Abstract
Background
According to the 2004 Surgeon General’s Report on Health Consequences of Smoking, after >15 years of abstinence, the cardiovascular risk of former smokers becomes similar to that of never-smokers. Whether this health benefit of smoking cessation varies by amount and duration of prior smoking remains unclear.
Methods and Results
Of the 4482 adults ≥65 years without prevalent heart failure (HF) in the Cardiovascular Health Study (CHS), 2556 were never-smokers, 629 current smokers, and 1297 former smokers with >15 years of cessation, of whom 312 were heavy smokers (highest quartile; ≥32 pack-years). Age-sex-race-adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for centrally-adjudicated incident HF and mortality during 13 years of follow-up were estimated using Cox regression models. Compared to never-smokers, former smokers as a group had similar risk for incident HF (aHR, 0.99; 95% CI, 0.85–1.16) and all-cause mortality (aHR, 1.08; 95% CI, 0.96–1.20), but former heavy smokers had higher risk for both HF (aHR, 1.45; 95% CI, 1.15–1.83) and mortality (aHR, 1.38; 95% CI, 1.17–1.64). However, when compared to current smokers, former heavy smokers had lower risk of death (aHR, 0.64; 95% CI, 0.53–0.77), but not of HF (aHR, 0.97; 95% CI, 0.74–1.28).
Conclusions
After >15 years of smoking cessation, older adults who smoked <32 pack-years appear to achieve the health profile of never-smokers. Although former heavy (≥32 pack-years) smokers may not achieve this health benefit of prolonged smoking cessation, their risk is clearly lower relative to current smokers.
Keywords: heart failure, mortality, smoking
Tobacco smoking is the most important modifiable risk factor for cardiovascular morbidity and mortality.1–5 The excess cardiovascular risk of smoking is reduced to half after one year of smoking abstinence and has been reported to decrease to the level of never-smokers after prolonged cessation.5–8 However, the duration of smoking cessation necessary for the risk of former smokers to become that of never-smokers varies widely between studies.9–11 The 2004 Surgeon General’s Report on The Health Consequences of Smoking concluded that the excess risk of coronary heart disease caused by smoking is reduced to that of never-smokers after 15 years of abstinence.6 However, whether this benefit of prolonged smoking cessation extends to heart failure (HF), other cardiovascular events, and mortality in community-dwelling older adults has not been well studied. Further, whether these benefits vary by the amount and duration of smoking prior to cessation remains unclear. In the current study, we examined whether the risk of incident HF and other outcomes among former older smokers who quit smoking >15 years ago varied by the amount and duration of prior smoking.
Methods
Study design and participants
The Cardiovascular Health Study (CHS) is an ongoing, prospective population-based study of cardiovascular risk factors among community-dwelling older adults. The methods and findings from the CHS have been previously described.12, 13 Briefly, random samples of Medicare-eligible male and female residents age ≥65 years were recruited from four U.S. counties. An original cohort of 5201 participants (1989–1990) was supplemented by a second cohort of 687 African Americans (1992–1993). For the current analysis, after obtaining appropriate permission from local institutional review board, de-identified copies of the CHS datasets were obtained from the National Heart, Lung, and Blood Institute, which also sponsored the CHS. Of the 5888 CHS participants, 5795 consented to be included in the public-use copy of the data.
Baseline smoking status and other measurements
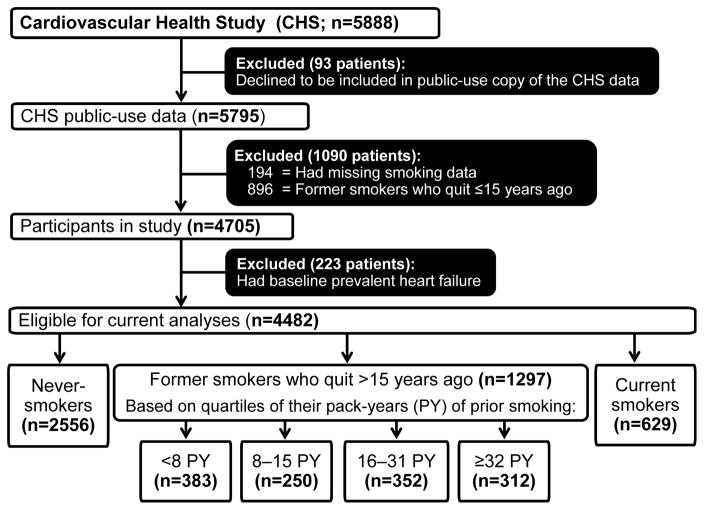
Baseline data on self-reported smoking included data on current smoking status, amount and duration of smoking, and duration of smoking abstinence.12, 14, 15 The amount and duration of smoking was measured using pack-years, which was estimated by multiplying the number of packs of cigarettes smoked per day by the number of years of smoking. Extensive data on baseline demographics, medical history including cardiovascular disease and risk factors, and clinical and laboratory findings were also collected. Of the 5795 participants in the public-use copy of the CHS data, baseline data on smoking were available for 5601 individuals. We excluded 896 former smokers who quit smoking ≤15 years ago. Of the remaining 4705 participants, 223 had centrally-adjudicated prevalent HF at baseline and were also excluded. Of the remaining 4482 participants, 629 (14%) were current smokers, 2556 (57%) were never-smokers, and 1297 (29%) were former smokers who quit smoking >15 years ago (Figure 1). The 1297 former smokers were categorized by their pre-cessation pack-year quartiles into light (<8 pack-years; n=383), moderate (8–15 pack-years; n=250 and 16–31 pack-years; n=352), and heavy (≥32 pack-years; n=312) smokers.
Figure 1.
