Abstract
Background and purpose
The use of uncemented fixation in total hip arthroplasty (THA) is increasing. Registry studies have indicated an increased risk of revision of uncemented implants due to early periprosthetic femoral fracture. In this paper, we describe the incidence and predisposing factors for intraoperative and early postoperative (≤ 90 days) periprosthetic femoral fractures after cemented and uncemented THA.
Patients and methods
This was a prospective observational study in 8 Danish high-volume centers from February 2010 to November 2013. We used the 90-day follow-up from the Danish National Patient Registry and patient records. We obtained intraoperative information from the Danish Hip Arthroplasty Registry and from surgical notes.
Results
Of 7,169 primary consecutive THAs, 5,482 (77%) were performed using uncemented femoral components. The total incidence of periprosthetic femoral fractures ≤ 90 days postoperatively was 2.1% (n = 150). 70 fractures were detected intraoperatively (46 required osteosynthesis). 51 postoperatively detected fractures occurred without trauma (42 of which were reoperated) and 29 were postoperative fall-related fractures (27 of which were reoperated). 134 fractures (2.4%) were found in uncemented femoral components and 16 (0.9%) were found in cemented femoral components (p < 0.001). Uncemented femoral stem (relative risk (RR) = 4.1, 95% CI: 2.3–7.2), medically treated osteoporosis (RR =2.8, CI: 1.6–4.8), female sex (RR =1.6, CI: 1.1–2.2), and age (RR =1.4 per 10 years, CI: 1.2–1.6) were associated with increased risk of periprosthetic femoral fracture when analyzed using multivariable regression analysis.
Interpretation
Uncemented femoral components were associated with an increased risk of early periprosthetic femoral fractures, especially in elderly, female, and osteoporotic patients.
The use of uncemented fixation technique in total hip arthroplasty (THA) is increasing in Scandinavia (NARA 2015), western European countries (NJR 2015), Australia (AOANJRR 2015), and the USA (Troelsen et al. 2013). In Denmark in 2014, only 12% of THAs were cemented, 18% were hybrids, and the remaining 70% were uncemented (DHR 2015). One reason for the high proportion of uncemented THAs may be lower revision rates due to aseptic loosening (Wechter et al. 2013, DHR 2015). Other reasons could be the shorter operation time or the potentially higher risk of pulmonary emboli (acute cementation syndrome) associated with the cementation procedure (Pitto et al. 1999, Olsen et al. 2014). However, results from the combined Nordic registries have shown an increased risk of revision of uncemented implants with early periprosthetic femoral fractures being the major course of failure (Makela et al. 2014, Thien et al. 2014). Furthermore, the revision procedures performed for periprosthetic fractures are complex surgical procedures often associated with a high risk of complications and mortality (Bhattacharyya et al. 2007, Zuurmond et al. 2010, Griffiths et al. 2013).
In addition to choice of fixation technique, osteoporosis, rheumatoid arthritis, high age, high BMI, female sex, previous surgery, and anatomical deformities have been associated with increased risk of early periprosthetic fractures (Sidler-Maier and Waddell 2015). Early mobilization on the day of surgery might also be a stress riser and increase the risk of early femoral periprosthetic fractures after uncemented THA (Franklin and Malchau 2007, Hu et al. 2010, Solgaard and Kjersgaard 2014).
Current knowledge of incidences and reasons for these fractures is mainly based on large-scale registry studies, and there have been no prospective multicenter studies including detailed information on patient characteristics (Sidler-Maier and Waddell 2015). Here we describe the incidence and predisposing factors for intraoperative and early postoperative (≤ 90 days) periprosthetic femoral fractures after cemented and uncemented THA.
Patients and methods
Data on 8,439 primary THA procedures were collected between February 2010 and November 2013 in 8 departments reporting to the Lundbeck Foundation Centre for Fast-track THA and TKA Database (LCDB). 7,169 primary elective THA procedures were available for analysis after exclusions (Figure 1). All acute procedures (fractures and sequelae after fractures (< 3 months)) and tumor cases were excluded. These exclusions are in accordance with previous studies based on data from the LCDB (Jorgensen et al. 2014, Pitter et al. 2016). All departments have implemented the fast-track methodology, including neuroaxial anesthesia, opioid-sparing analgesia with acetaminophen, non-steroid anti-inflammatory drugs (NSAIDs), and early mobilization, regardless of age or pre-existing comorbidity. The LCDB contains data on preoperative comorbidity and patient characteristics such as pharmacological treatment for osteoporosis, BMI, use of walking aids, alcohol consumption, smoking habits, and living conditions. Data are prospectively collected from patients within 1 month before surgery using self-completed questionnaires with staff available for assistance (Jorgensen and Kehlet 2013).
