction. J Psychiatr Res. 2010;44:956–63. doi: 10.1016/j.jpsychires.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 74.Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch Gen Psychiatry. 2003;60:289–94. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- 75.Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: Findings from the Heart and Soul Study. Health Psychol. 2012;31:194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cohen BE, Marmar C, Ren L, Bertenthal D, Seal KH. Association of cardiovascular risk factors with mental health diagnoses in Iraq and Afghanistan war veterans using VA health care. JAMA. 2009;302:489–92. doi: 10.1001/jama.2009.1084. [DOI] [PubMed] [Google Scholar]
- 77.Kronish IM, Edmondson D, Goldfinger J, Fei K, Horowitz C. Posttraumatic stress disorder and adherence to medications in survivors of strokes and transient ischemic attacks. Stroke. 2012 doi: 10.1161/STROKEAHA.112.655209. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kronish IM, Edmondson D, Li Y, Cohen BE. Post-traumatic stress disorder and medication adherence: Results from the mind your heart study. J Psychiatr Res. 2012;46:1595–9. doi: 10.1016/j.jpsychires.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shemesh E, Yehuda R, Milo O, et al. Posttraumatic stress, nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosom Med. 2004;66:521–6. doi: 10.1097/01.psy.0000126199.05189.86. [DOI] [PubMed] [Google Scholar]
- 80.Rosenbaum S, Stubbs B, Ward PB, Steel Z, Lederman O, Vancampfort D. The prevalence and risk of metabolic syndrome and its components among people with posttraumatic stress disorder: a systematic review and meta-analysis. Metabolis. 2015;64:926–33. doi: 10.1016/j.metabol.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 81.Vancampfort D, Rosenbaum S, Ward PB, et al. Type 2 Diabetes Among People With Posttraumatic Stress Disorder: Systematic Review and Meta-Analysis. Psychosom Med. 2016;78:465–73. doi: 10.1097/PSY.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 82.Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 83.Shemesh E, Rudnick A, Kaluski E, et al. A prospective study of posttraumatic stress symptoms and nonadherence in survivors of a myocardial infarction (MI) Gen Hosp Psychiatry. 2001;23:215–22. doi: 10.1016/s0163-8343(01)00150-5. [DOI] [PubMed] [Google Scholar]
- 84.Shemesh E, Yehuda R, Milo O, et al. Posttraumatic stress, nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosom Med. 2004;66:521–6. doi: 10.1097/01.psy.0000126199.05189.86. [DOI] [PubMed] [Google Scholar]
- 85.Favaro A, Gerosa G, Caforio AL, et al. Posttraumatic stress disorder and depression in heart transplantation recipients: the relationship with outcome and adherence to medical treatment. Gen Hosp Psychiatry. 2011;33:1–7. doi: 10.1016/j.genhosppsych.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 86.Kronish IM, Edmondson D, Goldfinger JZ, Fei K, Horowitz CR. Posttraumatic Stress Disorder and Adherence to Medications in Survivors of Strokes and Transient Ischemic Attacks. Stroke. 2012;43:2192–7. doi: 10.1161/STROKEAHA.112.655209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kronish IM, Lin JJ, Cohen BE, Voils CI, Edmondson D. Posttraumatic Stress Disorder and Medication Nonadherence in Patients With Uncontrolled Hypertension. JAMA Intern Med. 2014;174:468–70. doi: 10.1001/jamainternmed.2013.12881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Edmondson D. An Enduring Somatic Threat Model of Posttraumatic Stress Disorder Due to Acute Life-Threatening Medical Events. Soc Personal Psychol Compass. 2014;8:118–34. doi: 10.1111/spc3.12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kronish IM, Moise N, Bleck R, Hiti D, Edmondson D. PTSD and aversive cognitive associations about aspirin in acute coronary syndrome patients. American Psychosomatic Society; Savannah, GA: 2015. [Google Scholar]