Flow chart displaying assembly of study cohort based on the public-use copy of the Cardiovascular Health Study (CHS) data
Outcomes
The primary outcomes of interest for the current analysis included incident HF and all-cause mortality during 13 years of follow-up. Secondary outcomes included acute myocardial infarction, stroke, peripheral arterial disease, and cardiovascular and non-cardiovascular mortalities. All outcomes were centrally adjudicated by the CHS Events Committee, the process of which has been extensively documented in the literature.12, 16–18 Specifically, the CHS adjudication of HF has been reported to be comparable to that of the Framingham criteria, and HF patients diagnosed with both criteria have also been reported to be prognostically similar.19 Data on death were obtained and confirmed using death certificates, autopsy reports, medical records, and physician questionnaires.
Statistical analysis
Baseline characteristics of never-smokers, former smokers stratified by quartiles of pack-years of smoking, and current smokers were compared using Pearson’s Chi-square, analysis of variance, and Kruskal-Wallis tests as appropriate. We constructed Cox regression multivariable-adjusted models adjusting for 27 potential confounders to estimate associations of quartiles of former smokers and current smokers with incident HF and mortality using never-smokers as a reference. Because former smokers in our study quit smoking more than 15 years ago, many baseline characteristics of former smokers may have been affected by prior smoking. Further, because of the small number of subjects and hence events, data over-fitting is a concern in large multivariable-adjusted models. Therefore, we restricted our primary analyses to models adjusted for age, sex, and race only. Because former heavy smokers would be expected to have a shorter duration of smoking cessation and former light smokers would have a longer duration of smoking cessation, some of the risks of former heavy smokers would likely be mediated by their shorter duration of cessation and vice versa. To understand how the duration of smoking cessation may have modified the former smoking effect, we ran an additional model including duration of smoking cessation. We repeated the above process for other incident cardiovascular events; however, for each we excluded patients with those respective conditions at baseline. We then repeated all of the above analyses to estimate associations of quartiles of former smokers with incident HF and mortality, this time, using current smokers as reference. Log minus log plots were visually examined to verify the proportional hazards assumption and found no obvious indications of non-proportionality for the effect of smoking status. We also used the martingale residuals to test and found no evidence of any proportional hazards assumption violation (p = 0.26 for effect of current smoker, p = 0.79 for former smoker). Data over-fitting was checked by applying a backward elimination stepwise procedure to models, and changes in standard errors for all variables were less than 5%. All statistical tests were two-tailed with 95% confidence levels and p-values <0.05 were considered significant. SPSS 19 for Windows (2010; Armonk, NY: IBM Corp.) was used for all data analyses.
Results
Baseline characteristics
Overall, current smokers were younger than both never-smokers and former smokers with >15 years of smoking cessation (Table 1). Compared to both never-smokers and current smokers, these former smokers were more likely to be married white men who had a higher education and income as well as a higher prevalence of coronary artery disease and left ventricular systolic dysfunction (Table 1). However, former heavy smokers were more likely to have higher median values for markers of inflammation, including interleukin-6 and C-reactive protein when compared to never-smokers, but not compared to current smokers (Table 1). Former heavy smokers smoked a mean of 53 pack-years and had a mean abstinence of 23 years (Table 1), while former light and moderate smokers smoked a mean of 4 and 19 pack-years and quit a mean of 36 and 28 years ago, respectively. Finally, at baseline, current smokers had a mean of 44 pack-years of smoking history.
Table 1.
Baseline characteristics by quartiles of pack-years (PY) among 4482 Cardiovascular Health Study participants without baseline prevalent heart failure