Figure 1.
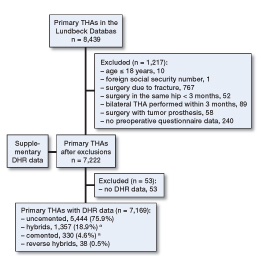
Study population. a Cemented femoral stems.
Supplementary data on types of implants, fixation technique, duration of surgery, indication, previous surgeries, and intraoperative complications (including intraoperative periprosthetic fractures) were available from the Danish Hip Arthroplasty Registry (DHR) in 99% of cases (Figure 1). Intraoperative periprosthetic fractures were registered in the DHR by the orthopedic surgeons performing the THA procedures. The early postoperative periprosthetic fractures within 90 days of surgery were divided into fall-related fractures and fractures without trauma, and identified/analyzed by examination of length of hospital stay (LOS) > 4 days and also 90-day re-admissions. All patients with a LOS of >4 days had their medical records examined to determine the reason for prolonged LOS. Using the patients’ unique Danish social security numbers (Central Office of Civil Registration), we obtained information on 90-day re-admissions from the Danish National Patient Registry (Lynge et al. 2011). As reporting to the Danish National Patient Registry is mandatory for hospitals to receive reimbursement, an almost complete follow-up (> 98.5%) is assured (Andersen et al. 1999). All unplanned admissions with an overnight hospital stay within 90 days postoperatively were evaluated using discharge records or patient records and were included as re-admissions if related to index surgery.
Statistics
Means (with ranges) are reported for normally distributed data and proportions are expressed as percentage with 95% confidence interval (CI). Normally distributed data were compared using Student’s t-test and crude comparisons of proportions were done using a chi-squared test. Analysis of potential risk factors associated with early periprosthetic femoral fractures was performed using a multivariable Poisson regression model with robust error variance, as described by Zou (2004). 58 cases with missing data (0.8%) were excluded from analysis. Results are given as relative risk (RR) estimates or percentages with CI. Any p-value of <0.05 was considered significant. Analysis was done using SPSS version 20.
Ethics and registration
The National Ethics Committee waived the need for approval, as this was an observational non-interventional study. Permission was obtained from the Danish Data Protection Agency and the Danish National Board of Health to review and store all data and medical records. The LCDB is registered at ClinicalTrials.gov (identifier: NCT01515670) as an ongoing study registry on preoperative patient characteristics and postoperative morbidity. Previous articles on preoperative risk factors and postoperative morbidity and complications have been published on this cohort (Pitter et al. 2016) and earlier cohorts that contributed to the patients included in this study (Jorgensen and Kehlet 2013).
Funding and potential conflicts of interests
This study was funded by the Lundbeck Foundation Centre for Fast-Track Hip and Knee Arthroplasty, Copenhagen, Denmark.
No competing interests declared.
Results
7,169 primary THA procedures were performed in 6,783 patients. The femoral component was uncemented in 5,482 procedures (77%) and cemented in 1,657 (23%) (Figure 1). The frequency of the use of uncemented femoral components varied between centers, from 47.6% to 97.7% (Table 1).
Table 1.