- 90.Cordova MJ, Riba MB, Spiegel D. PTSD and cancer. Lancet Psychiatry. doi: 10.1016/S2215-0366(17)30014-7. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: A meta-analytic review. PloS One. 2012;7:e38915. doi: 10.1371/journal.pone.0038915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sembi S, Tarrier N, O’Neill P, Burns A, Faragher B. Does post-traumatic stress disorder occur after stroke: a preliminary study. Int J Geriatr Psychiatry. 1998;13:315–22. doi: 10.1002/(sici)1099-1166(199805)13:5<315::aid-gps766>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 93.Bruggimann L, Annoni J, Staub F, Von Steinbüchel N, Van der Linden M, Bogousslavsky J. Chronic posttraumatic stress symptoms after nonsevere stroke. Neurology. 2006;66:513–6. doi: 10.1212/01.wnl.0000194210.98757.49. [DOI] [PubMed] [Google Scholar]
- 94.Field EL, Norman P, Barton J. Cross-sectional and prospective associations between cognitive appraisals and posttraumatic stress disorder symptoms following stroke. Behav Res Ther. 2008;46:62–70. doi: 10.1016/j.brat.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 95.Merriman C, Norman P, Barton J. Psychological correlates of PTSD symptoms following stroke. Psychol Health Med. 2007;12:592–602. doi: 10.1080/13548500601162747. [DOI] [PubMed] [Google Scholar]
- 96.Wang X, Chung MC, Hyland ME, Bahkeit M. Posttraumatic stress disorder and psychiatric co-morbidity following stroke: The role of alexithymia. Psychiatry Research. 2010;188:51–7. doi: 10.1016/j.psychres.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 97.Sagen U, Vik TG, Moum T, Mørland T, Finset A, Dammen T. Screening for anxiety and depression after stroke: Comparison of the Hospital Anxiety and Depression Scale and the Montgomery and Åsberg Depression Rating Scale. J Psychosom Res. 2009;67:325–32. doi: 10.1016/j.jpsychores.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 98.Kiphuth IC, Utz KS, Noble AJ, Köhrmann M, Schenk T. Increased Prevalence of Posttraumatic Stress Disorder in Patients After Transient Ischemic Attack. Stroke. 2014;45:3360–6. doi: 10.1161/STROKEAHA.113.004459. [DOI] [PubMed] [Google Scholar]
- 99.Noble S, Lewis R, Whithers J, Lewis S, Bennett P. Long-term psychological consequences of symptomatic pulmonary embolism: a qualitative study. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2013-004561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shemesh E, Koren-Michowitz M, Yehuda R, et al. Symptoms of Posttraumatic Stress Disorder in Patients Who Have Had a Myocardial Infarction. Psychosomatics. 2006;47:231–9. doi: 10.1176/appi.psy.47.3.231. [DOI] [PubMed] [Google Scholar]
- 101.Forneris CA, Gartlehner G, Brownley KA, et al. Interventions to Prevent Post-Traumatic Stress Disorder: A Systematic Review. Am J Prev Med. 2013;44:635–50. doi: 10.1016/j.amepre.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 102.Meister R, Princip M, Schmid JP, et al. Myocardial Infarction - Stress PRevention INTervention (MI-SPRINT) to reduce the incidence of posttraumatic stress after acute myocardial infarction through trauma-focused psychological counseling: study protocol for a randomized controlled trial. Trials [Electronic Resource] 2013;14:329. doi: 10.1186/1745-6215-14-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Meister RE, Weber T, Princip M, et al. Perception of a hectic hospital environment at admission relates to acute stress disorder symptoms in myocardial infarction patients. Gen Hosp Psychiatry. 2016;39:8–14. doi: 10.1016/j.genhosppsych.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 104.Edmondson D, Shimbo D, Ye S, Wyer P, Davidson KW. The Association of Emergency Department Crowding During Treatment for Acute Coronary Syndrome With Subsequent Posttraumatic Stress Disorder Symptoms. JAMA Intern Med. 2013;173:472–5. doi: 10.1001/jamainternmed.2013.2536. [DOI] [PMC free article] [PubMed] [Google Scholar]