| Variables n (%) or mean (±SD) or median (quartiles 1–3) |
Never-smokers (n = 2556) | Quartiles of PYs of prior smoking for former smokers with over 15 years of smoking cessation (n=1297) | Current smokers (n = 629) | Overall P-value | P-value of differences within former smokers | ||||
|---|---|---|---|---|---|---|---|---|---|
| <8 PY (n = 383) | 8–15 PY (n = 250) | 16–31 PY (n = 352) | ≥32 PY (n = 312) | Never vs. former | Current vs. former | ||||
| Age, years | 74 (±6) | 73 (±5) | 74 (±6) | 73 (±5) | 74 (±6) | 71 (±5) | <0.01 | <0.01 | <0.01 |
| Female | 1808 (71) | 203 (53) | 98 (39) | 112 (32) | 65 (21) | 382 (61) | <0.01 | <0.01 | <0.01 |
| African American | 406 (16) | 55 (14) | 36 (14) | 29 (8) | 16 (5) | 126 (20) | <0.01 | <0.01 | <0.01 |
| Married | 1629 (64) | 287 (75) | 179 (72) | 275 (78) | 237 (76) | 356 (57) | <0.01 | <0.01 | 0.33 |
| College or higher education | 1044 (41) | 191 (50) | 117 (47) | 179 (51) | 150 (48) | 250 (40) | <0.01 | <0.01 | 0.76 |
| Income ≥ $25,000/year | 881 (35) | 178 (47) | 121 (48) | 171 (49) | 150 (48) | 169 (27) | <0.01 | <0.01 | 0.94 |
| Smoke, pack-years | ––– | 4 (±2) | 12 (±2) | 24 (±5) | 53 (±22) | 44 (±28) | <0.01 | <0.01 | <0.01 |
| Duration of smoking cessation, years | ––– | 36 (±11) | 30 (±9) | 27 (±8) | 23 (±6) | 0.0 (±0.0) | <0.01 | <0.01 | <0.01 |
| Exposure to passive smoking | 243 (10) | 25 (7) | 24 (10) | 39 (11) | 32 (10) | 173 (28) | 0.27 | <0.01 | 0.16 |
| Alcohol, drinks per week | 1.3 (±4.3) | 2.7 (±6.4) | 3.2 (±6.5) | 3.6 (±7.8) | 4.4 (±8.1) | 3.8 (±8.1) | <0.01† | 0.09† | 0.01 |
| Self-reported fair to poor general health | 575 (23) | 69 (18) | 48 (19) | 70 (20) | 71 (23) | 187 (30) | 0.21 | <0.01 | 0.47 |
| Instrumental activities of daily living | 1.7 (1.1–2.4) | 1.6 (1.0–2.3) | 1.7 (1.2–2.5) | 1.7 (1.2–2.3) | 2.0 (1.4–2.7) | 2.0 (1.4–2.9) | <0.01† | <0.01† | 0.01 |
| Able to walk 0.5 miles without difficulty | 2160 (85) | 347 (91) | 223 (89) | 311 (88) | 261 (84) | 511 (81) | <0.01 | <0.01 | 0.04 |
| Blocks walked last week | 38 (±54) | 40 (±51) | 50 (±65) | 53 (±63) | 45 (±57) | 30 (±46) | <0.01† | <0.01† | 0.02 |
| Past medical history | |||||||||
| Coronary artery disease | 397 (16) | 67 (18) | 46 (18) | 77 (22) | 79 (25) | 95 (15) | <0.01 | <0.01 | 0.06 |
| Myocardial infarction | 155 (6) | 28 (7) | 20 (8) | 40 (11) | 37 (12) | 48 (8) | <0.01 | 0.07 | 0.11 |
| Hypertension | 1551 (61) | 204 (53) | 138 (55) | 212 (60) | 183 (59) | 332 (53) | 0.05 | 0.13 | 0.23 |
| Diabetes mellitus | 397 (16) | 49 (13) | 32 (13) | 54 (15) | 73 (23) | 77 (12) | <0.01 | <0.01 | <0.01 |
| Stroke | 82 (3) | 7 (2) | 10 (4) | 14 (4) | 20 (6) | 25 (4) | 0.02 | 0.05 | 0.02 |
| Atrial fibrillation | 54 (2) | 3 (1) | 3 (1) | 10 (3) | 13 (4) | 9 (1) | 0.02 | 0.01 | 0.01 |
| Peripheral arterial disease | 262 (10) | 27 (7) | 21 (8) | 33 (9) | 47 (15) | 133 (21) | 0.01 | <0.01 | <0.01 |
| Chronic obstructive pulmonary disease | 255 (10) | 38 (10) | 26 (10) | 39 (11) | 48 (15) | 101 (16) | 0.06 | 0.01 | 0.12 |
| Cancer | 340 (13) | 60 (16) | 27 (11) | 52 (15) | 60 (19) | 81 (13) | 0.02 | 0.04 | 0.05 |
| Clinical examination | |||||||||
| Body mass index, kg/m2 | 27 (±4) | 26 (±4) | 26 (±4) | 27 (±4) | 27 (±4) | 25 (±4) | 0.36 | <0.01 | 0.36 |
| Pulse, beats/minute | 68 (±11) | 67 (±11) | 66 (±11) | 66 (±11) | 67 (±11) | 70 (±12) | <0.01 | <0.01 | 0.59 |
| Systolic BP, mm Hg | 138 (±22) | 135 (±23) | 134 (±21) | 137 (±22) | 137 (±21) | 134 (±22) | 0.01 | 0.08 | 0.40 |
| Diastolic BP, mm Hg | 71 (±11) | 70 (±12) | 71 (±11) | 71 (±11) | 71 (±11) | 70 (±11) | 0.61 | 0.72 | 0.95 |
| Abnormal lung capacity | 126 (5) | 13 (3) | 11 (4) | 14 (4) | 10 (3) | 53 (8) | 0.46 | <0.01 | 0.87 |
| Medications | |||||||||
| ACE inhibitors | 152 (6) | 27 (7) | 22 (9) | 14 (4) | 22 (7) | 30 (5) | 0.13 | 0.06 | 0.10 |
| Beta–blockers | 330 (13) | 46 (12) | 34 (14) | 50 (14) | 40 (13) | 63 (10) | 0.93 | 0.32 | 0.84 |
| Diuretics | 686 (27) | 93 (24) | 61 (25) | 75 (21) | 86 (28) | 127 (20) | 0.18 | 0.10 | 0.32 |
| Aspirin | 1139 (45) | 173 (45) | 127 (51) | 169 (48) | 166 (53) | 285 (45) | 0.02 | 0.13 | 0.18 |
| Laboratory values | |||||||||
| Creatinine, mg/dL | 0.93 (±0.40) | 0.95 (±0.40) | 1.02 (±0.33) | 1.00 (±0.31) | 1.03 (±0.28) | 0.93 (±0.36) | <0.01† | <0.01† | 0.01 |
| Uric acid, mg/dL | 5.5 (±1.5) | 5.5 (±1.4) | 5.9 (±1.5) | 6.0 (±1.5) | 6.0 (±1.6) | 5.5 (±1.5) | <0.01 | <0.01 | <0.01 |