Surgical centers and related outcomes
| Center | Total n | Mean age | Uncemented femoral stem n (%) | Duration of surgery, min mean (range) | Fracturesa n (%) |
|---|---|---|---|---|---|
| 1 | 739 | 69 | 586 (79) | 75 (26–200) | 15 (2.0) |
| 2 | 1,158 | 67 | 1,058 (91) | 52 (23–210) | 46 (4.0) |
| 3 | 809 | 64 | 518 (64) | 68 (30–225) | 17 (2.1) |
| 4 | 1,269 | 69 | 1,050 (83) | 46 (18–200) | 15 (1.2) |
| 5 | 1,141 | 67 | 819 (72) | 60 (30–150) | 30 (2.6) |
| 6 | 1,118 | 69 | 569 (51) | 61 (30–218) | 6 (0.5) |
| 7 | 872 | 70 | 852 (98) | 53 (31–128) | 21 (2.4) |
| 8 | 63 | 69 | 30 (48) | 63 (35–150) | 0 |
Intraoperative and early postoperative
The total incidence of periprosthetic femoral fracture ≤90 days postoperatively was 2.1% (n = 150) (Table 2). 70 fractures (1.0%) were detected intraoperatively, 51 (0.7%) were detected postoperatively and occurred without trauma, and 29 (0.4%) occurred postoperatively and were fall-related (Table 3). The fracture incidence was 2.4% (n = 134) in cases with uncemented femoral components and 0.9% (n = 16) in cases with cemented femoral components (p < 0.001). The fracture incidence with uncemented femoral implants increased with increasing age (Figure 2).
Table 2.
Patient and surgical characteristics in relation to periprosthetic femoral fractures. Values are number of cases (percentage) unless otherwise stated
| Total cohort n = 7,169 | Uncemented femoral stem n = 5,482 (76.5%) | Cemented femoral stem n = 1,687 (23.5%) | |
|---|---|---|---|
| Patient characteristics | |||
| Age, mean (range) | 68 (18–100) | 66 (18–97) | 75 (31–100) |
| Female sex | 3,928 (56) | 2,811 (51) | 1,117 (66) |
| Medically treated osteoporosis | 241 (3.4) | 119 (2.2) | 122 (7.2) |
| BMI, mean (range)a | 27 (15–55) | 27 (15–55) | 26 (15–46) |
| Mobility aid | 1,858 (26) | 1,164 (21) | 694 (41) |
| Alcohol consumption >2 units/day | 575 (8.0) | 503 (9.2) | 72 (4.3) |
| Smoker (%) | 1,144 (16) | 940 (17) | 204 (12) |
| Surgical characteristics | |||
| Diagnosis other than primary arthrosisa | 985 (13) | 709 (13) | 276 (16) |
| Previous surgery in the same hip | 440 (6.1) | 305 (5.6) | 135 (8.0) |
| Duration of surgery (range)b | 58 (18–225) | 55 (18–218) | 69 (28–225) |
| Outcomes – periprosthetic femoral fractures | |||
| Intraoperative | 70 (1.0) | 58 (1.1) | 12 (0.7) |
| Postoperative, without trauma | 51 (0.7) | 48 (0.9) | 3 (0.2) |
| Postoperative, fall-related | 29 (0.4) | 28 (0.5) | 1 (0.1) |
| Early, in total | 150 (2.1) | 134 (2.4) | 16 (0.9) |
Data missing in 29 cases.
Data missing in 8 cases.
Table 3.
Causes of periprosthetic femoral fracture and consequences for the patient
| Causes of fracture/Consequences |
|---|
| Intraoperative periprosthetic femoral fracture (n = 70): |
| No osteosynthesis and full weight bearing: 23 |
| No osteosynthesis + limited weight bearing: 1 |
| Osteosynthesis and full weight bearing: 33 |
| Osteosynthesis + limited weight bearing: 13 |
| Postoperative periprosthetic femoral fracture without trauma (n = 51): |
| Conservative treatment: 9 |
| Reoperation: 5 (during primary admission) |
| Reoperation: 37 (re-admitted) |
| Postoperative periprosthetic femoral fracture, fall-related (n = 29): |
| Conservative treatment: 2 |
| Reoperation: 27 |
Figure 2.
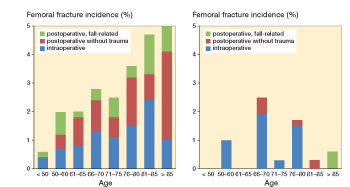
Incidence of early periprosthetic femoral fracture using uncemented (left panel) and cemented femoral components (right panel), in relation to age.
Uncemented femoral stem (RR =4.1, 95% CI: 2.3–7.2), medically treated osteoporosis (RR =2.8, CI: 1.6–4.8), female sex (RR =1.6, CI: 1.1–2.2), and age (RR =1.4 per 10 years, CI: 1.2–1.6) were associated with increased risk of periprosthetic femoral fracture when analyzed using multivariable regression analysis (Table 4).