| Albumin, g/dL | 3.98 (±0.29) | 4.03 (±0.31) | 4.00 (±0.29) | 4.02 (±0.29) | 4.02 (±0.28) | 3.99 (±0.29) | 0.01 | 0.22 | 0.65 |
| Hemoglobin, g/dL | 13.8 (±1.3) | 14.1 (±1.4) | 14.3 (±1.3) | 14.4 (±1.3) | 14.4 (±1.3) | 14.3 (±1.3) | <0.01 | <0.01 | <0.01 |
| Total cholesterol, mg/dL | 214 (±39) | 214 (±40) | 208 (±37) | 208 (±36) | 200 (±37) | 211 (±39) | <0.01 | <0.01 | <0.01 |
| Serum insulin, μIU/mL | 17 (±25) | 15 (±11) | 16 (±14) | 16 (±26) | 19 (±29) | 16 (±26) | 0.03† | 0.01† | 0.11 |
| Interleukin-6, units/mL | 1.7 (1.1–2.4) | 1.6 (1.0–2.3) | 1.7 (1.2–2.5) | 1.7 (1.2–2.3) | 2.0 (1.4–2.7) | 2.0 (1.4–2.9) | <0.01† | <0.01† | <0.01 |
| C-reactive protein, mg/dL | 2.4 (1.2–4.2) | 2.2 (1.0–3.9) | 2.0 (0.9–3.8) | 2.1 (1.0–3.7) | 2.8 (1.4–4.5) | 3.4 (1.7–6.4) | 0.01† | <0.01† | <0.01 |
| LV hypertrophy by electrocardiography | 120 (5) | 13 (3) | 8 (3) | 13 (4) | 15 (5) | 30 (5) | 0.58 | 0.69 | 0.73 |
| LV systolic dysfunction by echocardiography | 168 (7) | 25 (7) | 12 (5) | 35 (10) | 42 (14) | 42 (7) | <0.01 | <0.01 | <0.01 |
P-values based on independent-samples, nonparametric tests to compare medians across groups
ACE=angiotensin-converting enzyme; BP=blood pressure; LV=left ventricular
Association with incident HF
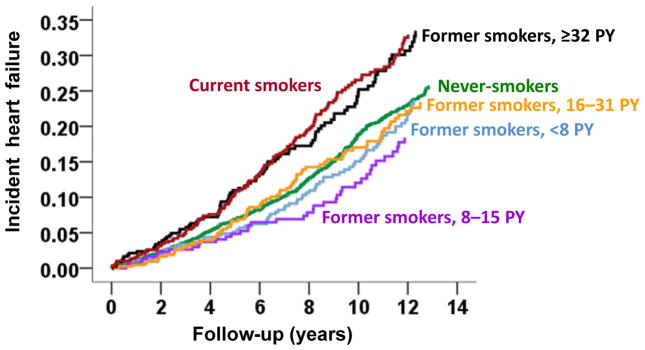
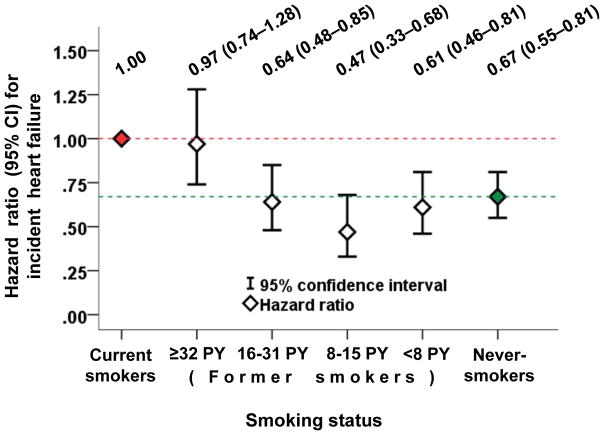
As a group, former smokers appeared to have similar risk for incident HF when compared to never-smokers (age-sex-race-adjusted hazard ratios {aHR}, 0.99; 95% confidence interval {CI}, 0.85–1.16), which was driven by former light and moderate smokers who had a similar risk to that of never-smokers (Table 2 and Figure 2). Former heavy smokers, on the other hand, had higher risk relative to that of never-smokers (aHR), 1.45; 95% CI, 1.15–1.83; Table 2 and Figure 2), but were similar to current smokers (aHR, 0.97; 95% CI, 0.74–1.28; Figure 3). The risk for former light and moderate smokers was lower than that of current smokers (Figure 3). These associations for former smokers when compared to never-smokers remained essentially unchanged after multivariable-adjustment (Table 2). When adjusted for duration of smoking cessation, compared to never-smokers, multivariable-adjusted HRs (95% CI) for incident HF associated with the four smoking categories from the lightest (<8 pack-years) to the heaviest (≥32 pack-years) were 1.97 (1.09–3.54), 1.45 (0.83–2.52), 1.56 (0.98–2.49) and 1.88 (1.27–2.79), respectively.
Table 2.
Association of former smokers who quit over 15 years ago (n=1297), overall and by quartiles of pack-years (PY) of smoking and current smokers (n=629) with incident heart failure, compared to never-smokers (n=2556)
| Incident heart failure | Events (%) | Hazard ratio (95% confidence interval); P-value | ||
|---|---|---|---|---|
| Unadjusted | Age-sex-race-adjusted | Multivariable-adjusted* | ||
| Never–smokers (n=2556) | 523 (21) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Former smokers, overall, (n=1297) | 273 (21) | 1.06 (0.91–1.22); P=0.473 | 0.99 (0.85–1.16); P=0.936 | 1.07 (0.91–1.25); P=0.404 |
| <8 PY (n=383) | 73 (19) | 0.89 (0.70–1.14); P=0.362 | 0.91 (0.71–1.17); P=0.452 | 1.06 (0.83–1.36); P=0.650 |
| 8–15 PY (n=250) | 39 (16) | 0.76 (0.55–1.05); P=0.091 | 0.71 (0.51–0.98); P=0.038 | 0.86 (0.62–1.20); P=0.369 |
| 16–31 PY (n=352) | 71 (20) | 1.00 (0.78–1.28); P=0.973 | 0.95 (0.74–1.23); P=0.692 | 0.99 (0.77–1.28); P=0.951 |
| ≥32 PY (n=312) | 90 (29) | 1.67 (1.33–2.09); P<0.001 | 1.45 (1.15–1.83); P=0.002 | 1.31 (1.03–1.65); P=0.027 |
| Current smokers (n=629) | 135 (22) | 1.19 (0.99–1.44); P=0.072 | 1.49 (1.23–1.81); P<0.001 | 1.52 (1.24–1.87); P<0.001 |
Adjusted for age, sex, race, education, income, alcohol consumption, exposure to passive smoking, ability to walk 0.5 miles without difficulty, daily energy expenditure in kilocalories, instrumental activities of daily living, body mass index, coronary artery disease, acute myocardial infarction, hypertension, diabetes mellitus, stroke, atrial fibrillation by electrocardiogram, peripheral artery disease by ankle-brachial index, chronic obstructive pulmonary disease, cancer, left ventricular hypertrophy, left ventricular systolic dysfunction, serum creatinine, C-reactive protein, use of angiotensin-converting enzyme inhibitors, beta-blockers and diuretics, and antecedent acute myocardial infarction occurring before incident heart failure
Figure 2.
Age-sex-race-adjusted survival plots for incident heart failure for never-smokers, former smokers who quit smoking over 15 years ago, stratified by quartiles of pack-years (PY) of prior smoking, and current smokers
Figure 3.
Age-sex-race-adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for incident heart failure for never-smokers and former smokers who quit smoking over 15 years ago, stratified by quartiles of pack-years (PY) of prior smoking, relative to current smokers. The red dotted line is the line of reference, and the green dotted line intersects the aHR for never-smokers
Association with mortality
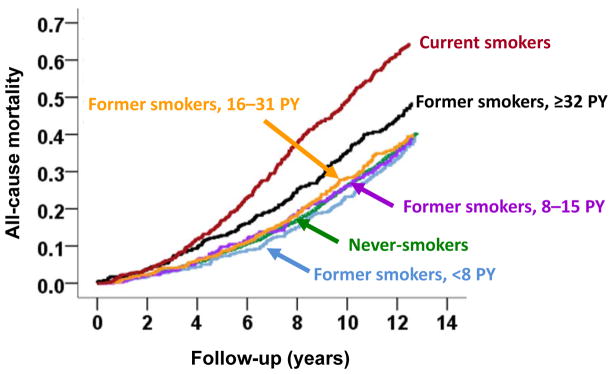
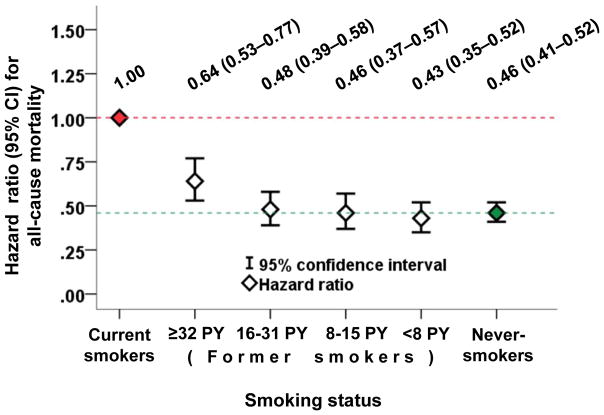
Former smokers as a group appeared to have similar risk for all-cause mortality when compared to never-smokers (aHR, 1.08; 95% CI, 0.96–1.20; Table 3), which was mainly driven by former light and moderate smokers (Figure 4). The risk for former heavy smokers was higher than that of never-smokers (aHR, 1.38; 95% CI, 1.17–1.64; Table 3 and Figure 4), but lower than that of current smokers (aHR, 0.64; 95% CI, 0.53–0.77; Figure 5). These associations remained essentially unchanged after multivariable-adjustment (Table 3). When adjusted for duration of smoking cessation, compared to never-smokers, multivariable-adjusted HRs (95% CI) for all-cause mortality associated with the four smoking categories from the lightest (<8 pack-years) to the heaviest (≥32 pack-years) were 1.40 (0.95–2.06), 1.37 (0.95–1.98), 1.40 (1.02–1.92) and 1.50 (1.15–1.97), respectively.
Table 3.
Association of former smokers who quit over 15 years ago (n=1297), overall and by quartiles of pack-years (PY) of smoking and current smokers (n=629) with all-cause mortality, compared to never-smokers (n=2556)
| All-Cause Mortality | Events (%) | Hazard ratio (95% confidence interval); P-value | ||
|---|---|---|---|---|
| Unadjusted | Age-sex-race-adjusted | Multivariable-adjusted* | ||
| Never–smokers (n=2556) | 1007 (39) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Former smokers, overall, (n=1297) | 568 (44) | 1.13 (1.02–1.26); P=0.017 | 1.08 (0.96–1.20); P=0.193 | 1.12 (1.01–1.25); P=0.039 |
| <8 PY (n=383) | 139 (36) | 0.88 (0.74–1.05); P=0.163 | 0.93 (0.77–1.11); P=0.402 | 1.04 (0.87–1.25); P=0.649 |
| 8–15 PY (n=250) | 104 (42) | 1.06 (0.87–1.30); P=0.570 | 1.00 (0.81–1.22); P=0.980 | 1.06 (0.87–1.31); P=0.560 |
| 16–31 PY (n=352) | 150 (43) | 1.09 (0.92–1.29); P=0.346 | 1.04 (0.87–1.24); P=0.650 | 1.12 (0.94–1.34); P=0.208 |
| ≥32 PY (n=312) | 175 (56) | 1.63 (1.39–1.91); P<0.001 | 1.38 (1.17–1.64); P<0.001 | 1.26 (1.06–1.49); P=0.008 |
| Current smokers (n=629) | 335 (53) | 1.56 (1.38–1.77); P<0.001 | 2.17 (1.91–2.47); P<0.001 | 2.04 (1.78–2.34); P<0.001 |
Adjusted for the same covariates as in Table 2
Figure 4.
Age-sex-race-adjusted survival plots for all-cause mortality for never-smokers, former smokers who quit smoking over 15 years ago, stratified by quartiles of pack-years (PY) of prior smoking, and current smokers
Figure 5.