Table 4.
Multivariable Poisson regression analysis of potential risk factors influencing the risk of periprosthetic femoral fracture
| Risk factor | Relative risk | 95% CI | p-value |
|---|---|---|---|
| Uncemeted femoral stem | 4.1 | 2.3–7.2 | < 0.001 |
| Cemented femoral stem (reference) | 1 | ||
| Diagnosis other than athrosis | 1.4 | 0.9–2.3 | 0.1 |
| Arthosis (reference) | 1 | ||
| Female sex | 1.6 | 1.1–2.2 | 0.009 |
| Male sex (reference) | 1 | ||
| Medically treated osteoporosis | 2.8 | 1.6–4.8 | < 0.001 |
| No osteoporosis (reference) | 1 | ||
| BMI ≥30 | 0.9 | 0.6–1.3 | 0.5 |
| BMI <30 (reference) | 1 | ||
| Age (per 10 years) | 1.4 | 1.2–1.6 | < 0.001 |
Discussion
Data on periprosthetic femoral fractures after THA have mainly been based on large-scale registry-based studies reporting revisions caused by periprosthetic fractures (Troelsen et al. 2013, Makela et al. 2014, Thien et al. 2014). The incidence of periprosthetic fractures causing revision within 2 years after THA is only 0.5% in the Nordic Arthroplasty Register Association database (Thien et al. 2014). Other authors have described incidences and risk factors for intraoperatively observed periprosthetic fractures (Sidler-Maier and Waddell 2015, Miettinen et al. 2016). We have presented a detailed analysis of both intraoperative and early postoperative periprosthetic femoral fractures, and not only fractures causing revision. Thus, the frequency of 2.1% of periprosthetic femoral fractures is close to the "true" incidence.
We found that the uncemented femoral components were used in 77% of all procedures, and that the incidence of periprosthetic femoral fractures in these cases increased with age. Furthermore, an uncemented femoral stem was associated with increased risk of periprosthetic fracture when analyzed in multivariable regression analysis. These findings are in accordance with the findings from the Nordic Arthroplasty Register database (Makela et al. 2014, Thien et al. 2014). Medically treated osteoporosis and female sex were also associated with an increased risk of early periprosthetic fractures in the present study, supporting the fact that osteoporosis and female sex are generally accepted as being independent risk factors for periprosthetic femoral fracture (Napoli et al. 2012, Bonnin et al. 2015, Ponzio et al. 2015, Sidler-Maier and Waddell 2015).
The 8 centers that contributed with data to this study were all part of the multicenter collaboration in the Lundbeck Foundation Centre for Fast-Track Hip and Knee Arthroplasty, with uniform perioperative setup. The indications for cemented and uncemented fixation technique were not uniform and varied considerably between centers, with some having >90% uncemented femoral components and others about 50%. The use of almost exclusively uncemented implants is also seen in many high-volume centers in the USA (Troelsen et al. 2013). A shorter operation time may be an explanation, but the main reason for the extensive use in some departments in Denmark is rather the potentially improved prosthetic survival with fewer cases of aseptic loosening (Wechter et al. 2013, DHR 2015).
One limitation of this multicenter study was the observational design, but large-scale randomized controlled trials addressing periprosthetic fractures are difficult to design due to the very large numbers needed to achieve sufficient power. Another limitation is the lack of information on surgeon volume, as THA surgery performed by a low-volume surgeon may be an independent risk factor for periprosthetic femoral fracture (Ravi et al. 2014). Some intraoperative periprosthetic fractures may not be reported to the DHR or may be unrecognized, but most of the potentially unrecognized intraoperative fractures are likely to be found and included as early postoperative fractures without trauma. We do acknowledge that the intraoperatively recognized fractures differ from the postoperative fractures in both treatment and outcome. The postoperative fractures are associated with complex reoperations, whereas the intraoperatively recognized fractures are treated immediately and are often associated with no restrictions—or only limited weight bearing. However, we chose to include all fractures to present the total incidence of early periprosthetic femoral fracture. Finally, no radiological analysis of fractures and no preoperative radiological evaluation of Dorr-type femur and its potential association with fractures was performed, as this was not part of the aim of the study. Both age and osteoporosis may be associated with Dorr-type femur, and the finding of advanced age and osteoporosis as risk factors for periprosthetic fracture may reflect reduced cortical thickness indices and lower Dorr type (Dorr B and especially C) (Nash and Harris 2014). A strength of the present study was the prospectively collected information on patient characteristics and surgical details, enabling multivariable regression analysis. Also, the almost complete (99%) follow-up in the DNPR (Andersen et al. 1999) supports our conclusions.