Age-sex-race-adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for all-cause mortality for never-smokers and former smokers who quit smoking over 15 years ago, stratified by quartiles of pack-years (PY) of prior smoking, relative to current smokers. The red dotted line is the line of reference, and the green dotted line intersects the aHR for never-smokers
Overall, similar patterns were observed for cardiovascular and non-cardiovascular mortality. Former smokers as a group had similar risk for cardiovascular mortality when compared to never-smokers (aHR, 1.00; 95% CI, 0.84–1.18). Although former heavy smokers were an exception (aHR, 1.37; 95% CI, 1.06–1.77; p=0.016), they had a trend toward lower risk relative to current smokers (aHR, 0.76; 95% CI, 0.56–1.03). In contrast, former smokers as a group had a trend toward higher risk of non-cardiovascular mortality relative to never-smokers (aHR, 1.14; 95% CI, 0.99–1.31), which was driven by former heavy smokers, who were the only group to have significantly higher risk (aHR, 1.40; 95% CI, 1.12–1.75). However, former heavy smokers too had lower risk for non-cardiovascular mortality when compared to current smokers (aHR, 0.61; 95% CI, 0.47–0.79).
Association with other outcomes
Among the 4154 participants without baseline acute myocardial infarction history, former smokers as a group had a similar risk for incident acute myocardial infarction as that of never-smokers (aHR, 1.08; 95% CI, 0.88–1.33). Former heavy smokers had higher risk compared to never-smokers (aHR, 1.65; 95% CI, 1.22–2.22), and remained high relative to current smokers (aHR, 1.35; 95% CI, 0.92–1.97).
Among the 3959 participants without baseline history of peripheral arterial disease, the incidence of peripheral arterial disease was low (2% among never-smokers) and there were no significant associations. Although the incidence of stroke was not low (15% among never-smokers), no significant associations emerged among the 4324 participants without baseline stroke.
Discussion
Findings from the current study demonstrate that community-dwelling older former smokers who quit >15 years ago had similar risk of incident HF and mortality as that of never-smokers. However, when stratified by pack-years of prior smoking, this benefit was only observed among former light and moderate (<32 pack-years) smokers, as former heavy (≥32 pack-years) smokers had a 45% higher risk for incident HF, a 65% higher risk for acute myocardial infarction, and a 38% higher risk for all-cause death, despite >15 years of cessation. Although HF risk for former heavy smokers was similar to that of current smokers, they had significantly lower risks for all-cause and non-cardiovascular deaths, and a trend toward lower cardiovascular death. These data support the overall conclusions of the U.S. Surgeon General about the health benefits of prolonged smoking cessation and provide additional insights about how this benefit may be modified by the amount and duration of prior smoking. While older former smokers who quit smoking >15 years ago may gain clear health benefits compared to current smokers, to achieve the health profile of never-smokers, it is important to smoke less and quit early.
The acute pro-thrombotic, pro-adrenergic, and pro-inflammatory properties of smoking are believed to underlie smoking-associated atherosclerosis and cardiovascular disease.4, 20 However, cessation has been shown to reverse smoking-associated endothelial dysfunction,21, 22 which reduces the cardiovascular risk of smoking soon after cessation.6 We observed that the risk of death for even former heavy smokers was lower than that of current smokers, suggesting a clear health benefit of cessation despite prolonged and/or heavy smoking. The higher risk among former heavy smokers relative to never-smokers is unlikely to be explained by the acute harmful effects of current smoking. Former heavy smokers who smoked an average of 53 pack-years had a mean of 23 years of smoking cessation at baseline and had a median time of 9 years from baseline to both incident HF and acute myocardial infarction. This long gap of over 30 years from smoking cessation to incident cardiovascular events suggests that atherosclerosis associated with prolonged smoking may cross a biological threshold for reversibility, which may in part explain the high risk of HF and acute myocardial infarction among former heavy smokers, which was similar to that of current smokers. This may in part be explained by the shorter duration of smoking cessation among heavy smokers because when adjusted for duration of smoking cessation, the health benefits of lighter smokers who had a longer duration of cessation were attenuated and became similar to that of heavy smokers with a shorter duration of cessation. Yet, we observed that former heavy smokers had lower risk of death compared to current smokers, suggesting a clear benefit of smoking cessation even with a relatively shorter duration of cessation. This may also in part be a survivor cohort effect as death of former heavy smokers at younger age, may have led to healthier, stronger older former smokers. A similar survivor cohort effect is also observed among very old African Americans, who have lower mortality than their white counterparts.23 Of note, all former smokers in our study had at least over 15 years of smoking cessation, the duration of smoking cessation that is currently believed to reduce the cardiovascular risk of smoking for all former smokers to that of never-smokers.
Prior studies of the benefits of smoking cessation may have failed to identify the high-risk profile of former heavy smokers due to lack of data on both the amount and duration of smoking by former smokers.11, 24, 25 Among women in the Nurses’ Health Study, the cardiovascular risk of former smokers (n=661) was similar to that of never-smokers (n=1115) after 10 to 14 years of cessation.11 In that study, former smokers were categorized into five groups based on their duration of smoking cessation, but data on their prior smoking (both amount and duration) were not collected. A large prospective study from Japan reported that the risk of cardiovascular disease for former (vs. current) smokers aged 65 to 79 years did not significantly decline until after 10 years of smoking cessation.24 However, data on health benefits of smoking cessation compared to never-smokers were not presented. Importantly, that study also lacked data on amount and duration of smoking prior to cessation. Similarly, we also observed that as a group former smokers had a similar health profile as that of never-smokers. However, when we stratified by pack-years of prior smoking, the cardiovascular risk for former heavy smokers was higher than that of never-smokers. Former heavy smokers also had a higher prevalence of diabetes, left ventricular systolic dysfunction, coronary artery disease and peripheral arterial disease as well higher median values for serum C-reactive protein and interleukin-6 levels relative to never-smokers. Since the higher prevalence of baseline risk factors may be explained by prior heavy smoking, adjustment for these mediators may in part explain the attenuation of the associations in the multivariable model. Nonetheless, despite this high cardiovascular risk relative to never-smokers, former heavy smokers clearly had lower risk of mortality relative to current smokers. To the best of our knowledge, the current study is the first to clarify the role of amount and duration of prior smoking on the health benefits of prolonged cessation for former smokers.
Findings from the current study have potential public health implications. They support the overall conclusion of the U.S. Surgeon General’s report that >15 years of smoking cessation allows most formers smokers to achieve the health profile of never-smokers. Although former heavy smokers may not achieve that benefit, they clearly had better survival odds than current smokers. These findings suggest that clinicians could target former heavy smokers for screening and interventions for other cardiovascular risk factors. All current smokers, including heavy smokers, should be counseled for smoking cessation as the excess cardiovascular risk starts decreasing soon after abstinence.5, 6, 26–28 Smokers who cannot quit should be encouraged to reduce their amount and/or duration of smoking as it has been shown to be associated with future smoking cessation.29
Several limitations of this study must be acknowledged. Self-reports of smoking were not validated by biochemical tests. However, most major smoking studies are based on self-reports, which have been shown to have high validity.30 Moreover, active smoking occurred >15 years before baseline (1989–1993). The amount and duration of prior smoking was estimated using pack-years. However, it is possible that the amount and duration of smoking have differential effects so that smoking three packs a day for fifteen years (45 pack-years) may be different from smoking one pack per day for 45 years (also 45 pack-years). Older former heavy smokers may be at risk of resuming smoking and self-misclassifying. However, longer duration of abstinence and older age have been shown to be associated with a lower risk of relapse.31 Heavy smokers in our study had a mean age of 74 years and mean cessation of 23 years. Residual confounding, specifically differences in unmeasured risk factors for HF between former heavy smokers versus other former smokers may help explain part of the differential risk of HF among former heavy smokers.
Conclusions
After >15 years of cessation, older former light and moderate (<32 pack-years) smokers appear to achieve the health profile of never-smokers. Although former heavy (≥32 pack-years) smokers may not achieve this, their risk is clearly lower relative to current smokers. These findings confirm the health benefit of smoking cessation compared to continued smoking, and suggest that avoidance of heavy or prolonged smoking may be necessary to achieve the full complement of health benefits of never-smokers.
Acknowledgments
Funding Sources: Amiya Ahmed is a 2012 Goldwater Scholar at the University of Alabama at Birmingham, supported by the Barry Goldwater Scholarship and Excellence in Education Program. Dr. Ahmed is supported by funds from the VA Capitol Health Care Network (VISN 5) to the Center for Health and Aging and was also in part supported by grants (R01-HL085561 and R01-HL097047) from the NHLBI, Bethesda, Maryland, which also sponsored the Cardiovascular Health Study (CHS)
Footnotes
Abstract Presentation: Preliminary results of the study were presented as two abstracts at the 2010 and 2011 American Heart Association Annual Scientific Sessions:
http://circ.ahajournals.org/cgi/content/meeting_abstract/122/21_MeetingAbstracts/A17788
http://circ.ahajournals.org/cgi/content/meeting_abstract/124/21_MeetingAbstracts/A18263
Disclosures: None
References
- 1.Lakier JB. Smoking and cardiovascular disease. Am J Med. 1992;93:8S–12S. doi: 10.1016/0002-9343(92)90620-q. [DOI] [PubMed] [Google Scholar]
- 2.Aronow WS, Cassidy J, Vangrow JS, March H, Kern JC, Goldsmith JR, Khemka M, Pagano J, Vawter M. Effect of cigarette smoking and breathing carbon monoxide on cardiovascular hemodynamics in anginal patients. Circulation. 1974;50:340–347. doi: 10.1161/01.cir.50.2.340. [DOI] [PubMed] [Google Scholar]
- 3.Aronow WS. Effect of passive smoking on angina pectoris. N Engl J Med. 1978;299:21–24. doi: 10.1056/NEJM197807062990105. [DOI] [PubMed] [Google Scholar]
- 4.Howard G, Wagenknecht LE, Burke GL, Diez-Roux A, Evans GW, McGovern P, Nieto FJ, Tell GS. Cigarette smoking and progression of atherosclerosis: The atherosclerosis risk in communities (aric) study. JAMA. 1998;279:119–124. doi: 10.1001/jama.279.2.119. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Smoking and cardiovascular disease. MMWR Morb Mortal Wkly Rep. 1984;32:677–679. [PubMed] [Google Scholar]
- 6.The Surgeon General of the United States. The health consequences of smoking: A report of the surgeon general. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2004. [Google Scholar]
- 7.von Eyben FE. Smoking cessation as a rigorous primary intervention for coronary events in middle-aged men. A commentary based on the woscop findings. West of scotland coronary prevention study. Eur Heart J. 1997;18:1187–1189. doi: 10.1093/oxfordjournals.eurheartj.a015417. [DOI] [PubMed] [Google Scholar]
- 8.Houston TK, Allison JJ, Person S, Kovac S, Williams OD, Kiefe CI. Post-myocardial infarction smoking cessation counseling: Associations with immediate and late mortality in older medicare patients. Am J Med. 2005;118:269–275. doi: 10.1016/j.amjmed.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 9.Rosenberg L, Kaufman DW, Helmrich SP, Shapiro S. The risk of myocardial infarction after quitting smoking in men under 55 years of age. N Engl J Med. 1985;313:1511–1514. doi: 10.1056/NEJM198512123132404. [DOI] [PubMed] [Google Scholar]
- 10.Omenn GS, Anderson KW, Kronmal RA, Vlietstra RE. The temporal pattern of reduction of mortality risk after smoking cessation. Am J Prev Med. 1990;6:251–257. [PubMed] [Google Scholar]