The surgical dilemma of choosing between the uncemented concept, accepting the increased risk of early periprosthetic fracture, and the cemented concept with the increased risk of aseptic loosening has not been solved by the present study, but it provides important additional information to the ongoing debate.
In summary, uncemented femoral components were found to increase the risk of early periprosthetic femoral fracture, especially in elderly, female, and osteoporotic patients, thus emphasizing the need for patient selection and careful surgical technique in order to minimize the number of early fractures when using uncemented femoral components.
MLL, CJ, AGK, SS, and HK wrote the protocol. MLL and CJ undertook all data gathering. MLL and CJ performed and evaluated the statistical analyses. MLL wrote the first draft of the manuscript and all authors including the collaborators revised the draft and approved the final version.
References
- AOANJRR 2015. Australian Orhtopaedic Association National Joint Replacement Registry, Annual Report 2015. Available from https://aoanjrr.sahmri.com/. [Google Scholar]
- DHR 2015. The Danish Hip Arthroplasty Register, Annual Report 2015. Available from http://www.dhr.dk/. [Google Scholar]
- LCDB Lundbeck Foundation Centre for Fast-Track Hip and Knee Replacement. Available from Lundbeck Foundation Centre for Fast-Track Hip and Knee Replacement http://www.fthk.dk/. [Google Scholar]
- NARA 2015. Nordic Arthroplastic Register Association (NARA), Annual Report 2015. Available from https://stratum.registercentrum.se/#!page?id=1150. [Google Scholar]
- NJR 2015. National Joint Registry for England and Wales (NRJ England Wales), Annual Report 2015. Available from http://www.njrcentre.org.uk/njrcentre/default.aspx. [Google Scholar]
- Andersen T F, Madsen M, Jorgensen J, Mellemkjoer L, Olsen J H.. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 1999; 46(3): 263–8. [PubMed] [Google Scholar]
- Bhattacharyya T, Chang D, Meigs J B, Estok D M, Malchau H.. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am 2007; 89(12): 2658–62. [DOI] [PubMed] [Google Scholar]
- Bonnin M P, Neto C C, Aitsiselmi T, Murphy C G, Bossard N, Roche S.. Increased incidence of femoral fractures in small femurs and women undergoing uncemented total hip arthroplasty - why? Bone Joint J 2015; 97-B(6): 741–8. [DOI] [PubMed] [Google Scholar]
- Franklin J, Malchau H.. Risk factors for periprosthetic femoral fracture. Injury 2007; 38(6): 655–660. [DOI] [PubMed] [Google Scholar]
- Griffiths E J, Cash D J, Kalra S, Hopgood P J.. Time to surgery and 30-day morbidity and mortality of periprosthetic hip fractures. Injury 2013; 44(12): 1949–52. [DOI] [PubMed] [Google Scholar]
- Hu K, Zhang X, Zhu J, Wang C, Ji W, Bai X.. Periprosthetic fractures may be more likely in cementless femoral stems with sharp edges. Ir J Med Sci 2010; 179(3): 417–21. [DOI] [PubMed] [Google Scholar]
- Jorgensen C C, Kehlet H.. Role of patient characteristics for fast-track hip and knee arthroplasty. Br J Anaesth 2013; 110(6): 972–80. [DOI] [PubMed] [Google Scholar]
- Jorgensen C C, Kjaersgaard-Andersen P, Solgaard S, Kehlet H.. Hip dislocations after 2,734 elective unilateral fast-track total hip arthroplasties: incidence, circumstances and predisposing factors. Arch Orthop Trauma Surg 2014; 134(11): 1615–22. [DOI] [PubMed] [Google Scholar]
- Lynge E, Sandegaard J L, Rebolj M.. The Danish National Patient Register. Scand J Public Health 2011; 39(7 Suppl): 30–33. [DOI] [PubMed] [Google Scholar]
- Makela K T, Matilainen M, Pulkkinen P, Fenstad A M, Havelin L, Engesaeter L, Furnes O, Pedersen A B, Overgaard S, Karrholm J, Malchau H, Garellick G, Ranstam J, Eskelinen A.. Failure rate of cemented and uncemented total hip replacements: register study of combined Nordic database of four nations. BMJ 2014; 348: f7592. [DOI] [PubMed] [Google Scholar]