- 11.Kawachi I, Colditz GA, Stampfer MJ, Willett WC, Manson JE, Rosner B, Hunter DJ, Hennekens CH, Speizer FE. Smoking cessation in relation to total mortality rates in women. A prospective cohort study. Ann Intern Med. 1993;119:992–1000. doi: 10.7326/0003-4819-119-10-199311150-00005. [DOI] [PubMed] [Google Scholar]
- 12.Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A, O’Leary DH, Psaty B, Rautaharju P, Tracy RP, Weiler PG. The cardiovascular health study: Design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 13.Psaty BM, Furberg CD, Kuller LH, Borhani NO, Rautaharju PM, O’Leary DH, Bild DE, Robbins J, Fried LP, Reid C. Isolated systolic hypertension and subclinical cardiovascular disease in the elderly. Initial findings from the cardiovascular health study. JAMA. 1992;268:1287–1291. [PubMed] [Google Scholar]
- 14.Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, Robbins JA, Gardin JM. Risk factors for 5-year mortality in older adults: The cardiovascular health study. JAMA. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 15.Higgins MW, Enright PL, Kronmal RA, Schenker MB, Anton-Culver H, Lyles M. Smoking and lung function in elderly men and women. The cardiovascular health study. JAMA. 1993;269:2741–2748. [PubMed] [Google Scholar]
- 16.Gottdiener JS, Arnold AM, Aurigemma GP, Polak JF, Tracy RP, Kitzman DW, Gardin JM, Rutledge JE, Boineau RC. Predictors of congestive heart failure in the elderly: The cardiovascular health study. J Am Coll Cardiol. 2000;35:1628–1637. doi: 10.1016/s0735-1097(00)00582-9. [DOI] [PubMed] [Google Scholar]
- 17.Psaty BM, Kuller LH, Bild D, Burke GL, Kittner SJ, Mittelmark M, Price TR, Rautaharju PM, Robbins J. Methods of assessing prevalent cardiovascular disease in the cardiovascular health study. Ann Epidemiol. 1995;5:270–277. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- 18.Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, Cruise RG, Theroux S. Surveillance and ascertainment of cardiovascular events. The cardiovascular health study. Ann Epidemiol. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 19.Schellenbaum GD, Rea TD, Heckbert SR, Smith NL, Lumley T, Roger VL, Kitzman DW, Taylor HA, Levy D, Psaty BM. Survival associated with two sets of diagnostic criteria for congestive heart failure. Am J Epidemiol. 2004;160:628–635. doi: 10.1093/aje/kwh268. [DOI] [PubMed] [Google Scholar]
- 20.Hung J, Lam JY, Lacoste L, Letchacovski G. Cigarette smoking acutely increases platelet thrombus formation in patients with coronary artery disease taking aspirin. Circulation. 1995;92:2432–2436. doi: 10.1161/01.cir.92.9.2432. [DOI] [PubMed] [Google Scholar]
- 21.Moreno H, Jr, Chalon S, Urae A, Tangphao O, Abiose AK, Hoffman BB, Blaschke TF. Endothelial dysfunction in human hand veins is rapidly reversible after smoking cessation. Am J Physiol. 1998;275:H1040–1045. doi: 10.1152/ajpheart.1998.275.3.H1040. [DOI] [PubMed] [Google Scholar]
- 22.Johnson HM, Gossett LK, Piper ME, Aeschlimann SE, Korcarz CE, Baker TB, Fiore MC, Stein JH. Effects of smoking and smoking cessation on endothelial function: 1-year outcomes from a randomized clinical trial. J Am Coll Cardiol. 2010;55:1988–1995. doi: 10.1016/j.jacc.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corti MC, Guralnik JM, Ferrucci L, Izmirlian G, Leveille SG, Pahor M, Cohen HJ, Pieper C, Havlik RJ. Evidence for a black-white crossover in all-cause and coronary heart disease mortality in an older population: The north carolina epese. Am J Public Health. 1999;89:308–314. doi: 10.2105/ajph.89.3.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iso H, Date C, Yamamoto A, Toyoshima H, Watanabe Y, Kikuchi S, Koizumi A, Wada Y, Kondo T, Inaba Y, Tamakoshi A, Group JS. Smoking cessation and mortality from cardiovascular disease among japanese men and women: The jacc study. Am J Epidemiol. 2005;161:170–179. doi: 10.1093/aje/kwi027. [DOI] [PubMed] [Google Scholar]
- 25.Wolf PA, D’Agostino RB, Kannel WB, Bonita R, Belanger AJ. Cigarette smoking as a risk factor for stroke. The framingham study. JAMA. 1988;259:1025–1029. [PubMed] [Google Scholar]
- 26.Bruintjes G, Bartelson BB, Hurst P, Levinson AH, Hokanson JE, Krantz MJ. Reduction in acute myocardial infarction hospitalization after implementation of a smoking ordinance. Am J Med. 2011;124:647–654. doi: 10.1016/j.amjmed.2011.02.022. [DOI] [PubMed] [Google Scholar]
- 27.Nides M. Update on pharmacologic options for smoking cessation treatment. Am J Med. 2008;121:S20–31. doi: 10.1016/j.amjmed.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 28.Hatsukami DK, Rennard S, Patel MK, Kotlyar M, Malcolm R, Nides MA, Dozier G, Bars MP, Jamerson BD. Effects of sustained-release bupropion among persons interested in reducing but not quitting smoking. Am J Med. 2004;116:151–157. doi: 10.1016/j.amjmed.2003.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Okuyemi KS, Thomas JL, Warren J, Guo H, Ahluwalia JS. Relationship between smoking reduction and cessation among light smokers. Nicotine Tob Res. 2010;12:1005–1010. doi: 10.1093/ntr/ntq138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: A review and meta-analysis. Am J Public Health. 1994;84:1086–1093. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hawkins J, Hollingworth W, Campbell R. Long-term smoking relapse: A study using the british household panel survey. Nicotine Tob Res. 2010;12:1228–1235. doi: 10.1093/ntr/ntq175. [DOI] [PubMed] [Google Scholar]