- Miettinen S S, Makinen T J, Kostensalo I, Makela K, Huhtala H, Kettunen J S, Remes V.. Risk factors for intraoperative calcar fracture in cementless total hip arthroplasty. Acta Orthop 2016; 87(2): 113–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napoli N, Jin J, Peters K, Wustrack R, Burch S, Chau A, Cauley J, Ensrud K, Kelly M, Black D M.. Are women with thicker cortices in the femoral shaft at higher risk of subtrochanteric/diaphyseal fractures? The study of osteoporotic fractures. J Clin Endocrinol Metab 2012; 97(7): 2414–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash W, Harris A.. The Dorr type and cortical thickness index of the proximal femur for predicting peri-operative complications during hemiarthroplasty. J Orthop Surg (Hong Kong) 2014; 22(1): 92–5. [DOI] [PubMed] [Google Scholar]
- Olsen F, Kotyra M, Houltz E, Ricksten S E.. Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: incidence, risk factors, and effect on outcome. Br J Anaesth 2014; 113(5): 800–6. [DOI] [PubMed] [Google Scholar]
- Pitter F T, Jorgensen C C, Lindberg-Larsen M, Kehlet H.. Postoperative morbidity and discharge destinations after fast-track hip and knee arthroplasty in patients older than 85 years. Anesth Analg 2016; 122(6): 1807–15. [DOI] [PubMed] [Google Scholar]
- Pitto R P, Koessler M, Kuehle J W.. Comparison of fixation of the femoral component without cement and fixation with use of a bone-vacuum cementing technique for the prevention of fat embolism during total hip arthroplasty. A prospective, randomized clinical trial. J Bone Joint Surg Am 1999; 81(6): 831–43. [DOI] [PubMed] [Google Scholar]
- Ponzio D Y, Shahi A, Park A G, Purtill J J.. Intraoperative proximal femoral fracture in primary cementless total hip arthroplasty. J Arthroplasty 2015; 30(8): 1418–22. [DOI] [PubMed] [Google Scholar]
- Ravi B, Jenkinson R, Austin P C, Croxford R, Wasserstein D, Escott B, Paterson J M, Kreder H, Hawker G A.. Relation between surgeon volume and risk of complications after total hip arthroplasty: propensity score matched cohort study. BMJ 2014; 348: g3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidler-Maier C C, Waddell J P.. Incidence and predisposing factors of periprosthetic proximal femoral fractures: a literature review. Int Orthop 2015; 39(9): 1673–82. [DOI] [PubMed] [Google Scholar]
- Solgaard S, Kjersgaard A G.. Increased risk for early periprosthetic fractures after uncemented total hip replacement. Dan Med J 2014; 61(2): A4767. [PubMed] [Google Scholar]
- Thien T M, Chatziagorou G, Garellick G, Furnes O, Havelin L I, Makela K, Overgaard S, Pedersen A, Eskelinen A, Pulkkinen P, Karrholm J.. Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the Nordic Arthroplasty Register Association database. J Bone Joint Surg Am 2014; 96(19): e167. [DOI] [PubMed] [Google Scholar]
- Troelsen A, Malchau E, Sillesen N, Malchau H.. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res 2013; 471(7): 2052–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechter J, Comfort T K, Tatman P, Mehle S, Gioe T J.. Improved survival of uncemented versus cemented femoral stems in patients aged <70 years in a community total joint registry. Clin Orthop Relat Res 2013; 471(11): 3588–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159(7): 702–6. [DOI] [PubMed] [Google Scholar]
- Zuurmond R G, van W W, van Raay J J, Bulstra S K.. High incidence of complications and poor clinical outcome in the operative treatment of periprosthetic femoral fractures: An analysis of 71 cases. Injury 2010; 41(6): 629–33. [DOI] [PubMed] [Google Scholar]


